Abstract
Purpose
Sleep disturbances are a common problem during adolescence. Often there is a relationship with the mental health of the affected person. The existing literature concerning the link between sleep disturbances and aggressive behavior and sleep disturbances and suicidality during adolescence shows no clear results. The present study tested a mediation model to prove the relation between sleep problems, aggressive behavior, and suicidality during adolescence. To take the link between suicidality and depression into account, the amount of depressive symptoms was included into the mediation model.
Methods
A sample of 93 adolescents aged 14–18 years (30% male) was studied. A survey was conducted to interview the adolescents about their mental health, sleep-related behaviors, aggressive behavior, and suicidality.
Results
Sleep problems and suicidality measures were significantly related to each other. Furthermore, aggressive behavior and suicidality showed a significant relationship. The expected link between sleep problems and aggressive behavior was not significant. For the mediation model, no significant influence of aggressive behavior on the relationship between the amount of sleep problems and suicidality was found. However, the impact of depressive symptoms on the relationship between sleep problems and suicidality was significant.
Conclusion
Sleep problems and overall suicidality in adolescents are significantly connected, even after adjusting for several possible influencing factors. Aggressive behavior could not be confirmed as a mediator for the association between sleep problems and suicidality in adolescents. Further studies to examine the link between insomnia symptoms, aggressive behavior, and suicidality in adolescents are necessary.
Keywords: adolescents, aggressive behavior, sleep problems, suicidality, depression
Introduction
Many processes that are important for human well-being take place during sleep. The whole function of sleep is not entirely clear, but some functions have been verified – for example, its role for information processing,1 memory consolidation,2–4 and learning processes.5,6 It is already known that sleep disturbances have negative effects on quality of life and psychosocial functioning.7,8 Despite the growing amount of research results for children and adolescents, there is still the need to examine the associations between sleep disturbances and their related consequences for this age group. Various findings already show that sleep problems are quite common in this population and they tend to last for long periods of time.8,9 Furthermore, there is a link between sleep disruptions and psychological disturbances.7,10–12
However, the specific link between sleep and aggression during childhood, adolescence, and adulthood has received less attention from research to date. Only a few studies with specific populations have examined the connection between aggression and sleep in adolescents. Haynes et al13 examined a sample of 23 (57% male) adolescents aged 13–19 years who had recently successfully completed substance abuse treatment. The authors’ interest was focused on assessing whether aggression was associated with a change in total sleep time during the course of behavioral sleep treatment. Adolescents who reported more aggression ideation also reported less total sleep time and less time in bed than adolescents showing less aggressive actions.13 When controlling for baseline aggression and frequency of substance abuse, there was still a link between the insufficient amount of sleep and aggressive behavior occurring later in adolescents. The authors concluded that successful sleep-problem treatment could be a crucial element in violence prevention. Furthermore, they stated that inadequate sleep led to a possible predisposition in adolescents for affective and behavioral disinhibition.13
Another study carried out by Ireland and Culpin14 assessed a sample of 80 juvenile (14–17-year-old) and 104 young (18–20-year-old) male offenders with regard to their sleeping behavior before and during their time in custody. The researchers examined the link between quantity and quality of sleep with aggression, anger, and impulsivity. They found that increased aggression measures were associated with reduced sleep. These results showed evidence that sleep quality and quantity are predicted by overall aggression measures. There were also hints of differences in sleep behavior before and during imprisonment, with some evidence pointing to poorer sleep during detention.14 Meijer et al15 conducted a longitudinal study over a period of 2 years examining the influence of age, sex, time in bed, and sleep quality on different problem behaviors during adolescence. In total, 650 adolescents (50.5% male) between 12 years and 15 years of age participated in the baseline assessment, and 2 years later, 493 adolescents (49.3% male) participated in the last measurement point. The authors’ results showed a link between poor sleep quality and overall problem behaviors in adolescents. Furthermore, the combination of less time in bed and low sleep quality at the baseline assessment was conducive to more aggressive behavior in boys. In general, the data showed that delinquent and aggressive behaviors were more likely when time in bed was shorter.15 The aforementioned studies showed some important points in the research regarding the link between sleep and aggression. Kamphuis et al16 concluded in their review that successful sleep-problem treatment can reduce aggression during the day. In their opinion, this supports the hypothesis that sleep problems are a risk factor for aggression.
The literature on the association between sleep and suicide or suicidal behavior during adolescence is sparse and exhibits mixed results.17–23 Some research results indicate the existence of an association between sleep and completed suicide or suicidal behavior, while one other study found no association after adjusting for demographic variables and depressive symptoms. Vignau et al21 examined a sample of 744 adolescents and young adults (59% male) aged 15–23 years. In contrast to the group of good sleepers (GP), poor sleepers (PS) showed significantly elevated rates for suicidal ideas (PS 38% versus GS 15%) and suicide attempts (PS 9% versus GS 1%). A large study conducted with 5,423 adolescents (51.2% male) aged 10–17 years was conducted by Roberts et al.20 They found that adolescents suffering from insomnia had a 3.41 times higher risk of having suicidal ideation compared to adolescents without sleep complaints. This result remained significant after controlling for sex, age, socioeconomic status, and other variables, with an odds ratio of 1.46 supporting the link between insomnia and suicide ideation.20
The link between completed suicide and sleep disturbances in adolescents was also studied by Goldstein et al.18 They assessed the data of 140 suicide completers (85% male) aged 13–19 years and 131 matched community controls (70% male). Significantly higher rates of insomnia in the suicide completer group compared to the control group were found. The association between suicide and sleep problems remained significantly elevated, even after controlling for the severity of depressive symptoms.18 These results support the assumption that there is a link between sleep and suicide in adolescents besides the influence of depressive symptoms. Another study assessed cross-sectional data for 12,154 and 14,782 adolescents in 2007 and 2009, respectively.17 The authors’ results indicated that short and long total sleep durations were associated with an increased risk for suicidality in adolescents for both years, and after adjusting for several confounding variables.17 Wong et al23 found that suicidal thoughts at 15–17 years of age were significantly predicted by having trouble sleeping from the ages of 12–14 years. In addition, a longitudinal investigation by Wong et al22 used data from 6,504 adolescents. The authors were able to reveal that sleep disturbances at the first assessment point significantly predicted suicidality at the second point, 1–2 years later, and at the third assessment point, 5–6 years later, after controlling for depressive symptoms and other possible influencing factors.22
In contrast to this, the study by Liu19 showed different results. The author surveyed a sample of 1,362 adolescents (60% male) aged 12–16 years. About 30.9% of adolescents with insomnia also reported suicidal ideation. When calculating univariate logistic regression, insomnia and suicidal ideation were significantly related to each other. However, after controlling for demographic variables and depressive symptoms, this relationship did not remain significant.19 In their review, Liu and Buysse24 concluded that it is a reasonable hypothesis that sleep disturbances or sleep deprivation are linked to a heightened risk for suicidal behavior during adolescence, even though most of the studies were conducted with special groups of adolescents.
The latest research literature shows that there is a relationship between the amount of depressive symptoms and suicidality in adolescents. Depressive symptoms were found to be a significant predictor of suicide attempts in adolescents.25 Furthermore, even mild depressive symptoms are associated with heightened suicidal ideation.26 Therefore, depressive symptoms were included as a possible mediating factor in this study.25,26
Bridge et al27 carried out a detailed literature review on the protective and risk factors for suicide and suicidal behavior in youth, resulting in a developmental–transactional model of youth suicidal behavior. This model of youth suicide takes two different groups of interacting, but still independent, vulnerability factors into account: major psychiatric disorders (mainly mood disorders) on the one hand; and the tendency to aggression (especially impulsive aggression) on the other hand.27 Therefore, the study at hand focuses on aggression and depression as influencing factors on adolescent suicidal behavior. Based on these results we developed a theoretical model exploring the relationship between sleep problems, aggressive behavior, and suicidality.
In sum, the study at hand was set up as a pilot study and focuses on sleep problems and their relationship with aggression and suicidal tendency in an adolescent sample. Based on previous studies, we hypothesized that 1) there is an existing link between sleep problems and aggressive behavior; 2) there is a link between sleep problems and suicidality; and 3) the amount of aggressive behavior has an impact on the relationship between sleep problems and suicidality in adolescents. Therefore, a mediation model was tested. To control for the possible influence of depression on the relationships inside the mediation model, depression was included as a second mediator.
Methods
Procedure
For this online survey, various standardized instruments were utilized. To distribute the study link, regional newspapers and flyers, which were distributed at different schools in Germany, were used. In order to obtain a higher number of participants, a raffle was linked to the survey. Informed consent was given by all participants before answering the questionnaire. Furthermore, the study followed the Declaration of Helsinki.
Sample
A total of 98 adolescents between 14 years and 18 years of age (mean =15.97 years; standard deviation =1.3 years) took part in the study. After excluding all participants who did not meet the inclusion criteria, the data of 93 adolescents (30.1% male) were included in the data analysis. Inclusion criteria were met when all questionnaires were filled out.
Measures
Sociodemographic data
Before asking sleep-, aggression-, and suicide-related questions, general information about age, sex, type of school (intermediate, secondary, etc), height and weight, and other items were collected (19 questions).
Sleep measures
Sleep and sleep-related problems were assessed with the Pittsburgh Sleep Quality Index (PSQI).28 The PSQI gathers data about sleep onset latency, sleep duration, time of waking up and going to bed, and several other items of sleep-related information during the previous 4 weeks. Seven subscales, as well as the global PSQI score, are generated out of the items. The PSQI global score can range between 0 and 21, with higher scores indicating more sleeping problems. A PSQI global score of 6 or higher indicates poor sleep quality and therefore identifies “poor” sleepers. Internal homogeneity was high with Cronbach’s α=0.83.28 Backhaus et al29 found high overall PSQI test–retest reliability (r=0.87). The subscales “sleep quality” (r=0.53) and “sleep disturbances” (r=0.69) were the only exceptions, with test–retest reliability falling in the middle range.
Aggression measure
To assess aggressive behavior in adolescents, the subscale “aggressive behavior” of the German Questionnaire for Acquiring Empathy, Prosociality, Readiness for Aggression, and Aggressive Behavior (Fragebogen zu Erfassung von Empathie, Prosozialität, Aggressionsbereitschaft und aggressivem Verhalten [FEPAA]30) was used. The FEPAA consists of four subscales measuring empathy, prosociality, readiness for aggression, and aggressive behavior. For the survey at hand, part three “prosociality and aggressive behavior” (13 items for prosociality, 15 items for aggressive behavior) of the parallel form A of the FEPAA was used. Items on the “prosociality and aggressive behavior” subscale had a dichotomous answering pattern – “true” or “not true”. Based on the answers, a sum score ranging between 15 and 30 for the aggressive behavior subscale was calculated, with higher scores indicating more aggressive behavior. Overall reliability of the FEPAA was found to be high with r=0.75.30
Suicide tendency measures
For the assessment of adolescent suicidal tendency, five questions generated by Paykel et al31 were assessed. The following questions were asked: 1) Have you ever felt that life was not worth living?; 2) Have you ever wished you were dead? For instance, that you could go to sleep and not wake up?; 3) Have you ever thought of taking your life, even if you would not really do it?; 4) Have you ever reached the point where you seriously considered taking your life, or perhaps made plans for how you would do it?; and 5) Have you ever made an attempt to take your life? Answers were given on a four-point rating scale with responses ranging from 0= “never” to 3= “often”. Based on these five questions, a sum score ranging from 0–15 for the Paykel Scale was calculated, with higher values indicating more intense suicidal feelings and therefore higher overall suicidality. The raw scores of the five suicide tendency questions were summed up given the correlations among the scores. Cronbach’s alpha for the overall suicidality score was high with α=0.82.
Depression measure
Based on other studies,17,18,20 the “anxiety/depression” subscale of the Youth Self-Report32 was conducted to control for depression as a confounding variable on the link between sleep problems and suicidality.
Analyses
All statistical analyses were performed with SPSS version 22.0 for Windows, and the mediation model was tested with SPSS AMOS, version 22.0 for Windows.
According to Buysse et al,28 who reliably distinguished between good (PSQI global score of 0–5) and poor sleepers (PSQI global score of 6 or higher) using the PSQI global score, we grouped our sample. The PSQI scores ranged from 1–18, resulting in a grouping of 47 good and 46 poor sleeping adolescents.
The Shapiro–Wilk test was used to check for a normal distribution in all relevant variables. All variables showed significant deviation from a normal distribution. According to these results, Mann–Whitney U tests were applied to test group differences for aggressive behavior and suicidality measures.
In order to test for a possible effect of aggressive behavior on the link between the amount of sleep problems and suicidality scores, a mediation model was applied. Given the fact that sleep problems are also a symptom of depression and depressed mood, depression was included in the mediation model. Following this approach, it was possible to evaluate depression as a mediator of the link between sleep problems and suicidality, and to control for its influence on the link between sleep problems and suicidality mediated by aggressive behavior. The PSQI sum score was used to assess the influence of the amount of sleep problems. To test the significance of the standardized coefficients, as well as the direct and indirect effects in the mediation model, bootstrapping with 2,000 iterations was applied. To rate the influence of each mediator separately, and to get separate indirect effects, the phantom model approach was applied.33 The calculated effect sizes were interpreted according to the guidelines proposed by Cohen.34
Results
The median (Mdn), mean, and standard deviation of the PSQI scores for the two groups and the whole sample are depicted in Table 1.
Table 1.
Median, mean, and standard deviation of the PSQI scores
| Group | Median | Mean | Standard deviation |
|---|---|---|---|
| Whole sample | 5 | 6.35 | 3.70 |
| Good sleepers (n=47) | 4 | 3.74 | 1.20 |
| Poor sleepers (n=46) | 8 | 9.02 | 3.48 |
Abbreviations: PSQI, Pittsburgh Sleep Quality Index; n, number.
Sleep and aggressive behavior
First, we compared good sleeping adolescents with poor sleeping adolescents. The results showed no significant differences in the amount of aggressive behavior between these two groups (U=1,087.500, not significant; r=0.005) (Table 2).
Table 2.
Results of the Mann–Whitney U tests comparing aggressive behavior and suicidality in good and poor sleepers
| Good sleepers (n=47)
|
Poor sleepers (n=46)
|
U | Z | P | r | |
|---|---|---|---|---|---|---|
| Median | Median | |||||
| Aggressive behavior | 17.00 | 17.00 | 1,087.500 | 0.051 | 0.960 | 0.005 |
| Suicidality | 2.00 | 5.00 | 1,554.00 | 3.667 | <0.001* | 0.380 |
Notes: U = the Mann–Whitney U test statistic; Z = the Mann–Whitney U test Z-score. P = significance; r = effect size. P is the two-tailed significance. *Significance level P<0.05.
Abbreviation: n, number.
Sleep and suicidality
In a next step, suicidality scores between good and poor sleepers were compared. The Mann–Whitney U test results showed that adolescents in the poor sleeper group (Mdn =5.00) had significantly higher scores on suicidality measures (U=1,554.000; P<0.000; r=0.380) when compared to the adolescents sleeping well (Mdn =2.00), with a medium effect size. Table 2 gives an overview of the results of the Mann–Whitney U tests of the group comparisons in good versus bad sleepers for aggressive behavior and suicidality scores.
Sleep, aggressive behavior, and suicidality
Furthermore, based on previous findings, we tested the theoretical model that the relationship between sleep problems and overall suicidality in adolescents is mediated by aggressive behavior and depression. An overview of the unstandardized and standardized coefficients and effects for the full mediation model is given in Table 3.
Table 3.
Unstandardized and standardized coefficients, as well as the total, direct, and indirect effect of the full mediation model
| Regression coefficient
|
Standardized regression coefficient
|
||||
|---|---|---|---|---|---|
| B | SE | P | β | P | |
| SP->suicide | 0.220 | 0.092 | 0.021* | 0.192 | 0.021* |
| Aggr->suicide | 0.250 | 0.106 | 0.012* | 0.175 | 0.012* |
| Depr->suicide | 0.361 | 0.052 | 0.001* | 0.564 | 0.001* |
| SP->Aggr | 0.029 | 0.084 | 0.702 | 0.036 | 0.702 |
| SP->Depr | 0.695 | 0.172 | 0.001* | 0.389 | 0.001* |
| Β | LLCI | ULCI | P | ||
|
| |||||
| Total effect | |||||
| SP->suicide | 0.418 | 0.177 | 0.619 | 0.001* | |
| Direct effect | |||||
| SP->suicide | 0.192 | 0.025 | 0.374 | 0.021* | |
| Indirect effect (via Aggr and Depr) | |||||
| SP->suicide | 0.226 | 0.093 | 0.356 | 0.002* | |
Notes: B = regression coefficient; β = standardized regression coefficient P = significance.
Significance level P<0.05.
Abbreviations: SE, standard error; SP, sleep problems; Aggr, aggression; Depr, depression; LLCI, lower-level confidence interval; ULCI, upper-level confidence interval.
Regression analyses
First, regression analyses with 2,000 bootstrap iterations for the mediation model were calculated. The amount of sleep problems (SP) showed a significant standardized influence on adolescent suicidality (suicide) (βSP−>suicide=0.192; P=0.021) and the amount of aggressive behavior (aggr) also showed a significant influence on suicidality (βaggr−>suicide=0.175; P=0.012). Furthermore, a high significant effect of depressive symptoms (depr) on adolescent suicidality was found (βdepr−>suicide=0.564; P=0.001). Besides these results for the influences on adolescent suicidality, the regression analyses revealed a nonsignificant effect of sleep problems on aggressive behavior (βSP−>aggr=0.036; P=0.702) and a significant effect of sleep problems on depressive symptoms in adolescents (βSP−>depr=0.389, P=0.001).
Mediation effects
The total standardized effect of sleep problems on adolescent suicidality was fairly high and significant (βSP−>suicide=0.418; P=0.001). This result remained significant for the direct effect of sleep problems on suicidality (βSP−>suicide=0.192; P=0.021). Since aggressive behavior and depression were included in the full mediation model, the indirect effect of sleep problems on suicidality was the total effect of the mediators, aggressive behavior and depression, together. The indirect effect of sleep problems on suicidality in adolescents for the full mediation model was still significant (βSP−>suicide=0.226; P=0.002), which points toward a partial mediation. Almost 50% of the variance in adolescent suicidality can be explained by the full mediation model (R2=0.495; P=0.001). The phantom model approach showed that for aggressive behavior, the indirect effect was very small and not statistically significant (β=0.032; P=0.710).33 The indirect effect of depression was larger and statistically significant (β=0.533; P=0.001). These results present depression as a partial mediator of the relationship between sleep problems and suicidality, whereas aggressive behavior could not be confirmed as a mediator. The results for the complete mediation model with depression and aggressive behavior included as the mediators are shown in Figure 1.
Figure 1.
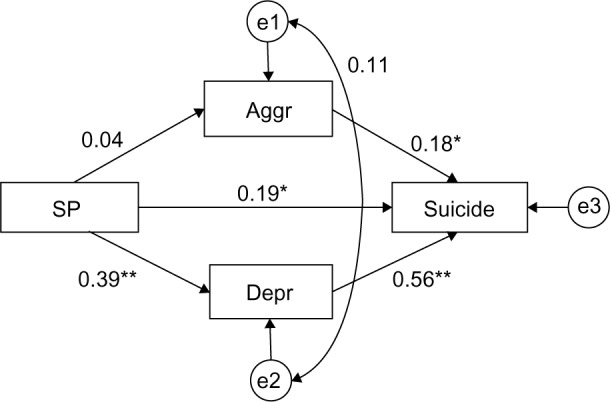
Full mediation model of SP, Aggr, Depr, and suicide.
Notes: *P<0.05; **P<0.001.
Abbreviations: SP, sleep problems; Aggr, aggression; Depr, depression; suicide, suicidality; e1, e2, e3, residuals.
Discussion
The present study was based on the latest research results and aimed to examine the association between insomnia symptoms, aggressive behavior, and suicidality in adolescents. In particular, the link between sleep problems and aggressive behavior, and sleep problems and suicidality in adolescents was examined. Another point of interest was the relationship between sleep problems, aggressive behavior, and suicidality. A mediation model was applied to examine this link more closely. Depression was included as a second potential mediator to control for its influence on the relationship between sleep problems and suicidality.
Contrary to our expectations and the results of other studies,13–15,35 the amount of aggressive behavior did not significantly differ between good and poor sleeping adolescents. However, it is necessary to keep in mind that the results of previous studies on the relationship between sleep problems and aggression/aggressive behavior were based on data from special populations (eg, Haynes et al,13 and Ireland and Culpin14).
The degree of suicidality in our study was significantly higher in poor sleeping adolescents when compared to good sleeping adolescents. This result was in line with our expectations and the results from the existing research literature.18,20,21 Previous studies assessed different aspects of suicidality. The results are therefore very diverse. Some researchers examined adolescents who committed suicide.18,36,37 Other researchers asked only one question regarding suicide.21,38 Nock et al39 implemented three suicide-related questions concerning suicide ideation, suicide plans, and suicide attempts. A strength of the study at hand is the application of the standardized Paykel Scale as a measure for suicidality.31 Furthermore, a sum score of the five Paykel questions was used to assess the amount of overall suicidality in adolescents in order to obtain the best possible measure.
A mediation model was applied to test whether aggressive behavior mediates the relationship between sleep problems and suicidality in adolescents. To control for the influence of depression on this relationship, we included depression as a second mediator in the mediation model. The full mediation model with aggressive behavior and depression as mediators was able to explain ~50% of the variation in suicidality measures. The direct effect of sleep problems on the amount of suicidality was not very high, but it was statistically significant. This result indicates that there is an effect of sleep problems on the amount of suicidality, which is in addition to the influence of aggressive behavior and depression on this relationship. Looking at the indirect effect of the influence of aggressive behavior on the relationship between sleep problems and suicidality, no significant indirect effect was found. Contrary to our expectations, aggressive behavior is not a mediator of the assessed relationship. Conversely, the second indirect effect between sleep problems and suicidality mediated by depression was high and statistically significant. In conclusion, depression can be interpreted as a mediator. Summarizing the mediation model, a partial mediation of the relationship between sleep problems and suicidality was detected, and this was mediated by depression but not by aggressive behavior. Moreover, there is a link between sleep problems and suicidality in adolescents, which is in addition to the influence of depression. These results can be added to the existing research literature.
In particular, the association between sleep problems, aggressive behavior, and suicidality in adolescents received no research attention to date. The links between sleep problems and aggression,13–15 sleep problems and suicidality,16,20,37 and aggressive behavior and suicidality39 already got some, even though sparse, research attention. The present study went a step further and assessed the link between sleep problems, aggressive behavior, and suicidality combined, within a nonspecialized adolescent sample.
Limitations
Like other studies, the study at hand has some limitations, too. The analyses of the present study are exclusively based on self-report measures for all of the assessed variables, which can be seen as a methodological restriction. Self-reported aggression measures can be especially critical because, for example, social expectancy can influence the answers given in self-report measures when compared to objective measures.40
Another methodological limitation is the sample. A sample size of 93 is not critical when the calculations include all of the participants. However, the good sleeper and bad sleeper comparisons used only 47 and 46 participants for the calculations, respectively. Conclusions from the study at hand can therefore only partially be generalized to all adolescents.
Furthermore, based on previous studies, in the present study, we only assessed aggressive behavior, which is only one aspect of the construct of aggression. Future studies should take the differences in aggression measures into account when measuring aggression. The focus could be on different aspects of aggression and how they differ with regard to their influence on sleep and sleep problems. Alternatively, future research could focus on one single aspect of aggression and its influence on insomnia symptoms, thus requiring data collection on only one aspect of aggression.
As was discussed previously, subsequent studies need to verify the methodological aspects used in order to assess the association between sleep problems, aggressive behavior, and suicidality more closely. One important step would be the use of different sleep disturbance and aggression measures.
Conclusion
All in all, this study shows that sleep problems are significantly associated with overall suicidality in adolescents, even after adjusting for aggressive behavior and depressive symptoms. Aggressive behavior does not influence the relationship between sleep problems and suicidality, despite its own significant association with overall suicidality. These results show that it is necessary to conduct subsequent studies to further examine and assess the link between sleep problems, aggression, and suicidality. In order to prevent adolescent suicidal behavior or adolescent suicide death, it is essential to implement the assessment of sleep and possible sleep disturbances into general practice and in regularly performed health assessments.
Acknowledgments
We acknowledge support for the Article Processing Charge by the Deutsche Forschungsgemeinschaft and the Open Access Publication Fund of Bielefeld University. The authors wish to thank all the adolescents in this study for their time.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Maddox WT, Glass BD, Wolosin SM, et al. The effects of sleep deprivation on information-integration categorization performance. Sleep. 2009;32(11):1439–1448. doi: 10.1093/sleep/32.11.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nissen C, Kloepfer C, Feige B, et al. Sleep-related memory consolidation in primary insomnia. J Sleep Res. 2011;20:129–136. doi: 10.1111/j.1365-2869.2010.00872.x. [DOI] [PubMed] [Google Scholar]
- 3.Rasch B, Born J. About sleep’s role in memory. Physiol Rev. 2013;93(2):681–766. doi: 10.1152/physrev.00032.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker MP, Stickgold R. Sleep, memory, and plasticity. Annu Rev Psychol. 2006;57:139–166. doi: 10.1146/annurev.psych.56.091103.070307. [DOI] [PubMed] [Google Scholar]
- 5.Brawn TP, Fenn KM, Nusbaum HC, Margoliash D. Consolidating the effects of waking and sleep on motor-sequence learning. J Neurosci. 2010;30(42):13977–13982. doi: 10.1523/JNEUROSCI.3295-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill CM, Hogan AM, Karmiloff-Smith A. To sleep, perchance to enrich learning? Arch Dis Child. 2007;92(7):637–643. doi: 10.1136/adc.2006.096156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41(8):964–971. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Roberts RE, Roberts CR, Duong HT. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42(3):294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, Largo RH. A longitudinal study of bed sharing and sleep problems among Swiss children in the first 10 years of life. Pediatrics. 2005;115(Suppl 1):233–240. doi: 10.1542/peds.2004-0815E. [DOI] [PubMed] [Google Scholar]
- 10.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16(2):129–136. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Ohayon MM, Roberts RE, Zulley J, Smirne S, Priest RG. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39(12):1549–1556. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Quach J, Hiscock H, Canterford L, Wake M. Outcomes of child sleep problems over the school-transition period: Australian population longitudinal study. Pediatrics. 2009;123(5):1287–1292. doi: 10.1542/peds.2008-1860. [DOI] [PubMed] [Google Scholar]
- 13.Haynes PL, Bootzin RR, Smith L, Cousins J, Cameron M, Stevens S. Sleep and aggression in substance-abusing adolescents: results from an integrative behavioral sleep-treatment pilot program. Sleep. 2006;29(4):512–520. [PubMed] [Google Scholar]
- 14.Ireland JL, Culpin V. The relationship between sleeping problems and aggression, anger, and impulsivity in a population of juvenile and young offenders. J Adolesc Health. 2006;38(6):649–655. doi: 10.1016/j.jadohealth.2005.05.027. [DOI] [PubMed] [Google Scholar]
- 15.Meijer AM, Reitz E, Deković M, van den Wittenboer GL, Stoel RD. Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. J Child Psychol Psychiatry. 2010;51(11):1278–1286. doi: 10.1111/j.1469-7610.2010.02261.x. [DOI] [PubMed] [Google Scholar]
- 16.Kamphuis J, Meerlo P, Koolhaas JM, Lancel M. Poor sleep as a potential causal factor in aggression and violence. Sleep Med. 2012;13(4):327–334. doi: 10.1016/j.sleep.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 17.Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and suicidality: results from the youth risk behavior surveys of 2007 and 2009. J Clin Sleep Med. 2011;7(4):351–356. doi: 10.5664/JCSM.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76(1):84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27(7):1351–1358. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 20.Roberts RE, Roberts CR, Chen IG. Functioning of adolescents with symptoms of disturbed sleep. J Youth Adolesc. 2001;30(1):1–18. [Google Scholar]
- 21.Vignau J, Bailly D, Duhamel A, Vervaecke P, Beuscart R, Collinet C. Epidemiologic study of sleep quality and troubles in French secondary school adolescents. J Adolesc Health. 1997;21(5):343–350. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 22.Wong MM, Brower KJ, Zucker RA. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res. 2012;46(7):953–959. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. 2011;45(4):505–511. doi: 10.1016/j.jpsychires.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu X, Buysse DJ. Sleep and youth suicidal behavior: a neglected field. Curr Opin Psychiatry. 2006;19(3):288–293. doi: 10.1097/01.yco.0000218600.40593.18. [DOI] [PubMed] [Google Scholar]
- 25.Kim HS, Kim HS. Risk Factors for Suicide Attempts among Korean Adolescents. Child Psychiaty Hum Dev. 2008;39:221–235. doi: 10.1007/s10578-007-0083-4. [DOI] [PubMed] [Google Scholar]
- 26.Cukrowicz KC, Schlegel EF, Smith PN, et al. Suicide ideation among college students evidencing subclinical depression. J Am Coll Health. 2011;59(7):575–581. doi: 10.1080/07448481.2010.483710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3–4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 29.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53(3):737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 30.Lukesch H. FEPAA – Fragebogen zur Erfassung von Empathie, Prosozialität, Aggressionsbereiteschaft und aggressivem Verhalten [FEPAA - Questionnaire for acquiring empathy, prosociality, readiness for aggression and aggressive behavior] Göttingen. Germany: Hogrefe Verlag; 2006. [Google Scholar]
- 31.Paykel ES, Myers JK, Lindenthal JJ, Tanner J. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124(0):460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 32.Working group German Child Behavior Checklist . Questionnaire for adolescents; German Adaption of the Youth Self-Report (YSR) of the Child Behavior Checklist. In: Döpfner M, Plücke J, Bölte S, Len K, Melchers P, Heim K, editors. Introduction and instruction for scoring by hand. 2nd edition. Cologne, Germany: Working group children, adolescents, and family diagnostic; 1998. [Google Scholar]
- 33.Macho S, Ledermann T. Estimating, testing, and comparing specific effects in structural equation models: the phantom model approach. Psychol Methods. 2011;16(1):34–43. doi: 10.1037/a0021763. [DOI] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 35.Coulombe JA, Reid GJ, Boyle MH, Racine Y. Sleep problems, tiredness, and psychological symptoms among healthy adolescents. J Pediatr Psychol. 2011;36(1):25–35. doi: 10.1093/jpepsy/jsq028. [DOI] [PubMed] [Google Scholar]
- 36.Brent DA, Johnson BA, Perper J, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33(8):1080–1086. doi: 10.1097/00004583-199410000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Renaud J, Berlim MT, McGirr A, Tousignant M, Turecki G. Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: a case-control study. J Affect Disord. 2008;105(1–3):221–228. doi: 10.1016/j.jad.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 38.An H, Ahn JH, Bhang SY. The association of psychosocial and familial factors with adolescent suicidal ideation: A population-based study. Psychiatry Res. 2010;177(3):318–322. doi: 10.1016/j.psychres.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 39.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muntaner C, Walter D, Nagoshi C, Fishbein D, Haertzen CA, Jaffe JH. Self-report vs laboratory measures of aggression as predictors of substance abuse. Drug Alcohol Depend. 1990;25(1):1–11. doi: 10.1016/0376-8716(90)90133-y. [DOI] [PubMed] [Google Scholar]


