Abstract
Corneal transplantation is the most common form of organ transplantation in the United States with between 45,000 and 55,000 procedures performed each year. While several animal models exist for this procedure and mice are the species that is most commonly used. The reasons for using mice are the relative cost of using this species, the existence of many genetically defined strains that allow for the study of immune responses, and the existence of an extensive array of reagents that can be used to further define responses in this species. This model has been used to define factors in the cornea that are responsible for the relative immune privilege status of this tissue that enables corneal allografts to survive acute rejection in the absence of immunosuppressive therapy. It has also been used to define those factors that are most important in rejection of such allografts. Consequently, much of what we know concerning mechanisms of both corneal allograft acceptance and rejection are due to studies using a murine model of corneal transplantation. In addition to describing a model for acute corneal allograft rejection, we also present for the first time a model of late-term corneal allograft rejection.
Keywords: Immunology, Issue 93, Transplantation, Allograft Responses, Immune Privilege, Cornea, Inflammatory cells, T cells, Macrophages
Introduction
Corneal transplantation is one of the most successful and common types of transplantation performed in humans. The reasons why this surgery is performed are a result of injury, infectious disease1, or other forms of non-infectious corneal disease2. Figures from the Eye Bank Association of America indicate that over 46,000 were performed in 2011 (see web site at: restoresight.org/eye_banks/eye_banks.html). An indication of its success is that one year failure rates for allogeneic corneal grafts range from 10 to 15% and at 5 years the success is in excess of 70%3-8. As many studies have shown, the success of corneal allografts is directly related to the fact that the eye is an immunologically privileged site. Factors responsible for the corneas status as an immune privilege site include the lack of both blood and lymph vessels in the cornea, a relative absence of antigen presenting cells, factors produced by the cornea that suppress immune effector funtions9-15, low expression of MHC antigens16, and the expression of FasL17-20.
However, in spite of these factors predisposing these grafts for success, they do undergo rejection3-7. Consequently, understanding those mechanisms that mediate this rejection as well as testing various therapies to prevent rejection is of critical importance. To that end, we describe here a murine model of corneal transplantation that has been in use for over 20 years to study corneal transplantation in a controlled experimental environment. Since transplantation responses involve many different factors working in concert that will ultimate determine whether the transplanted tissue fails or succeeds, it is not possible to understand the importance of those factors in any in vitro model. Consequently, studies using intact animals are required to determine what factors are important to either success or failure of transplanted tissue.
While other species of animals have been used to study corneal transplantation, the murine model has several advantages when compared to using other species. The first is the existence of many strains of mice that express certain transgenes or have been gene-targeted to lack expression of specific immunological factors whose function in transplantation can be better studied. In addition, there are many reagents (both recombinant factors and antibodies that neutralize factors) that are specific for mice and which do not exist for many other species of animals. Because of the existence of these factors, this model has been used extensively to identify relevant factors involved in acute corneal allograft responses15,17,18,20-29. Furthermore, many of the factors involved in corneal transplantation are also known to be functional in transplantation of other tissues.
Protocol
NOTE: All animals used in this procedure are treated in accordance with the Association for Research in Vision and Ophthalmology statement for the Use of Animals in Ophthalmic and Vision Research as well as the guidelines set down by the animal oversight committee at Saint Louis University. NOTE: All surgical instruments and solutions are sterilized prior to surgery to limit microbial infection of the eye. It should be noted that while the animals do experience some pain from this procedure, we do not employ analgesics. The reason for this is because all analgesics are anti-inflammatory and since corneal transplantation responses involve inflammation, the use of anti-inflammatory drugs would compromise our ability to determine what factors are involved in corneal graft failure.
1. Anesthesia
Place donor and recipient mice under general anesthesia by IP injections of ketamine (86.98 mg/kg) and xylazine (13.04 mg/kg).
Keep the recipient mouse under anesthesia throughout the procedure which typically takes 30 min to an hr. Consequently, constantly monitor the mouse for any signs of regaining consciousness.
Apply puralube ointment to the eye that will not undergo surgery after the animal is anesthetized to prevent dryness.
2. Corneal Grafting
- Obtaining the donor corneal button.
- Once the animal is fully anesthetized, achieve adequate mydriasis by administration of a couple of eye drops of 1% tropicamide and 2.5% phenylephrine hydrochloride.
- Position the head of the donor animal horizontally on a board placed on a sturdy movable support. Fix the head with a strip of tape across the neck to ensure that the eye is in a horizontal position throughout the entire operation.
- Using a 2 mm diameter trephine, whose tip was dyed with methyl blue, outline the central cornea graft site.
- With a sharp blade, penetrate the cornea and inject healon into the anterior chamber to deepen it to reduce the chance of damage to the donor endothelium and underlying lens.
- Excise the donor graft with vannas scissors and place into a dish containing Hanks’ balanced salt solution until use.
- After the donor graft has been the removed, euthanize the donor mouse via CO2 inhalation.
- Preparing the graft bed.
- Repeat the same steps as described in 2.1.1 through 2.1.2 for the recipient.
- Using a 1.5 mm diameter trephine, outline the recipient graft site.
- With a sharp blade, penetrate the cornea and inject healon into the anterior chamber to deepen it to reduce the chance of damage to the underlying lens.
- Remove the outlined central corneal button from the recipient using vannas scissors and discard.
- Suturing the graft
- Place the donor cornea over the graft bed in the recipient’s cornea. Be sure that adequate healon is under the donor cornea to protect the donor endothelial cells from damage by direct contact with lens.
- Using super fine tipped microforceps, place the first bite of 11-0 nylon suture into the donor side, through the donor with 90% depth of full thickness to recipient’s side, then tie off.
- Once the cornea is anchored in place, perform midcardinal interrupted sutures such that the cornea has 8 to 10 total sutures and the donor cornea is securely lined up with and attached to the recipient corneal graft bed.
- Deepening the anterior chamber
- Deepen the anterior chamber by injecting HBSS or air bubble into the anterior chamber and gently check the integrity of the corneal graft for leakage with a cellulose sponge. NOTE: If the anterior chamber cannot be reformed then there is a high probability of cataract which will make future evaluations of the transplanted cornea very difficult and will also potentially lead to donor corneal endothelium dysfunction and thus graft failure.
- Final evaluation
- Observe the eye to determine that the pupil is round and the depth of the anterior chamber is normal. NOTE: If the pupil is not round this indicates that during suturing the iris was damaged and thus the graft is considered a technical failure.
- Apply antibiotic ointment to the eye. Optional: Close the eye lid with a 7-0 silk suture.
- Observe mice until they are fully awake and then individually house them for a minimum of two days post-surgery.
3. Suture Removal
In those cases where lid suture is used, anesthetize mice as described above and remove the lid suture at 48 hr.
Anesthetize mice on day 7 postoperatively. Remove the sutures securing the corneal graft. Once the sutures are removed and the animal has fully awakened, return it to its cage.
4. Clinical Evaluation
- Examine the eye for indications of procedural complications which include, cataract (clouding of the lens), hyphema (blood in the anterior chamber), an anterior chamber that is not of the proper depth, or significant opacity of the cornea. Consider those that demonstrate these complications as “compromised” and euthanize them by CO2 inhalation.
- Perform all examinations on unanesthetized mice. Hold the mouse with one hand thus restraining the mouse so that the other hand can proptose the eye to enable a better view of the eye. Once observations are completed, return the animal to its cage.
- Have an observer unfamiliar with the treatment groups evaluate transplanted corneas 2 to 3 times a week for signs of corneal graft rejection episodes or corneal graft failure. Use either the surgical microscope or a horizontal slit-lamp biomicroscope for these observations.
- Evaluate every cornea for opacity using a scale of 0 to 5. The scale is defined as follows:
- Assign a score of 0 to those corneas that have no signs of opacity.
- Assign a score of 1 to those corneas that show minimal superficial opacity.
- Assign a score of 2 to corneas that display mild and deeper opacity but the underlying pupil and iris are still discernable.
- Assign a score of 3 to cornea that display stromal opacity wherein the iris cannot be seen in detail with the exception of the pupil margins.
- Assign a score of 4 to cornea that display dense stromal opacity and if no underlying structures can be viewed.
- Assign a score of 5 to cornea that display complete opacity and intensive stromal edema, with pupil and iris totally obscured.
- Also evaluate every cornea for the degree of blood vessel infiltration (neovascularization) using a rating scale of 1 to 8. To accomplish this, view the cornea as consisting of 4 equal quadrants and determine the amount of blood vessels in each of these quadrants with a score that will range from 0 (no vessels) to 2 for extensive vascularization of that quadrant. Add the individual scores from each quadrant to calculate the final neovascularization score.
- Classify corneas as acutely rejected if they have a score of 3 for two consecutive observations for time points up to 5 weeks.
- Classify mice whose corneas were clear at 5 weeks but develop opacification at times >45 days post engraftment, with a score of 3 for two consecutive time points, as having undergone late-term corneal allograft rejection. Use Kaplan-Meier survival curves to analyze graft survival.
5. Manipulation of the Model
- Preparation of single cells from the spleen.
- To prepare single cells, first euthanize the donor mouse. Then, remove the spleen.
- Place the spleen in a cell strainer and disrupt it with a syringe plunger from a 3 ml syringe.
- Wash cells and resuspend in 10 ml of Hanks Balanced Salt Solution.
- Remove 10 μl of cell suspension and add to 10 μl of 0.4% trypan blue and mix. Add that to hemocytometer and count the cells in the central grid. The number of cells in tube is the cell count x 104 x 2 (dilution factor in trypan blue) x 10 (volume in the tube).
- Injection into the anterior chamber.
- Anesthetize mice as previously described.
- Perform injections using a dissecting microscope. For each intracameral injection, use 106 spleen cells in a 0.005 ml volume and a 0.25 ml microliter syringe fitted with a 33 G needle. NOTE: Other manipulations of the model can be performed by treating animals with reagents that act as either antagonists or agonists to determine the role that a particular factor may play following orthotopic corneal allograft surgery.
Representative Results
The murine model of corneal transplantation has been used for over 20 years to successfully characterize mechanisms of both corneal allograft rejection19-23 and corneal allograft acceptance13,15,16,18, 24-27. This model was used to establish the importance of FasL expression in corneal allograft acceptance, in that animals that lack FasL were not able to accept corneal allografts15. It has also been used to demonstrate that vascular endothelial growth factor receptor 1 morpholino treatment significantly increases corneal graft survival28. In a very recent report this model was used to test whether pretreatment of mice prior to corneal engraftment with corticosteroids held any therapeutic benefit29. The authors showed that such pretreatment did improve the survival rate of corneal allografts29. These reports clearly demonstrate that the primary advantage of this model is that one can study in a live animal those things that are believed to be important to the success of corneal transplants in humans.
Previous studies from this laboratory have reported that one of the chief mechanisms responsible for corneal allograft rejection is the establishment of systemic delayed-type hypersensitivity (DTH) to specific alloantigens expressed by the corneal allograft19,20. We have since used this model to test whether establishment of systemic alloantigen DTH tolerance to alloantigens expressed by the donor corneal allograft improves survival of such grafts. As shown in Figure 1, BALB/c mice tolerized to C57BL/10 (B10) alloantigens did not improve corneal allograft acceptance as measured by mean survival time for these corneal allografts. Thus the mean survival time for rejected corneas was the same whether mice were tolerized or not. We also performed similar studies using skin graft responses as a means of testing the effectiveness of systemic DTH tolerization. These studies demonstrated that when DTH tolerance was established in BALB/c mice towards B10 alloantigens, skin grafts bearing some (B10.D2 and C.B10-H-2b) or all of B10 alloantigens did not display any increased mean survival time (Figure 2). We concluded from these studies that BALB/c mice that had established antigen-specific DTH responses did not derive any measurable benefit from such tolerance for either corneal or skin allografts. These data also indicate that information generated studying a murine model of corneal transplantation will, at times, be directly applicable to other forms of solid tissue transplantation.
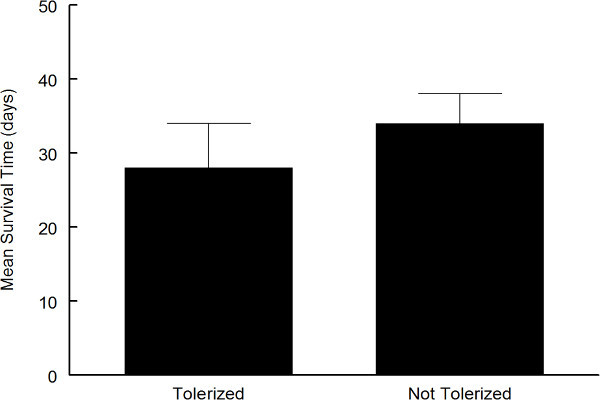 Figure 1. BALB/c mice were injected into the anterior chamber with 106 spleen cells from C57BL/10 (B10) mice. Full thickness B10 corneal grafts were then placed on BALB/c mice injected with B10 (n = 10) or mock injected BALB/c mice (n = 11). Mice were observed for 50 days and evaluated for corneal graft rejection. Data reported as mean survival time for those grafts that were rejected for “tolerized” mice (B10 injected, 6 mice) or not tolerized (mock injected, 6 mice). These curves did not demonstrate statistical significance (p >0.05).
Figure 1. BALB/c mice were injected into the anterior chamber with 106 spleen cells from C57BL/10 (B10) mice. Full thickness B10 corneal grafts were then placed on BALB/c mice injected with B10 (n = 10) or mock injected BALB/c mice (n = 11). Mice were observed for 50 days and evaluated for corneal graft rejection. Data reported as mean survival time for those grafts that were rejected for “tolerized” mice (B10 injected, 6 mice) or not tolerized (mock injected, 6 mice). These curves did not demonstrate statistical significance (p >0.05).
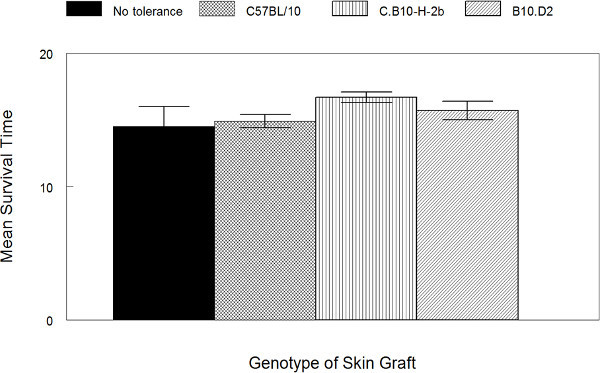 Figure 2. Injection of spleen cells into the anterior chamber does not impact survival of allogeneic skin grafts. BALB/c mice were injected into the anterior chamber with 106 spleen cells from C57BL/10 mice. After one week these mice were separately engrafted with skin from C57BL/10, n = 10, B10.D2, n = 7, C.B10-H-2b, n = 7 mice and compared to mice that were not injected and engrafted with C57BL/10 skin, n = 10. Results are expressed as the mean survival time + SEM.
Figure 2. Injection of spleen cells into the anterior chamber does not impact survival of allogeneic skin grafts. BALB/c mice were injected into the anterior chamber with 106 spleen cells from C57BL/10 mice. After one week these mice were separately engrafted with skin from C57BL/10, n = 10, B10.D2, n = 7, C.B10-H-2b, n = 7 mice and compared to mice that were not injected and engrafted with C57BL/10 skin, n = 10. Results are expressed as the mean survival time + SEM.
Discussion
The murine model of corneal transplantation described here enables the investigator to study human corneal allograft rejection in a model that is predictive of what factors are best associated with both rejection15,17,18,20, 26-30 and acceptance21-25 of corneal allografts. Unlike human corneal transplantation, in which patients are given either topical or systemic steroid treatment to either treat or prevent rejection31, this model is typically used to determine those factors that are relevant to allograft rejection in the absence of such therapy. In addition to a model for acute corneal allograft rejection, which typically occurs within 30 to 40 days of transplantation, we also present a late-term model of such rejection that occurs 45 days post-engraftment in mice and mimics many of the features of late-term and chronic rejection32,33 which thus far have not been modeled in animals.
The model’s strengths are that one can dissect various mechanisms that are responsible for the relatively high rate of corneal allograft acceptance as well as determining which mechanisms are most responsible for corneal allograft failure. This model also allows one to test various therapeutic strategies in an animal which possesses an immune system that is very similar to the human immune system. To that end, the existence of many reagents that react with murine factors as well as transgenic and gene-targeted mice, allow for the evaluation of so many more factors than would be the case with other species. This ability to evaluate so many different factors which are important to both success and failure of corneal allografts is a significant positive in favor of using this murine model versus other animal models in which surgery is easier to perform due to the increased size of the eyes of these species.
While there are several weaknesses of this model, we believe the strengths far outweigh them. One of the most significant, which was alluded to above, is the technical expertise involved in performing corneal transplantation in mice. Due to the small size of the murine eye, this requires someone who is adept at microsurgery, both in performing the transplantation as well as removal of sutures. Consequently, repeated practice is required to master and maintain proficiency at this technique. The second weakness is that while mice are very similar to humans, they are not the same. These animals display a greater tendency towards neovascularization, than do human corneas. Furthermore, this model will not mimic the surgical procedures meant to treat endothelial cell dysfunction like Fuch’s dystrophy2. Prior to recent year’s full thickness transplants like the ones used in the described protocol were employed. Presently, endothelial transplants involving only the endothelial portion of the cornea have been employed34,35. Such transplants have not been modeled thus far in mice due to the difficulty of performing this surgery in such small animals.
For late-term rejection (>45 days) two factors unique to this version of the model stand out. The first weakness with this form of the model being that mice must be maintained for a minimum of two to three months in order to study late-term rejection. And secondly, the corneas must first survive potential acute rejection reactions. Such acute rejections occur in 50 to 70% of recipients17,20-24. Thus to study late-term rejection one will engraft mice whose transplants will be rejected acutely and will not survive until 45 days post-engraftment. In order to mitigate this we have found that the rejection rate in male mice is less than that observed for female mice (manuscript in preparation) and thus to study late term rejection it is advised that only male mice be used. We also attempted to prolong corneal allograft survival with steroid treatment, but this did not prove to be particularly useful (personal observations) and thus do not recommend that steroid treatment be used. In spite of these complications and the caveat that likely approximately half or somewhat more of those engrafted with allogeneic corneas will remain clear until after 45 days, this is still a very useful model to study those factors that are relevant to late-term rejection.
Disclosures
The authors have no competing financial interests.
Acknowledgments
The authors would like to thank the many individuals who have worked on and perfected this technique and have been responsible for the generation of many manuscripts both in this lab and others. This work was supported by National Institutes of Health Grant EY12707 (PMS) and an unrestricted grant from Research to Prevent Blindness to Department of Ophthalmology.
References
- Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv. Ophthalmol. 2012:448–462. doi: 10.1016/j.survophthal.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gipson IK. Age-related changes and diseases of the ocular surface and. Invest. Opthlamol. Vis. Sci. 2013;54:48–53. doi: 10.1167/iovs.13-12840. [DOI] [PubMed] [Google Scholar]
- Edwards M, et al. Indications for corneal transplantation in New Zealand: 1991-1999. Cornea. 2002;21:152–155. doi: 10.1097/00003226-200203000-00004. [DOI] [PubMed] [Google Scholar]
- Thompson RW, Price MO, Bowers PJ, Price FW. Long-term survival after penetrating keratoplasty. Ophthalmol. 2003;110:1396–1402. doi: 10.1016/S0161-6420(03)00463-9. [DOI] [PubMed] [Google Scholar]
- Williams KA, Roder D, Esterman A, Muehlberg SM, Coster DJ. Factors predictive of corneal graft survival. Report form the Australian Corneal Graft Registry. Ophthalmology. 1992;99:403–414. doi: 10.1016/s0161-6420(92)31960-8. [DOI] [PubMed] [Google Scholar]
- Larkin DF. Corneal allograft rejection. Br. J. Ophthalmol. 1994;78:649–652. doi: 10.1136/bjo.78.8.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisjoly HM, et al. Risk factors of corneal graft failure. Ophthalmol. 1993;100:1728–1735. doi: 10.1016/s0161-6420(93)31409-0. [DOI] [PubMed] [Google Scholar]
- Sugar A, et al. Recipient Risk Factors for Graft Failure in the Cornea Donor Study. Ophthalmol. 2009;116:1023–1028. doi: 10.1016/j.ophtha.2008.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namba K, Kitaichi N, Nishida T, Taylor AW. Induction of regulatory T cells by the immunomodulating cytokines alpha-melanocyte-stimulating hormone and transforming growth factor-beta2. J. Leukoc. Biol. 2002;72:946–952. [PubMed] [Google Scholar]
- Taylor AW, Yee DG, Streilein JW. Suppression of nitric oxide generated by inflammatory macrophages by calcitonin gene-related peptide in aqueous humor. Invest. Ophthalmol. Vis. Sci. 1998;39:1372–1378. [PubMed] [Google Scholar]
- Wilbanks GA, Mammolenti M, Streilein JW. Studies on the induction of anterior chamber-associated immune deviation (ACAID). III. Induction of ACAID depends upon intraocular transforming growth factor-beta. Eur. J. Immunol. 1992;22:165–173. doi: 10.1002/eji.1830220125. [DOI] [PubMed] [Google Scholar]
- Volpert OV, et al. Inducer-stimulated Fas targets activated endothelium for destruction by anti-angiogenic thrombospondin-1 and pigment epithelium-derived factor. Nat. Med. 2002. pp. 8–349. [DOI] [PubMed]
- Apte RS, Sinha D, Mayhew E, Wistow GJ, Niederkorn JY. Cutting edge: role of macrophage migration inhibitory factor in inhibiting NK cell activity and preserving immune privilege. J. Immunol. 1998;160:5693–5696. [PubMed] [Google Scholar]
- Kennedy MC, et al. Novel production of interleukin-1 receptor antagonist peptides in normal human cornea. J. Clin. Invest. 1995;95:82–88. doi: 10.1172/JCI117679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimmura-Tomita M, Wang M, Taniguchi H, Akiba H, Yagita H, Hori J. Galectin-9-mediated protection from allo-specific T cells as a mechanism of immune privilege of corneal allografts. PLoS One. 2013;8 doi: 10.1371/journal.pone.0063620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg MF, Ferguson TA, Pepose JS. Detection of cellular adhesion molecules in inflamed human corneas. Ophthalmol. 1994;101:161–168. doi: 10.1016/s0161-6420(94)31370-4. [DOI] [PubMed] [Google Scholar]
- Stuart PM, Griffith TS, Usui N, Pepose JS, Yu X, Ferguson TA. CD95 ligand (FasL)-induced apoptosis is necessary for corneal allograft survival. J Clin Invest. 1997;99:396–402. doi: 10.1172/JCI119173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamagami S, et al. Role of Fas-Fas ligand interactions in the immunorejection of allogeneic mouse corneal transplants. Transplantation. 1997;64:1107–1111. doi: 10.1097/00007890-199710270-00004. [DOI] [PubMed] [Google Scholar]
- Stuart PM, Pan F, Plambeck S, Ferguson TA. Fas/Fas ligand interactions regulate neovascularization in the cornea. Invest. Ophthalmmol. Vis. Sci. 2003;44:93–98. doi: 10.1167/iovs.02-0299. [DOI] [PubMed] [Google Scholar]
- Stuart PM, Yin XT, Pan F, Haskova Z, Plambeck S, Ferguson TA. Inhibitors of matrix metalloproteinases activity prolong corneal allograft acceptance by increasing FasL expression. Invest. Ophthalmol. Vis. Sci. 2004;45:1169–1173. doi: 10.1167/iovs.03-0932. [DOI] [PubMed] [Google Scholar]
- Joo C-K, Pepose JS, Stuart PM. T-cell mediated responses in a murine model of orthotopic corneal transplantation. Invest.Ophthalmol. Vis. Sci. 1995;36:1530–1540. [PubMed] [Google Scholar]
- Sonoda Y, Sano Y, Ksander B, Streilein JW. Characterization of cell-mediated immune responses elicited by orthotopic corneal allografts in mice. Invest. Ophthalmol. Vis. Sci. 1995;36:427–434. [PubMed] [Google Scholar]
- Sano Y, Osawa H, Sotozono C, Kinoshita S. Cytokine expression during orthotopiccorneal allograft rejection in mice. Invest. Ophthalmol. Vis. Sci. 1998;39:1953–1957. [PubMed] [Google Scholar]
- Haskova Z, Usui N, Ferguson TA, Pepose JS, Stuart PM. CD4+ T cells are critical in corneal but not skin allograft rejection. Transplantation. 2000;69:483–488. doi: 10.1097/00007890-200002270-00004. [DOI] [PubMed] [Google Scholar]
- Tan Y, et al. Immunological disruption of antiangiogenic signals by recruited allospecific T cells leads to corneal allograft rejection. J. Immunol. 2012;188:5962–5969. doi: 10.4049/jimmunol.1103216. [DOI] [PubMed] [Google Scholar]
- Dana MR, Yamada J, Streilein JW. Topical interleukin-1 receptor antagonist promotes corneal transplant survival. Transplantation. 1997;63:1501–1507. doi: 10.1097/00007890-199705270-00022. [DOI] [PubMed] [Google Scholar]
- Cunnusamy K, Chen PW, Niederkorn JY. IL-17A-dependent CD4+CD25+ regulatory T cells promote immune privilege of corneal allografts. J. Immunol. 2011;186:6737–6745. doi: 10.4049/jimmunol.1100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu H, et al. Arginine depletion as a mechanism for the immune privilege of corneal allografts. Eur. J. Immunol. 2011;41:2997–3005. doi: 10.1002/eji.201141683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina CA, Rowe AM, Yun H, Knickelbein JE, Lathrop KL, Hendricks RL. Azithromycin treatment increases survival of high-risk corneal allotransplants.Cornea. 2013. pp. 32–658. [DOI] [PMC free article] [PubMed]
- Cho YK, Zhang X, Uehara H, Young JR, Archer B, Ambati B. Vascular Endothelial Growth Factor Receptor 1 morpholino increases graft survival in a murine penetrating keratoplasty. Invest. Ophthalmol. Vis. Sci. 2012;53:8458–8471. doi: 10.1167/iovs.12-10408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HK, Choi JA, Uehara H, Zhang X, Ambati BK, Cho YK. Presurgical corticosteroid treatment improves corneal transplant survival in mice. Cornea. 2013;32:1591–1598. doi: 10.1097/ICO.0b013e31829ebb0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamazoe K, Yamazoe K, Shimazaki-Den S, Shimazaki J. Prognostic factors for corneal graft recovery after severe corneal graft rejection following penetrating keratoplasty. BMC Ophthalmol. 2013;13:5. doi: 10.1186/1471-2415-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda A, Vanathi M, Kumar A, Dash Y, Priya S. Corneal graft rejection. Surv. Ophthalmol. 2007;52:375–396. doi: 10.1016/j.survophthal.2007.04.008. [DOI] [PubMed] [Google Scholar]
- Patel SV. Graft survival and endothelial outcomes in the new era of endothelial keratoplasty. Exp. Eye Res. 2012;95:40–47. doi: 10.1016/j.exer.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anshu A, Price MO, Tan DT, Price FW., Jr Endothelial keratoplasty: a revolution in evolution. Surv. Ophthalmol. 2013;57:236–252. doi: 10.1016/j.survophthal.2011.10.005. [DOI] [PubMed] [Google Scholar]


