Abstract
Background
Medication errors may occur during prescribing, transcribing, prescription auditing, preparing, dispensing, administration, and monitoring. Medication administration errors (MAEs) are those that actually reach patients and remain a threat to patient safety. The Joint Commission International (JCI) advocates medication error prevention, but experience in reducing MAEs during the period of before and after JCI accreditation has not been reported.
Methods
An intervention study, aimed at reducing MAEs in hospitalized patients, was performed in the Second Affiliated Hospital of Zhejiang University, Hangzhou, People’s Republic of China, during the journey to JCI accreditation and in the post-JCI accreditation era (first half-year of 2011 to first half-year of 2014). Comprehensive interventions included organizational, information technology, educational, and process optimization-based measures. Data mining was performed on MAEs derived from a compulsory electronic reporting system.
Results
The number of MAEs continuously decreased from 143 (first half-year of 2012) to 64 (first half-year of 2014), with a decrease in occurrence rate by 60.9% (0.338% versus 0.132%, P<0.05). The number of MAEs related to high-alert medications decreased from 32 (the second half-year of 2011) to 16 (the first half-year of 2014), with a decrease in occurrence rate by 57.9% (0.0787% versus 0.0331%, P<0.05). Omission was the top type of MAE during the first half-year of 2011 to the first half-year of 2014, with a decrease by 50% (40 cases versus 20 cases). Intravenous administration error was the top type of error regarding administration route, but it continuously decreased from 64 (first half-year of 2012) to 27 (first half-year of 2014). More experienced registered nurses made fewer medication errors. The number of MAEs in surgical wards was twice that in medicinal wards. Compared with non-intensive care units, the intensive care units exhibited higher occurrence rates of MAEs (1.81% versus 0.24%, P<0.001).
Conclusion
A 3-and-a-half-year intervention program on MAEs was confirmed to be effective. MAEs made by nursing staff can be reduced, but cannot be eliminated. The depth, breadth, and efficiency of multidiscipline collaboration among physicians, pharmacists, nurses, information engineers, and hospital administrators are pivotal to safety in medication administration. JCI accreditation may help health systems enhance the awareness and ability to prevent MAEs and achieve successful quality improvements.
Keywords: medication administration, medication errors, nurse, quality improvements
Introduction
Medication errors are ongoing problems among hospitalized patients and may occur during prescribing, transcribing, prescription auditing, preparing, dispensing, administration, and monitoring. Near misses are errors that happened but were captured before reaching the patient, whereas medication administration errors (MAEs) are those errors that actually reach patients and pose a threat to patient safety.1
Understanding MAEs is necessary because the identification of its determinants helps to undertake designed interventions. A systematic review by Keers et al showed that error-provoking conditions influencing MAEs included inadequate written communication (prescriptions, documentation, transcription); problems with medicine supply and storage (pharmacy dispensing errors and ward stock management); high perceived workload; problems with ward-based equipment (access, functionality); patient factors (availability, acuity); staff health status (fatigue, stress); and interruptions/distractions during drug administration.2 Data have shown that incorporating barcode verification technology within an electronic medication administration system substantially reduced the rate of errors in medication administration.3 A before–after study showed that educational sessions about good medication administration practices provided by a pharmacist was a very simple way to decrease MAE rates.4 Kim and Bates developed a checklist using basic medication administration guidelines; however, they found that it was not effective in reducing MAEs, indicating that more practical guidelines for medication administration should be made for clinical nurses to adhere to.5 Although interventions for reducing MAEs have been sporadically documented, comprehensive quality improvement programs on MAEs in large-scale hospitals are rarely available in the PubMed database.
The Joint Commission International (JCI) advocates the pursuit of continuous improvement in decreasing medication errors so as to enhance patient safety.6 We have illustrated the effectiveness of clinical interventions in reducing prescribing-related medication errors during the journey to JCI accreditation.7 However, literature about experiences in reducing MAEs during the periods before and after JCI accreditation has not been available. The Second Affiliated Hospital of Zhejiang University (SAHZU), Hangzhou, People’s Republic of China, successfully passed the JCI accreditation as an academic medical center hospital on February 24, 2013. A working group composed of nurses, pharmacists, information engineers, physicians, and administrators was established to implement multifaceted interventions at the individual, organizational, and policy levels to reduce MAEs during the journey to JCI accreditation and in the post-JCI accreditation era (first half-year of 2011 to first half-year of 2014). The aim of this article is to discuss the effectiveness of such stewardship intervention in inpatient care and provide some reference for international counterparts.
Methods
Data collection
A 3-and-half-year intervention program focusing on MAEs in inpatient nursing care was performed in SAHZU, a 3,200-bed hospital with 3.5 million outpatient visits and 90,000 discharged patients annually (data in 2013) in Zhejiang Province, People’s Republic of China, which has a population of approximately 54.4 million. MAEs made by nursing staff every half-year were derived from a compulsory electronic medication error reporting system in SAHZU during the period January 2011 to June 2014. Data mining was performed, focusing on types of MAEs, severity rating, high-alert medications involved, administration route, times of occurrence and identification of MAEs, ward distribution, and nurse qualification (ie, professional title, levels of nursing experience).
The sorting of professional title was as follows: senior nurse-in-charge > nurse practitioner > nurse. According to Benner’s novice to expert model,8 levels of nursing experience were as follows: N0= novice; N1= advanced beginner; N2= competent nurse; N3= proficient nurse; N4= expert nurse. Referencing the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) Index for Categorizing Medication Errors,9 SAHZU proposed four categories of MAEs, ie, type 1 errors (category C: errors occurred that reached the patient but did not cause patient harm); type 2 errors (category D: errors occurred that reached the patient and required monitoring to confirm that they resulted in no harm to the patient and/or required intervention to preclude harm); type 3 errors (category E to category F: errors occurred that may have contributed to or resulted in temporary harm to the patient and required intervention, initial or prolonged hospitalization); and type 4 errors (errors occurred that may have contributed to or resulted in permanent patient harm [category G], errors occurred that required intervention necessary to sustain life [category H], and errors occurred that may have contributed to or resulted in patient’s death [category I]).
The data presented in the study are available in the archives of the Drug and Therapeutics Committee (DTC) of SAHZU. Access and use of these data need permission from the SAHZU DTC.
Comprehensive intervention measures
Quality improvement tools
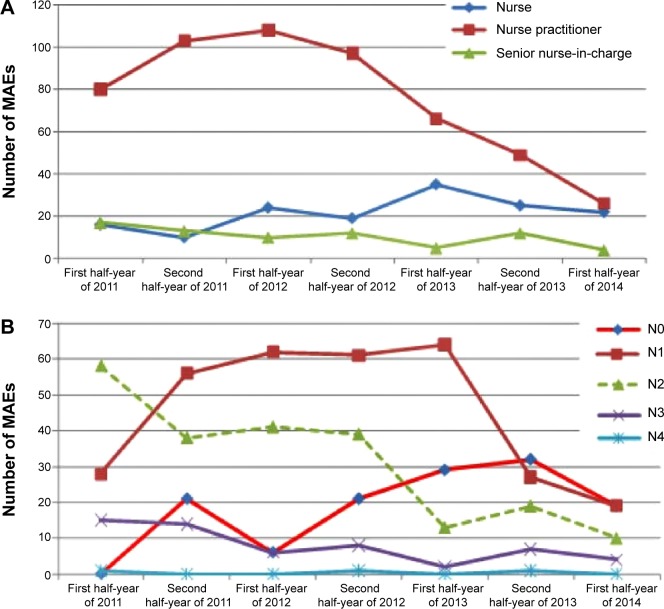
Quality improvement tools like plan–do–check–act, quality control circles (QCCs), and continuous quality improvement (CQI) were utilized. During 2011–2014, the Division of Nursing conducted 1,686 quality improvement programs, including 1,391 plan–do–check–acts, 207 QCCs, and 88 CQIs. There were 117 medication-related programs, among which 73 programs focused on prevention of MAEs (Figure 1).
Figure 1.
Medication- or MAE-related quality improvement programs during the period January 2011 to June 2014.
Abbreviations: MAE, medication administration error; PDCA, plan–do–check–action cycle; QCC, quality control circle; CQI, continuous quality improvement.
Meanwhile, the inpatient pharmacy also conducted many quality improvement programs, such as preventing near misses related to look-alike or sound-alike medications; enhancing medication management and use of high-alert medications; reducing the kinds and quantities of medications stored outside of the pharmacy; shortening the period of time from writing stat (ST) physician orders to medication administration; standardizing the rule associated with skin tests and contraindications concerning cross allergy;10,11 and promoting the awareness of rational nasogastric administration.12
Organizational measures
In 2011, the Committee of Quality and Safety Management affiliated with the Division of Nursing established the Section of Safe Medication Administration, which consisted of ten head nurses as core members. In the first half-year of 2012, a three-level stewardship mechanism was formed toward safe medication administration, including on-site inspections on medication management in wards by inpatient pharmacists every month (first level), self-evaluation by each nursing unit every half-year (second level), and auditing by the Section of Safe Medication Administration every year (third level). Also, SAHZU established 16 functional groups according to chapters of JCI accreditation standards in June 2011. The medication management and use group and the international patient safety goal group played important roles in quality improvements and patient safety. Medication safety meetings were held quarterly by the Division of Nursing, Pharmacy and Therapeutics Committee, and Office of Quality Management. Brainstorming and multidiscipline coordination meetings were held if necessary. All the meeting summaries were documented. In the beginning of 2013, a tracing mode was first introduced into medication management and use and nursing quality evaluation. Case tracing and systematic tracing were combined to enhance the awareness of patient safety among physicians, pharmacists, logistic workers, nursing staff, and information engineers, and to help administrators easily catch the systematic problems in health care for inpatients.
Information technology measures
The main information technology interventions related to MAEs were as follows:
Developing an electronic medication tracing system. Such a system was established in June 2011 and embedded into pharmacy management information and electronic nursing record systems. It provided a powerful tool for process management in handling physician orders because it was traceable regarding the time of prescribing, transcribing, prescription auditing, sterile admixing (for intravenous [IV] drugs), starting time of logistics delivery, the time of receiving medications by ward nursing staff, starting time of dosing, and end time of IV infusion. Regarding the efficiency of handling ST physician orders, in November 2011, each nursing unit was equipped with an audio device which would sound out the alarm “there are ST orders, please handle them immediately”. The alarm would sound again 1 minute later if nursing staff did not respond. The ST orders alarm would also sound in the inpatient pharmacy.
Developing an online query system of appearance (color, size, shape) of tablet or capsule. Such a platform was established in June 2011 and was a great help to nurses regarding checking medication or identifying the corresponding medications which were ordered but temporarily discontinued by the physician.
Developing web-based software for prescription screening and drug counseling. Such a system was introduced and embedded into the pharmacy management information system, the electronic medical record (EMR), and the electronic nursing record system in October 2011. Nurses can conveniently look up key points of medication knowledge through this software.
Developing a mode of unit dose labeling in accordance with JCI requirements. As of July 2012, each medication dispensed from the inpatient pharmacy had been accompanied with a unit dose label containing barcode, patient name, identification number, drug information (name, dose, route, frequency, time), and warnings (drip rate, stability, signs of high-alert medication identification, medications to be refrigerated, medications requiring light protection, medications requiring special types of infusion sets, and medications that increase fall risk).13–15
Developing a sophisticated interface for the pharmacy management information system for prescription auditing in accordance with JCI requirements. Such an interface was successfully established in January 2013. Since then, competent pharmacists could review physician orders based not only on information that had been already available as of the end of 2012 (ie, patient name, identification number, age, diagnosis, medication name, dose, administration route, and dose frequency), but also other key information (eg, current medications information, allergy history, body weight, body surface area, nutrition status, and clinical laboratory test results such as hepatic and renal function, international normalized ratio, blood routine examination, and serum drug levels).
Enhancing investments in information technology equipments for nursing care. SAHZU began to apply personal digital assistants (PDAs) and mobile nursing carts in some wards in June 2011. In the second half-year of 2012, every nursing unit was equipped with four to eight PDAs and three to four mobile nursing carts, with a total sum of 330 PDAs and 137 mobile nursing carts. The application of mobile nursing carts brought great convenience to nursing staff, while perfect medication label information in combination with barcode scanning prior to dosing was believed to enhance medication administration safety.
Process optimization-based measures
Process optimization in the inpatient pharmacy was as follows. 1) As of November 2010, a centralized IV admixture service was provided by the inpatient pharmacy to all wards except the intensive care unit (ICU), emergency ICU, and neurological ICU. In October 2012, the ICU, emergency ICU, and neurological ICU also obtained this service. 2) As of October 2012, zero storage of high-concentration electrolytes had been achieved outside of pharmacy and ready-to-use infusion bags of potassium chloride were provided by the inpatient pharmacy. 3) The unit dose dispensing mode was also strengthened for non-injectable medications. Two automated unit dose packaging machines for oral pills were installed in the inpatient pharmacy in January 2011. 4) The inpatient pharmacy started to provide 24-hour pharmaceutical care from the beginning of 2012.
Process optimization in each ward was as follows. 1) The change order of physician orders required timely printing and the checking process was standardized. The primary nurse had to check and sign the physician order within 1 hour after printing the change order. The signed change order was required to be kept for 3 months. 2) For sustained infusion via micro-pump, the primary nurse was required to administer the infusion to the patient according to the executing sheet of physician orders. Each shift nurse had to sign the executing sheet after checking the infusion label and infusion speed. 3) A standardized, independent double-check at the bedside was compulsory prior to administering special high-alert medications (ie, opioids, IV insulin, IV heparin, and chemotherapeutic agents) from the second half-year of 2012. Furthermore, a PDA was used to record identification information of the two operators during this process in case process traceability was warranted.
Intensified human resource management and educational measures
In 2013, 130 nursing job descriptions were revised. In evaluating individual nursing performance, the statistical weight of job performance was elevated by 40%. Human resources in each nursing unit were optimized. Each nursing unit was divided into two groups. Each group was allocated with a nursing group leader. It was arranged that each primary nurse would manage rooms in the same group for a consecutive 2 weeks. A good nursing qualification management was set up. An occupational development file was established for each nurse. The Division of Nursing strove to enhance the awareness of self-management among nursing staff and strengthen the personalized management plan. Multi-level training was organized for nursing staff with different levels of nursing experience according to Benner’s novice to expert model. From the beginning of 2013, the Division of Nursing arranged educational training for N0 (20 credit hours), N1 (20 credit hours), N2 (20 credit hours), N3 (21 credit hours), and other nursing staff (8 credit hours) annually. Physicians were given targeted training on how to give orders via EMR and attended a series of lectures on rational medication use, annually.
Outcome measures
The outcome measures included number of MAEs made by nurses; occurrence rate of MAEs (number of MAEs divided by number of discharged patients during the same period); number of MAEs related to high-alert medications; occurrence rate of MAEs related to high-alert medications (number of MAEs related to high-alert medications divided by number of discharged patients during the same period); occurrence rate of omission; trends of MAEs with different severity ratings; administration route; times of occurrence and identification of MAEs; and relative percentage of particular MAE subtypes.
Statistical analysis
A descriptive analysis was performed. Chi-square tests were used for testing occurrence rate differences between two groups using SPSS (v 13.0) software. Fisher’s exact test was used when two cells (50.0%) of a contingency table had an expected count less than 5. Pearson’s chi-square continuity correction was used when one cell (25.0%) had an expected count less than 5. Pearson’s chi-square was used when 0 cells (0.0%) had an expected count less than 5. A P-value <0.05 was considered to be statistically significant.
Results
Number and occurrence rate of MAEs
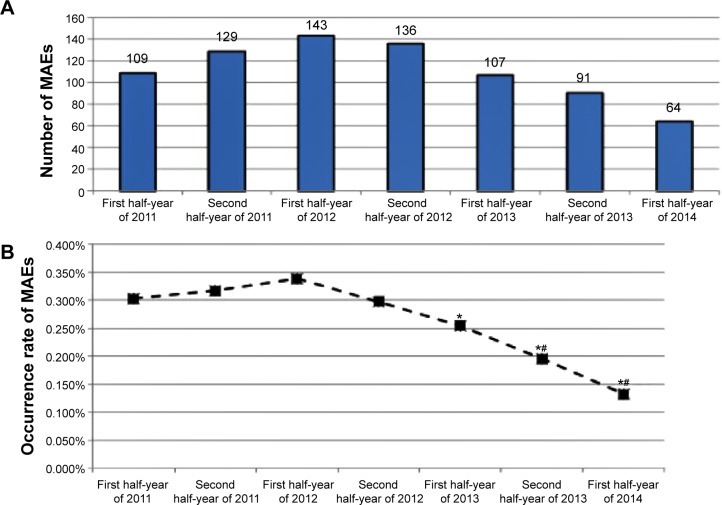
The number of MAEs exhibited an increasing trend during the first half-year of 2011 to the first half-year of 2012. However, there was no statistically significant difference in the occurrence rates of MAEs during this period (P>0.05). The number of MAEs made by nursing staff continuously decreased from 143 to 64 during the first half-year of 2012 to the first half-year of 2014. The number of discharged patients in SAHZU steadily increased from 35,920 (first half-year of 2011) to 48,397 (first half-year of 2014), whereas the occurrence rate of MAEs made by nursing staff decreased by 56.4% (0.303% [109/35,920] versus 0.132% [64/48,397]) (Figure 2).
Figure 2.
MAEs made by nursing staff during the period January 2011 to June 2014.
Notes: (A) Number of MAEs. (B) Occurrence rate of MAEs (%). *P<0.05 (compared with data in the first half-year of 2012); #P<0.05 (compared with data in the first half-year of 2011).
Abbreviation: MAEs, medication administration errors.
Types of MAEs
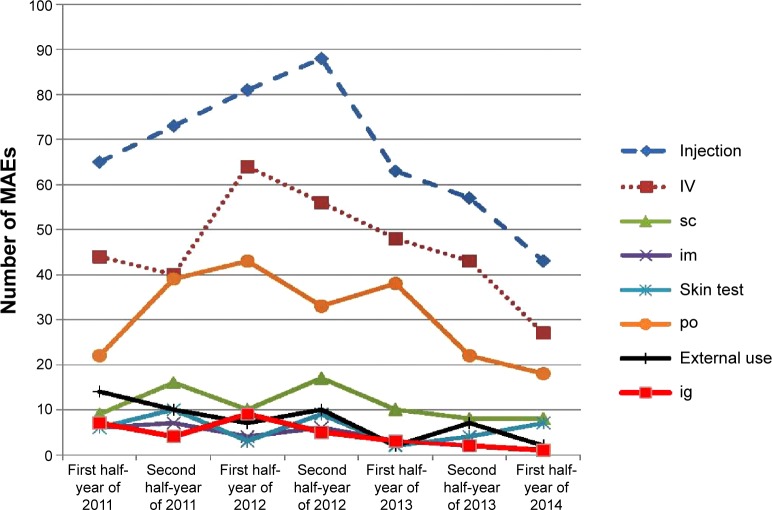
Omission accounted for 33.4% of all MAEs during 2011–2014, followed by wrong patient error (17.8%), preparation error (13.0%), dosing time error (9.2%), dose error (8.8%), nonadherence to the rule associated with skin tests and contraindications concerning cross allergy (7.4%), route error (3.5%), duplicate dosing (2.7%), speed (1.9%), improperly handling computerized physician orders prior to sending them to inpatient pharmacy (1.7%), and venous exosmosis (0.5%). The number of omissions decreased by 50% (40 cases versus 20 cases) between the first half-year of 2011 and the first half-year of 2014 (Table 1), and the occurrence rate of omission decreased by 62.9% (0.1114% [40/35,920] versus 0.0413% [20/48,397], P<0.05) in the same period. Improvements were also observed in medication preparation errors, wrong patient errors, dosing time errors, nonadherence to the rule associated with skin tests and contraindications concerning cross allergy, improper handling physician order, and venous exosmosis. However, wrong patient errors showed a rebounding trend during the first half-year of 2014. Regarding administration route, injection administration accounted for 60.3% (470/779) of all MAEs during 2011–2014, followed by oral administration (27.6% [215/779]), external use (6.7% [52/779]), and nasogastric administration (4.0% [31/779]). IV administration errors were the top error type (41.3% of total MAEs); however, this type of error dramatically decreased from 64 (first half-year of 2012) to 27 (first half-year of 2014) (Figure 3). Improvements were also observed with oral administration, nasogastric administration, external use, and intramuscular administration.
Table 1.
Subtypes of MAEs during the intervention program period
| Period | Subtype of MAEs
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Omission | Wrong patient error | Preparation error | Time error | Dose error | Nonadherence to the rule on skin tests and contraindications concerning cross allergy | Route error | Duplicate dosing | Speed error | Improperly handling computerized physician orders prior to sending them to inpatient pharmacy | Exosmosis | |
| First half-year of 2011 | 40 (0.11%) | 14 (0.039%) | 15 (0.042%) | 10 (0.028%) | 8 (0.022%) | 10 (0.028%) | 1 (0.003%) | 3 (0.008%) | 1 (0.003%) | 4 (0.011%) | 2 (0.006%) |
| Second half-year of 2011 | 31 (0.076%) | 23 (0.057%) | 16 (0.039%) | 12 (0.030%) | 11 (0.027%) | 14 (0.034%) | 7 (0.017%) | 4 (0.010%) | 3 (0.007%) | 3 (0.007%) | 2 (0.005%) |
| First half-year of 2012 | 44 (0.10%) | 30 (0.071%) | 19 (0.045%) | 14 (0.033%) | 12 (0.028%) | 8 (0.019%) | 1 (0.002%) | 6 (0.014%) | 3 (0.007%) | 5 (0.012%) | 0 (0%) |
| Second half-year of 2012 | 45 (0.099%) | 21 (0.046%) | 19 (0.042%) | 14 (0.031%) | 11 (0.024%) | 11 (0.024%) | 8 (0.018%) | 2 (0.004%) | 3 (0.007%) | 0 (0%) | 0 (0%) |
| First half-year of 2013 | 46 (0.11%) | 16 (0.038%) | 12 (0.029%) | 12 (0.029%) | 9 (0.021%) | 4 (0.010%) | 3 (0.007%) | 1 (0.002%) | 4 (0.010%) | 0 (0%) | 0 (0%) |
| Second half-year of 2013 | 31* (0.066%) | 13 (0.028%) | 14 (0.030%) | 7 (0.015%) | 13 (0.028%) | 4 (0.009%) | 5 (0.011%) | 0 (0%) | 1 (0.002%) | 1 (0.002%) | 0 (0%) |
| First half-year of 2014 | 20* (0.041%) | 20 (0.041%) | 5 (0.010%) | 2 (0.004%) | 4 (0.008%) | 6 (0.012%) | 2 (0.004%) | 5 (0.010%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Sum | 257 | 137 | 100 | 71 | 68 | 57 | 27 | 21 | 15 | 13 | 4 |
Notes: Data are presented as absolute number of a subtype of MAE (its occurrence rate, ie, number of this subtype’s MAEs divided by number of discharged patients during the same period).
P<0.05 (versus first half-year of 2011).
Abbreviation: MAEs, medication administration errors.
Figure 3.
Administration route and MAEs during the period January 2011 to June 2014.
Abbreviations: MAEs, medication administration errors; IV, intravenous administration; sc, subcutaneous administration; im, intramuscular administration; po, oral administration; ig, nasogastric administration.
Severity ratings of MAEs
There were no type 4 errors during 2011–2014. Type 2 errors accounted for the largest proportion (88.96% [693/779]) of all MAEs during 2011–2014, followed by type 1 errors (8.98% [70/779]) and type 3 errors (2.05% [16/779]). The number of type 2 errors exhibited an increasing trend from the first half-year of 2011 to the first half-year of 2012. However, there was no statistically significant difference in the occurrence rates of type 2 errors during this period (P>0.05). The number of type 2 errors continuously decreased from 133 (first half-year of 2012) to 53 (first half-year of 2014), with a statistically significant change in the occurrence rate (0.3148% [133/42,252] versus 0.1095% [53/48,397], P<0.05) (Figure 4).
Figure 4.
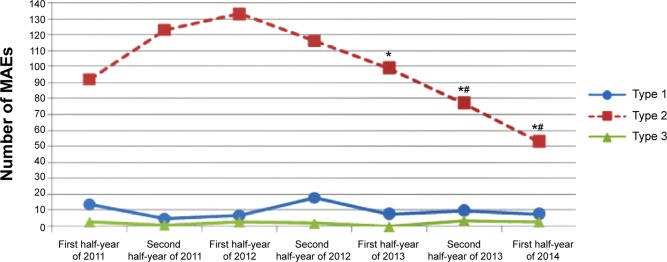
Number of MAEs according to error severity rating.
Notes: Type 1: errors occurred that reached the patient but did not cause patient harm. Type 2: errors occurred that reached the patient and required monitoring to confirm that they resulted in no harm to the patient and/or required intervention to preclude harm. Type 3: errors occurred that may have contributed to or resulted in temporary harm to the patient and required intervention, initial or prolonged hospitalization. *P<0.05 (compared with data in the first half-year of 2012); #P<0.05 (compared with data in the first half-year of 2011).
Abbreviation: MAEs, medication administration errors.
MAEs related to high-alert medications
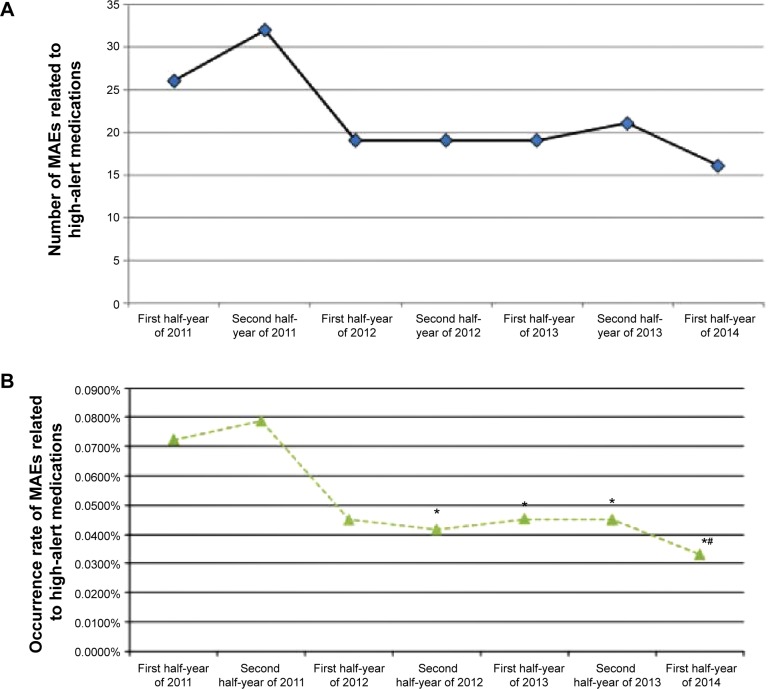
With respect to high-alert medications, the number of MAEs made by nursing staff decreased from 32 (second half-year of 2011) to 16 (first half-year of 2014), and the occurrence rate of MAEs decreased by 57.9% (0.0787% [32/40,670] versus 0.0331% [16/48,397], P<0.05) (Figure 5).
Figure 5.
MAEs associated with high-alert medications during the period January 2011 to June 2014.
Notes: (A) Number of MAEs associated with high-alert medications. (B) Occurrence rate of MAEs related to high-alert medications (%). *P<0.05 (compared with data in the second half-year of 2011); #P<0.05 (compared with data in the first half-year of 2011).
Abbreviation: MAEs, medication administration errors.
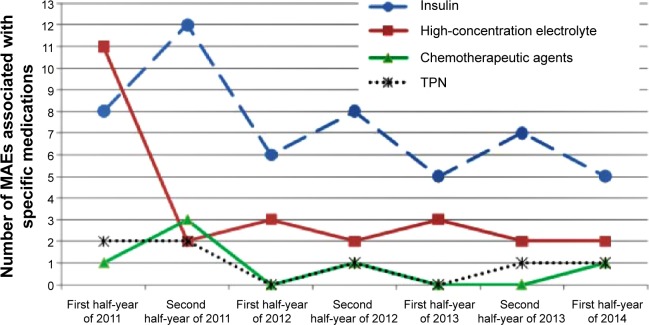
The involved high-alert medications included insulin, oral hypoglycemic drugs, high-concentration electrolyte (eg, 10% potassium chloride, 10% sodium chloride), total parenteral nutrition, contrast agents, anticoagulants, chemotherapeutic agents, opioids/psychotropic drugs, adrenergic agonists, aminophylline, and IV antiarrhythmics. Overall, improvements were observed for four types of high-alert medications (ie, insulin, high-concentration electrolyte, chemotherapeutic agents, and total parenteral nutrition) (Figure 6).
Figure 6.
MAEs associated with four categories of high-alert medications during the period January 2011 to June 2014.
Abbreviations: MAEs, medication administration errors; TPN, total parenteral nutrition.
Identification time of MAEs
A moderate increase was observed in the percentage of MAEs identified within 5 minutes, 30 minutes, 1 hour, 2 hours, and 12 hours from the second half-year of 2012. Only about 8.1%–14.7% (median: 9.8%) of MAEs were identified within 5 minutes; 16.9%–27.1% (median: 22%) of MAEs were identified within 30 minutes; 22.4%–36.4% (median: 30.1%) of MAEs were identified within 1 hour; and 4.7%–15.4% (median: 13.2%) of MAEs were identified 24 hours after administration.
Occurrence time of MAEs
MAEs between 8 am and 6 pm accounted for 47%–69% (median: 64%) of all MAEs. Occurrence of MAEs between 8 am and 6 pm, but not between 6 pm and 8 am (next day), exhibited a significant continuous decrease from the first half-year of 2012 (0.2319% [98/42,252] versus 0.0847% [(41/48,397], first half-year of 2012 versus first half-year of 2014, respectively, P<0.05). The number of MAEs between 6 pm and 8 am (next day) reduced by 50% during the first half-year of 2014, and the corresponding occurrence rate of MAEs fell from 0.1008% (47/46,622) to 0.0475% (23/48,397) (P<0.05).
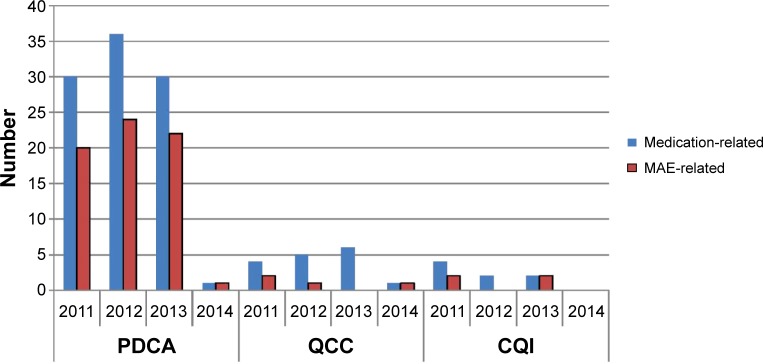
MAEs according to nurse qualification
Nurse practitioners were the largest population (about 80%) of nursing staff administering medications. The majority of MAEs during 2011–2014 were made by nurse practitioners (67.9% [529/779]), followed by nurses (19.4% [151/779]) and senior nurses-in-chief (9.4% [73/779]). A clear continuous decrease in the number of MAEs was observed among nurse practitioners (108 versus 26, second half-year of 2012 versus first half-year of 2014, respectively). N1 nurses accounted for the largest proportion of MAEs during 2011–2014 (43.0% [317/737]), followed by N2 (29.6% [218/737]), N0 (17.4% [128/737]), N3 (7.6% [56/737]), and N4 (0.4% [3/737]) nurses. N2 nurses accounted for 55% of MAEs in the first half-year of 2011 and a continuous decrease in MAEs was observed from then on. N1 nurses became the main population to make MAEs during the second half-year of 2011 to the first half-year of 2013. The relative percentage of MAEs made by N0 nurses increased from 5% to 37% during the first half-year of 2012 to the first half-year of 2014. The number of MAEs made by N3 nurses continuously decreased from 15 to four, and the number of MAEs made by N4 nurses was not more than one during 2011–2014 (Figure 7). The sequence of relative percentage of MAEs seemed reasonable in the second half-year of 2013 (N0 [36.0%] > N1 [30.3%] > N2 [21.3%] > N3 [7.9%] > N4 [1.1%]) and first half-year of 2014 (N0 [36.5%] > N1 [36.5%] > N2 [19.2%] > N3 [7.7%] > N4 [0%]), which indicated that more experienced registered nurses made fewer medication errors.
Figure 7.
Nurse qualification and MAEs during the period January 2011 to June 2014.
Notes: (A) MAEs made by nursing staff with different professional titles. The sorting of professional titles was as follows: senior nurses-in-charge > nurse practitioner > nurse. (B) MAEs made by personnel with different levels of nursing experience according to Benner’s novice to expert model:8 N0= novice; N1= advanced beginner; N2= competent nurse; N3= proficient nurse; N4= expert nurse.
Abbreviation: MAEs, medication administration errors.
Ward distribution
ICU wards accounted for 7.4% (58/779) of all MAEs during 2011–2014. A statistically significant difference was observed in the occurrence rates of MAEs in ICU and non-ICU wards (1.81% [58/3,196] versus 0.24% [721/298,280], P<0.001). Compared with non-ICU wards, ICU wards exhibited higher occurrence rates of subtypes of MAEs including omission, dose error, speed error, preparation error, wrong patient error, route error, dosing time error, type 1 error, type 2 error, and type 3 error (ICU > non-ICU, P<0.05) (Table 2). The ratio of number of MAEs in surgical wards versus medicinal wards was 1.89 (472/249), similar to the ratio of number of discharged patients in surgical wards versus medicinal wards, indicating no difference in occurrence of MAEs between surgical wards and medicinal wards (P>0.05). However, compared with medicinal wards, surgical wards exhibited a more obvious decrease in the absolute number of MAEs (88 to 41 [surgical] versus 45 to 20 [medicinal]) from the first half-year of 2012 to the first half-year of 2014.
Table 2.
Comparison of MAE subtypes in ICU and non-ICU wards during 2011 to the first half-year of 2014
| ICU
|
Non-ICU
|
P | |||
|---|---|---|---|---|---|
| Number | Occurrence rate (%) | Number | Occurrence rate (%) | ||
| Number of discharged patients (n) | 3,196 | 298,280 | |||
| Subtypes of MAEs | |||||
| Improper handling physician order | 0 | 0 | 14 | 0.00469 | |
| Nonadherence to the rule associated with skin tests and contraindications concerning cross allergy | 2 | 0.0625 | 56 | 0.0188 | 0.256a |
| Venous exosmosis | 1 | 0.0313 | 3 | 0.00101 | 0.042b |
| Omission | 19 | 0.594 | 239 | 0.0801 | <0.001a |
| Dose error | 10 | 0.313 | 59 | 0.0198 | <0.001a |
| Speed error | 2 | 0.0626 | 14 | 0.00469 | 0.001a |
| Preparation error | 4 | 0.125 | 95 | 0.0318 | 0.016a |
| Wrong patient error | 8 | 0.250 | 132 | 0.0443 | <0.001a |
| Route error | 4 | 0.125 | 23 | 0.00771 | <0.001a |
| Dosing time error | 7 | 0.219 | 64 | 0.0214 | <0.001a |
| Duplicate dosing | 1 | 0.0313 | 20 | 0.00671 | 0.554a |
| MAE severity ratings | |||||
| Type 1 errors | 8 | 0.250 | 63 | 0.0211 | <0.001a |
| Type 2 errors | 47 | 1.471 | 646 | 0.216 | <0.001c |
| Type 3 errors | 3 | 0.0939 | 13 | 0.00436 | <0.001a |
| Total number of MAEs | 58 | 1.815 | 721 | 0.241 | <0.001c |
Notes:
Pearson’s chi-square continuity correction test
Fisher’s exact test
Pearson’s chi-square test. Type 1 errors: errors occurred that reached the patient but did not cause patient harm. Type 2 errors: errors occurred that reached the patient and required monitoring to confirm that they resulted in no harm to the patient and/or required intervention to preclude harm. Type 3 errors: errors occurred that may have contributed to or resulted in temporary harm to the patient and required intervention, initial or prolonged hospitalization.
Abbreviations: MAEs, medication administration errors; ICU, intensive care unit.
Discussion
The number of MAEs exhibited an increasing trend in the first year after the initiation of intervention. However, there was no statistically significant difference in the occurrence rates of MAEs during this period. The explanation for this phenomenon may be that the previous intervention effectiveness was offset by three factors. The first factor was an unusual recruitment scale. In August 2011, 288 fresh nurses were recruited by the Division of Nursing, which was different from the usual scale (ie, 200 fresh nurses annually). These novices were more susceptible to making MAEs during training (half or full year) than after training. The second factor was the implementation of a new policy that all ward beds should be coordinated and managed by a special center from the beginning of 2012. Cross-discipline admission was encouraged for the sake of better bed turnover and operating efficiency. Ward nurses may have been unfamiliar with special medications given to the cross-discipline-admitted patients. The third factor was the low coverage of PDAs in wards before August 2012.
Because nursing staff are the last personnel who deal with medications prior to drug administration, it is assumed that prevention of near misses made by nursing staff will help reduce MAEs. In 2011, two programs were implemented in SAHZU to decrease near misses made by nursing staff. The Neurosurgery ward 1 had seven MAEs during the first half-year of 2011, so this ward conducted a QCC during the period July to November 2011. After intervention, near misses successfully decreased, from 17 cases per week to five cases per week. The oral surgery ward initiated a CQI to decrease IV medication-related near misses by nursing staff in June 2011. After 6 months, near misses in the oral surgery ward successfully decreased, from ten cases per week to 0.5 cases per week. We are not certain of the exact number of near misses made by nursing staff in SAHZU (the above numbers are estimates), because such near misses are rarely found in the voluntary reporting system; as such, we are not able to investigate the association of MAEs and near misses made by nurses in this study. SAHZU is attempting to achieve further improvements by encouraging nursing staff to report their near misses.
Wrong time, omission, and wrong dosage were the most frequently reported MAEs.16 However, omission, wrong patient error, and preparation error were the top three subtypes of MAEs in our study. Dosing time error and wrong dose error took the fourth and fifth position, respectively. “Right patient” is one of the international patient safety goals in the JCI accreditation standards. SAHZU requires staff to confirm a patient’s identity by checking the patient’s name and medical record number. Each patient has a unique medical record number. Barcode scanning can replace the process of checking the medical record number. The continuous decrease in wrong patient errors may be due to the strengthened on-site inspection since the second half-year of 2012.
It is also assumed that the implementation rate of bar-code scanning with PDAs is pivotal to correct medication administration. In the second quarter of 2012, the rate of barcode scanning prior to medication administration was only 50%; however, it showed an increasing trend during 2012–2014 through enhanced educational training, regular maintenance of PDAs, wireless signal improvements, the release of standard operation procedures for using PDAs, and on-site inspections. The implementation rate in the second quarter of 2013 was statistically higher than that in the second quarter of 2012 (76.7% versus 50%, P<0.05). Furthermore, the data in the third quarter of 2013 were more optimistic than those in the second quarter of 2013 (87.4% versus 76.7%, P<0.05).
Working environment improvements seemed helpful in reducing MAEs between 8 am and 6 pm. In the beginning of 2012, a standard operation procedure was formulated to strengthen management of guests visiting inpatients because noise and unnecessary counseling from these guests would bring too much interference to nurses when nurses were administering medications to patients. Under this procedure, a person accompanying an inpatient should have a special certificate signed by the head nurse of the ward. During visiting times (ie, 10 am to 12 pm, 2 pm to 9 pm), each inpatient should not be accompanied by more than two visiting guests and the visit time should not exceed 40 minutes. This intervention measure may partly explain the phenomenon that occurrence of MAEs between 8 am and 6 pm, but not between 6 pm and 8 am (next day), exhibited a significant continuous decrease from the first half-year of 2012.
ICU wards accounted for 7.4% of all MAEs during 2011–2014, similar to the data reported by Latif et al (6.6%).17 A cross-sectional study showed that, compared with non-ICU settings, ICU errors were more likely to be associated with any harm (odds ratio 1.89), permanent harm (odds ratio 2.45), harm requiring life-sustaining intervention (odds ratio 2.91), or death (odds ratio 2.48).17 In our study, no category G to category I incidents occurred during 2011–2014. However, compared with non-ICU wards, ICU wards exhibited higher occurrence rates of omission, dose error, speed error, preparation error, wrong patient error, route error, dosing time error, type 1 error, type 2 error, and type 3 error. Kaushal et al reported that a full-time unit-based clinical pharmacist could substantially decrease the rate of serious medication errors at all stages of the medication-use process by 79% in a pediatric ICU, whereas a part-time pharmacist was not as effective in general-care pediatric units.18 The results of our study and the studies of Latif et al17 and Kaushal et al18 strongly indicate that it is very necessary to allocate full-time clinical pharmacists in ICUs. SAHZU has had a clinical pharmacist in the general ICU since April 2012. However, clinical pharmacists have not participated in other ICU wards, including emergency ICU, surgery ICU, and neurosurgery ICU. It is necessary to train more clinical pharmacy specialists in the future. Further study is needed to investigate the role of full-time clinical pharmacists in reducing MAEs in ICUs.
A systematic review by Keers et al showed that reductions in MAE rates could be achieved by automated drug dispensing, computerized physician order entry, barcode-assisted medication administration with electronic administration records, nursing education/training using simulation, and clinical pharmacist-led training.19 The results of our study support the finding of Keers et al. Furthermore, our study also reveals that MAEs made by nurses reflect the level of pharmacy administration and hospital information infrastructure and that it is essential to apply quality improvement tools, take organizational measures, and implement process optimization.
During the journey to JCI accreditation, SAHZU has established a process to identify and to report medication errors and near misses. The process includes defining a medication error and near miss, using a standardized format for reporting, and educating staff on the process and importance of reporting. Definitions and processes are developed through a collaborative process that includes all those involved in the different steps in medication management. All SAHZU staff are encouraged to anonymously report near misses via an online, voluntary, no-fault reporting system. The identity of the staff who reports a near miss is only known by the Office of Quality Management, and the staff will be rewarded with 20 renminbi per case. As we are reminded by Stefl, “To err is human”.20 “Blame” should not be directed to an individual when other factors likely contribute to errors. Therefore, the personnel who make near misses will not be blamed or punished. Regarding MAEs, the Division of Nursing established a special online, compulsory, real-name MAE reporting system, and all MAEs must be reported via this system. A culture of quality has been instilled in the heart of each nursing staff. If an MAE is concealed and not reported, the involved staff, head nurse, and nursing unit will suffer severe punishment, such as informed criticism and cancelation of participation qualifications for the annual zero-defect award in nursing practice. On the contrary, no punishment or blame will be inflicted on nursing staff if an MAE is honestly reported. The reporting process has become a part of the organization’s quality and patient safety program. The reports are directed to one or more individuals who are accountable for taking action. The program focuses on preventing medication errors through understanding the types of errors and why near misses occur. Interestingly, we observed a phenomenon in our study, ie, more near misses are made by other staff (physicians, pharmacists, information engineers, and logistic workers) and fewer MAEs are made by nursing staff. The percentage of MAEs on such near misses was 7.65% (279/3,645) in 2012. This indicator was 4.38% (198/4,521) in 2013 and reduced to 1.95% (64/3,275) in the first half-year of 2014. Further study is necessary to confirm the association of MAEs made by nursing staff and near misses made by other staff.
With respect to the fact that numbers of discharged patients were enormously increased during the first half-year of 2011 to the first half-year of 2014, we would like to explain this phenomenon. 1) SAHZU has two campuses. Jiefang Campus, established in 1869, had 2,300 beds in 2013. In May 2013, SAHZU established the Binjiang Campus, with 900 beds. The two campuses are managed by the same chief executive officer. The addition of Binjiang Campus made SAHZU a 3,200-bed hospital. 2) SAHZU has significantly shortened the average hospitalization time from 9.7 days (2011 data) to 7.8 days (2014 data) and increased the bed turnover of inpatients in recent years. In our opinion, it is JCI accreditation that helps SAHZU enhance the awareness and ability to prevent medication errors and achieve successful quality improvements despite rapid expansion of the scale of the hospital.
The limitations of our study include the following. First, we did not quantitatively investigate the association of the number of MAEs with the number of doses administered. In SAHZU, nurse practitioners are the largest population (about 80%) of nursing staff administering medications, and they are also the majority of nursing staff (67.9%) who make the most MAEs. This indicates that the risk of making MAEs might be higher with a greater number of doses administered by a nursing staff member. However, further study is needed to address this issue.
Second, changes in patient case mix could have interfered with the MAE reduction, considering that numbers of discharged patients were enormously increased during the first half-year of 2011 to the first half-year of 2014. Although the case mix index in SAHZU has been stable, at 0.99–1.03, in recent years, it is absolutely underestimated. The concepts of case mix and diagnosis-related groups were newly introduced in the People’s Republic of China in recent years. The first page of a patient’s EMR is directly transferred to the National Health and Family Planning Commission of the People’s Republic of China, which publishes the case mix index of each hospital. Many physicians often forget to input secondary diagnoses in the first page of a EMR, so their hospital will get a low case mix index. There is a long way to go toward applying the case mix index to evaluate the medical level of a Chinese hospital.21 Currently, we are not able to present the “real” case mix index that truly reflects the severity and complexity of disease treated by SAHZU, a comprehensive large-scale academic medical center ranked in the top 20 in eleven of the 27 specialty areas in the People’s Republic of China, including burn care, cardiology, cancer, dermatology, emergency medicine, general surgery, neurology, neurosurgery, orthopedics, ophthalmology, pulmonary medicine, and nursing. The relationship of case mix and occurrence of MAEs was not addressed in this study, and further study is needed to address this question.
Third, although we presented an excellent example of how to correctly implement a patient-safety policy in a complex hospital by addressing multiple factors influencing the occurrence of medication errors, we only performed a trend analysis during the journey to JCI accreditation and in the post-JCI accreditation era (first half-year of 2011 to first half-year of 2014) and could not clearly define the first phase (ie, before intervention) and the second phase (ie, after intervention) and conduct strict comparison of the two phases. Multicenter study may be necessary to compare MAE occurrence in JCI-accredited hospitals versus non- JCI-accredited hospitals.
Conclusion
In this article, we summarized the experience of SAHZU in reducing MAEs during the journey to JCI accreditation and in the post-JCI accreditation era. A 3-and-a-half-year intervention program on MAEs was confirmed to be effective. MAEs made by nursing staff could not be eliminated; however, they could be reduced. The depth, breadth, and efficiency of multidiscipline collaboration among physicians, pharmacists, nurses, information engineers, and hospital administrators are pivotal to safety in medication administration. JCI accreditation may help health systems enhance the awareness and ability to prevent MAEs and achieve successful quality improvements.
Acknowledgments
This work was supported by the Zhejiang Provincial Bureau of Education (grant N20140209), Zhejiang Provincial Bureau of Health (number 2012KYA090 and 2013KYB137), Zhejiang Provincial Bureau of Traditional Chinese Medicine (number 2011ZB075), and National Health and Family Planning Commission of the People’s Republic of China (National Key Clinical Discipline Construction: Clinical Nursing Specialist). Also, we would like to thank Miss Na Lv, Professor Xiao-na Dai, Mr Sheng-dong Pan, and Mr Dong Cai for their kind help in the process of data collecting.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Haw C, Stubbs J, Dickens GL. Barriers to the reporting of medication administration errors and near misses: an interview study of nurses at a psychiatric hospital. J Psychiatr Ment Health Nurs. 2014;21(9):797–805. doi: 10.1111/jpm.12143. [DOI] [PubMed] [Google Scholar]
- 2.Keers RN, Williams SD, Cooke J, Ashcroft DM. Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf. 2013;36(11):1045–1067. doi: 10.1007/s40264-013-0090-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poon EG, Keohane CA, Yoon CS, et al. Effect of bar-code technology on the safety of medication administration. N Engl J Med. 2010;362(18):1698–1707. doi: 10.1056/NEJMsa0907115. [DOI] [PubMed] [Google Scholar]
- 4.Verrue CL, Mehuys E, Somers A, Van Maele G, Remon JP, Petrovic M. Medication administration in nursing homes: pharmacists’ contribution to error prevention. J Am Med Dir Assoc. 2010;11(4):275–283. doi: 10.1016/j.jamda.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 5.Kim J, Bates DW. Medication administration errors by nurses: adherence to guidelines. J Clin Nurs. 2013;22(3–4):590–598. doi: 10.1111/j.1365-2702.2012.04344.x. [DOI] [PubMed] [Google Scholar]
- 6.Joint Commission International Accreditation Standards for Hospitals. 5th ed. Oak Brook, IL: Joint Commission Resources; 2013. [Google Scholar]
- 7.Zhu LL, Zhou Q. Intervention for improving the appropriateness of physician orders for oral medications in geriatric VIP patients during the journey to JCI accreditation. Ther Clin Risk Manag. 2013;9:273–275. doi: 10.2147/TCRM.S46733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benner P. From novice to expert. Am J Nurs. 1982;82(3):402–407. [PubMed] [Google Scholar]
- 9.Cousins DD, Heath WM. The National Coordinating Council for Medication Error Reporting and Prevention: promoting patient safety and quality through innovation and leadership. Jt Comm J Qual Patient Saf. 2008;34:700–702. doi: 10.1016/s1553-7250(08)34091-4. [DOI] [PubMed] [Google Scholar]
- 10.Li W, Zhu LL, Zhou Q. Safe medication use based on knowledge of information about contraindications concerning cross allergy and comprehensive clinical intervention. Ther Clin Risk Manag. 2013;9:65–72. doi: 10.2147/TCRM.S42013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu LL, Song P, Zhou Q. A pragmatic approach to β-lactam use in patients with penicillin allergy. Allergy Asthma Proc. 2013;34(2):193. doi: 10.2500/aap.2013.34.3649. [DOI] [PubMed] [Google Scholar]
- 12.Zhu LL, Xu LC, Wang HQ, Jin JF, Wang HF, Zhou Q. Appropriateness of administration of nasogastric medication and preliminary intervention. Ther Clin Risk Manag. 2012;8:393–401. doi: 10.2147/TCRM.S37785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lan MJ, Zhu LL, Zhou Q. Medication administration errors made by nurses reflect the level of pharmacy administration and hospital information infrastructure. J Clin Nurs. 2014;23(5–6):894–895. doi: 10.1111/jocn.12495. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Zhu LL, Zhou Q. Effects of drug pharmacokinetic/pharmacodynamic properties, characteristics of medication use, and relevant pharmacological interventions on fall risk in elderly patients. Ther Clin Risk Manag. 2014;10:437–448. doi: 10.2147/TCRM.S63756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu LL, Li W, Song P, Zhou Q. Injection device-related risk management toward safe administration of medications: experience in a university teaching hospital in The People’s Republic of China. Ther Clin Risk Manag. 2014;10:165–172. doi: 10.2147/TCRM.S59199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keers RN, Williams SD, Cooke J, Ashcroft DM. Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother. 2013;47(2):237–256. doi: 10.1345/aph.1R147. [DOI] [PubMed] [Google Scholar]
- 17.Latif A, Rawat N, Pustavoitau A, Pronovost PJ, Pham JC. National study on the distribution, causes, and consequences of voluntarily reported medication errors between the ICU and non-ICU settings. Crit Care Med. 2013;41(2):389–398. doi: 10.1097/CCM.0b013e318274156a. [DOI] [PubMed] [Google Scholar]
- 18.Kaushal R, Bates DW, Abramson EL, Soukup JR, Goldmann DA. Unit-based clinical pharmacists’ prevention of serious medication errors in pediatric inpatients. Am J Health Syst Pharm. 2008;65(13):1254–1260. doi: 10.2146/ajhp070522. [DOI] [PubMed] [Google Scholar]
- 19.Keers RN, Williams SD, Cooke J, Walsh T, Ashcroft DM. Impact of interventions designed to reduce medication administration errors in hospitals: a systematic review. Drug Saf. 2014;37(5):317–332. doi: 10.1007/s40264-014-0152-0. [DOI] [PubMed] [Google Scholar]
- 20.Stefl ME. To err is human: building a safer health system in 1999. Front Health Serv Manage. 2001;18(1):1–2. [PubMed] [Google Scholar]
- 21.Jian WY, Lu M, Cui T, Hu M. Evaluating performance of local case-mix system by international comparison: a case study in Beijing, China. Int J Health Plann Manage. 2011;26(4):471–481. doi: 10.1002/hpm.1111. [DOI] [PubMed] [Google Scholar]