Abstract
Background/Aims
Patellar instability limits activity and promotes arthritis. Correcting genu valgum with selective hemiepiphyseodesis can treat patellar instability.
Methods
We retrospectively reviewed 26 knees with patellar instability and associated genu valgum that underwent hemiepiphyseodesis.
Results
Average anatomic lateral distal femoral angle (aLDFA) significantly corrected. Symptoms improved in all patients. All competitive athletes returned to sports. One complication occurred.
Conclusions
In genu valgum, the patella seeks an abnormal mechanical axis, resulting in patellar instability. By correcting the mechanical axis with hemiepiphyseodesis, patellar instability symptoms improve and patients return to sports. Complications are rare. Selective hemiepiphyseodesis is recommended when treating patellar instability with associated genu valgum.
Keywords: Patellar instability, Genu valgum, Epiphyseodesis, Guided growth
1. Introduction
Patellar instability, including patellar subluxation and dislocation, is a condition often encountered in children and adolescents. Lateral patellar subluxation or dislocation is the most common instability pattern and is often associated with genu valgum.1 Genu valgum can be defined both clinically and radiographically. Clinically, genu valgum is characterized by an intermalleolar distance greater than 8 cm and a tibiofemoral angle greater than 15°.2, 3 Radiographically, genu valgum is characterized by an anatomic lateral distal femoral angle (aLDFA) <79°, an anatomic medial proximal tibial angle >90°, and a mechanical axis line that passes through the lateral half of the knee joint.4 As knee valgus increases, the stresses at the lateral patellofemoral joint increase5 and this can lead to patellofemoral pain and instability. Additionally, increased lateral patellofemoral joint contact pressures can lead to degenerative changes over time.1
Historically, the mainstay of treating lateral patellar instability has been non-operative, including activity modification, physical therapy for quadriceps stretching and strengthening, and bracing.6 In the setting of genu valgum, this approach often fails, necessitating surgical management. Traditionally, surgical treatment of patellar instability has focused on realignment of the extensor mechanism. Several procedures have been described, but none has been uniformly successful in preventing recurrence of patellar instability. Reported unsatisfactory results range from 20% to 80%.7 Furthermore, these procedures are invasive, have high complication rates and require extensive rehabilitation.8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20
Selective hemiepiphyseodesis, where one or more physes are surgically closed at the medial distal femur or the proximal tibia, is a well described and accepted treatment for correcting primary and secondary genu valgum in pediatric patients.21, 22, 23, 24 This technique can restore or improve the normal mechanical alignment of the knee and knee extensor mechanism.25 Unlike some operations directed at realigning the extensor mechanism, selective hemiepiphyseodesis is minimally-invasive and can be performed as an outpatient procedure. Both extremities can be addressed simultaneously. Patients are encouraged to begin range of motion exercises and bear weight as tolerated immediately after surgery. Release to full activities occurs once the surgical wounds have healed. Stevens et al25 reviewed 152 knees in 76 patients who underwent hemiphyseal stapling for idiopathic adolescent genu valgum and showed improved clinical and radiographic parameters as well as a high degree of patient satisfaction. The authors suggested that this technique be used in treating symptomatic genu valgum, including patellar instability, although it is unclear how many patients in their study had patellar subluxation or dislocation episodes. Additionally, 4 knees in their series underwent concomitant lateral retinacular release, but it is unclear if these patients had patellar instability.
We were unable to find any published studies that focus on treatment of patellar instability by correcting genu valgum with selective hemiepiphyseodesis at the knee. The purpose of this study is to report the results of treating pediatric patients with patellar instability by correcting excessive genu valgum with selective hemiepiphyseodesis. The intent is to make orthopaedic surgeons aware of the efficacy, simplicity and safety of this treatment strategy and its application in the armamentarium of treatment methods for pediatric patients with patellar instability.
2. Methods
We obtained institutional review board (IRB) approval for this retrospective review of patient records and radiographs. All patients with patellar instability symptoms with associated genu valgum who underwent selective hemiepiphyseodesis at the knee from January 1999 through July 2009 at a university-based children's hospital were identified, resulting in a total of 22 patients. Seven patients were excluded. Of these, 4 patients did not have a documented episode of patellar instability, only patellofemoral joint pain. Two patients underwent concomitant soft tissue procedures about the knee and 1 patient was skeletally mature at the time of surgery. Fifteen patients were included in the study.
Data about the frequency of pre- and post-operative patellar subluxation and dislocation episodes as well as changes in activity level were obtained from the patient's history documented in the medical records. A subluxation episode was recorded when a patient described a painful and excessive lateral movement of the patella that spontaneously reduced, while a dislocation required a patient description involving a manual patellar reduction. Although the exact numbers of pre- and post-operative patellar instability episodes were not specifically documented, the records did document whether there was a relative improvement in symptoms after surgery. Similarly, relative improvement in activity level was apparent in the patient records, particularly regarding ability to participate in competitive sports.
On exam, all patients were noted to have clinically apparent genu valgum. We could not include clinical measurements of genu valgum in this study (i.e. intermalleolar distance, tibiofemoral angle) as these were not consistently documented in the physical exam. Radiographically, we used the anatomic lateral distal femoral angle (aLDFA) to quantify pre-operative genu valgum and the amount of knee alignment correction obtained post-operatively. This was measured from the pre- and post-operative anterior-posterior (AP) knee radiographs by measuring the angle between the femoral shaft and the distal femoral articular surface. Normal aLDFA measurements can range between 79 and 83°.4, 26 A value <79° indicates excessive genu valgum. Since all patients did not have pre- and post-operative full length lower extremity radiographs, tibiofemoral angle and mechanical axis alignment zone could not be accurately calculated.
Patients underwent a trial of conservative management prior to surgery, consisting of activity modification, physical therapy for quadriceps strengthening and, in some cases, bracing with a patellar cut-out orthotic. The indications for surgery included continued painful patellar subluxation or dislocation in the setting of clinical and radiographic genu valgum in a skeletally immature patient following at least 6 months of conservative management if remaining growth allowed.
The goal of surgery was to eliminate patellar instability by reestablishing normal patella tracking. Our approach used the principle of guided growth to restore the normal anatomic relationship of the knee joint and the extensor mechanism by correcting the mechanical axis to the center of the knee. The medial distal femoral physis was treated in all cases because it was the primary site of deformity. The medial proximal tibial physis was treated if the anatomic medial proximal tibial angle was >90°. Blount staples (Zimmer, Warsaw, IN) were implanted exclusively from 1999 to 2003 with a change to 8-plates (Orthofix, McKinney, TX) thereafter. If needed, both knees were treated simultaneously. Surgery was typically performed on an outpatient basis. Post-operatively, immediate knee motion and weight bearing as tolerated were encouraged. Once the surgical wounds were healed at 10–14 days, patients were released to full activities as tolerated.
Implant removal was routinely performed on an outpatient basis when the mechanical axis was slightly overcorrected. The previous surgical scar was often resected at the time of implant removal to create a thin, cosmetically-pleasing scar. Full activity was permitted after hardware removal once the wound healed in 10–14 days. All complications were reported.
Summary statistics were used to describe the research variables as means and percentages.
All statistical calculations were done using a Student's t-test with an alpha level set at 0.05.
3. Results
Twenty-six knees in 15 patients, 6 males and 9 females, were included. The average age at surgery was 12+0 years (range 9+3 to 14+6), with males averaging 12+10 years and females 11+5 years. Twelve patients were diagnosed with idiopathic genu valgum. One patient was diagnosed with acrodysostosis and 1 had Soto's syndrome. These underlying conditions may have contributed to the bilateral genu valgum seen in these patients. The final patient sustained a proximal tibia fracture, leading to genu valgum and subsequent patellar instability of the affected extremity.
Pre-operatively, all 15 patients described multiple painful patellar subluxation episodes and 7 patients reported 1 or more patellar dislocations requiring manual reduction (Table 1). Six patients were active in competitive sports and stated that patellar instability limited or acutely prohibited their participation. In cases where remaining growth allowed, patients underwent a trial of conservative management consisting of a combination of activity modification, physical therapy and bracing for a range of 3–33 months before proceeding with surgery.
Table 1.
Summary of patient patellar symptomatology and radiographic alignment before and after selective hemiepiphyseodesis for treatment of patellar instability (HWR = hardware removal).
| Patient | Knee | Pre-op symptoms |
Implant | aLDFA (deg) |
Post-op symptoms | Follow-up (months) | |||
|---|---|---|---|---|---|---|---|---|---|
| Subluxation | Dislocation | Pre-op | Latest F/U | Changea | |||||
| 1 | L | + | + | Staple | 80.0 | 86.0 | 6.0 | Less frequent recurrent | 49.5 |
| R | + | + | Staple | 77.0 | 87.0 | 10.0 | Subluxations/dislocations | 59.4 | |
| 2 | L | + | – | Staple | 78.0 | 86.0 | 8.0 | None | 9.2 |
| R | + | – | Staple | 78.0 | 88.0 | 10.0 | None | 9.2 | |
| 3 | L | + | – | Staple | 79.0 | 86.0 | 7.0 | None | 35.3 |
| R | + | – | Staple | 73.0 | 88.0 | 15.0 | None | 35.2 | |
| 4 | L | + | – | Staple | 80.0 | 85.0 | 5.0 | None | 9.4 |
| R | + | – | Staple | 80.0 | 87.0 | 7.0 | None | 9.4 | |
| 5 | L | + | – | Staple | 75.0 | 83.0 | 8.0 | None | 71.9 |
| R | + | – | Staple | 77.0 | 85.0 | 8.0 | None | 71.9 | |
| 6 | L | + | + | Staple | 76.0 | 83.0 | 7.0 | None | 22.2 |
| R | + | – | Staple | 78.0 | 85.0 | 7.0 | None | 22.2 | |
| 7 | L | + | + | 8-plate | 75.7 | 79.0 | 3.3 | None | 27.4 |
| R | + | + | 8-plate | 77.7 | 80.7 | 3.0 | Mild recurrent subluxations | 27.4 | |
| 8 | L | + | + | 8-plate | 81.8 | 82.3 | 0.5 | 1 self-reduced dislocation | 42.8 |
| 9 | L | + | – | 8-plate | 77.1 | 80.5 | 3.4 | None | 28.6 |
| R | + | + | 8-plate | 77.7 | 81.1 | 3.4 | 1 recurrent dislocation | 28.6 | |
| 10 | L | + | – | 8-plate | 75.7 | 79.6 | 3.9 | None | 23.4 |
| R | + | – | 8-plate | 77.0 | 80.6 | 3.6 | None | 23.4 | |
| 11 | L | + | – | 8-plate | 77.6 | 82.7 | 5.1 | None | 35.3 |
| R | + | – | 8-plate | 78.3 | 86.1 | 7.8 | None | 13.7 | |
| 12 | R | + | – | 8-plate | 78.0 | 86.0 | 8.0 | 1 subluxation episode | 32.9 |
| 13 | R | + | + | 8-plate | 76.8 | 90.0 | 13.2 | None | 24.1 |
| 14 | L | + | – | 8-plate | 80.0 | 86.4 | 6.4 | Less frequent recurrent | 20.7 |
| R | + | – | 8-plate | 78.6 | 89.4 | 10.8 | Subluxations | 20.7 | |
| 15 | L | + | + | 8-plate | 74.0 | Unavailable | n/a | None | 15.7 |
Note: This reflects overall change in the aLDFA from time of pre-op to latest follow-up. In some cases, significant rebound growth was observed after hardware removal. This is detailed in Table 2.
Twenty-six medial distal femurs and 4 medial proximal tibias underwent selective hemiepiphyseodesis, using Blount staples (Zimmer, Warsaw, IN) across 16 physes and 8-plates (Orthofix, McKinney, TX) across 14 physes. Average follow-up duration was 30.9 months (range 9.2–71.9 months). The average anatomic lateral distal femoral angle (aLDFA) significantly improved from 77.7° pre-operatively (range 73.0°–81.8°) to 84.5° post-operatively (range 79.0°–90.0°) (p < 0.001) (Table 1). Twenty knees (77%) underwent hardware removal at an average of 9.6 months post-operatively to prevent overcorrection. Of these knees, 9 had adequate follow-up radiographs to document rebound growth. In this subset, the average aLDFA significantly rebounded from 85.6° (range 79.1°–92.2°) at the time of hardware removal to 82.9° (range 79.6°–87.0°) at latest follow-up, giving an average rebound growth of 2.7° (range 0.0°–9.9°) (p = 0.03) (Table 2).
Table 2.
Rebound growth of the anatomic lateral distal femoral angle (aLDFA) from time of hardware removal (HWR) to latest follow-up.
| Patient | Knee | aLDFA (deg) |
||
|---|---|---|---|---|
| HWR | Latest F/U | Rebound | ||
| 1 | R | 87 | 87 | 0.0 |
| 2 | L | 88 | 86 | 2.0 |
| 3 | L | 90 | 86 | 4.0 |
| 8 | L | 92.2 | 82.3 | 9.9 |
| 9 | L | 82.3 | 80.5 | 1.8 |
| R | 82.8 | 81.1 | 1.7 | |
| 10 | L | 79.1 | 79.6 | −0.5 |
| R | 82.4 | 80.6 | 1.8 | |
| 11 | L | 86.5 | 82.7 | 3.8 |
| Mean | 85.6 | 82.9 | 2.7 | |
Of the 26 knees treated, 18 (69%) had complete symptom resolution and 8 (31%) had significant reduction in symptoms (Table 1). All 6 competitive athletes returned to full sports participation (Fig. 1a–c). No further procedures were required after hardware removal in any patient and none of the knees developed excessive genu varum from overtreatment. The only complication that occurred was a staple that required reinsertion after partially backing out.
Fig. 1.
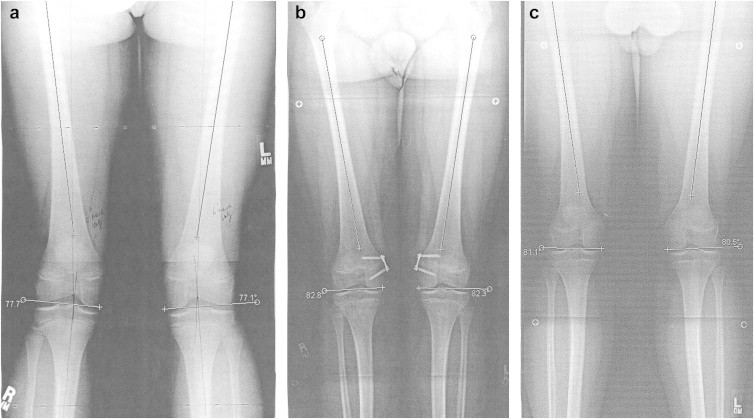
a. Pre-operative radiograph of a patient with multiple bilateral patellar subluxations and recurrent right patellar dislocations interfering with participation in competitive basketball. Anatomic lateral distal femoral angles (aLDFA) indicate bilateral excessive genu valgum. Bilateral medial distal femoral hemiepiphyseodesis was performed with plate-screw constructs. b. At the time of hardware removal, both knees were symptom-free and the patient had returned to competitive basketball. The aLDFA corrected to normal bilaterally. c. At near 30 months post-op, the patient remained symptom-free in the left knee and had experienced only 1 recurrent dislocation of the right patella, even with full participation in competitive basketball. The aLDFA rebounded since the time of hardware removal, but remains normal bilaterally.
4. Discussion
The treatment principle behind the most commonly utilized procedures for treating adolescent patellar instability is that a malaligned patella must be brought to an anatomically aligned knee joint. Anatomic alignment means that the center of the knee joint lies on the mechanical axis line of the limb. To achieve this, extensive soft tissue procedures, osteotomies, or both have been reported. Following these procedures, hospitalization is often necessary to observe for compartment syndrome, provide adequate pain control, and to begin the rehabilitation process. A significant period of protected weight bearing, knee immobilization, and prolonged rehabilitation under the supervision of a physical therapist is often necessary. Patients and parents are forced to take time off of school and work. Staging is often necessary if both extremities are involved, making the total recovery and rehabilitation time several months long. Outcomes are not reliable and complications are common.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20
Some adolescents with patellar instability have a malaligned knee joint. Genu valgum creates a structural malalignment between the frontal plane position of the knee and the mechanical axis of the limb. As a mobile object, the patella tries to seek the mechanical axis, which can result in painful patellar subluxations and dislocations depending on the severity of the malalignment and possibly other anatomic features, such as trochlear dysplasia. The treatment principle for procedures performed on this group of patients should be to bring the malaligned knee joint to the properly aligned patella, so that both will align with the mechanical axis of the limb. When this unique pathoanatomy is not appreciated, these patients undergo inappropriate treatment modalities that attempt to bring the well aligned patella to the malaligned knee joint. Conservative management can reduce symptoms in some cases, but is impractical and ineffective for most patients. Physical therapy for quadriceps stretching and strengthening has minimal lasting effects on symptoms, and certainly has no effect on the structural deformity. Although bracing and taping can help relieve symptoms, they do not change knee alignment or stabilize the patellofemoral joint effectively,27 nor do they offer any additional benefit to standard physical therapy.28 Lifestyle restrictions are often unacceptable in active, young patients who have a strong desire to compete in sports. Additionally, some patients are symptomatic simply with walking or stair climbing. Activity modification is especially difficult for these patients.
Surgery is indicated for patients with painful patellar instability when it is evident that conservative measures have failed to adequately relieve their symptoms. For skeletally immature patients with patellar instability associated with genu valgum, the most logical and simple surgical approach is to normalize the mechanical axis of the limb with selective hemiepiphyseodesis. This effectively brings the malaligned knee to the properly aligned patella, restoring both structures to the normal mechanical axis of the limb. In this series, consistent and quick resolution of genu valgum was observed, with average aLDFA improvement from 77.7° to 84.5° and an average time to hardware removal of 9.6 months. Our results are comparable to the results reported by Stevens et al25 for the treatment of idiopathic genu valgum with staples. They reported an average aLDFA improvement from 78° to 84° and an average time to correction or hardware removal of 10 months. Our results further demonstrate that, by normalizing the mechanical axis, patellar instability and pain improve significantly in all patients, with 69% reporting complete resolution of symptoms. Additionally, all athletes returned to competitive sports post-operatively.
The procedure was performed on an outpatient basis in most cases and, where appropriate, both extremities were treated under the same anesthetic. Post-operatively, patients were encouraged to bear weight and perform knee range of motion as tolerated as soon as possible. All were released to full activity once the surgical wounds healed.
In this series, only 1 hardware complication occurred in 26 treated knees (3.8%). A staple partially backed out and required re-insertion. Staple migration is a reported complication of hemiphyseal stapling. Stevens and Klatt29 reported a 45% (24/53) incidence of staple migration in children with rickets treated with hemiphyseal stapling, though Stevens et al25 reported no staple migrations in 152 knees treated for idiopathic genu valgum. Considering the small but inconvenient reported rate of staple migration, we switched to 8-plates (Orthofix, McKinney, TX) when they became commercially available. There were no further hardware complications after switching to this device.
Like hardware failure, other complications of hemiepiphyseodesis are rare. Stevens et al25 reported 4 superficial wound infections in 152 knees, all treated successfully with oral antibiotics. Fraser et al24 reported 1 infection in 27 knees stapled for secondary genu valgum. Stevens and Klatt29 reported 1 superficial and 2 deep infections in children with rickets undergoing 68 hemiphyseal treatments with staples or plate-screw constructs. There were no infections in the 26 knees treated in this series.
Premature physeal closure and iatrogenic fracture are perhaps the most concerning complications associated with hemiepiphyseodesis. Although these complications have been reported, they are exceedingly rare. Fraser et al24 reported 1 premature physeal closure in 43 knees treated for primary and secondary genu valgum. Stevens et al25 reported no premature physeal closures in 152 knees stapled for treatment of idiopathic genu valgum. There were no nerve deficits or iatrogenic fractures reported in either of these studies. We had no premature physeal closures or iatrogenic fractures in this series.
Rebound growth has been well described after hemiphyseal treatment of genu valgum. It occurs after the hardware is removed and the ipsilateral hemiphysis temporarily grows at a faster rate than normal, which is thereby faster than the contralateral side of the physis. This results in some loss of alignment correction. Stevens et al25 reported an average rebound growth of 3°, where the aLDFA measured 87° at staple removal verses 84° at latest follow-up. Of the 152 knees with idiopathic genu valgum in their series, 8 required repeat stapling for successful correction of the rebound growth. In children with secondary genu valgum, there is a much higher incidence of recurrent malalignment due to rebound growth.29 Due to this phenomenon, most authorities recommend correcting the mechanical axis to neutral or slightly beyond neutral prior to hardware removal. Our approach parallels this thinking.
Due to its retrospective nature, a limitation of this study is the inability to include additional clinical and radiographic quantification of pre- and post-operative limb alignment, specifically intermalleolar distance, tibiofemoral angle, and mechanical axis alignment zone. Although aLDFA is an accepted measure of genu valgum, additional measurements would have provided additional objective evidence of deformity correction. However, the indications for surgery were knee pain and patellar instability. The most important outcome measures were relief of knee pain and improvement in patellar stability. These outcomes measures are related to, but not dependent upon, objective radiographic measurements.
Another caution when interpreting the information in this study is that this technique is only successful in treating patellar instability when genu valgum is present. This technique is not appropriate in cases of recurrent patellar instability in the setting of normal mechanical alignment of the limb. It, therefore, brings to light the importance of assessing limb alignment in all patients with patellar instability. Clinically, mechanical alignment is assessed by observing the gross tibiofemoral angle in stance and measuring the intermalleolar distance. Radiographic assessment should include standing full-length radiographs of the lower extremities to calculate the aLDFA, tibiofemoral angle, and mechanical axis alignment zone. Once limb alignment has been properly assessed, this simple and effective treatment for patellar instability can be considered.
5. Conclusion
This is the first study to focus on the use of selective hemiepiphyseodesis to treat painful patellar instability in adolescent patients with associated genu valgum. We have shown that symptoms reliably improve or resolve with this treatment, thereby improving function, including return to competitive sports. It is imperative to assess mechanical limb alignment with a careful clinical exam and appropriate radiographs in all patients with patellar instability. If genu valgum is detected in skeletally immature patients, selective hemiepiphyseodesis is recommended as a minimally-invasive, safe, and effective treatment for this group of patients. If pain or patellar instability persist after anatomic limb alignment has been achieved, patella centralization procedures can be performed. These were not necessary in our patients.
Conflicts of interest
All authors have none to declare.
References
- 1.Boden B.P., Pearsall A.W., Garrett W.E. Patellofemoral instability: evaluation and management. J Am Acad Orthop Surg. 1997;5:47–57. doi: 10.5435/00124635-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 2.White G.R., Mencio G.A. Genu valgum in children: diagnostic and therapeutic alternatives. J Am Acad Orthop Surg. 1995;3:275–283. doi: 10.5435/00124635-199509000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Heath C.H., Staheli L.T. Normal limits of knee angle in white children. Genu varum and genu valgum. J Pediatr Orthop. 1993;13:259–262. [PubMed] [Google Scholar]
- 4.Paley D., Herzenberg J.E., Tetsworth K. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 5.Hungerford D.S., Barry M. Biomechanics of the patellofemoral joint. Clin Orthop Relat Res. 1979;144:9–15. [PubMed] [Google Scholar]
- 6.Arendt E.A., Fithian D.C., Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21:499–519. doi: 10.1016/s0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 7.Joo S.Y., Park K.B., Kim B.R. The “four-in-one” procedure for habitual dislocation of the patella in children. J Bone Joint Surg Br. 2007;89B:1645–1649. doi: 10.1302/0301-620X.89B12.19398. [DOI] [PubMed] [Google Scholar]
- 8.Deie M.O., Sumen Y., Yasumoto K. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85B:887–890. [PubMed] [Google Scholar]
- 9.Steiner T.M., Torga-Spak R., Teitge R.A. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34:1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 10.Farr J., Schepsis A.A. Reconstruction of the medial patellofemoral ligament for recurrent patellar instability. J Knee Surg. 2006;19:307–316. doi: 10.1055/s-0030-1248123. [DOI] [PubMed] [Google Scholar]
- 11.Nomura E., Inoue M. Hybrid medial patellofemoral ligament reconstruction using the semitendinosus tendon for recurrent patellar dislocation: minimum 3 years' follow-up. Arthroscopy. 2006;22:787–793. doi: 10.1016/j.arthro.2006.04.078. [DOI] [PubMed] [Google Scholar]
- 12.Albright J.C., Noyes F.R. Reconstruction of the medial patellofemoral ligament with autologous quadriceps tendon. Arthroscopy. 2006;22:904e1–904e7. doi: 10.1016/j.arthro.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 13.Utting M.R., Mulford J.S., Eldridge J.D. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br. 2008;90:180–185. doi: 10.1302/0301-620X.90B2.20017. [DOI] [PubMed] [Google Scholar]
- 14.Kolowich P.A., Paulos L.E., Rosenberg T.D. Lateral release of the patella: indications and contraindications. Am J Sports Med. 1990;18:359–365. doi: 10.1177/036354659001800405. [DOI] [PubMed] [Google Scholar]
- 15.Fulkerson J.P. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop. 1983;177:176–181. [PubMed] [Google Scholar]
- 16.Fulkerson J.P., Becker G.J., Meaney J.A. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490–497. doi: 10.1177/036354659001800508. [DOI] [PubMed] [Google Scholar]
- 17.Fondren F.B., Goldner J.L., Bassett F.H. Recurrent dislocation of the patella treated by the modified Roux-Goldthwait procedure. J Bone Joint Surg Am. 1985;7:993–1005. [PubMed] [Google Scholar]
- 18.Marsh J.S., Daigneault J.P., Sethi P. Treatment of recurrent patellar instability with a modification of the Roux-Goldthwait technique. J Pediatr Orthop. 2006;26:461–465. doi: 10.1097/01.bpo.0000217711.34492.48. [DOI] [PubMed] [Google Scholar]
- 19.Koskinen S.K., Rantanen J.P., Nelimarkka O.I. Effect of Elmslie-Trillat and Roux-Goldthwait procedures on patellofemoral relationships and symptoms in patients with patellar dislocations. Am J Knee Surg. 1998;11:167–173. [PubMed] [Google Scholar]
- 20.Vahasarja V., Kinnunen P., Lanning P. Operative realignment of patellar malalignment in children. J Pediatr Orthop. 1995;15:281–285. doi: 10.1097/01241398-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Bowen J.R., Torres R.R., Forlin E. Partial epiphysiodesis to address genu varum or genu valgum. J Pediatr Orthop. 1992;12:359–364. doi: 10.1097/01241398-199205000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Zuege R.C., Kempken T.G., Blount W.P. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 23.White G.R., Mencio G.A. Genu valgum in children: diagnostic and therapeutic alternatives. J Am Acad Orthop Surg. 1995;275:275–283. doi: 10.5435/00124635-199509000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Fraser R.K., Dickens D.R.V., Cole W.G. Medial physeal stapling for primary and secondary genu valgum in late childhood and adolescence. J Bone Joint Surg Br. 1995;77B:733–735. [PubMed] [Google Scholar]
- 25.Stevens P.M., Maguire M., Dales M.D. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19:645–649. [PubMed] [Google Scholar]
- 26.Principles of Deformity Correction. Springer; New York: 2003. [Google Scholar]
- 27.Lysholm J., Nordin M., Ekstrand J. The effect of a patella brace on performance in a knee extension strength test in patients with patellar pain. Am J Sports Med. 1984;12:110–112. doi: 10.1177/036354658401200204. [DOI] [PubMed] [Google Scholar]
- 28.Kowall M.G., Kolk G., Nuber G.W. Patellar taping in the treatment of patellofemoral pain: a prospective randomized study. Am J Sports Med. 1996;24:61–66. doi: 10.1177/036354659602400111. [DOI] [PubMed] [Google Scholar]
- 29.Stevens P.M., Klatt J.B. Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop. 2008;28:632–639. doi: 10.1097/BPO.0b013e3181841fda. [DOI] [PubMed] [Google Scholar]


