Abstract
The blood-brain-barrier is ultrastructurally assembled by a monolayer of brain microvascular endothelial cells (BMEC) interconnected by a junctional complex of tight and adherens junctions. Together with other cell-types such as astrocytes or pericytes, they form the neurovascular unit (NVU), which specifically regulates the interchange of fluids, molecules and cells between the peripheral blood and the CNS. Through this complex and dynamic system BMECs are involved in various processes maintaining the homeostasis of the CNS. A dysfunction of the BBB is observed as an essential step in the pathogenesis of many severe CNS diseases. However, specific and targeted therapies are very limited, as the underlying mechanisms are still far from being understood.
Animal and in vitro models have been extensively used to gain in-depth understanding of complex physiological and pathophysiological processes. By reduction and simplification it is possible to focus the investigation on the subject of interest and to exclude a variety of confounding factors. However, comparability and transferability are also reduced in model systems, which have to be taken into account for evaluation. The most common animal models are based on mice, among other reasons, mainly due to the constantly increasing possibilities of methodology. In vitro studies of isolated murine BMECs might enable an in-depth analysis of their properties and of the blood-brain-barrier under physiological and pathophysiological conditions. Further insights into the complex mechanisms at the BBB potentially provide the basis for new therapeutic strategies.
This protocol describes a method to isolate primary murine microvascular endothelial cells by a sequence of physical and chemical purification steps. Special considerations for purity and cultivation of MBMECs as well as quality control, potential applications and limitations are discussed.
Keywords: Neuroscience, Issue 93, Blood brain barrier, central nervous system, endothelial cells, immune cell trafficking, neuroinflammation, neurodegeneration, neurovascular unit
Introduction
Brain microvascular endothelial cells (BMEC) form monolayers that are an integral part of the highly specialized blood-brain-barrier (BBB). BMECs are interconnected by junctional proteins attached to a basement membrane. Together with pericytes, smooth muscle cells, astrocytic end feet and circulating blood cells they build up the so-called neurovascular unit (NVU)1. Against the previous notion of an impermeable barrier between blood and the central-nervous-system (CNS), the NVU is a dynamic, highly specific and regulated interface that controls the transition of fluids, molecules and cells between cerebral blood vessels and the CNS2. A dysfunction or dysregulation of the NVU may initiate and/or contribute to a variety of neurovascular, infectious, inflammatory or degenerative diseases of the CNS, such as ischemic stroke, HIV-encephalopathy, multiple sclerosis, Alzheimer’s or Parkinson’s disease3-6.
The BMEC monolayer is tightly sealed by a junctional complex constituted of tight (TJ) and adherens junctions (AJ)7. The high electrical resistance and the low paracellular permeability of the BBB are mainly based on TJ proteins8. The TJs are complexes formed by the transmembrane proteins of the claudin and occludin family, which are linked to the cytoskeleton of the endothelial cells by adapter molecules, such as the zonulaoccludens (ZO) proteins ZO1-34. Adherens junctions are mainly assembled by the integral membrane protein vascular endothelial (VE)-cadherin, which is linked to the cytoskeleton via catenins8.
The tight sealing of the BBB prevents the free exchange of substrates and cells between blood and CSF. Exceptions to this rule are lipophilic, small molecules with a molecular weight <400 Da, which are able to cross the BBB by lipid-mediated diffusion9. The passage of larger and/or hydrophilic molecules, such as glucose, amino acids, peptides, proteins and many drugs is restricted to highly controlled transcellular transport systems10, which can be classified into five main categories: carrier-mediated transport, ion transport, active efflux transport, receptor-mediated transport, and caveolae-mediated transport4. These transporter systems help maintaining the homeostasis of the CNS, which is required for an accurate signal generation, transduction and integration. Moreover, BMECs are able to actively control the transition of distinct molecules by the expression of a variety of ectoenzymes. These enzymes are localized on the cell surface and modify specific endogenous and exogenous substrates hindering or allowing the transition of the BBB11.
Whereas the CNS was considered as an immune-privileged organ for a long-time, recent findings suggest a rather dynamic and tightly regulated system of immune surveillance of the CNS. The BMECs are critically involved in the regulation of immune cell transmigration. By the expression of selectins on their surface lymphocytes are selectively induced to loosely attach to the endothelium. The secretion of chemokines that encounter with specific receptors on leukocytes leads to the expression or conformational changes of leukocyte integrins, such as LFA-1 (lymphocyte function associated antigen-1) and VLA-4 (very late antigen-4). The integrins mediate a firm adhesion by binding their endothelial counterreceptors, e.g. VCAM-I (vascular cell adhesion molecule), ICAM-I (intercellular adhesion molecule) enabling the transmigration into the brain parenchyma between or through BMECs of the BBB12-14. These and other findings underline the active role of the endothelium itself in regulating immune cell migration.
Furthermore, BMECs as part of the NVU are involved in the regulation of the cerebral blood flow linked to local neuronal metabolic demands. Upon astrocytic stimulation endothelial cells produce vasoactive substances such as nitric oxide leading to relaxation of vascular smooth muscle cells15.
Angiogenesis and neurogenesis in the developing as well as in the adult brain show parallel patterning and development and share many properties of regulation1,4. Endothelial cells are critically involved in these processes16,17.
In summary, BMECs provide essential features to warrant a proper development and functioning of the CNS. BBB dysfunction is linked to many severe neurologic disorders. However, only very few targets have been identified at the brain-vasculature interface for a specific and efficient treatment18. Simplified in vitro models have been used to understand the mechanisms involved in function and regulation of complex physiologic systems for a long time. The isolation as described by this manuscript and the in vitro study of murine BMECs, given the wide variety of specific mouse knockout-strains, might provide a further understanding of BBB function and regulation under physiological and pathophysiological conditions opening up new therapeutic avenues.
Protocol
All animal experiments were approved by the local authorities (“LandesamtfürNatur, Umwelt und Verbraucherschutz NRW; Fachbereich 87, Tiergesundheit, Tierschutz; Recklinghausen, Germany”) and conducted according to the German law of animal protection.
1. General Comments for Mouse Experiments
Perform all experiments using mice in accordance with the guidelines of the respective Institutional Animal Care and Use Committee.
Keep the mice under pathogen-free conditions and enable them to have access to food and water ad libitum.
Use age- and sex-matched mice in experimental groups because biological properties can vary with age and gender.
Whenever possible try to reduce, refine or replace animal experiments.
2. Preparation of the Percoll Gradient
Mix 19 ml of 1x PBS with 1 ml 10x PBS, 1 ml FCS and 10 ml Percoll.
Perform sterile filtration in a glass tube (diameter of filter pores: 0.2 µm). Afterwards store the solution at 4 °C.
3. Preparation of Endothelium Cell Medium and Coating of Cell Culture Plates
- Endothelial cell medium:
- Preparation of 500 ml medium: Mix 400 ml DMEM medium (approx. 80%) with 100 ml PDS (approx. 20%), 0.25 ml bFgF (20 µg/ml; approx. 0.05%), 0.5 ml heparin (100 µl/ml; approx. 0.1%) and 0.5 ml pyrumycin (4 mg/ml; approx. 0.1%). Add pyrumycin only for cell culture medium used in the first 2 days of culture.
- Perform sterile filtration in a glass tube (diameter of filter pores: 0.2 µm). Afterwards store the solution at 4 °C.
- Coating of cell culture plates:
- For 1 ml of coating solution, prepare a solution of 500 µl ddH2O, 400 µl collagen IV (0.4 mg/ml) and 100 µl fibronectin (0.1 mg/ml).
- Cover the whole surface of each well of the cell culture plate with the coating solution. Store the plate at 4 °C overnight.
4. Isolation of Murine Brain Microvascular endothelial cells (MBMEC)
Sacrifice 10 adult mice (8 - 12 weeks old, C57BL/6) by cervical dislocation. Afterwards isolate the mouse-brains and store in 5 ml of PBS (Caveat: Work sterile!).
Remove brain stems, cerebella and thalami with a forceps. Detach meninges by carefully rolling the brains on a sterile blotting paper. Collect the resulting meninges-free forebrains.
Transfer the brains to a 50 ml Falcon tube filled with 13.5 ml of DMEM.
Mince the tissue, first with a 25 ml pipette, then with a 10 ml pipette until the media becomes milky.
Then digest the tissue with a mixture of 0.6 ml collagenase CLS2 (10 mg/ml in DMEM) and 0.2 ml DNAse (1 mg/ml in PBS) in Dulbecco’s Modified Eagle Medium (DMEM) for 1 hr at 37 °C on an orbital shaker at 180 rpm.
Add 10 ml of DMEM added to the tissue suspension and centrifuge the cells at 1,000 x g for 10 min at 4 °C.
Discard supernatant (Caveat: PELLET IS EASY TO LOSE!)
To remove the myelin, resuspend the pellet with a 25 ml pipette in 25 ml of BSA-DMEM (20% w/v) (approx. 25 times), and centrifuge at 1,000 x g for 20 min at 4 °C.
Discard the upper myelin layer (milky) with a broken glass Pasteur pipette with larger diameter, and then discard the BSA layer with a normal Pasteur pipette.
Resuspend the pellet in 9 ml DMEM and add 1 ml collagenase/dispase (final concentration is 1 mg/ml) and 0.1 ml DNAse. Digest the solution for 1 hr at 37 °C on an orbital shaker at 180 rpm (caveat: do not use the pipette to resuspend – cells can be lost).
During the digestion, centrifuge the Percoll solution to set up the density gradient using an ultracentrifuge at 3,000 x g for 1 hr at 4 °C, with acceleration, without brake.
Add 10 ml of DMEM to the digested cell suspension. Centrifuge the suspension at 1,000 x g for 10 min at 4 °C. Then discard the supernatant and resuspend the pellet in 2 ml of DMEM.
Add the resuspended cells carefully on top of the Percoll gradient and centrifuge at 700 x g for 10 min at 4 °C without acceleration and brake. Note: The cells are visible as a cloud in the interphase.
Take approx. 12 ml of the interphase with cells with a long sterile needle and place it in a new 50 ml Falcon with 5 ml of DMEM.
Centrifuge the cells again at 1,000 x g for 10 min at 4 °C. Afterwards resuspend the pellet in endothelial cell medium (use approx. 0.2 ml of medium per 1 cm2 surface of cell culture plate).
Remove coating solution from coated cell culture plates (see step 3.2) and rinse every well with sterile PBS in two consecutive washing steps.
Maintain cell cultures in endothelial cell medium at 37 °C and 5% CO2 in a sterile incubator. Change the medium every two to three days. Split cells at 90% confluence.
Representative Results
Immediately after isolation, murine BMECs and contaminating cells form conglomerates floating in the cell culture medium (Figure 1A, day 0). The treatment with pyrumycin leads to a selection of murine BMECs since they express high levels of efflux transporters such as P-glycoprotein leading to a relative resistance to toxins. Contaminating cells are much more susceptible to pyrumycin mediated cytotoxicity19. During the process of pyrumicin selection, contaminating cells enter apoptotic or necrotic cell death, whereas MBMECs begin to attach to the collagen IV/fibronectin coated cell culture plates (Figure 1A, day 1 and day 2). Until day 5, the MBMECs proliferate to a density of approx. 80 - 90%. They are characterized by the typical spindle-shaped appearance. At confluence, they form a monolayer of tightly packed, longitudinally aligned and non-overlapping contact-inhibited cells (Figure 1A, day 5). By pyrumicin selection, a high purity of up to 99% MBMEC is reached as demonstrated by the endothelial cell marker CD31 (PECAM1; Figure 1B). The MBMECs form tightly sealed monolayers interconnected by tight junction proteins. After 7 - 8 days of culture, the endothelial cell layers build up stable values for electrical resistance (reaching typical values between 20 - 30 Ω x cm2) and capacitance (Figure 1C). At this time-point functional assays such as cell-migration experiments3,20,21 and permeability tests, e.g. with Evans blue or Dextran, should be performed.
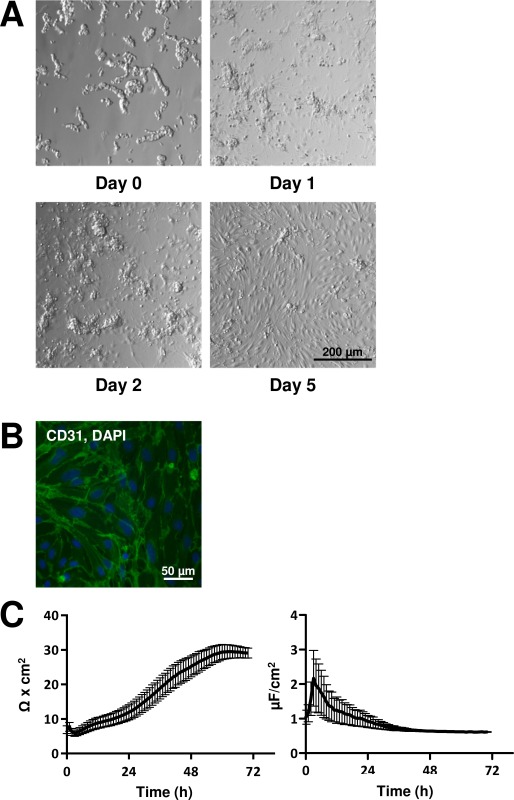 Figure 1. Morphological and Functional Properties of Murine BMECs. (A) Representative time course of cultured BMECs viewed by transmission light microscopy over 5 days. Scale bar applies for all images. (B) Immunofluorescence staining for the endothelial cell marker CD31 at day 5. CD31 (green) and DAPI (blue). (C) Cells were precultured for 5 days and then transferred to an automated system for the analysis of biophysical properties (resistance and capacitance). Please click here to view a larger version of this figure.
Figure 1. Morphological and Functional Properties of Murine BMECs. (A) Representative time course of cultured BMECs viewed by transmission light microscopy over 5 days. Scale bar applies for all images. (B) Immunofluorescence staining for the endothelial cell marker CD31 at day 5. CD31 (green) and DAPI (blue). (C) Cells were precultured for 5 days and then transferred to an automated system for the analysis of biophysical properties (resistance and capacitance). Please click here to view a larger version of this figure.
Discussion
Blood-brain-barrier dysfunction is a hallmark of various deleterious CNS diseases, e.g. a breakdown of the BBB in multiple sclerosis extensively facilitates the CNS invasion by autoreactive immune cells and enables the encounter and destruction of oligodendrocytes. In ischemic stroke the disruption of the BBB and the subsequent formation of brain edema are critical factors that influence secondary infarct growth and the overall survival of patients6. Furthermore, by alterations of the BBB in remote areas focal ischemic lesions are able to induce widespread functional alterations of the brain. However, the underlying molecular mechanisms are largely unknown5. In contrast, the high density and diversity of efflux transporters in functional BMECs reduces the concentration of beneficial drugs such as chemotherapeutics for brain malignancies or antibiotics for infectious diseases. Therefore, a deeper understanding of the blood-brain-barrier function under physiological and pathophysiological conditions is required to develop pharmacological agents that are able to specifically regulate the barrier function in the favored direction21. Reliable in vitro models of the BBB are indispensable tools to study the regulatory mechanisms at the BBB.
Many immortalized brain endothelial cell lines have been established and employed as in vitro BBB models22. These cell lines offer certain advantages over primary BMECs as they grow faster and keep certain BBB characteristics over several passages. However, endothelial cell lines cannot fully substitute for primary cells as important properties are changed that intermingle with the transferability of experimental findings to the in vivo situation. For instance, the murine brain endothelial cell line bEnd.5 expresses only low levels of discontinuously distributed tight junction proteins leading to high paracellular permeability23. BEnd.3, another frequently used murine brain endothelial cell line, demonstrates dense and continuous distributed tight junctions, a high transendothelial resistance, several efflux transporters and low paracellular permeability. However, bEND.3 cell layers compared to primary BMECs lack a real discrimination with respect to the permeation of certain transcellular and paracellular substrates24.
In preparations of primary cell cultures, contaminating cells can significantly interfere with the validity of experimental findings. In the described protocol, pyrumicin is used as a selective agent for endothelial cells to achieve high purity. Nevertheless, a regular quality control of the cell culture is inevitably needed to guarantee for reliable experiments. There are several methods for quality control, besides typical morphological properties of endothelial cells (see Figure 1A), the transendothelial resistance might be measured or the expression of endothelial cell marker such as CD31 (see Figure 1B) or von Willebrand factor (vWF) might be evaluated.
The number of brain endothelial cells isolated from one mouse brain is relatively low and to set up a proper cell culture for multiple experiments, the brains of several mice have to be pooled. In our experience, at least 10 mice need to be used for one experiment which might be a limiting factor depending on the resources of the respective animal facility. In order to avoid bias or confounding factors, only mice with an identical genetic and environmental background should be pooled. In contrast, bovine and porcine brain endothelial cell preparations provide a large number of brain endothelial cells available in one brain. However, besides the uncomplicated breeding and housing, the broad and ever increasing repertoire of available transgenic mice renders primary murine BMECs as an ideal model to study blood-brain-barrier function.
Several key findings concerning the functions of the BBB and the underlying molecular mechanisms have come from studies in 2D tissue culture systems. Recently, 3D culture systems have been developed25, where endothelial cells are placed within a collagen matrix enabling them to form lumen and tubular networks. These new cell culture systems allow for an even more accurate reproduction of vascular processes in the intact organism in vivo. The involvement of further cells of the NVU in 3D cell culture systems, such as pericytes and astrocytes might revolutionize the in vitro studying of blood-brain-barrier function; first models have recently been developed26.
There are some recommendations for troubleshooting. First of all sterile working is essential for the quality of the endothelial cell culture. Second, pyrumycin should only be added for cell culture medium used in the first 2 days of culture, longer application might lead to increased MBMEC cell death and low quality barrier function. Third, the enzymes applied in this protocol should be used and stored according to the manufacturer’s instructions; otherwise their proper function might be compromised. Furthermore, the coating of cell culture plates might be amended if endothelial cells do not attach. Concentrations of fibronectin and collagen might be changed or other matrix proteins might be added to the coating solution. Lastly, age, gender, season of the year and environmental conditions within the animal facility are important factors that might influence the quality of MBMEC isolation and comparability of experiments. It should be ensured that conditions are comparable between independent experiments.
The described protocol should be considered as a basic neuroimmunological method to isolate murine BMECs. The isolated cells might be used for a wide variety of applications to gain further insight into BBB function, such as migration assays, gene and protein expression studies, electrophysiological evaluations or permeability experiments. As mentioned above, 3D cell culture systems of BMECs might provide new opportunities to study the complex mechanisms involved in the regulation of the BBB in the context of the NVU. Therefore, the isolation of primary endothelial cells will remain an invaluable technique in the field of BBB research in the future.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
This work was supported by the Interdisciplinary Center for Clinical Research (IZKF) Münster (SEED 03/12, SB), by the Deutsche Forschungsgemeinschaft (DFG), Cells-in-Motion Cluster of Excellence (EXC 1003 – CiM), University of Muenster (to SB and SGM) and by the Else Kröner-Fresenius-Stiftung (2012_A88 to SB and SGM). We thank Heike Blum for the excellent illustrations.
References
- Neuwelt EA, et al. Engaging neuroscience to advance translational research in brain barrier biology. Nature reviews. Neuroscience. 2011;12:169–182. doi: 10.1038/nrn2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuki S, Terasaki T. Contribution of carrier-mediated transport systems to the blood-brain barrier as a supporting and protecting interface for the brain; importance for CNS drug discovery and development. Pharmaceutical Research. 2007;24:1745–1758. doi: 10.1007/s11095-007-9374-5. [DOI] [PubMed] [Google Scholar]
- Bittner S, et al. Endothelial TWIK-related potassium channel-1 (TREK1) regulates immune-cell trafficking into the CNS. Nature Medicine. 2013;19:1161–1165. doi: 10.1038/nm.3303. [DOI] [PubMed] [Google Scholar]
- Zlokovic BV. The blood-brain barrier in health and chronic neurodegenerative disorders.Neuron. 2008;57:178–201. doi: 10.1016/j.neuron.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Stoll G, et al. Transient widespread blood-brain barrier alterations after cerebral photothrombosis as revealed by gadofluorine M-enhanced magnetic resonance imaging. Journal of Cerebral Blood Flow & Metabolism. 2009;29:331–341. doi: 10.1038/jcbfm.2008.129. [DOI] [PubMed] [Google Scholar]
- Kleinschnitz C, et al. Glucocorticoid insensitivity at the hypoxic blood-brain barrier can be reversed by inhibition of the proteasome. Stroke. 2011;42:1081–1089. doi: 10.1161/STROKEAHA.110.592238. [DOI] [PubMed] [Google Scholar]
- Hawkins BT, Davis TP. The blood-brain barrier/neurovascular unit in health and disease. Pharmacological reviews. 2005;57:173–185. doi: 10.1124/pr.57.2.4. [DOI] [PubMed] [Google Scholar]
- Bazzoni G, Dejana E. Endothelial cell-to-cell junctions: molecular organization and role in vascular homeostasis. Physiological reviews. 2004;84:869–901. doi: 10.1152/physrev.00035.2003. [DOI] [PubMed] [Google Scholar]
- Pardridge WM. Blood-brain barrier delivery. Drug Discovery Today. 2007;12:54–61. doi: 10.1016/j.drudis.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Persidsky Y, Ramirez SH, Haorah J, Kanmogne GD. Blood-brain barrier: structural components and function under physiologic and pathologic conditions. Journal of neuroimmunepharmacology : the official journal of the Society on NeuroImmune Pharmacology. 2006;1:223–236. doi: 10.1007/s11481-006-9025-3. [DOI] [PubMed] [Google Scholar]
- Pardridge WM. Molecular biology of the blood-brain barrier. Molecular Biotechnology. 2005;30:57–70. doi: 10.1385/MB:30:1:057. [DOI] [PubMed] [Google Scholar]
- Ley K, Laudanna C, Cybulsky MI, Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nature Reviews Immunology. 2007;7:678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- Wilson EH, Weninger W, Hunter CA. Trafficking of immune cells in the central nervous system. Journal of Clinical Investigation. 2010;120:1368–1379. doi: 10.1172/JCI41911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt B, Capture Ransohoff RM. crawl, cross: the T cell code to breach the blood-brain barriers. Trends in Immunology. 2012;33:579–589. doi: 10.1016/j.it.2012.07.004. [DOI] [PubMed] [Google Scholar]
- Zonta M, et al. Neuron-to-astrocyte signaling is central to the dynamic control of brain microcirculation. Nature Neuroscience. 20003;6:43–50. doi: 10.1038/nn980. [DOI] [PubMed] [Google Scholar]
- Daneman R, Zhou L, Kebede AA, Barres BA. Pericytes are required for blood-brain barrier integrity during embryogenesis. Nature. 2010;468:562–566. doi: 10.1038/nature09513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt H, et al. VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. Journal of Cell Biology. 2003;161:1163–1177. doi: 10.1083/jcb.200302047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt B, Sorokin L. The blood-brain and the blood-cerebrospinal fluid barriers: function and dysfunction. Seminars in immunopathology. 2009;31:497–511. doi: 10.1007/s00281-009-0177-0. [DOI] [PubMed] [Google Scholar]
- Perriere N, et al. Puromycin-based purification of rat brain capillary endothelial cell cultures. Effect on the expression of blood-brain barrier-specific properties. J. Neurochem. 2005;93:279–289. doi: 10.1111/j.1471-4159.2004.03020.x. [DOI] [PubMed] [Google Scholar]
- Ruck T, et al. CD4+NKG2D+ T cells exhibit enhanced migratory and encephalitogenic properties in neuroinflammation. PLoS One. 2013;8:81455. doi: 10.1371/journal.pone.0081455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weidenfeller C, Schrot S, Zozulya A, Galla HJ. Murine brain capillary endothelial cells exhibit improved barrier properties under the influence of hydrocortisone. Brain Res. 2005;1053:162–174. doi: 10.1016/j.brainres.2005.06.049. [DOI] [PubMed] [Google Scholar]
- Gumbleton M, Audus KL. Progress and limitations in the use of in vitro cell cultures to serve as a permeability screen for the blood-brain barrier. J. Pharmaceutal Sci. 2001;90:1681–1698. doi: 10.1002/jps.1119. [DOI] [PubMed] [Google Scholar]
- Watanabe T, et al. Paracellular barrier and tight junction protein expression in the immortalized brain endothelial cell lines bEND.3, bEND.5 and mouse brain endothelial cell 4. Biological & Pharmaceutical Bulletin. 2013;36:492–495. doi: 10.1248/bpb.b12-00915. [DOI] [PubMed] [Google Scholar]
- Omidi Y, et al. Evaluation of the immortalised mouse brain capillary endothelial cell line, b.End3, as an in vitro blood-brain barrier model for drug uptake and transport studies. Brain Research. 2003;990:95–112. doi: 10.1016/s0006-8993(03)03443-7. [DOI] [PubMed] [Google Scholar]
- Sacharidou A, et al. Endothelial lumen signaling complexes control 3D matrix-specific tubulogenesis through interdependent Cdc42- and MT1-MMP-mediated events. Blood. 2010;115:5259–5269. doi: 10.1182/blood-2009-11-252692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urich E, et al. Multicellular self-assembled spheroidal model of the blood brain barrier. Scientific reports. 2013;3 doi: 10.1038/srep01500. [DOI] [PMC free article] [PubMed] [Google Scholar]


