Abstract
Sepsis remains a leading cause of mortality among neonates, especially in developing countries. Most cases of neonatal sepsis are attributed to Escherichia coli and other members of the Enterobacteriaceae family. Shewanella algae (S. algae) is a gram-negative saprophytic bacillus, commonly associated with the marine environment, which has been isolated from humans. Early onset neonatal sepsis caused by S. algae is uncommon. We report a case of S. algae blood stream infection in a newborn with early onset neonatal sepsis.
Keywords: Neonatal sepsis, Shewanella algae, blood stream infection, blood culture
What this study adds:
-
What is known about this subject?
Shewanella algae is a marine bacteria and an uncommon cause of infection in humans. However, these infections are often associated with high mortality. Prematurity is a known risk factor.
-
What new information is offered in this study?
We report an uncommon case of early onset neonatal sepsis caused by S. algae in a newborn delivered by Caesarean section at 35 weeks of gestation. S. algae is a saprophytic bacterium and a novel pathogen for neonatal sepsis, particularly in an institutional setup, where exposure to contaminated water is unlikely.
-
What are the implications for research, policy, or practice?
This case highlights the importance of a clinical microbiology laboratory in identifying the correct aetiological agent for neonatal sepsis (S. algae in our case), thereby facilitating the use of an appropriate antibiotic, which resulted in a better clinical outcome.
Background
Neonatal sepsis, a blood stream infection occurring during the first month of life, is associated with increased morbidity and mortality.1 Early onset neonatal sepsis (EONS) develops within three days of birth. The organisms associated with it are derived from the mother during the intrapartum period; these are Group B streptococci, Escherichia coli, Streptococcus viridans, enterococci, Staphylococcus aureus, Pseudomonas aeruginosa, and other gram-negative bacilli.2,3 Shewanella spp., saprophytic nonfermenting gram-negative bacilli, are an uncommon cause of human disease associated with three characteristic patterns of human infection; i.e., soft tissue infection, bacteremia, and neonatal sepsis.4 Here, we describe a case of neonatal sepsis caused by Shewanella algae.
Case details
A 27-year-old multipara at 35 weeks of pregnancy presented with complaints of watery fluid per vaginum. On examination, premature rupture of membranes with leakage of amniotic fluid was identified. Emergency lower segment Caesarean section (LSCS) was done due to pregnancy-induced hypertension and a 2.5kg male baby was delivered. Apgar score was 8/10 at one minute and 9/10 at five minutes. The general condition of the baby was normal until the third day when the baby became lethargic, had weak cry, and refused feeds. On examination, the heart rate was 120 beats/minute, respiratory rate was 55/minute and temperature was 37.1°C. However, neonatal sepsis was suspected clinically despite the absence of other signs of sepsis, such as thermal instability (fever or hypothermia), poor peripheral circulation with cold extremities, bulging fontanelle, shallow respiration, distended abdomen, and no seizures.
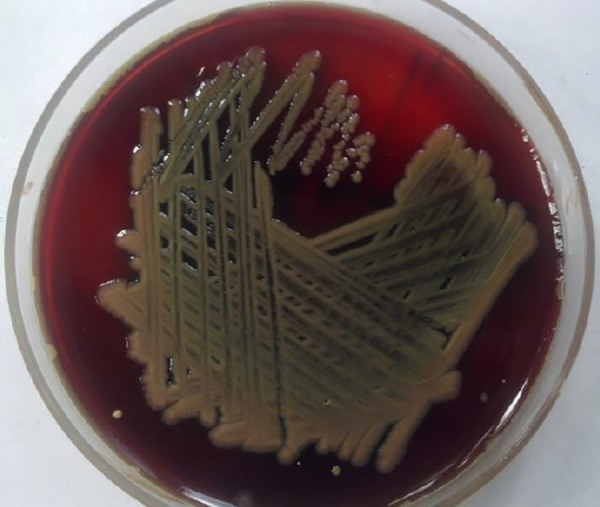
Sepsis screen showed raised CRP (2.4mg/dl), and a normal total white blood cell count of 6500/mm3. The differential leucocyte count (neutrophils 58 per cent, lymphocytes 38 per cent, monocytes 3 per cent, and eosinophils 1 per cent) was normal. The immature to total neutrophils ratio (I/T ratio) was 0.2. ampicillin (400mg/kg/d ÷ q 8-12 hr I.V.) and gentamicin (5mg/kg body weight) were started as empirical therapy based on these septic screen tests. Blood culture was done by automated Becton, Dickinson and Company BACTEC culture system, which gave a positive result after 24 hours. Gram-negative bacilli were isolated from this blood sample, which produced β-haemolytic colonies on blood agar medium with a tan pigment (Figure 1), and lactose non-fermenting colonies on MacConkey agar.
Figure 1: Showing β-haemolytic colonies on blood agar medium with tan pigment.
The isolate was identified as Shewanella sp. based on the following standard biochemical reactions: oxidase positive, indole negative, citrate-negative, urease positive, with Triple Sugar Iron agar showing an alkaline slant with black discolouration in the butt due to hydrogen sulphide (H2S). The glucose oxidation/fermentation test indicated it was oxidative. The isolate was identified as S. algae based on its growth characteristics and biochemical reactions, which distinguished it from S. putrefaciens. It showed growth on Salmonella-Shigella agar (SS agar), grew at 42βC and in the presence of 6.5 per cent NaCl (sodium chloride), produced haemolysis on sheep blood agar, and failed to use maltose and L-arabinose.
The isolate was subjected to susceptibility testing by the Kirby-Bauer disc diffusion method. It was resistant to ceftazidime, colistin, and polymyxin-B, and sensitive to ciprofloxacin, imipenem, amikacin, gentamicin, tobramycin, and netilmycin. Following the culture report, the empirical antibiotics administered were changed to gentamicin alone, and the neonate responded well to it. A repeat blood culture done on the sixth postnatal day was negative and CRP was within normal limits. The neonate was discharged on the eighth day. An attempt was made to identify the source by looking for Shewanella spp. in water sources in the postnatal ward. However, no Shewanella spp. could be isolated from the environment.
Discussion
The genus Shewanella is an oxidative, H2S producing gramnegative bacillus.5 The two biotypes, S. algae and S. putrifaciens are differentiated based on haemolytic property on blood agar, ability to ferment carbohydrates, growth at 42°C, ability to grow on Salmonella-Shigella agar and 6.5 per cent NaCl.5 Shewanella spp. are often isolated from natural habitats like water and soil. Human infection caused by this group of organisms is rare. Common infections caused by this organism include skin and soft tissue infection, and bacteremia, including neonatal sepsis. Commonly, infections caused by this organism are associated with exposure to environmental sources like water.6
Since traditional newborn care practices like bathing or prelacteal feeding are widespread in rural populations, adherence to the standard obstetric care and health education would be imperative in preventing these infections, especially in the case of non-institutional deliveries. In hospital setups, vigilant nursing care along with surveillance of hospital environment and facility for rapid laboratory diagnosis is likely to reduce the risk of Shewanella infections. In our patient, the source of infection remained undetected. Although the infection was acquired postnatally, water was unlikely to be source in this case, as the baby was not exposed to water for bathing or prelacteal feeding. Moreover, the environmental screening of water sources in the postnatal ward failed to grow Shewanella spp.
Shewanella bacteremia has been reported in infants, premature, and term neonates. Brink et al. studied Shewanella bacteremia in 24 patients, of which the majority were premature neonate (66 per cent, 16 out of 24).7 Pneumonia and respiratory distress were strongly associated with Shewanella bacteremia. However, in our case, the infant had no associated respiratory illness. In the case series by Brink et al., 75 per cent (18 out of 24) of cases were polymicrobial.7 In another study, 64 per cent of Shewanella infections were polymicrobial in nature.8 Sharma et al. reported a case series of infections by Shewanella spp. However, all the patients were adult and mainly presented with wound and soft tissue infections, which were chronic in nature.9
Although S. algae has been isolated from various human samples, EONS caused by this organism is uncommon. Around 13–28 per cent mortality has been reported with Shewanella infection.10,11 Shewanella isolates have been found to show high in vitro susceptibility to cephalosporins, gentamicin, and ciprofloxacin in various studies.11 This is in accordance with our findings. Since our isolate was a sensitive strain, early detection, and initiation of treatment with gentamicin led to a successful outcome.
Conclusion
S. algae is an unusual human pathogen. Blood stream infection by S. algae in neonate is uncommon. Unlike the adults, the source and mode of transmission may remain unidentified in neonatal infections. This case shows the relevance of laboratory findings in diagnosing the aetiology and guiding the correct antibiotic therapy for neonatal sepsis, which may help in improved clinical outcomes.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
PATIENT CONSENT
The authors, Charles MVP, Srirangaraj S, and Kali A declare that:
- They have obtained written, informed consent for the publication of the details relating to the patient(s) in this report.
- All possible steps have been taken to safeguard the identity of the patient(s).
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Charles MVP, Srirangaraj S, Kali A. Neonatal sepsis caused by Shewanella algae: A case report. AMJ 2015;8(2):64–66. http//dx.doi.org/10.4066/AMJ.2015.2292
References
- 1.Hornik CP, Fort P, Clark RH, Watt K, Benjamin DK Jr., Smith PB. et al. Early and late onset sepsis in very-lowbirth- weight infants from a large group of neonatal intensive care units. Early Hum Dev. 2012;88(2):S69–74. doi: 10.1016/S0378-3782(12)70019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker CJ, Barrett FF. Group B streptococcal infections in infants. The importance of the various serotypes. JAMA. 1974;230:1158–60. [PubMed] [Google Scholar]
- 3.Shah BA, Padbury JF. Neonatal sepsis: an old problem with new insights. Virulence. 2014;5:170–8. doi: 10.4161/viru.26906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Otsuka T, Noda T, Noguchi A, Nakamura H, Ibaraki K, Yamaoka K. Shewanella infection in decompensated liver disease: a septic case. J Gastroenterol. 2007;42:87–90. doi: 10.1007/s00535-006-1957-0. [DOI] [PubMed] [Google Scholar]
- 5.Khashe S, Janda JM. Biochemical and pathogenic properties of Shewanella alga and Shewanella putrefaciens. J Clin Microbiol. 1998;36:783–7. doi: 10.1128/jcm.36.3.783-787.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pagani L, Lang A, Vedovelli C, Moling O, Rimenti G, Pristera R. et al. Soft tissue infection and bacteremia caused by Shewanella putrefaciens. J Clin Microbiol. 2003;41:2240–1. doi: 10.1128/JCM.41.5.2240-2241.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brink AJ, van Straten A, van Rensburg AJ. Shewanella (Pseudomonas) putrefaciens bacteremia. Clin Infect Dis. 1995;20:1327–32. doi: 10.1093/clinids/20.5.1327. [DOI] [PubMed] [Google Scholar]
- 8.Chen YS, Liu YC, Yen MY, Wang JH, Wann SR, Cheng DL. Skin and soft-tissue manifestations of Shewanella putrefaciens infection. Clin Infect Dis. 1997;25:225–9. doi: 10.1086/514537. [DOI] [PubMed] [Google Scholar]
- 9.Sharma KK, Kalawat U. Emerging infections: Shewanella–a series of five cases. J Lab Physicians. 2010;2:61–5. doi: 10.4103/0974-2727.72150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu PY, Lin CF, Tung KC, Shyu CL, Wu MJ, Liu JW. et al. Clinical and microbiological features of Shewanella bacteremia in patients with hepatobiliary disease. Intern Med. 2013;52:431–8. doi: 10.2169/internalmedicine.52.8152. [DOI] [PubMed] [Google Scholar]
- 11.Vignier N, Barreau M, Olive C, Baubion E, Theodose R, Hochedez P. et al. Human infection with Shewanella putrefaciens and S. algae: report of 16 cases in Martinique and review of the literature. Am J Trop Med Hyg. 2013;89:151–6. doi: 10.4269/ajtmh.13-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]


