Abstract
BACKGROUND
Hypertension (HTN) considers as one of the most common risk factors, which potentially raises the risk of cardiovascular disease. Regarding high prevalence of HTN among Iranian population this study designed to examine a range of socio-demographic and clinical variables to determine the association with failure to achieve blood pressure control in a cohort of hypertensive subjects.
METHODS
This retrospective cohort study is a part of Isfahan cohort study which carried out on adults aged 35 years old or more. Subjects with confirmed HTN entered in this sub-study. For all subjects questionnaire included socio-demographic characteristics, clinical data and lifestyle behavior completed by trained nurses. Uncontrolled HTN was defined as systolic and diastolic blood pressure more than 140/90 in the presence or absent of pharmacological treatment.
RESULTS
The prevalence of uncontrolled men was significantly higher than controlled in both 2001 and 2007 (P < 0.001). A significant association was found between sex and control of blood pressure: compared with women, being men [odds ratio (OR) = 2.31; 95 % confidence interval (CI) = 1.64-3.24] was significantly associated with uncontrolled HTN in 2001 and (OR = 2.38; 95% CI = 1.78-3.18). Among lifestyle behaviors, tendency for more consumption of salty foods increased the risk of uncontrolled HTN in 2001 by 1.73 times [OR = 1.73, 95% CI = 1.20-2.50, (P = 0.003)]. Patients who were naive to mono-therapy without considering the type of antihypertensive drug were found to be associated with uncontrolled blood pressure (OR = 0.14; 95 % CI =0.1-0.2).
CONCLUSION
Uncontrolled HTN was sex, marital status, diabetes, tendency to salty foods and medication adherence. Assessment of them presence of these risk factors is warranted to recommend an aggressive HTN management with the goal of reducing excessive risk of cardiovascular events caused by uncontrolled HTN.
Keywords: Prevalence, Hypertension, Uncontrolled, Risk Factors
Introduction
Hypertension (HTN) considers as one of the most common risk factors, which potentially raises the risk of cardiovascular disease (CVD)1 and consider as a major public health problem in most developed and in developing countries.2 HTN affects around one billion individuals around the world, and the relationship between blood pressure and the risk of cardiovascular events is continuous, consistent, and independent of other risk factors.3 The national surveillance step-wise study which was done by the Iranian Ministry of Health demonstrated a prevalence of 25% for HTN among adults aged 25-64 years.4 Moreover, according to available data, the rate of controlled HTN is widely varied among different countries ranged from 2.2% in Eastern Europe, < 5% in China to more than 38.0% in Western Europe, North America and 18.0% in Iran.5 It follows from all the above mentioned that a growing number of hypertensive patients are faced with undiagnosed HTN and or uncontrolled HTN.6 More importantly, a large part of the patients (17.6% female and 18.0% of male) faced to uncontrolled HTN in Iran.7
Several reports described key variables of uncontrolled HTN, which these barriers varied in different population. 6 poor medication, sedentary lifestyle and unhealthy eating, as well as high salt consumption, have defined as main fences in control of HTN around the world.8,9
Many studies have examined risk factors for HTN, and several comprehensive management guidelines have been published.7,10-12 However, the risk factors for uncontrolled HTN are less well established.7,11,12 Previous studies claimed that individuals diagnosed with HTN whether they have untreated, undertreated or treatment-resistant HTN, have consistent characteristics that could provide insight to improve blood pressure control.12-14
As intensive efforts need to control blood pressure and hence we have to evaluate determinants to achieving higher HTN control rates. The aim of this study was to examine a range of socio-demographic and clinical variables to determine the association with failure to achieve blood pressure control in a cohort of hypertensive subjects.
Materials and Methods
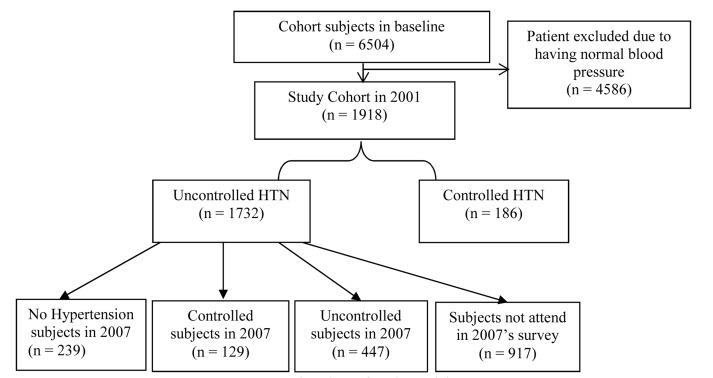
The Isfahan cohort study (ICS), Iran, is a population-based, ongoing longitudinal study of adults aged 35 years old or more, living in urban and rural areas of three counties in central Iran namely Isfahan, Najafabad and Arak.15 Baseline data collection for the ICS began in 2001. Participants were selected by multistage random sampling and were recruited to reflect the age, sex and urban/rural distribution of the community.16,17 The Ethics Committee of the Isfahan Cardiovascular Research Center approved the study. The study sample included 6504 subjects 35 ≥ years of age (average 51.0 ± 11.7 years) that had complete demographic data, diagnoses, vital signs, pharmacy utilization, and personal information. In this sub-study, totally 1986 patients with a diagnosis of HTN were identified in the ICS database. The study cohort was 186 cases with controlled HTN and 1732 with uncontrolled HTN in 2001 (Figure 1). All participants provided their informed consent to participate in the clinical examination and follow-up study.
Figure 1.
Flowchart of study participants HTN: Hypertension
This sub-study sought to identify patient risk factors for uncontrolled blood pressure among Iranian patients with HTN. This study evaluated patients with a diagnosis of HTN over a 3-year period between 2001 and 2007.
In addition, each subject had at least 3 HTN diagnostic coding events and at least 3-recorded BP readings. The minimum 3 blood pressure readings occurred within the 3-year study period and were obtained at separate office visits. A subject’s blood pressure was measured once, however, if elevated, a repeat BP was taken 5 min later. The lowest blood pressure reading was recorded. HTN was defined as systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg17, HTN for diabetic and renal failure patients defined as defined, as a blood pressure ≥ 130/80 mmHg is an extremely common co-morbid condition in diabetes. Subjects who had an HTN diagnosis for < 6 months, patients with no medical record, and patients who were pregnant were excluded from the study.
Uncontrolled HTN was defined as SBP and DBP more than 140/90 in the presence or absent of pharmacological treatment.
After obtaining informed written consent, medical interview and physical examination were conducted. Measurements of blood pressure, anthropometric parameters, as well as fasting blood tests, were carried out following standard protocols and using calibrated instruments as has been described previously.18 Waist circumference (WC) was taken as the smallest circumference at or below the costal margin. HTN was defined as SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg in men and women or treatment of previously diagnosed HTN. Subjects who smoked daily were considered as current smoker. In 2007 (the 7th year of follow-up), participants were invited for repeated laboratory measurements, physical examination and interview using the same protocol as a baseline survey. Laboratory measurement methods were similar in 2001 and 2007 but the auto analyzer was different (Eppendorf, Hamburg, Germany in 2001 and Hitachi 902, Japan in 2007). Both instruments have been validated with an external standard laboratory center.
Pharmacological treatment: using angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker, a-blocker, b-blocker, vasodilators, dihydropyridine calcium channel blocker, Non-dihydropyridine calcium channel blocker, aldosterone antagonist, potassium-sparing diuretic, thiazide were consider in this study as mono-therapy or combination therapy.
Data are presented as number (percentage), means and standard deviation, chi-square and t-test were used to compare characteristics between two groups. Multiple logistic regression was used in an explanatory framework for evaluating the relationship between potential determinants of controlling HTN on all the derived demographic, administrative, and pharmacy records. The statistical software SPSS for windows (version 20.0, SPSS Inc., Chicago, IL, USA) was used. P < 0.050 was considered to be significant.
Results
A comparison of patient baseline characteristics for controlled and controlled HTN is presented in table 1. The prevalence of uncontrolled men was significantly higher than controlled in both 2001 and 2007 (P < 0.001). No significant changes observed between educational level in both 2001 and 2007 between subjects with and without controlled HTN (P = 0.265, P = 0.696). Regarding comorbid disease diabetes was significantly higher among uncontrolled subjects in 2001 and 2007 (P < 0.001). Tendency to using salty food was significantly higher between controlled HTN and uncontrolled patients in 2001 (P < 0.001), but in 2007 smoking habit was higher among uncontrolled subjects (P = 0.020). Mono-therapy by anti-hypertensive drugs was more prevalent among subjects with controlled HTN (P = 0.001), similarly combination therapy by two antihypertensive drugs was more prevalent among patients with controlled HTN (P = 0.001).
Table 1.
Demographic characteristics of study participants based on control of hypertension (HTN) and year of follow-up
| 2001 |
2007 |
|||||
|---|---|---|---|---|---|---|
| Controlled | Uncontrolled | P | Controlled | Uncontrolled | P | |
| Age | 60.67 ± 11.14 | 57.39 ± 11.65 | < 0.001 | 60.8 ± 10.63 | 60.8 ± 10.45 | 0.761 |
| Sex (male) | 49 (26.34) | 783 (45.20) | < 0.001 | 82 (30.59) | 488 (51.20) | < 0.001 |
| Residency (rural) | 36 (19.40) | 515 (29.70) | 0.003 | 57 (21.30) | 277 (29.10) | 0.011 |
| Education | ||||||
| Illiterate | 107 (57.52) | 888 (51.27) | 0.265 | 110 (41.04) | 416 (43.65) | 0.696 |
| Primary school | 50 (26.88) | 541 (31.23) | 93 (34.70) | 325 (34.10) | ||
| More than primary school | 29 (15.59) | 303 (17.49) | 65 (24.25) | 212 (22.24) | ||
| Insurance | 235 (87.70) | 827 (87.00) | 0.754 | - | - | |
| Marital status | ||||||
| Married | 135 (72.58) | 1491(86.08) | < 0.001 | 222 (83.14) | 817 (86.00) | 0.125 |
| Single | 0 (0) | 8 (0.50) | 0 (0) | 3 (0.30) | ||
| Divorced | 1 (0.50) | 7 (0.40) | 1 (0.40) | 0 (0) | ||
| Widowed | 50 (29.60) | 226 (13.00) | 44 (16.50) | 130 (13.70) | ||
| Comorbid disease | ||||||
| Obesity* | 46 (24.73) | 518 (29.90) | 0.140 | 92 (34.32) | 309 (32.42) | 0.557 |
| Diabetes | 8 (4.30) | 375 (21.65) | < 0.001 | 48 (17.90) | 335 (35.20) | < 0.001 |
| Dyslipidemia | 22 (91.35) | 1548 (91.00) | 0.851 | 209 (78.00) | 775 (81.30) | 0.222 |
| Lifestyle Behavior | ||||||
| Smoking habits | 27 (14.50) | 307 (17.80) | 0.388 | 21 (7.90) | 133 (14.40) | 0.020 |
| Tendency to salty foods | 116 (62.30) | 1146 (66.20) | < 0.001 | 87 (32.60) | 303 (31.00) | 0.113 |
| Physical inactivity | 149 (80.10) | 1416(81.75) | 0.581 | 213 (79.47) | 743 (77.96) | 0.595 |
| Pharmacological treatment | ||||||
| Mono-therapy | 132 (70.90) | 458 (26.40) | < 0.001 | 172 (64.20) | 311 (32.60) | 0.006 |
| Combination therapy by Two drug | 10 (5.40) | 66 (3.80) | 37 (13.80) | 70 (7.30) | ||
| Combination therapy by three | 4 (2.10) | 9 (0.51) | 15 (5.60) | 14 (1.50) | ||
| No drug usage | 40 (21.50) | 1199 (69.20) | 44 (16.40) | 558 (58.50) | ||
| Knowledge | 186 (100.00) | 1623 (93.70) | 268 (100) | 919 (97.20) | ||
| Practice | 127 (68.27) | 453 (61.88) | 0.106 | 101 (37.70) | 166 (31.80) | 0.098 |
Obesity defined as (body mass index > 30)
Table 2 shows demographic and clinical aspects of uncontrolled hypertensive subjects after 7 years of follow-up. After 6 years of follow-up, from 1732 subjects who were uncontrolled HTN in 2001, 129, 447 and 239 patients were controlled, uncontrolled and no signs of HTN respectively. Otherwise, 917 subjects were lost of follow-up. Among above-mentioned subjects mean of age was significantly higher among uncontrolled HTN (P < 0.001), whereas, no significant changes has seen regarding education and marital status (0.071, 0.291). Among co-morbid disease, obesity was more prevalent among controlled HTN subjects but diabetes and dyslipidemia was more prevalent among uncontrolled subjects. Lifestyle behavior except tendency to salty food has not any significant difference among groups. No drug usage is more prevalent among uncontrolled subjects (41.2%), (P < 0.001).
Table 2.
Demographic and clinical aspects of uncontrolled hypertensive subjects after 7 years of follow-up
| Subjects in 2007 | Subjects with Uncontrolled Hypertension in 2001 (n = 1732*) | |||
|---|---|---|---|---|
| Controlled (n = 129) | Uncontrolled (n = 447) | No hypertension (n= 239) | P | |
| Age | 62.66 ± 10.62 | 67.81 ± 10.04 | 58.86 ± 11.57 | < 0.001 |
| Sex (male) | 38 (29.50) | 209 (46.80) | 119 (49.80) | < 0.001 |
| Education | ||||
| Illiterate | 56 (43.40) | 213 (47.70) | 88 (36.80) | 0.071 |
| Primary school | 44 (34.10) | 146 (32.70) | 86 (36.00) | |
| More than primary school | 29 (22.50) | 88 (19.70) | 65 (27.20) | |
| Marital Status | ||||
| Married | 111 (86.7) | 377 (84.7) | 209 (88.2) | 0.291 |
| Single | 0 (0.0) | 0 (0.0) | 1 (0.4) | |
| Divorced | 1 (0.8) | 0 (0.0) | 0 (0.0) | |
| Widowed | 16 (12.5) | 68 (15.3) | 27 (11.4) | |
| Co morbid disease | ||||
| Obesity | 52 (40.3) | 151 (33.8) | 65 (27.2) | 0.032 |
| Diabetes | 32 (24.8) | 190 (42.5) | 52 (21.8) | < 0.001 |
| Dyslipidemia | 103 (79.8) | 365 (81.7) | 174 (72.8) | 0.025 |
| Lifestyle Behavior | ||||
| Smoking Habits | 6 (4.7) | 23 (5.2) | 21 (8.9) | 0.127 |
| Tendency to salty Foods | 64 (50.0) | 243 (54.5) | 159 (67.4) | 0.001 |
| Physical inactivity | 100 (77.5) | 345 (77.2) | 188 (78.7) | 0.905 |
| Drugs | ||||
| One drug | 76 (58.9) | 202 (45.2) | 0 (0.0) | < 0.001 |
| Two drugs | 24 (18.6) | 50 (11.2) | 0 (0.0) | |
| Three drugs | 9 (7.0) | 11 (2.5) | 1 (0.4) | |
| No drugs | 15(15.5) | 184(1.2) | 238 (9.6) | |
917 subjects did not attend in the 2007 survey
Odds ratios (ORs) > 1 were associated with uncontrolled HTN, and ORs < 1 were associated with controlled HTN (Table 3). A significant association was found between sex and control of blood pressure; compared with women, being men (OR = 2.31; 95% CI = 1.64-3.24) was significantly associated with uncontrolled HTN in 2001 and (OR = 2.38; 95% CI = 1.78-3.18). Education was not associated with blood pressure control in both 2001 and 2007 [OR = 1.26; 95% CI = 1.26 (0.82-1.94) and OR = 0.86, 95% CI (0.61-1.22) respectively]. However, partner status has associated with uncontrolled blood pressure (OR, 0.41; 95% CI [0.29-0.58]) Diabetes considered as a powerful predictor for controlled HTN in both 2001 and 2007 [2001: OR = 6.15; 95% CI (3.00-12.60), 2007: OR = 2.48; 95% CI (1.77-3.48), respectively]. Among lifestyle behaviors, tendency for more consumption of salty foods increased the risk of uncontrolled HTN in 2001 by 1.73 times [OR = 1.73, 95% CI (1.20-2.50), (P = 0.003)] but this item was not associated with control of blood pressure in 2007 (P = 0.069). Patients who were naive to mono-therapy without considering the type of antihypertensive drug were found to be associated with uncontrolled blood pressure [OR = 0.14; 95% CI (0.1-0.2)].
Table 3.
Assessment factors affecting on the uncontrolled hypertension (HTN)
| 2001 |
2007 |
|||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age | 0.97 (0.96-0.98) | < 0.001 | 1.00 (0.99-1.01) | 0.987 |
| Sex (male) | 2.31 (1.64-3.24) | < 0.001 | 2.38 (1.78-3.18) | < 0.001 |
| Education | ||||
| Illiterate | 1 | 1 | ||
| Primary school | 1.30 (0.92-1.85) | 0.140 | 0.92 (0.68-1.26) | 0.620 |
| More than primary school | 1.26 (0.82-1.94) | 0.294 | 0.86 (0.61-1.22) | 0.405 |
| Marital status | ||||
| Married | 1 | 1 | ||
| Single | - | - | - | - |
| Divorced | 0.63 (0.77-5.19) | 0.671 | - | - |
| Widowed | 0.41 (0.29-0.58) | < 0.001 | 0.80 (0.55-1.16) | 0.248 |
| Comorbid disease* | ||||
| Obesity | 1.29 (0.92-1.84) | 0.142 | 0.92 (0.69-1.22) | 0.558 |
| Diabetes | 6.15 (3.00-12.60) | < 0.001 | 2.48 (1.77-3.48) | < 0.001 |
| Dyslipidemia | 0.95 (0.55-1.63) | 0.857 | 1.22 (0.88-1.71) | 0.223 |
| CVD | 1.25 (0.81-1.93) | 0.313 | 0.68 (0.48-0.97) | 0.031 |
| Lifestyle behavior | ||||
| Smoking habits | 1.27 (0.83-1.95) | 0.270 | 1.88 (1.03-3.42) | 0.040 |
| Tendency to salty foods | 1.73 (1.20-2.50) | 0.003 | 1.29 (0.98-1.69) | 0.069 |
| Physical inactivity | 0.89 (0.61-1.31) | 0.582 | 1.09 (0.74-1.52) | 0.596 |
| Pharmacological treatment | ||||
| No drugs | 1 | - | 1 | - |
| Mono-therapy | 0.12 (0.09-0.18) | < 0.001 | 0.14 (0.10-0.20) | < 0.001 |
| Combination therapy by two drug | 0.27 (0.11-0.65) | 0.002 | 0.15 (0.90-0.20) | 0.085 |
| Combination therapy by three drug | 0.08 (0.02-0.27) | < 0.001 | 0.7 (0.30-0.20) | 0.095 |
Control hypertension (HTN) consider as reference group; Control of Co-morbid disease consider as not having these conditions; OR: Odds ratio; CI: Confidence interval; CVD: Cardiovascular disease
Discussion
This retrospective cohort study recognized major patient features associated with uncontrolled HTN were sex, marital status, diabetes, tendency to salty foods and medication adherence. To the best of our knowledge, this is the first report, which focused on uncontrolled HTN in a sample of cohort Iranian population. Similarly, Egan et al. demonstrated this sex-dependent uncontrolled HTN.12 Marital status also showed a significant relationship with HTN control, partnered hypertensive patients were at higher risk of uncontrolled HTN. Studies conducted in Europe also evaluated partner status, and its association with HTN. Similarly, in a Dutch population, patients without a partner were found to have had a higher risk for uncontrolled HTN.19 Similarly, de Gaudemaris et al.20 and Lessa et al.21 studied on French population observed that single men might have had an association with the prevalence of HTN; however, this finding was not statistically significant.
Our results showed education could not play a crucial role to having controlled HTN. Similar to our obtained results, a recent study in Brazil has shown that education was not a good predictor for adherence to treatment of HTN.22 Association of cardiovascular risk factors and blood pressure was described previously.23-25 But how other cardiovascular risk factors could effect on the control of HTN is still on in debt. Our data showed that there is a potentially negative role of diabetes in the control of HTN for hypertensive patients. Similarly, Bog-Hansen et al. showed uncontrolled blood pressure is in both sexes related to type 2 diabetes.26 The VIIDA registry, which was also carried out in Spain, identified DM and left ventricular hypertrophy as the main factors associated with lack of BP control.27
In this study, although central obesity in subjects with uncontrolled HTN was significantly higher than other group but overall obesity was not significantly associated with control of blood pressure. Previously, Cordero et al. discussed the effect of metabolic alterations associated with obesity might be associated with the intra-abdominal visceral fatty mass.28 In effect, it was shown that the type of visceral adipose tissue was associated with intolerance to glucose and high lipid levels, even after adjustment for BMI and age. The link between smoking and CVD has been evidently recognized. Our results show that smoking is also associated with uncontrolled HTN. Smoking induces endothelial dysfunction, vasoconstriction, insulin resistance, and dyslipidemia, certain forms of which could explain our results.29 Instead, smokers are more sedentary and have unhealthy diets, and these are factors, which can directly raise blood pressure. Subjects with unhealthful lifestyles such as propensity to salty foods and diets are also associated with poorer with blood pressure control.30
We also found that age and CVD were associated with blood pressure control, which could reflect CVD subjects have better practice about their disease. It seems that these patients are more aware of control of HTN. The number of antihypertensive drugs used showed a much weaker association with control of blood pressure. We did not find any significant difference between type of one drug and control of HTN (data not showed) but these results showed without considering the type of antihypertensive drugs, treatment by one or two drug could not useful to control of HTN, so combination therapy may be useful based on clinical aspects of penitents. Treatment guidelines note that the combination of an angiotensin receptor blocker and a calcium channel blocker, similar to the combination of an angiotensin-converting enzyme inhibitor or an ARB plus a diuretic, provides an effective option for patients with HTN.
For greater success, treatment must always be associated with other non-pharmacological interventions. The cost of medication may be a barrier for the control of HTN and must be an important factor in the choice of antihypertensive drugs.
The results of the study that done by Allemann et al. showed combining antihypertensive drugs with complementary mechanisms of action for the treatment of patients with HTN. They indicated that combination therapy lowers blood pressure to a greater degree than mono-therapy.31
Study strengths and limitations
These studies strengthen to random and large patient population reflecting the communities from which it was drawn. In addition, a large number of variables were investigated to explore multiple associations with uncontrolled blood pressure. Although some previous studies reported acceptable control of HTN, but their results were limited to small sample size which were under control by regular clinic visiting. However, several limitations exist in our investigation. First, there are inherent limitations associated with the retrospective cohort study design. Second, in our questionarie we asked about attitude and practice of patients regarding control of HTN but there is a lack of data regarding regular visiting patients in clinics or home monitoring.
Conclusion
Uncontrolled HTN was sex, marital status, diabetes, tendency to salty foods and medication adherence. Assessment of them presence of these risk factors is warranted to recommend an aggressive HTN management with the goal of reducing excessive risk of cardiovascular events caused by uncontrolled HTN.
Acknowledgments
This study was done as a residency thesis and was done as a part of ICS which conducted by ICRC affiliated with the Isfahan University of Medical Sciences.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Carretero OA, Oparil S. Essential hypertension. Part I: definition and etiology. Circulation. 2000;101(3):329–35. doi: 10.1161/01.cir.101.3.329. [DOI] [PubMed] [Google Scholar]
- 2.Ching GW, Beevers DG. Hypertension. Postgrad Med J. 1991;67(785):230–46. doi: 10.1136/pgmj.67.785.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haghdoost AA, Sadeghirad B, Rezazadehkermani M. Epidemiology and heterogeneity of hypertension in Iran: a systematic review. Arch Iran Med. 2008;11(4):444–52. [PubMed] [Google Scholar]
- 4.Noohi F, Sarrafzadegan N, Khosravi A, Andalib E. The first Iranian recommendations on prevention, evaluation and management of high blood pressure. ARYA Atheroscler. 2012;8(3):97–118. [PMC free article] [PubMed] [Google Scholar]
- 5.Gharipour M, Khosravi A, Sadeghi M, Roohafza H, Hashemi M, Sarrafzadegan N. Socioeconomic characteristics and controlled hypertension: Evidence from Isfahan Healthy Heart Program. ARYA Atheroscler. 2013;9(1):77–81. [PMC free article] [PubMed] [Google Scholar]
- 6.Maimaris W, Paty J, Perel P, Legido-Quigley H, Balabanova D, Nieuwlaat R, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med. 2013;10(7):e1001490. doi: 10.1371/journal.pmed.1001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation. 2005;112(11):1651–62. doi: 10.1161/CIRCULATIONAHA.104.490599. [DOI] [PubMed] [Google Scholar]
- 8.Kannel WB. Prevalence and implications of uncontrolled systolic hypertension. Drugs Aging. 2003;20(4):277–86. doi: 10.2165/00002512-200320040-00004. [DOI] [PubMed] [Google Scholar]
- 9.Tavassoli A, Gharipour M, Toghianifar N, Sarrafzadegan N, Khosravi A, Zolfaghari B, et al. The impact of obesity on hypertension and diabetes control following healthy Lifestyle Intervention Program in a developing country setting. J Res Med Sci. 2011;16(Suppl 1):S368–S376. [PMC free article] [PubMed] [Google Scholar]
- 10.Khosravi A, Mehr GK, Kelishadi R, Shirani S, Gharipour M, Tavassoli A, et al. The impact of a 6-year comprehensive community trial on the awareness, treatment and control rates of hypertension in Iran: experiences from the Isfahan healthy heart program. BMC Cardiovasc Disord. 2010;10:61. doi: 10.1186/1471-2261-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ezzati M, Oza S, Danaei G, Murray CJ. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation. 2008;117(7):905–14. doi: 10.1161/CIRCULATIONAHA.107.732131. [DOI] [PubMed] [Google Scholar]
- 12.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124(9):1046–58. doi: 10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egan BM, Zhao Y, Li J, Brzezinski WA, Todoran TM, Brook RD, et al. Prevalence of optimal treatment regimens in patients with apparent treatment-resistant hypertension based on office blood pressure in a community-based practice network. Hypertension. 2013;62(4):691–7. doi: 10.1161/HYPERTENSIONAHA.113.01448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Egan BM, Laken MA. Is blood pressure control to less than 140/less than 90 mmHg in 50% of all hypertensive patients as good as we can do in the USA: or is this as good as it gets? Curr Opin Cardiol. 2011;26(4):300–7. doi: 10.1097/HCO.0b013e3283474c20. [DOI] [PubMed] [Google Scholar]
- 15.Sarrafzadegan N, Talaei M, Sadeghi M, Kelishadi R, Oveisgharan S, Mohammadifard N, et al. The Isfahan cohort study: rationale, methods and main findings. J Hum Hypertens. 2011;25(9):545–53. doi: 10.1038/jhh.2010.99. [DOI] [PubMed] [Google Scholar]
- 16.Gharipour M, Sarrafzadegan N, Sadeghi M, Andalib E, Talaie M, Shafie D, et al. Predictors of metabolic syndrome in the Iranian population: waist circumference, body mass index, or waist to hip ratio? Cholesterol. 2013;2013:198384. doi: 10.1155/2013/198384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Talaei M, Sadeghi M, Mohammadifard N, Shokouh P, Oveisgharan S, Sarrafzadegan N. Incident hypertension and its predictors: the Isfahan Cohort Study. J Hypertens. 2014;32(1):30–8. doi: 10.1097/HJH.0b013e32836591d4. [DOI] [PubMed] [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 19.van Rossum CT, van de Mheen H, Witteman JC, Hofman A, Mackenbach JP, Grobbee DE. Prevalence, treatment, and control of hypertension by sociodemographic factors among the Dutch elderly. Hypertension. 2000;35(3):814–21. doi: 10.1161/01.hyp.35.3.814. [DOI] [PubMed] [Google Scholar]
- 20.de Gaudemaris R, Lang T, Chatellier G, Larabi L, Lauwers-Cances V, Maitre A, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension. 2002;39(6):1119–25. doi: 10.1161/01.hyp.0000018912.05345.55. [DOI] [PubMed] [Google Scholar]
- 21.Lessa I, Fonseca J. Race, compliance to treatment and/or consultation and control of arterial hypertension. Arq Bras Cardiol. 1997;68(6):443–9. [PubMed] [Google Scholar]
- 22.Busnello RG, Melchior R, Faccin C, Vettori D, Petter J, Moreira LB, et al. Characteristics associated with the dropout of hypertensive patients followed up in an outpatient referral clinic. Arq Bras Cardiol. 2001;76(5):349–54. doi: 10.1590/s0066-782x2001000500001. [DOI] [PubMed] [Google Scholar]
- 23.Christofaro DG, Fernandes RA, Oliveira AR, Freitas Junior IF, Barros MV, Ritti-Dias RM. The association between cardiovascular risk factors and high blood pressure in adolescents: a school-based study. Am J Hum Biol. 2014;26(4):518–22. doi: 10.1002/ajhb.22555. [DOI] [PubMed] [Google Scholar]
- 24.Vishram JK, Borglykke A, Andreasen AH, Jeppesen J, Ibsen H, Jorgensen T, et al. Do other cardiovascular risk factors influence the impact of age on the association between blood pressure and mortality? The MORGAM Project. J Hypertens. 2014;32(5):1025–32. doi: 10.1097/HJH.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 25.Juraschek SP, Kovell LC, Miller ER, Gelber AC. Dose-response association of uncontrolled blood pressure and cardiovascular disease risk factors with hyperuricemia and gout. PLoS One. 2013;8(2):e56546. doi: 10.1371/journal.pone.0056546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bog-Hansen E, Lindblad U, Gullberg B, Melander A, Rastam L. Metabolic disorders associated with uncontrolled hypertension. Diabetes Obes Metab. 2003;5(6):379–87. doi: 10.1046/j.1463-1326.2003.00288.x. [DOI] [PubMed] [Google Scholar]
- 27.Redon J, Cea-Calvo L, Moreno B, Monereo S, Gil-Guillen V, Lozano JV, et al. Independent impact of obesity and fat distribution in hypertension prevalence and control in the elderly. J Hypertens. 2008;26(9):1757–64. doi: 10.1097/HJH.0b013e3283077f03. [DOI] [PubMed] [Google Scholar]
- 28.Cordero A, Bertomeu-Martinez V, Mazon P, Facila L, Bertomeu-Gonzalez V, Cosin J, et al. Factors associated with uncontrolled hypertension in patients with and without cardiovascular disease. Rev Esp Cardiol (Engl Ed) 2011;64(7):587–93. doi: 10.1016/j.recesp.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 29.Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ. 1989;298(6676):784–8. doi: 10.1136/bmj.298.6676.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aggarwal B, Mosca L. Lifestyle and psychosocial risk factors predict non-adherence to medication. Ann Behav Med. 2010;40(2):228–33. doi: 10.1007/s12160-010-9212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allemann Y, Fraile B, Lambert M, Barbier M, Ferber P, Izzo JL. Efficacy of the combination of amlodipine and valsartan in patients with hypertension uncontrolled with previous monotherapy: the Exforge in Failure after Single Therapy (EX-FAST) study. J Clin Hypertens (Greenwich) 2008;10(3):185–94. doi: 10.1111/j.1751-7176.2008.07516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]