Abstract
Lipotransfer is a vital tool in the surgeon’s armamentarium for the treatment of soft tissue deficits of throughout the body. Fat is the ideal soft tissue filler as it is readily available, easily obtained, inexpensive, and inherently biocompatible.1 However, despite its burgeoning popularity, fat grafting is hampered by unpredictable results and variable graft survival, with published retention rates ranging anywhere from 10-80%. 1-3
To facilitate investigations on fat grafting, we have therefore developed an animal model that allows for real-time analysis of injected fat volume retention. Briefly, a small cut is made in the scalp of a CD-1 nude mouse and 200-400 µl of processed lipoaspirate is placed over the skull. The scalp is chosen as the recipient site because of its absence of native subcutaneous fat, and because of the excellent background contrast provided by the calvarium, which aids in the analysis process. Micro-computed tomography (micro-CT) is used to scan the graft at baseline and every two weeks thereafter. The CT images are reconstructed, and an imaging software is used to quantify graft volumes.
Traditionally, techniques to assess fat graft volume have necessitated euthanizing the study animal to provide just a single assessment of graft weight and volume by physical measurement ex vivo. Biochemical and histological comparisons have likewise required the study animal to be euthanized. This described imaging technique offers the advantage of visualizing and objectively quantifying volume at multiple time points after initial grafting without having to sacrifice the study animal. The technique is limited by the size of the graft able to be injected as larger grafts risk skin and fat necrosis. This method has utility for all studies evaluating fat graft viability and volume retention. It is particularly well-suited to providing a visual representation of fat grafts and following changes in volume over time.
Keywords: Medicine, Issue 95, autologous, fat graft, fat injection, lipofilling, lipotransfer, volume retention, micro-computed tomography, graft viability, graft survival, graft monitoring
Introduction
Soft tissue defects arise from a variety of causes including trauma, tumor resection, aging, and congenital anomaly. They can be debilitating for patients, and represent one of the most common, yet challenging problems for reconstructive surgeons. Many methods exist for addressing soft tissue deficiencies, such as local and free flaps, collagen injections, and synthetic fillers.4-8 However, since its first documented use by Neuber in 18931, autologous fat transfer remains the gold standard for the repair of soft tissue deficits, as it is ready available, easy and safe to harvest, and naturally compatible.1,2
Despite these advantages, autologous fat grafts suffer from unpredictable and variable survival, with retention rates ranging anywhere from 10-80% over time.1-3,9 In order to account for this expected loss of volume and symmetry, surgeons must often overcorrect when filling soft tissue defects, or perform multiple follow-up procedures.
Poorly vascularized graft beds are partly to blame for this tissue resorption. Additionally, the lack of a benchmark analysis method to compare graft survival may also contribute to the inconsistency in reported results. A precise method for measuring graft volume would reduce measurement error when evaluating retention rates. This in turn would help researchers more accurately identify the causative factors that affect graft survival. Although many laboratory animal models have facilitated both quantitative and qualitative assessment of human fat graft survival, most are based on histological and biochemical means and require sacrificing the study animal to yield a single measurement.3,10-12 Little has been reported on the use of imaging techniques to enumerate fat graft volume retention in vivo.
A handful of clinical studies have shown more effective measurement techniques using imaging. Magnetic Resonance Imaging (MRI) was employed by Hörl et al. to measure fat graft survival13, and CT was utilized by Har-Shai et al. and Fontdevila et al. in their analyses of volume retention after grafting in patients who suffered from HIV.14,15 Employing three-dimensional (3D) imaging software, Meier et al. measured volume retention in humans after autologous fat grafting by comparing images from the preoperative and postoperative period.16
Yet, a standardized method employing imaging to measure fat graft survival is lacking in basic science research. A high resolution imaging approach for assessing the volumes of fat grafts would allow not only for accurate and reproducible volume measurements, but also for repeated measurements allowing visualization of the evolution of fat graft survival in a real time fashion.
Protocol
NOTE: Experimental protocols and patient consent forms for obtaining fat were reviewed and approved by the Stanford University Institutional Review Board (Protocol #2188). All animal procedures were approved by the Stanford Administrative Panel on Laboratory Animal Care (APLAC) under Protocol #9999. All experiments were conducted with strict adherence to animal safety and humane care guidelines.
1. Fat Harvesting
Using the Coleman procedure17-19, obtain human adipose tissue from the abdomen, flank, and/or thigh regions of healthy female patients undergoing elective liposuction.
To process the lipoaspirate for grafting, begin by allowing the fat to settle for 30 min.
Lipoaspirate typically settles into three layers, with oil at the top, fat in the middle, and blood at the bottom. Aspirate and discard the top oil layer and the bottom blood layer.
To further remove any remaining tumescent fluid or cell debris, centrifuge the fat for 5 min at 350 x g and 4 °C, and aspirate the bottom aqueous layer.
Calculate the amount of fat needed for grafting, allowing for 20% delivery error, and transfer the desired volume of fat to 50 ml conical(s). Multiply 400 by the number of mice in the study to obtain microliters of fat needed for grafting.
At this point, if performing Cell Assisted Lipotransfer20,21, place volume of fat for grafting on ice. Then harvest adipose-derived stromal cells (ASCs) from the remaining fat using the standard technique described by Zuk et al22.
2. Fat Grafting
Obtain female, homozygous CD-1 nude mice for the experimental study. Choose mice between 8 - 12 weeks of age.
To induce anesthesia, place mouse into a knockdown box with 2.5% isoflurane/oxygen mixture at 2 L/min for approximately 10 min. Please note that recommended isoflurane dose varies with mouse strain.
When the respiration rate of the mouse has slowed, confirm adequate sedation with a toe pinch. Apply veterinary lubricating ophthalmic ointment to both eyes of the mouse.
If mouse does not flinch in response to toe pinch, this confirms a sufficient plane of anesthesia. Place the mouse’s nose into a nosecone delivering 2.5% isoflurane/oxygen mixture at 1-2 L/min. If mouse retracts from toe pinch, return to knockdown box and retest after 5 min.
Set up sterile field under mouse and then sterilize scalp with 2.5% povidone-iodine followed by 70% ethanol solution. Repeat two more times.
Place surgical drapes over the mouse and be careful to maintain sterile field. Sterile instruments, gloves, and PPE should be used at all times.
If fat volume to be grafted was previously placed on ice, allow fat to first adjust to RT before delivery.
Backload a 1 ml luer-lock syringe with 1 ml of fat.
Connect a 14 G, 8 cm long fat grafting cannula to the end of the syringe.
Prime system by depressing the syringe plunger until between 200 and 400 µl of fat remains in the syringe. While depressing the syringe plunger confirm that the cannula has fully filled with fat by observing fat exiting the distal cannula hole.
Using fine forceps, lift the dorsal skin in the midline overlying the caudal-most aspect of the skull. Make a 1.5 mm cut in the skin using fine scissors.
Place a single 6-0 nylon suture through middle of the cut that will later be used to bring the wound edges together after grafting is performed. Do not tie the suture.
Create a subcutaneous pocket over the skull by inserting the cannula through the skin incision and passing the cannula back and forth in a fan-shaped pattern over the skull to free any connective tissue attachments to the overlying skin.
Once the pocket has been created, position the cannula in the midline of the mouse directly over the skull until the tip lies at the rostral-most aspect of the pocket which should be just behind a line drawn between the eyes. (Figure 1A)
Slowly inject the fat in a retrograde fashion, advancing the plunger while pulling the cannula back. Using forceps, bring the wound edges together and lift them up to keep any fat from leaking out of the pocket.
Tie the suture that was previously placed, making sure that the first knot lies lightly against the skin. Tie three more square knots and cut the suture with a 3 mm tail. (Figure 1B)
Confirm with visualization and manual palpation that the pocket is not overfilled and skin overlying the pocket is not tense. If the pocket has been overfilled, cut the suture and remove all fat from within the pocket. Wash the pocket out with phosphate buffered saline (PBS) pH 7.4 and re-inject a smaller volume of fat.
Remove mouse from anesthesia and place on its back or side in a clean cage by itself. Monitor the animal for regular breathing, normal movements, absence of bleeding, and signs of pain or distress. Administer buprenorphine 0.1 mg/kg subcutaneously every 6 hr for up to 48 hr if the animal is in pain.
Make sure that the animal has woken up sufficiently to maintain sternal recumbency before leaving it unattended. Do not place animal into a cage with other animals until it has fully recovered.
After 4 hr, ensure that the animal is able to eat and drink, move, and breathe normally and that there is no bleeding from the operative site. Return it to the animal care facility.
3. Micro-CT
Scan mice for baseline volume by post-operative Day 3, and then repeat scans at post-operative Weeks 2, 4, 6 and 8.
When imaging the mice at each time point, follow pre- and post-procedural sedation and animal care guidelines as outlined previously in Steps 2.2-2.4 and 2.17-2.19.
Perform scans on a micro-CT scanner with a reconstruction voxel size of 100 µm or better.
With a peak X-ray kilovoltage of 80 kVp and an anode current of 450 µA, administer a ration dose of approximately 5 centiGy during a 9 min scan to each mouse. Please note these values vary depending upon the scanning protocol.
Prior to performing the first scan, calibrate micro-CT with an imaging phantom that distinguishes between air, water, and bone intensity.
Place four mice into scanner in the ventral position with two mice on top and two on bottom. A scanning bed can easily be constructed using 60 ml syringes to hold the mouse body and 10 ml syringes as nose cones.23
Maintain mice under anesthesia with a 2.5% isoflurane/oxygen mixture at 1-2 L per min.
Confirm with scout image that the entire skull of the mouse, from nose to first cervical vertebra, and from top of skull to base of skull, will be imaged.
4. Micro-CT Analysis
Open the reconstructed images with a micro-CT imaging analysis software that allows the creation of Regions of Interest (ROI’s) by selecting voxels using thresholds for pixel intensity. Software also allows creation of 3D surfaces through the interpolation of selected voxels, and for volume analysis.
Start by loading the reconstructed CT images in two-dimensional (2D) coronal, axial, and sagittal views. (Figure 2A)
Using the axial slice as a guide, navigate to the sagittal slice that corresponds to the left-most aspect of the fat graft. Select an upper and lower threshold for pixel intensity that captures all voxels corresponding to the fat graft, but that excludes the surrounding tissue and bone. (Figure 2B)
Define an ROI in the sagittal view that corresponds to the fat graft using previously defined pixel intensity thresholds. Repeat this procedure every fifth sagittal slice, navigating until the right-most aspect of the graft is reached. (Figure 2C)
Interpolate selected voxels from all 2D ROI’s into a single, combined 3D ROI. (Figure 2D)
Record ROI volume calculated by the software.
Render the 3D isosurface to visualize the final fat graft volume. (Figure 2E)
In subsequent analyses, be sure to keep the pixel intensity maximum and minimum threshold values the same as those used for the baseline analysis.
5. Fat Harvest
After mice have been scanned for the week 8 24,25 time point, anesthetize the mice as previously described above in Steps 2.2-2.4 and 2.17-2.19.
Following APLAC guidelines, euthanize the mice by separating their spinal columns.
Place mouse in operative field. Using tenotomy scissors, carefully open the pocket and dissect the overlying skin and connective tissue attachments from the fat graft.
At this point, it may help to excise a patch of the overlying dorsal skin to aid in extraction of the graft. (Figure 3A)
Lightly maintain traction on the graft with forceps and turn graft from side to side to visualize successive points of tension that need to be released with scissors.
Stay as close to the graft as possible when excising to minimize the connective tissue taken with the graft. (Figure 3B)
After excising graft, measure mass on a tared scale that is accurate to at least 0.01 grams.
Calculate the volume of the fat graft using the measured mass value and the average density of human fat (0.9 g/ml) as a conversion rate.
Compare calculated volume of fat graft to that obtained using micro-CT.
Fat grafts can be processed for histology or further analysis if needed.
Representative Results
Fat grafts progressively decreased in volume over the course of study, resulting in 62.2% average survival by Week 8. (Figure 4A)24At the completion of the Week 8 scan, each fat graft was extracted in a single piece. A Wilcoxan rank sum test was used to compare the difference between volume measurements of fat grafts obtained by either micro-CT or calculated from physical mass. No significant difference was found between these two methods (two-sided p-value = 0.9362). (Figure 4B)
With 5 centiGy per scan and five scan time points, each mouse received no more than a total of 25 centiGy over the course of the study. Consistent with this, none of the mice displayed any gross evidence of cutaneous radiation burns.
 Figure 1. (A) A 14 G cannula on a 1 ml syringe, positioned in the midline and at the rostral-most aspect of the pocket prior to beginning fat injection. (B) Nude mouse upon completed fat grafting, with a single nylon suture used to bring wound edges together. The pocket has been filled but is not tense.
Figure 1. (A) A 14 G cannula on a 1 ml syringe, positioned in the midline and at the rostral-most aspect of the pocket prior to beginning fat injection. (B) Nude mouse upon completed fat grafting, with a single nylon suture used to bring wound edges together. The pocket has been filled but is not tense.
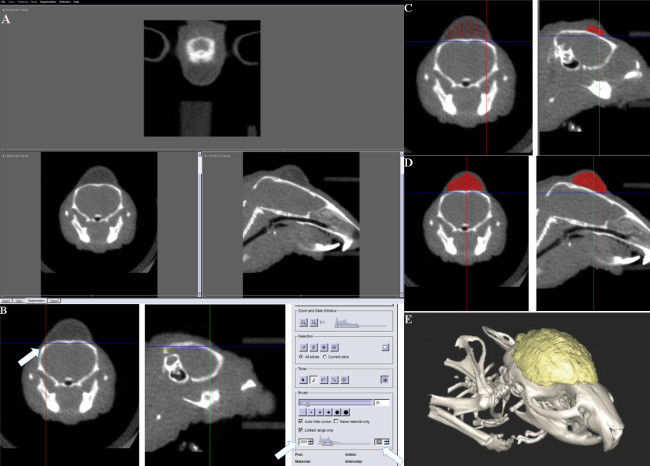 Figure 2. (A) The reconstructed images initially displayed in axial, coronal, and sagittal views. (B) Using the axial view as a guide to navigate to the left most aspect of the graft on sagittal view. Setting a threshold for pixel intensity so that all voxels selected within the threshold range will represent adipose tissue, thus allow for the demarcation of the fat graft volume. (C) ROI’s defined on sagittal view starting at the left most aspect of the graft and continued every fifth slice moving to the other end of the graft. (D) All selected voxels from 2D ROI’s interpolated into a single 3D ROI. (E) A three-dimensional surface was created using cubic-spline interpolation to visualize the total fat graft volumes.
Figure 2. (A) The reconstructed images initially displayed in axial, coronal, and sagittal views. (B) Using the axial view as a guide to navigate to the left most aspect of the graft on sagittal view. Setting a threshold for pixel intensity so that all voxels selected within the threshold range will represent adipose tissue, thus allow for the demarcation of the fat graft volume. (C) ROI’s defined on sagittal view starting at the left most aspect of the graft and continued every fifth slice moving to the other end of the graft. (D) All selected voxels from 2D ROI’s interpolated into a single 3D ROI. (E) A three-dimensional surface was created using cubic-spline interpolation to visualize the total fat graft volumes.
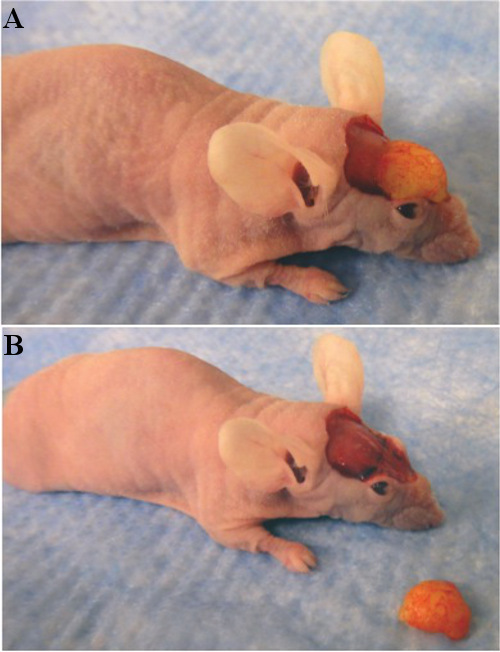 Figure 3. (A) Fat graft before explantation, with dorsal patch of skin removed. (B) Fat graft after explantation.
Figure 3. (A) Fat graft before explantation, with dorsal patch of skin removed. (B) Fat graft after explantation.
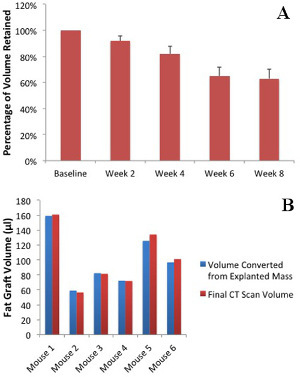 Figure 4. (A) Micro-CT volumetric analysis demonstrated gradual loss of fat graft volume over eight weeks. (B) Final fat graft volumes, as measured by micro-CT, corresponded closely to volumes calculated from the masses of explanted fat grafts. The average density of human fat (0.9 g/ml) was used as a conversion rate.
Figure 4. (A) Micro-CT volumetric analysis demonstrated gradual loss of fat graft volume over eight weeks. (B) Final fat graft volumes, as measured by micro-CT, corresponded closely to volumes calculated from the masses of explanted fat grafts. The average density of human fat (0.9 g/ml) was used as a conversion rate.
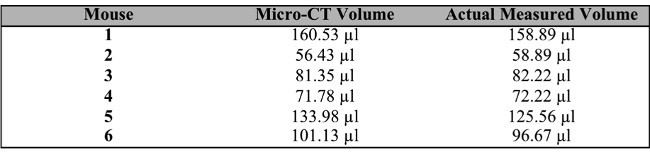 Table 1. Calculated Micro-CT Volume vs. Actual Measured Fat Volume
24
Table 1. Calculated Micro-CT Volume vs. Actual Measured Fat Volume
24
Discussion
Up until this point, most researchers have relied on non-imaging modalities to quantify the long-term survival of fat grafts, but these methods require the sacrifice of the study animal and yield only a single measurement. 3,10-12 Our study represents an improved analysis method that permits objective, real-time quantification of fat graft survival in a mouse model.
Critical in this process is ensuring that sufficiently immunocompromised mice are used for the study, as this prevents the graft rejection that would occur if mice with intact immune systems are used. Preserving fat integrity is critical during the harvest, processing, and placement phases of grafting. In accordance with traditionally accepted standards, fat for grafting should be obtained by suction assisted liposuction (SAL). During placement, fat should be injected at a steady flow rate no faster than 0.5 ml/sec. A 14 gauge cannula is preferred for grafting in a mouse, but larger diameter cannulas may be used without any injury to the fat. Smaller cannulas and needles—especially those narrower than 16 gauge—are discouraged during placement as they may cause the fat to breakdown due to increased shear stress. Although we describe our preferred technique for processing above, any combination of sedimentation, centrifugation, and/or filtration may be used as long as the oil and blood layers are adequately separated out from the fat prior to grafting.
Fat grafts should be at least 200 µl in size to minimize variance in results due to the inconsistent nature of fat grafting. Larger grafts up to 400 µl in size may be used, but above this volume, impaired vascular supply and excessive skin tension may result in fat and skin necrosis. Ultimately, maximum fat graft size will be determined by surface area and volume of the pocket. To increase the volume of a graft that can be safely delivered, the pocket can be expanded by more extensive dissection. However, this may place fat beyond the boundaries of the top of the skull, which will make the contrast between the graft and surrounding tissue less clear. Hence, subsequent voxel selection will become more difficult.
If initial skin incision is small enough, a suture may not be needed as long as fat remains contained and is not seen leaking out of the pocket. If a suture is placed, care must be taken not to tie the first knot too tightly, otherwise skin breakdown may occur. A non-absorbable monofilament suture such as nylon is preferred, as it limits the inflammatory reaction and is less likely to harbor infection. Re-epithelialization of the incision will occur within 24 to 48 hr post-operatively, and the suture may be removed at this time. Absorbable and braided sutures should not be used. Skin should always be handled with the least force necessary, and the surgeon should take care not to crush the skin while holding up wound edges.
Depending on the investigators’ imaging analysis software, the exact relationship between pixel intensity and the density of tissue may vary. Investigators should choose pixel intensity thresholds to obtain a maximum and minimum range that most accurately distinguishes the fat graft from the surrounding tissue. The same maximum and minimum threshold values should be used during all volume analyses to maintain consistency.
There are multiple methods to select graft volume once pixel intensity threshold values have been set. Although we find painting with a brush tool in the sagittal view best in our hands, other voxel selection methods to create an ROI can be used such as drawing with the spline tool or painting in the axial view. It is preferable if a single person performs all volume analyses as consistently as possible in order to reduce measurement error.
The non-invasive nature of this method and the real-time visualization of graft evolution offer significant advantages over traditional techniques. However, this technique is limited in its ability to identify the viability and health of remnant grafts. Furthermore, it cannot demonstrate relative revascularization of grafts. Though changes in appearance and graft density may hint at fat necrosis, infection, cyst formation, or liquefaction, it is difficult to draw exact conclusions from micro-CT alone.
We hope this technique will serve as a foundation upon which future studies can be conducted to better understand the causative factors in fat graft survival and loss. Variations on this theme may elucidate the role that stem cells, growth factors, cytokines, genes, and cell surface markers play in the ultimate preservation of fat graft volume. With this improved tool to test contrasting hypotheses, we look forward to a better understanding of fat transfer that transforms a capricious technique for treating soft tissue deficits into a more predictable one.
Disclosures
None of the authors have any competing financial interest to report.
Acknowledgments
This study was supported by the Oak Foundation, the Hagey Laboratory for Pediatric Regenerative Medicine, and the National Institute of Health, Grants NIHR21DE019274, NIHR01DE019434, NIHR01DE021683, and NIHU01HL099776 to M.T.L. D.C.W. was supported by the ACS Franklin H. Martin Faculty Research Fellowship, the Hagey Laboratory for Pediatric Regenerative Medicine, and the Stanford University Child Health Research Institute Faculty Scholar Award. Micro-CT was conducted at the Stanford Center for Innovation in In Vivo Imaging.
References
- Gir P, et al. Fat grafting: evidence-based review on autologous fat harvesting, processing, reinjection, and storage. Plast Reconstr Surg. 2012;130(1):249–258. doi: 10.1097/PRS.0b013e318254b4d3. [DOI] [PubMed] [Google Scholar]
- Kaufman MR, et al. Autologous fat transfer national consensus survey: trends in techniques for harvest, preparation, and application, and perception of short- and long-term results. Plast Reconstr Surg. 2007;119(1):323–331. doi: 10.1097/01.prs.0000244903.51440.8c. [DOI] [PubMed] [Google Scholar]
- Smith P, et al. Autologous human fat grafting: effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg. 2006;117(6):1836–1844. doi: 10.1097/01.prs.0000218825.77014.78. [DOI] [PubMed] [Google Scholar]
- Eppley BL, Dadvand B. Injectable soft-tissue fillers: clinical overview. Plast Reconstr Surg. 2006;118(4):98e–106e. doi: 10.1097/01.prs.0000232436.91409.30. [DOI] [PubMed] [Google Scholar]
- Yarborough JM. The treatment of soft tissue defects with injectable collagen. Am J Med Sci. 1985;290(1):28–31. doi: 10.1097/00000441-198507000-00001. [DOI] [PubMed] [Google Scholar]
- Baumann DP, Butler CE. Soft tissue coverage in abdominal wall reconstruction. Surg Clin North Am. 2013;93(5):1199–1209. doi: 10.1016/j.suc.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Tukiainen E. Chest wall reconstruction after oncological resections. Scand J Surg. 2013;102(1):9–13. doi: 10.1177/145749691310200103. [DOI] [PubMed] [Google Scholar]
- Zan T, et al. Surgical treatment of facial soft-tissue deformities in postburn patients: a proposed classification based on a retrospective study. Plast Reconstr Surg. 2013;132(6):1001e–1014e. doi: 10.1097/PRS.0b013e3182a97e81. [DOI] [PubMed] [Google Scholar]
- Bucky LP, Percec I. The science of autologous fat grafting: views on current and future approaches to neoadipogenesis. Aesthet Surg J. 2008;28(3):313–321. doi: 10.1016/j.asj.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Lee JH, et al. The effect of pressure and shear on autologous fat grafting. Plast Reconstr Surg. 2013;131(5):1125–1136. doi: 10.1097/PRS.0b013e3182879f4a. [DOI] [PubMed] [Google Scholar]
- Kirkham JC, et al. The impact of liposuction cannula size on adipocyte viability. Ann Plast Surg. 2012;69(4):479–481. doi: 10.1097/SAP.0b013e31824a459f. [DOI] [PubMed] [Google Scholar]
- Medina MA, et al. 3rd et al. Polymer therapy: a novel treatment to improve fat graft viability. Plast Reconstr Surg. 2011;127(6):2270–2282. doi: 10.1097/PRS.0b013e3182139fc1. [DOI] [PubMed] [Google Scholar]
- Horl HW, Feller AM, Biemer E. Technique for liposuction fat reimplantation and long-term volume evaluation by magnetic resonance imaging. Ann Plast Surg. 1991;26(3):248–258. doi: 10.1097/00000637-199103000-00007. [DOI] [PubMed] [Google Scholar]
- Har-Shai Y, Lindenbaum ES, Gamliel-Lazarovich A, Beach D, Hirshowitz B. An integrated approach for increasing the survival of autologous fat grafts in the treatment of contour defects. Plast Reconstr Surg. 1999;104(4):945–954. doi: 10.1097/00006534-199909040-00008. [DOI] [PubMed] [Google Scholar]
- Fontdevila J, et al. Assessing the long-term viability of facial fat grafts: an objective measure using computed tomography. Aesthet Surg J. 2008;28(4):380–386. doi: 10.1016/j.asj.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Meier JD, Glasgold RA, Glasgold MJ. Autologous fat grafting: long-term evidence of its efficacy in midfacial rejuvenation. Arch Facial Plast Surg. 2009;11(1):24–28. doi: 10.1001/archfacial.2008.518. [DOI] [PubMed] [Google Scholar]
- Coleman SR. Structural fat grafts: the ideal filler. Clin Plast Surg. 2001;28(1):111–119. [PubMed] [Google Scholar]
- Coleman SR. Structural fat grafting: more than a permanent filler. Plast Reconstr Surg. 2006;118(3 Suppl):108S–120S. doi: 10.1097/01.prs.0000234610.81672.e7. [DOI] [PubMed] [Google Scholar]
- Pu LL, Coleman SR, Cui X, Ferguson RE, Vasconez HC. Autologous fat grafts harvested and refined by the Coleman technique: a comparative study. Plast Reconstr Surg. 2008;122(3):932–937. doi: 10.1097/PRS.0b013e3181811ff0. [DOI] [PubMed] [Google Scholar]
- Matsumoto D, et al. Cell-assisted lipotransfer: supportive use of human adipose-derived cells for soft tissue augmentation with lipoinjection. Tissue Eng. 2006;12(12):3375–3382. doi: 10.1089/ten.2006.12.3375. [DOI] [PubMed] [Google Scholar]
- Yoshimura K, Suga H, Eto H. Adipose-derived stem/progenitor cells: roles in adipose tissue remodeling and potential use for soft tissue augmentation. Regen Med. 2009;4(2):265–273. doi: 10.2217/17460751.4.2.265. [DOI] [PubMed] [Google Scholar]
- Zuk PA, et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7(2):211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- Habte F, et al. Impact of a multiple mice holder on quantitation of high-throughput MicroPET imaging with and without Ct attenuation correction. Mol Imaging Biol. 2013;15(5):569–575. doi: 10.1007/s11307-012-0602-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung MT, et al. Micro-computed tomography evaluation of human fat grafts in nude mice. Tissue Eng Part C Methods. 2013;19(3):227–232. doi: 10.1089/ten.tec.2012.0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thanik VD, et al. A murine model for studying diffusely injected human fat. Plast Reconstr Surg. 2009;124(1):74–81. doi: 10.1097/PRS.0b013e3181a80509. [DOI] [PubMed] [Google Scholar]


