Abstract
BACKGROUND
Despite exercise is recommended as an adjunct to medication therapy in patients with heart failure (HF), non-adherence to exercise is a major problem. While improving self-efficacy is an effective way to increase physical activity, the evidence concerning the relationship between strategies to enhance self-efficacy and exercise among HF has not been systematically reviewed. The objective of this systematic review is to assess the effect of interventions to change the self-efficacy on exercise in patients with HF.
METHODS
A systematic database search was conducted for articles reporting exercise self-efficacy interventions. Databases such as PubMed, ProQuest, CINAHL, Scopus, and PsycINFO, and the Cochrane Library were searched with restrictions to the years 2000-June 2014. A search of relevant databases identified 10 studies. Published randomized controlled intervention studies focusing strategies to change self-efficacy to exercise adherence in HF were eligible for inclusion. In addition, studies that have applied self-efficacy-based interventions to improve exercise are discussed.
RESULTS
Limited published data exist evaluating the self-efficacy strategies to improve exercise in HF. Dominant strategies to improve patients’ self-efficacy were performance accomplishments, vicarious experience, verbal persuasion, emotional arousal.
CONCLUSION
Evidence from some trials supports the view that incorporating the theory of self-efficacy into the design of an exercise intervention is beneficial. Moreover, exercise interventions aimed at integrating the four strategies of exercise self-efficacy can have positive effects on confidence and the ability to initiate exercise and recover HF symptoms. Findings of this study suggest that a positive relationship exists between self-efficacy and initiating and maintaining exercise in HF, especially in the short-term period.
Keywords: Self-Efficacy, Heart Failure, Exercise
Introduction
Heart failure (HF) affects 2-4% of general population. Prevalence of HF greatly increases at the age of 75; and hence it reaches 10-20% in the ages 70-80. At early ages, due to coronary artery diseases (CAD) in the past decades of life, HF is more prevalent in men than in women. However, in older ages, the incidence is equal for both sexes.1 HF accounts for the highest hospital admission expenses for patients with a total of more than $ 20 billion.2-4
HF is a debilitating disease which affects patients’ function and quality of life (QOL).2,3 HF is often a progressive process. Breathlessness, fatigue, and reduced exercise capacity are common clinical manifestations of HF.4 The results of symptoms for the patients are disorders in their lives, and this means that people with HF, who experience impaired exercise and functional capacity, experience some restrictions in their lives.5 Subsequently, poor exercise adherence and deconditioning happen to these patients, and this leads to a decline in the necessary confidence for initiating and maintaining a regular exercise.6-8
Guidelines from the European Society of Cardiology recommend that all patients with stable chronic HF should exercise regularly.1 A number of studies have shown the benefits of exercise for patients with HF,9 including submaximal exercise capacity10 lower hospital rate and mortality7 and improved QOL.11 Exercise can also reduce many of the symptoms of fatigues and breathlessness because of its effect on the musculoskeletal and cardiovascular systems (European HF Training Group, 1998). For each 1 h exercise, a 5% reduction in all causes of death, a reduction in the rate of hospitalization for all causes, and an increase in maximal oxygen consumption and measures of health status have been observed.12 Strategies to increase physical activity in these patients can improve disease symptoms and outcomes13 and help to prevent hospitalizations and worsening of symptoms.14 80% of patients who suffer from HF believe that exercise is a health behavior.15 However, only 39% of them really participate in exercising.16,17 Indeed, it is difficult for patients with HF to follow and compliance with the recommendations and many of them, even those who have been referred to cardiac rehabilitation centers, do not continue the organized activities.15
The researchers have focused the effect of interventions influencing the exercise in HF.18 Several studies have shown that, in addition to demographic factors, psychosocial factors are also related to physical activity.19 Among that, self-efficacy has been the most dominant variable.20 Self-efficacy is a key component in social cognitive theory (SCT) 21. It has been defined as “the belief in one’s capabilities to organize and execute the courses of action required to produce given attainments.”21 Studies have shown that those with higher self-efficacy significantly spend more energy to keep physically active.22 Among cardiac patients who participated in cardiac rehabilitation programs, self-efficacy is a predictor of exercising behavior for 3 months.23 Furthermore, there is documented evidence that changes in self-efficacy can mediate the effects of behavior change interventions on improving in exercise compliance in chronic obstructive pulmonary disease (COPD).24
Self-efficacy is considered as an important predictor of behavior because it works as an independent construct of the skills of an individual’s activities. It should be noted that the role of self-efficacy in initiating and maintaining health behaviors and compliance to treatment in other chronic diseases such as diabetes type II has been proven.25 However, other studies on coronary artery patients showed no association between exercise self-efficacy, the compliance rate, and exercise intensity.26
Whilst a number of reviews have therefore attempted to provide evidence of what constructs to target in exercise interventions in HF patients, evidence of how to change these constructs is currently unclear. Self-efficacy has a significant influence on exercising in various clinical conditions, the actual impact of strategies to improve self-efficacy for exercise remains ambiguous. Thus, this review was conducted to assess the effect of interventions to change the self-efficacy on exercise of patients with HF.
Materials and Methods
We searched the literature published between January 2000 and June 2014 in the following database: PubMed, ProQuest, CINAHL, Scopus, and PsycINFO, and the Cochrane central register of controlled. We used both controlled vocabulary (e.g., medical subject heading terms) and key words including HF, congestive HF, chronic HF, cardiac failure, left ventricular failure, physical activity, physical training, exercise, training, aerobic training, and self-efficacy and combination of them. We included articles limited to full studies in the English language.
Whilst a number of reviews have therefore attempted to provide evidence of what constructs to target in exercise interventions in HF patients, evidence of how to change these constructs is currently unclear. Self-efficacy has a significant influence on exercising in various clinical conditions, the actual impact of strategies to improve self-efficacy for exercise in HF remain ambiguous. Thus, this review was conducted to assess the effect of interventions to change the self-efficacy on exercise of patients with HF.
This review included the investigations that focused on HF patients who were 18 years old or greater. In systematic step of search, we chose studies, which had a control group in the design, including clinical trial or quasi-experimental. We also included the studies that had an intervention or a strategy to improve the exercise. We included studies of any type of exercise, training or physical activity (i.e., home-based, hospital-based, or cardiac rehabilitation).
We excluded article if: (1) no definition of HF was given including New York Heart Association functional class (NYHA) or physical examination and impaired left ventricular ejection fraction (2) cross-sectional and other observational studies (3) if self-efficacy reflected confidence in recognizing symptoms and didn’t indicate self-efficacy for exercise. (4) HF with preserved ejection fraction (5) poor methodological quality [scored 3 on the physiotherapy evidence database (PEDro) scale].27
As the self-efficacy has been shown that self-efficacy is an influential predictor of exercise, the outcome was defined as exercise self-efficacy that lead to increase any type of physical activity. The exercise could be a subset of physical activity that is planned, structured, and repetitive bodily movement done to improve or maintain at least one of the strength, flexibility, or endurance.28 Exercise could be measured by oxygen consumption at peak exercise test peak oxygen uptake (PVO2), 6 min walk distance test, self-reported questionnaire, or physical function subscale on QOL questionnaires. In this study, exercise and physical activity are generally used interchangeability.
In the initial screen, titles and abstracts of the available electronic resources were reviewed for their potential relevance to the topic by first author (Rajati F). In the included articles, no difference was observed between the three terms of HF, chronic HF, and congestive HF; hence these three phrases were used interchangeably. Keywords that were related to self-efficacy for exercise in HF patients were primarily searched in titles, abstracts and keywords. Then, all articles were reviewed by another author (Hasandokht, T). Kappa coefficient of 0.86 indicated a high degree of agreement in the selected literature. Then, in the second screen, we assessed the articles related to the present review and also articles that did not present enough information in title or abstract by the same two authors to determine whether articles met the inclusion criteria. We excluded some of the articles due to lack of inclusion criteria. At this stage, the Kappa coefficient of 0.89 was obtained. We resolved lack of agreement and final decision about included studies through discussion with a third reviewer.
The quality of individual studies was assessed with the PEDro scale.27 This scale scores article between 0 and 10 depending on whether the 10 items of methodologic rigor are present or absent. Trails were included if a PEDro score was 4 or more. According to the PEDro, quality was assessed by reviewers (Rajati F, Hasandokht T) independently. Any disagreements between the reviewers were resolved by consensus.
Results
Study search and description of studies
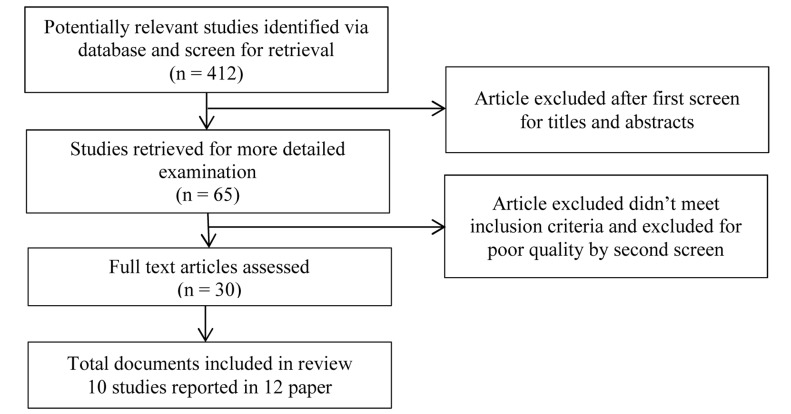
The search to find relative papers located 412 possible references (including duplication between databases): 47 from Pubmed, 16 from PsycINFO, 34 from ProQuest, 20 from cochrane library, and 54 from scopus. All papers that seem relevant from the title and abstract were assessed in full text (n = 30). We excluded 18 studies as they either did not meet review criteria (n = 13)29-40 were poor methodologic quality (PEDro score, < 4) (n = 1)41 or the authors reported only the protocol study (n = 4)42-45 (Figure 1).
Figure 1.
Flow of study selection
This left a total of 8 randomized controlled trials (RCTs) and 2 non-RCT for detailed review. Two studies reported the findings in the four papers.46-49Table 1summarizes the findings of the included articles.
Table 1.
Characteristics of Studies Included in a systematic review
| Author | Sample size | Design | Purpose | Content of intervention to increase self-efficacy | Duration and type of physical activity/exercise | Outcome measurement | NYHA classification | Findings included self-efficacy and exercise |
|---|---|---|---|---|---|---|---|---|
| Barkley and Fahrenwald.50 | 65 Int = 35 (20 male), Con = 40 ( 24 male) | Quasi-experimental | To determine the effect of an SCI in levels of exercise self-efficacy, levels of barrier self-efficacy, and independent exercise | Attention to minute of exercise, reinforcement/using daily log/persuasion about successful exercise, barrier identify/goal setting, plan setting, overcome barrier/self-monitoring of symptom and exertion level | 12 weeks structural exercise with the intensity of 4-5 metabolic equivalents (METs)/3 days/week | - ESE - BARSE scale A self-report of daily independent exercise | Not clear | Patient’s self-efficacy for exercise increased from mean (SD) of 85.35 (17.54) to 86.64 (18.90) on ESE scale. BARSE scores increased from mean (SD) 67.69 (21.33) to 78.22 (20.97), and independent exercise increased from mean (SD) 42.59 (77.06) to 116.72 (80.78) min/week. Within group analysis was significant for change in BARSE (t = 2.347, P = 0.03) and independent exercise (t = 4.210, P < 0.001) |
| Brodie and Inoue46 ,Brodie et al.47 | 60 SC = 20 Int = 18 SC + Int = 22 | Randomized three-group controlled intervention Design | Examination of the effect of physical activity “lifestyle” intervention, based on motivational interviewing, on improvement quality of life at 5 months from baseline, compared with routine care | Motivational interviewing/client-centered counseling/problem-solving | Regular physical activity such as walking | - Leisure-time physical activity questionnaire expressed as kcal/kg/day - 3 day physical activity diary - Medical outcomes short form-36 health survey (SF-36) - MLHF questionnaire A visual tool to assess readiness-to-change | II-III-IV | Self-reported physical activity in the short-term increased (>2 kcal/kg/day). Self-efficacy and motivation scores improved after 5 months follow up in comparison with baseline that none of the patients were not in the stages mentioned above in preparation stage improvements in physical functioning (P < 0.07) and role physical (P < 0.02), on SF-36 were seen |
| Barnason et al.52 | 35 Int = 18 (14 male), Con = 17 (10 male) | Randomized clinical trial repeated measures | To determine the impact of a home communication intervention for HF Coronary Artery Bypass Graft (CABG) patients, self-efficacy, coronary artery disease risk factor modification and functioning | Symptom self-management/risk factor modification education/self-care for CABG/positive reinforcement | 6 weeks home communication intervention (tele health) providing: assessment of patient symptoms, CAD risk factor modification education, Education on CABG recovery, positive reinforcement to increase patients’ self-efficacy | - Barnason Efï¬پcacy expectation scale - Cardiovascular Risk Factor Modiï¬پcation Adherence - Medical Outcomes Study Short - Form-36 | I- II | Patients’ self-efficacy increased over time [F(1,29) = 6.40, P <0.02] in the intervention group than in the control group |
| Collins et al.51 | 31 Int = 15 (15 male), Con = 16 (16 male) | Randomizd controlled clinical trial | To evaluate the effect of 12 weeks rehabilitation program on quality of life, aerobic fitness, difficulty with symptoms of HF, self-efficacy for exercise, and daily activity levels compare with control group | Increasing gradually exercise | 12 weeks Polestriding or/and treadmill walking Cardiac rehabilitation/duration of exercise gradually increased up to 45 to 50 min 3 days/week | - Exercise cardiac self-efficacy - MHLF questionnaire - SF-36-questionnire Physical activity questionnaire | II-III-I | Self-efficacy improved after 12 weeks of training (55.3-12.1 to 63.0-10.9, P = 0.10); 17% improvement in the intervention group compare with the no change in the control group (52.5-16.3 to 52.9-14.7, P = 0.83). self-efficacy improved for patients who continued to exercise at 12 (22%, P = 0.01) and 36 (40%, P = 0.06) weeks. 14% improvement from baseline to 12 weeks on physical functioning score was seen in the intervention group. Difference in the change score on the MLHF was not statistically significant between the 2 groups. Overall activity level was not significantly increased (P = 0.94) |
| Pozehl et al.48 Duncan and Pozehl49 | 42 Int = 22 (12 male), Con = 20 (12 male) | Randomized experimental repeated measures | To assess the effects of a 12 weeks multicomponent exercise training intervention (HF Exercise And Training Camp Heart Camp) on self-efficacy | Exercise accomplishment, goal setting, graphic feedback, and problem-solving, role modeling overcome barrier, self-monitoring about heart rate, rating of perceived exercise, and symptom | 12 weeks structured aerobic exercise with 40-60% Max HR, 3 days/week in a hospital-based rehabilitation setting, and resistance training 2 days/week at home | - Self-efï¬پcacy for exercise MOS SF-36 physical function subscale, KCCQ | II-III | Heart Camp intervention improved patient self-efficacy for exercise over 12 weeks [F(1,2) = 31.25, P = 0.03] compared with a non-significant change [F(1,2) = 2.33, P = 0.27] in control group. The group × time interaction was not significant for the physical function subscale of the SF-36 [F(1,4) = 0.96, P = 0.39] or the physical limitations subscale of the KCCQ [F(1,4)= 0.54, P = 0.50] |
| Gary6 | 32 Int =16 (0 male), Con= 16 (0 male) | Randomized controlled two-group experimental design | The effect of home-based exercise combined walking and education program on exercise self-efficacy in older women with HF | Increasing gradually exercise | 12 weeks Walking with intensity at 40-60% Max HR, 30 min/day, 3 days/week | - Exercise Self-Efficacy, - Outcome expectancy 6-minWT-test - MLHF - A monitor heart rate polar beat watch | II-III | Improving self-efficacy for exercise that resulted in improved functioning on the 6 min Walk Test (203 feet increase in the intervention group via 93 feet decline in the control) increasing physical function on MLHF |
| Maddison et al.54 | 20 (15 male) Int =10 Con = 10 | Randomized controlled trial | To examine the effect of a modeling intervention on increase PVO2 and self-efficacy in people diagnosed with CHF | Role model presentation (DVD) | Exercise test using ramp protocol increasing periods of time (i.e., 2, 4, 6, 8, 10, and 12 min) at three intensities (i.e., easy, moderate, and hard) | - Standardized exercise testing (ramp), - Self-efficacy scale | II-III | The effect of modeling (DVD) intervention on PVO2 F(1,19) = 4.38, P = 0.05 and self-efficacy F(1,19) = 5.80, P < 0.05 was statistically significant |
| Yeh et al.55 | 100 Int = 50 (28 male), Con = 50 (36 male) | Single-blind, multisite, parallel-group, randomized controlled trial | To investigate the effect of Tai Chi exercise on improving functional capacity and quality of life in patients with HF | Skill mastery/showing videotape/encouragement | 12 weeks Tai Chi with intensity at 50-74% Max HR, 60 min/day, 2 days/week | - Standardized exercise testing (ramp) - 6-min walk test - Metabolic cart - Cardiac Exercise Self-efficacy questionnaire | II-III | QoL improved on MLHF (-19 [-23, -3] in the intervention group versus 1 [-16, 3], P = 0.02 control group). Self-efficacy enhanced on cardiac exercise self-efficacy (0.1 [0.1, 0.6] in the intervention versus -0.3 [-0.5, 0.2], P 0.001) in the control group) |
| Oka et al.56 | 24 Int = 12 (12 male), Con = 12 (12 male) | Randomized controlled trial | To evaluate the effect of performance of a single treadmill exercise test and participation in a 3-month program of walking and resistance exercise on self-efficacy in HF patients | Exercise performance/skill mastery | 12 weeks aerobic walking with intensity at 70% Max HR, 40-60 min/day, 3 days/week | - Exercise test - Borg ratings of perceived exertion scale - Self-efficacy expectations scales | II | Self-efficacy scores for walking improved after 3 months of walking and resistance exercise program (P = 0.04). The relationship between self-efficacy for climbing with physical fitness (r = 0.51, P = 0.01) and walking with physical fitness (r = 0.48, p = 0.02) (measured by PVO2) was significant |
| Smeulders et al.53 | 317 Int = 131 (89 male), Con= 186 (141 male) | Randomized, controlled trial | To assess the effects of the CDSMP on health behavior and healthcare utilization in HF | Skills mastery, goal setting, group sessions reinterpretation of symptoms, modelling, and social persuasion | 6 weeks exercise which was not clear duration, frequency, or type | - Physical Activities Scale of (a) walking; (b) swimming; (c) cycling; (d) other physical activity | II-III | Physical activity for walking improved at 6 but not 12 months. differences between intervention and control group patients for swimming or bicycling were not significant |
SC: Standard care, Int: Intervention group; Con: Control group; PVO2: Peak oxygen consumption; CABG: Coronary artery bypass graft; Max HR: Maximum heart rate; SCI: Self-efficacy coaching intervention; ESE: Self-efficacy scale; BARSE: Barriers to self-efficacy for exercise; MLHF: Minnesota living with heart failure questionnaire; KCCQ: Kansas City Cardiomyopathy Questionnaire; CDSMP: Chronic disease management program; SD: Standard deviation; NYHA: New York Heart Association; HF: Heart failure
Reviewed studies were conducted in the United States, New Zealand, and Netherlands. The total number of patients enrolled in included studies was 800, and their sample size ranged from 20 to 317. The majority of patients were 65 ± 10 years. Except for one study46 with II, III, and IV NYHA classification, all the studies included patients with mild (NYHA II) or moderate (NYHA III) HF as measured by the NYHA classification. Three studies were conducted in the cardiac rehabilitation program48,50,51 Barnason et al.52 recruited patients a specific group of HF who had undergone coronary artery bypass graft surgery (CABG); Smeulders et al. also included patients with diastolic dysfunction.53 Most of the studies were performed by Bandura’s self-efficacy theory, whilst another study applied the trans theoretical model (TTM) to develop self-efficacy for exercise.21 All included studies scored over 4 out of 10 on the PEDro scale, with a mean score of 5.6 (range 4- 8) (Table 2).
Table 2.
Quality of included article using PEDro score (ranging from 0 to 10)
| Study | Random allocation | Concealed allocation | Group similar at baseline | Subject blinding | Therapist blinding | Assessor blinding | Less than 15% dropouts | Intention-to-treat analysis | Between-group statistical comparisons | Point measures and variability data | PEDro score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Barkley and Fahrenwald.50 | Y | N | N | N | N | N | Y | N | Y | Y | 4 |
| Barnason et al.52 | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Brodie and Inoue.46 | Y | Y | Y | N | N | N | N | N | Y | Y | 5 |
| Collins et al.51 | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Pozehl et al.48 | Y | N | Y | Y | N | N | N | Y | Y | Y | 6 |
| Gary6 | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Maddison et al.54 | Y | N | N | N | N | N | Y | Y | Y | Y | 5 |
| Yeh et al.55 | Y | N | Y | Y | N | N | Y | Y | Y | Y | 7 |
| Oka et al.56 | Y | N | N | N | N | N | Y | N | Y | Y | 4 |
| Smeulders et al.53 | Y | Y | Y | Y | Y | N | N | Y | Y | Y | 8 |
Y: Yes, N: No
PEDro: Physiotherapy evidence database
Evaluation of the amount exercise was various. Intensity of exercise was specified using energy expenditure 51 or exercise capacity. In several investigations, exercise capacity assessed by 6-min WT 6, 46 or PVO2.54-56 Brodie and Inoue.46 used a leisure-time questionnaire57 walk test. Barnason et al.52 evaluated the differences in exercise level after intervention through cardiovascular risk factor Modification adherence instrument, whilst Collins et al.51 used the 3-day activity diary. Pozehl et al.48 used physical function subscale on SF-36 questionnaire. Smeulder et al.53 measured physical activity level using physical activity scale comprising walking, swimming, bicycling, and other activity domains. Self-efficacy measured using cardiac exercise self-efficacy (CESE) instrument in three included studies.48,51,55 Brodie and Inoue. used a visual scale of readiness to change physical activity to assess the self-efficacy.46 Only one of the studies examines the self-efficacy strategies on physical activity but didn’t use any self-efficacy instrument.53 The strategies to increase self-efficacy for exercise were fairly various. Exercise performance, education, self-monitoring, motivational interview, self-management, goal setting, graphic feedback, problem solving used for enhancing self-efficacy. According to data extraction from included studies, we can categorize following strategies used to enhance exercise self-efficacy in patients HF.
Learning by doing
As it is shown in table 2, in the selected studies, the role of exercise performance on changing self-efficacy to increase regular physical activity is clearly evident. Some studies have shown that self-efficacy in patients gradually increases with exercising. Patients who increase intensity, duration, and frequency of exercising step- by step will be better prepared to participate in exercise activities in future.6,51,56 Therefore, participation in exercise leads to increase self-efficacy for exercise. Self-efficacy in HF is related to the risk factors for cardiovascular disease.52 In the Barnason et al.’s 52 study, there were significant correlations between all medical outcomes study short form-36 subscale scores and self-efficacy scores at 6 weeks after CABG surgery, except for the mental health subscale in the RC group. The relationship in the intervention group was also significant for the “bodily pain” subscale which represents the special relationship between self-efficacy and physical function of the participants’ body. According to the study by Collins et al., which was conducted focusing on cardiac rehabilitation of patients with HF, in the control group after rehabilitation and without any cognitive interventions, self-efficacy of patients did not change for performing physical activities, but in the intervention group the self- efficacy significantly increased.51 Although there was no significant difference in self-efficacy between two groups, but the improved self-efficacy of rehabilitation of patients after 12 and 36 weeks was still survive.51
Recommendation and prescription for home-based exercise through communication intervention lead to increase the self-efficacy in the intervention group compared with the control group in Barnason’s et al.52 study. Collins et al. used the intensity supervised aerobic exercise program for enhancing the self-efficacy in HF patients. In addition to physical function and PVO exercise, self-efficacy of 17% improved in the intervention group.51 Yeh et al. used the tai chi exercise to increase exercise capacity and functional status in their investigation. The tai chi exercise improved self-efficacy scores after 12 weeks intervention.55 Furthermore, 12 weeks cardiac rehabilitation program cause to improve self-efficacy of 31%.48
Providing successful performance strategies derived from self-efficacy theory used to increase the exercise level in the majority of the included articles. One of the upcoming studies conducted a home-based exercise program in women with HF.6
The researcher emphasized the individualized and graded exercise in the intervention group. Program was begun at 40% intensity and 3 days/week. Duration of walking was increased gradually. The goal was to have patients walking at 60% intensity for a minimum of 30 min by the end of 12 weeks. Hypothesis of the study was supported by results that women participated in a walking program would significantly improve their self-efficacy for exercise.6
Role modeling
As exercise tolerance assesses by maximal oxygen uptake (vo2), Maddison et al.54 evaluated the self-efficacy for doing exercise test using role modeling strategy. They provided the observational learning opportunities for patients before performing the exercise. The mean score of self-efficacy for performing exercise tolerance was more in the intervention group than the control group. The model was provided by video film for patients. Maddison et al. conclude self-efficacy served to mediate relations between the role modeling intervention and PVO2.54
Role modeling by a physical therapist of cognitive processes was provided to overcome difficulties with exercise. The small-group sessions were held to increase self-efficacy through incorporating social learning, social exchange, and social comparison. Pozehl et al. reported the 31% improvement in self-efficacy for exercise in the intervention group over 12 weeks.48 Successes of other participants in the cardiac rehabilitation program are a good model to perform the exercise.50
Positive feedback
One of the strategies provided how exercise progress for patients was feedback. Dougherty and et al.45 applied self-regulation strategies included education for integrative self-management, self-evaluation, self-monitoring skills and self-reinforcement. They employed self-evaluation and self-reinforcement to control an aspect of behavior over time. Self-efficacy also can increase through verbal persuasion from expert source. One of the studies used motivational interview to promote physical activity.46 Verbal persuasion trough motivational interview encouraged participants to undertake some form of physical activity, such as walking. In this study, readiness to change ruler, extracted from Procheska and DiClemente’s TTM, was used to classify patients in the contemplation (intending to change) phase of behavior change or pre-contemplation (not thinking about becoming more active). The theory-based framework, which proposes that interventions should be tailored to an individual’s readiness to change, shaped the project by 46 Using motivational interviewing principles demonstrated improvement in self-efficacy scores. The result of the study also indicated the most patients were either in contemplation or in pre-contemplation changing their activity levels.46 Brodie and Inoue. evaluated the patients’ physical activity by selected aspect of the general QOL (SF-36) questionnaire.46 Restating the benefit of exercise by cardiologist, coaching by physical therapist, and providing web-based educational material pertain to exercising attended by the intervention in Pozehl et al.48 Barnason et al. contrasted the effect of usual care with a home communication intervention on exercise. Positive reinforcement was provided to improve patients’ self-efficacy related to symptom management and CAD risk factor modification through telephone intervention. Results showed self-efficacy improved over time when patients reinforced in adoption physical activity after CABG.52 Working staffs with participants to set goal and overcome barriers lead to enhance exercise self-efficacy and self-efficacy to overcome barriers.50
Recognition of sign and problem-solving
Symptom assessment education and recognition of symptoms are strategies were used to increase physical activity in several included studies. Brodei et al. used the brain storming in the motivational intervention sessions to find a solution to overcome physical activity barrier.46 Assessment of HF symptoms (e.g., fatigue or sleep problems) and strategies to manage symptoms through telephone intervention lead to increase patient’s self-efficacy in the communication intervention compared with the standard care group in the Barnason et al. investigation.52 Incorporating several strategies to improve self-efficacy were applied in the Pozehl et al.’s study. These techniques included supervised exercise and performance accomplishment, persuasion, role modeling and vicarious experience, reinterpretation, recognition,48 and problem-solving relating to symptoms46,48 such as shortness of breath by, for example, relaxation techniques and breathing exercise.53 Self-monitoring of symptom severity and self-monitoring of exertion level integrated to the walking program were three components of the 12 week walking intervention in the Gary’s educational investigation.6 Self-monitoring was conducted through measuring the rate of perceived exertion (RPE) borg, a method to determine the level of exercise intensity, and polar beat watch,58 device to monitor heart rate.6,50 The results showed women in the intervention group increased their self-efficacy for adhering to a walking program for a greater duration.6 Finally, one of the included studies applied several methods such as self-care and managing feelings about HF and education for dealing with symptoms in addition to exercise intervention.55
Discussion
The purpose of this study was to investigate recent literature regarding the effect of interventions to improve self-efficacy on HF patients’ exercise. 10 studies were identified that examine aspects of self-efficacy and exercise behavior. All studies presented some source of self-efficacy as an intervention such as exercising gradually, providing role model, feedback, self-monitoring, and problem-solving strategies. As the exercise is a necessary component of self-care or self-management in practical management,59 some studies investigated the effect of self-efficacy on exercise as a part of self-care or self-management behavior.60 Several studies investigated the relationship between exercise self-efficacy and the exercise in the cardiac rehabilitation program.48,50 The 14-year review period allowed for investigation of the most-recent studies regarding self-efficacy and exercise behaviors in patients with HF.
The finding of this review suggests that self-efficacy has a positive effect on initiating and maintaining to physical exercise. The significant correlation between exercise self-efficacy scores and any type of exercise defined in the current study reinforce the hypotheses of the predictability role of self-efficacy in exercise performance. Moreover, there is clear evidence demonstrated that self-efficacy plays a marked role in compliance of regular exercise recommendation in CAD.53 Self-efficacy has been shown to predict physical activity in HF, and enhancing self-efficacy has been demonstrated to have influential short-term effect on adherence to exercise in HF.6,48,49,61 According to Brodie and Inoue, self-efficacious individuals are expected to develop more success in optimistic behavioral change. In addition, improving in self-efficacy predicts the duration and intensity of physical activity as well as performing the treadmill test.46 In investigation of cardiac patients, self-efficacy has been considered as a predictor of cardiac recovery management, social, mental and physical, functioning.52
Exercise self-efficacy is the degree of confidence in individual capability to initiate and maintain participation in exercise. Provides a framework for achieving skills to manage and change exercise behavior.50,62 Four strategies influence an individual’s level of self-efficacy. The included studies used one or more strategies to improve self-efficacy as a mediator to exercise adherence. They are successful performance/mastery experience, vicarious experience, verbal persuasion and physiological arousal.
Successful performance/mastery experience
This strategy will be useful for HF patients who are not able to undertake higher intensity exercise because of physical limitation, breathlessness, fatigues, and other symptoms. Initiating exercise in a low intensity and then increasing to gradually lead to promote confidence in physical activity. However, researchers suggest successful performance will develop through several self-regulation techniques (i.e., heart RPE, and symptoms), goal-setting, and reward of accomplishment.48 Some investigations use the RPE, which could assist patients to feel more confident about monitoring exercise intensity level.49,63,64 Nevertheless, graded mastery experience produces lower effects on self-efficacy than other techniques in non-patients population.65
Vicarious experience
Vicarious experience springs from observational learning. Role modeling from a physical therapist makes the exercise easier for patients. Participating in a group exercise may help patients share several strategies to overcome obstacles (i.e., problem-solving and relapse prevention). According to study of Barkley and Fahrenwald 50, the nature of grouping exercise in the cardiac rehabilitation program gives patients the opportunity to practice exercise in a safe environment and to receive feedback from professionals and other skillful exercise participant. Patients who take part in a home-based program, therefore, may be deprived from the feedback and coaching. Role modeling by a physical therapist of cognitive processes provides to overcome difficulties with exercise. The physical therapist and health care provider should be awareness from probability of cardiac rehabilitation participants’ fear about exercising outside a clinical setting.66 There is well documented evidence showed interventions that used vicarious experience produced significantly higher levels of physical activity self-efficacy than studies where this technique was not included in non-patients population.65
Verbal persuasion
In accordance with self-efficacy theory, the messages using verbal persuasion enhances attitude via vicarious experiences. This strategy influences individual to believe in the capabilities to attain a goal.21 Studies showed interventions that include persuasion and barrier overcoming were related to lower level of self-efficacy those that did not include these strategies.65 Studies in non-cardiac patients have shown verbal persuasion in e-health intervention is a good strategy for improving self-efficacy. Pozehl et al. administered the web-based educational material related to exercising in HFl.48 The study of Barkley and Fahrenwald, staff members use verbal persuasion to support patients, reinforce performances, and structure situations that result in success.50 Providing feedback related to individual progress, and focusing on exercise benefit leads to increase the level of self-efficacy. However, this technique produces a lower level of self-efficacy in adult.65
Physiologic and affective states
Symptom assessment education and recognition and reinterpretation of symptoms affect the patients’ status to continue exercise48. Professional monitoring of exercise capacity guides patients to a better recognition of changes in physical status, and greater self-management.43 Education about exercise-based self-monitoring of heart rate, RPE, and symptoms in HF have a positive effect on self-efficacy.50 Providing reinsurance to individual and guiding to problem solving assist patients to be more self-efficacious in overcoming barriers.43 However, barrier identification in individual without any chronic disease produces a lower level of physical activity self-efficacy.65
The majority of studies showed using any of the techniques above were associated with a higher self-efficacy in the intervention group than the control, except for one study by Barkley and Fahrenwald 50 They concluded no significant between-groups differences. This result may be due to use of the exercise self-efficacy questionnaires that have not been designed specifically for a cardiac population. Whist using the CESE leads to confirm the increasing self-efficacy after intervention in Pozehl et al.48 and Yeh et al.55
Agreement and disagreement with other studies and review
We found three published systematic review about exercise adherence in patients with HF.18,66,67 Although Krista et al. illustrated social support, goal setting, variety of exercise training, supervised booster exercise to enhance exercise training in HF, they concluded the nature of exercise adherence in these patients is unknown. Based mainly on the results of 20 qualitative researches,18 conducted that for patients with HF, exercise influenced by patient’s perception of their body, which affects self-confidence and motivation to exercise. Our review suggests that considering psychosocial factors to engaging individuals in exercising is very important. Tierney et al. also investigated common strategies used to improve adherence to exercise in HF through nine studies.18 Authors showed that motivational strategies such as goal setting, positive reinforcement, and problem-solving might be effective in short term. We also concluded that the mention strategies are a part of sources to enhance self-efficacy for exercise and it leads to exercise adherence. However, in nonclinical population, providing persuasion or motivation, and graded mastery produced a lower level of self-efficacy than other strategies.65
Limitation of the study
Although the majority of studies included in this review had adequate sample size, some investigation used samples that were not characteristic of the population under investigation.54 Some included papers didn’t use a questionnaire that measured the value of self-efficacy. They reported self-efficacy improved after exercise intervention without any note about using a self-efficacy questionnaire.53 Common limitations of studies were not blinding assessing outcome. As blinding study HF patients and therapist in RCTs of exercise is very difficult, none of the upcoming studies reported the therapist blinding criteria, with the except of Smeulder et al.’s syudy.53 However, two studies reported blinding participants.48,55 Only one of the studies included the patients with NYHA class IV.46 There was considerable variation between studies in how outcomes were evaluated and this prevented the pooling of findings in a meta-analysis. For example, exercise was determined based on physical subscale on QoL questionnaire, PVO, 6 min WT, or physical activity questionnaire.
Implications and recommendations for future studies
Although education for regular physical activity is available comprehensively as an inevitable part of the HF management, and considering there is an evidence for clinical and psychological benefits, several clinics faces with the fact that cardiac rehabilitation participation and adherence to exercise in these patients are low. Given that the study shows that theory-based intervention can improve exercise self-efficacy in patients with HF, Besides upon the strategies enhancing motivation such as ongoing feedback to patients, theory-guided behavioral interventions such as SCT, which focusing on self-efficacy could be effective.54 Improving perceived self-efficacy plays a pivotal role in health status.68 Patients had a fear of engaging in activities that cause to HF symptoms. Therefore, it would be beneficial to health care professional and physical therapist to know about patients’ perceived self-efficacy.55 Considering the limited number of studies investigating the effect of self-efficacy strategies on exercise in HF, more research is needed in this area. Bandura’s SCT provides a good framework that health educators can use to develop interventions that encourage patients with HF to perform exercise. As self-efficacy is the key component of SCT and according to findings of other systematic review in nonclinical population that concluded using only one strategy has a weak impact on self-efficacy,62 future studies should use incorporated strategies focusing on improving self-efficacy to examine physical activity level in patients with HF. Several studies investigated the role of predictability of self-efficacy in health status and other clinic outcome in patients with HF and COPD39,68,69 the ability to examine the casualty effect of self-efficacy is limited. This illustrates a need for more studies using clinical trial in this area. In order to minimize variation future study choosing physical activity questionnaire measured the frequency, duration, and intensity components of physical activity is needed.
Conclusion
The evidence shows self-efficacy has a marked effect on performing the exercise in patients with HF. Additionally, this review suggests that all four sources of self-efficacy (i.e., Successful performance, vicarious experience, and verbal persuasion, physiologic and affective states) are important in developing exercise and maintaining exercise behaviors in patients with HF. These strategies in HF could be conducted as performing exercise gradually and graded mastery, applying vicarious experience, providing feedback and persuasion for physical activity, and physiologic and affective interference with HF symptoms and problem-solving regarding barrier of physical activity.15 However, there is not enough evidence to evaluate which type of strategies is the most beneficial in this process.
Findings of this study suggest that a positive relationship exists between self-efficacy and initiating and maintaining exercise in HF, especially in short-term period. Interventions based on integrating all four sources of self-efficacy might also be helpful to promote exercise adherence in a longer term. The review would benefit from research to identify which components of intervention are related to better exercise outcome in HF.
Acknowledgments
We gratefully acknowledge Dr Mohammad Hadi Abbasi from Zahedan University of Medical Sciences for the participation in gathering and grading articles included in the review
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–89. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87(3):235–41. doi: 10.1136/heart.87.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stavem K, Lossius MI, Kvien TK, Guldvog B. The health-related quality of life of patients with epilepsy compared with angina pectoris, rheumatoid arthritis, asthma and chronic obstructive pulmonary disease. Qual Life Res. 2000;9(7):865–71. doi: 10.1023/a:1008993821253. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton AL, Killian KJ, Summers E, Jones NL. Muscle strength, symptom intensity, and exercise capacity in patients with cardiorespiratory disorders. Am J Respir Crit Care Med. 1995;152(6 Pt 1):2021–31. doi: 10.1164/ajrccm.152.6.8520771. [DOI] [PubMed] [Google Scholar]
- 5.Dunderdale K, Thompson DR, Miles JN, Beer SF, Furze G. Quality-of-life measurement in chronic heart failure: do we take account of the patient perspective? Eur J Heart Fail. 2005;7(4):572–82. doi: 10.1016/j.ejheart.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Gary R. Exercise self-efficacy in older women with diastolic heart failure: results of a walking program and education intervention. J Gerontol Nurs. 2006;32(7):31–9. doi: 10.3928/00989134-20060701-05. [DOI] [PubMed] [Google Scholar]
- 7.Flynn KE, Pina IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1451–9. doi: 10.1001/jama.2009.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKelvie RS, Teo KK, Roberts R, McCartney N, Humen D, Montague T, et al. Effects of exercise training in patients with heart failure: the Exercise Rehabilitation Trial (EXERT). Am Heart J. 2002;144(1):23–30. doi: 10.1067/mhj.2002.123310. [DOI] [PubMed] [Google Scholar]
- 9.O'Connor CM, Whellan DJ. Understanding heart failure through the HF-ACTION baseline characteristics. Am Heart J. 2009;158(4 Suppl):S1–S5. doi: 10.1016/j.ahj.2009.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalal H, et al. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;4:CD003331. doi: 10.1002/14651858.CD003331.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies EJ, Moxham T, Rees K, Singh S, Coats AJ, Ebrahim S, et al. Exercise training for systolic heart failure: Cochrane systematic review and meta-analysis. Eur J Heart Fail. 2010;12(7):706–15. doi: 10.1093/eurjhf/hfq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keteyian SJ. Exercise training in congestive heart failure: risks and benefits. Prog Cardiovasc Dis. 2011;53(6):419–28. doi: 10.1016/j.pcad.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 13.Bennett SJ, Milgrom LB, Champion V, Huster GA. Beliefs about medication and dietary compliance in people with heart failure: an instrument development study. Heart Lung. 1997;26(4):273–9. doi: 10.1016/s0147-9563(97)90084-4. [DOI] [PubMed] [Google Scholar]
- 14.van der Wal MH, Jaarsma T, Moser DK, van Veldhuisen DJ. Development and testing of the Dutch Heart Failure Knowledge Scale. Eur J Cardiovasc Nurs. 2005;4(4):273–7. doi: 10.1016/j.ejcnurse.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 15.van der Wal MH, Jaarsma T. Adherence in heart failure in the elderly: problem and possible solutions. Int J Cardiol. 2008;125(2):203–8. doi: 10.1016/j.ijcard.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 16.Schnell-Hoehn KN, Naimark BJ, Tate RB. Determinants of self-care behaviors in community-dwelling patients with heart failure. J Cardiovasc Nurs. 2009;24(1):40–7. doi: 10.1097/01.JCN.0000317470.58048.7b. [DOI] [PubMed] [Google Scholar]
- 17.van der Wal MH, Jaarsma T, Moser DK, Veeger NJ, van Gilst WS, van Veldhuisen DJ. Compliance in heart failure patients: the importance of knowledge and beliefs. Eur Heart J. 2006;27(4):434–40. doi: 10.1093/eurheartj/ehi603. [DOI] [PubMed] [Google Scholar]
- 18.Tierney S, Mamas M, Woods S, Rutter MK, Gibson M, Neyses L, et al. What strategies are effective for exercise adherence in heart failure? A systematic review of controlled studies. Heart Fail Rev. 2012;17(1):107–15. doi: 10.1007/s10741-011-9252-4. [DOI] [PubMed] [Google Scholar]
- 19.Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006;25(4):510–20. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- 20.McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exerc Sport Sci Rev. 2000;28(2):85–8. [PubMed] [Google Scholar]
- 21.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 22.Foley L, Prapavessis H, Maddison R, Burke S, McGowan E, Gillanders L. Predicting physical activity intention and behavior in school-age children. Pediatr Exerc Sci. 2008;20(3):342–56. doi: 10.1123/pes.20.3.342. [DOI] [PubMed] [Google Scholar]
- 23.Carlson JJ, Norman GJ, Feltz DL, Franklin BA, Johnson JA, Locke SK. Self-efficacy, psychosocial factors, and exercise behavior in traditional versus modified cardiac rehabilitation. J Cardiopulm Rehabil. 2001;21(6):363–73. doi: 10.1097/00008483-200111000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Kaplan RM, Atkins CJ, Reinsch S. Specific efficacy expectations mediate exercise compliance in patients with COPD. Health Psychol. 1984;3(3):223–42. doi: 10.1037//0278-6133.3.3.223. [DOI] [PubMed] [Google Scholar]
- 25.Mishali M, Omer H, Heymann AD. The importance of measuring self-efficacy in patients with diabetes. Fam Pract. 2011;28(1):82–7. doi: 10.1093/fampra/cmq086. [DOI] [PubMed] [Google Scholar]
- 26.Jeng C, Braun LT. The influence of self-efficacy on exercise intensity, compliance rate and cardiac rehabilitation outcomes among coronary artery disease patients. Prog Cardiovasc Nurs. 1997;12(1):13–24. [PubMed] [Google Scholar]
- 27.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21. [PubMed] [Google Scholar]
- 28.Briffa TG, Maiorana A, Sheerin NJ, Stubbs AG, Oldenburg BF, Sammel NL, et al. Physical activity for people with cardiovascular disease: recommendations of the National Heart Foundation of Australia. Med J Aust. 2006;184(2):71–5. doi: 10.5694/j.1326-5377.2006.tb00121.x. [DOI] [PubMed] [Google Scholar]
- 29.Caldieraro-Bentley AJ, Andrews JO. An integrative review: application of self-efficacy instruments for walking in populations with peripheral arterial disease. J Vasc Nurs. 2013;31(3):118–30. doi: 10.1016/j.jvn.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Dunbar SB, Butts B, Reilly CM, Gary RA, Higgins MK, Ferranti EP, et al. A pilot test of an integrated self-care intervention for persons with heart failure and concomitant diabetes. Nurs Outlook. 2014;62(2):97–111. doi: 10.1016/j.outlook.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joekes K, Van ET, Schreurs K. Self-efficacy and overprotection are related to quality of life, psychological well-being and self-management in cardiac patients. J Health Psychol. 2007;12(1):4–16. doi: 10.1177/1359105306069096. [DOI] [PubMed] [Google Scholar]
- 32.Dontje ML, van der Wal MH, Stolk RP, Brugemann J, Jaarsma T, Wijtvliet PE, et al. Daily physical activity in stable heart failure patients. J Cardiovasc Nurs. 2014;29(3):218–26. doi: 10.1097/JCN.0b013e318283ba14. [DOI] [PubMed] [Google Scholar]
- 33.Klompstra LV, Jaarsma T, Stromberg A. An in-depth, longitudinal examination of the daily physical activity of a patient with heart failure using a Nintendo Wii at home: a case report. J Rehabil Med. 2013;45(6):599–602. doi: 10.2340/16501977-1151. [DOI] [PubMed] [Google Scholar]
- 34.Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013;19(2):77–84. doi: 10.1111/chf.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parish TR, Kosma M, Welsch MA. Exercise training for the patient with heart failure: Is your patient ready? Cardiopulm Phys Ther J. 2007;18(3):12–20. [Google Scholar]
- 36.Fu D, Fu H, McGowan P, Shen YE, Zhu L, Yang H, et al. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: randomized controlled trial. Bull World Health Organ. 2003;81(3):174–82. [PMC free article] [PubMed] [Google Scholar]
- 37.Frank AM, McConnell TR, Rawson ES, Fradkin A. Clinical and functional predictors of health-related quality of life during cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2011;31(4):223–9. doi: 10.1097/HCR.0b013e31820333b3. [DOI] [PubMed] [Google Scholar]
- 38.Tierney S, Elwers H, Sange C, Mamas M, Rutter MK, Gibson M, et al. What influences physical activity in people with heart failure?: a qualitative study. Int J Nurs Stud. 2011;48(10):1234–43. doi: 10.1016/j.ijnurstu.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 39.Sarkar U, Ali S, Whooley MA. Self-efficacy as a marker of cardiac function and predictor of heart failure hospitalization and mortality in patients with stable coronary heart disease: findings from the Heart and Soul Study. Health Psychol. 2009;28(2):166–73. doi: 10.1037/a0013146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Subramanian U, Hopp F, Mitchinson A, Lowery J. Impact of provider self-management education, patient self-efficacy, and health status on patient adherence in heart failure in a Veterans Administration population. Congest Heart Fail. 2008;14(1):6–11. doi: 10.1111/j.1751-7133.2008.07174.x. [DOI] [PubMed] [Google Scholar]
- 41.Lawson KL, Jonk Y, O'Connor H, Riise KS, Eisenberg DM, Kreitzer MJ. The impact of Telephonic Health Coaching on Health Outcomes in a High-risk Population. Glob Adv Health Med. 2013;2(3):40–7. doi: 10.7453/gahmj.2013.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rajati F, Mostafavi F, Sharifirad G, Sadeghi M, Tavakol K, Feizi A, et al. A theory-based exercise intervention in patients with heart failure: A protocol for randomized, controlled trial. J Res Med Sci. 2013;18(8):659–67. [PMC free article] [PubMed] [Google Scholar]
- 43.Du HY, Newton PJ, Zecchin R, Denniss R, Salamonson Y, Everett B, et al. An intervention to promote physical activity and self-management in people with stable chronic heart failure The Home-Heart-Walk study: study protocol for a randomized controlled trial. Trials. 2011;12:63. doi: 10.1186/1745-6215-12-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DeWalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, et al. Comparison of a one-time educational intervention to a teach-to-goal educational intervention for self-management of heart failure: design of a randomized controlled trial. BMC Health Serv Res. 2009;9:99. doi: 10.1186/1472-6963-9-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dougherty CM, Steele BG, Hunziker J. Testing an intervention to improve functional capability in advanced cardiopulmonary illness. J Cardiopulm Rehabil Prev. 2011;31(1):35–41. doi: 10.1097/HCR.0b013e3181f1fd77. [DOI] [PubMed] [Google Scholar]
- 46.Brodie DA, Inoue A. Motivational interviewing to promote physical activity for people with chronic heart failure. J Adv Nurs. 2005;50(5):518–27. doi: 10.1111/j.1365-2648.2005.03422.x. [DOI] [PubMed] [Google Scholar]
- 47.Brodie DA, Inoue A, Shaw DG. Motivational interviewing to change quality of life for people with chronic heart failure: a randomised controlled trial. Int J Nurs Stud. 2008;45(4):489–500. doi: 10.1016/j.ijnurstu.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 48.Pozehl B, Duncan K, Hertzog M, Norman JF. Heart Failure Exercise and Training Camp: effects of a multicomponent exercise training intervention in patients with heart failure. Heart Lung. 2010;39(6 Suppl):S1–13. doi: 10.1016/j.hrtlng.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Duncan K, Pozehl B. Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabil Nurs. 2003;28(4):117–22. doi: 10.1002/j.2048-7940.2003.tb01728.x. [DOI] [PubMed] [Google Scholar]
- 50.Barkley SA, Fahrenwald NL. Evaluation of an intervention to increase self-efficacy for independent exercise in cardiac rehabilitation. Behav Med. 2013;39(4):104–10. doi: 10.1080/08964289.2013.804804. [DOI] [PubMed] [Google Scholar]
- 51.Collins E, Langbein WE, Dilan-Koetje J, Bammert C, Hanson K, Reda D, et al. Effects of exercise training on aerobic capacity and quality of life in individuals with heart failure. Heart Lung. 2004;33(3):154–61. doi: 10.1016/j.hrtlng.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 52.Barnason S, Zimmerman L, Nieveen J, Schmaderer M, Carranza B, Reilly S. Impact of a home communication intervention for coronary artery bypass graft patients with ischemic heart failure on self-efficacy, coronary disease risk factor modification, and functioning. Heart Lung. 2003;32(3):147–58. doi: 10.1016/s0147-9563(03)00036-0. [DOI] [PubMed] [Google Scholar]
- 53.Smeulders ES, van Haastregt JC, Ambergen T, Janssen-Boyne JJ, van Eijk JT, Kempen GI. The impact of a self-management group programme on health behaviour and healthcare utilization among congestive heart failure patients. Eur J Heart Fail. 2009;11(6):609–16. doi: 10.1093/eurjhf/hfp047. [DOI] [PubMed] [Google Scholar]
- 54.Maddison R, Prapavessis H, Armstrong GP, Hill C. A modeling intervention in heart failure. Ann Behav Med. 2008;36(1):64–9. doi: 10.1007/s12160-008-9050-y. [DOI] [PubMed] [Google Scholar]
- 55.Yeh GY, Wayne PM, Phillips RS. T'ai Chi exercise in patients with chronic heart failure. Med Sport Sci. 2008;52:195–208. doi: 10.1159/000134300. [DOI] [PubMed] [Google Scholar]
- 56.Oka RK, DeMarco T, Haskell WL. Effect of treadmill testing and exercise training on self-efficacy in patients with heart failure. Eur J Cardiovasc Nurs. 2005;4(3):215–9. doi: 10.1016/j.ejcnurse.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 57.Booth ML, Owen N, Bauman A, Gore CJ. Relationship between a 14-day recall measure of leisure-time physical activity and a submaximal test of physical work capacity in a population sample of Australian adults. Res Q Exerc Sport. 1996;67(2):221–7. doi: 10.1080/02701367.1996.10607948. [DOI] [PubMed] [Google Scholar]
- 58.Leger L, Thivierge M. Heart rate monitors: validity, stability, and functionality. Physician and Sportsmedicine. 1988;16(5):143–8. doi: 10.1080/00913847.1988.11709511. [DOI] [PubMed] [Google Scholar]
- 59.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. doi: 10.1186/1471-2261-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smeulders ES, van Haastregt JC, van Hoef EF, van Eijk JT, Kempen GI. Evaluation of a self-management programme for congestive heart failure patients: design of a randomised controlled trial. BMC Health Serv Res. 2006;6:91. doi: 10.1186/1472-6963-6-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dolansky MA, Stepanczuk B, Charvat JM, Moore SM. Women's and men's exercise adherence after a cardiac event. Res Gerontol Nurs. 2010;3(1):30–8. doi: 10.3928/19404921-20090706-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bandura A. Social foundations of thought and action: a social cognitive theory. New York, NY: Prentice-Hall; 1986. [Google Scholar]
- 63.Jolly K, Taylor RS, Lip GY, Davies M, Davis R, Mant J, et al. A randomized trial of the addition of home-based exercise to specialist heart failure nurse care: the Birmingham Rehabilitation Uptake Maximisation study for patients with Congestive Heart Failure (BRUM-CHF) study. Eur J Heart Fail. 2009;11(2):205–13. doi: 10.1093/eurjhf/hfn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Piotrowicz E, Baranowski R, Bilinska M, Stepnowska M, Piotrowska M, Wojcik A, et al. A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail. 2010;12(2):164–71. doi: 10.1093/eurjhf/hfp181. [DOI] [PubMed] [Google Scholar]
- 65.Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol. 2010;15(Pt 2):265–88. doi: 10.1348/135910709X461752. [DOI] [PubMed] [Google Scholar]
- 66.Tierney S, Mamas M, Skelton D, Woods S, Rutter MK, Gibson M, et al. What can we learn from patients with heart failure about exercise adherence? A systematic review of qualitative papers. Health Psychol. 2011;30(4):401–10. doi: 10.1037/a0022848. [DOI] [PubMed] [Google Scholar]
- 67.Barbour KA, Miller NH. Adherence to exercise training in heart failure: a review. Heart Fail Rev. 2008;13(1):81–9. doi: 10.1007/s10741-007-9054-x. [DOI] [PubMed] [Google Scholar]
- 68.Bentsen SB, Wentzel-Larsen T, Henriksen AH, Rokne B, Wahl AK. Self-efficacy as a predictor of improvement in health status and overall quality of life in pulmonary rehabilitation--an exploratory study. Patient Educ Couns. 2010;81(1):5–13. doi: 10.1016/j.pec.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 69.Oka RK, Gortner SR, Stotts NA, Haskell WL. Predictors of physical activity in patients with chronic heart failure secondary to either ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1996;77(2):159–63. doi: 10.1016/s0002-9149(96)90588-3. [DOI] [PubMed] [Google Scholar]