Abstract
Background/Aims
We compared the accuracy of US to 3 T Tesla MRI for the detection of rotator cuff and long biceps tendon pathologies before joint replacement.
Methods
45 patients were prospectively included.
Results
For the supraspinatus tendon, the accuracy of US when using MRI as reference was 91.1%. For the infraspinatus tendon, the accuracy with MRI as reference was 84.4%. The subscapularis tendon was consistently assessed by US and MRI in 35/45 patients (accuracy 77.8%). For the long biceps tendon the accuracy was 86.7%.
Conclusion
US detection of rotator cuff and biceps tendon integrity is comparable to MRI and should be preferred in revision cases.
Keywords: Rotator cuff, Ultrasound, MRI, Shoulder, Supraspinatus
1. Introduction
Before implantation of shoulder prostheses imaging techniques routinely include plain X-rays and computed tomography (CT) for the assessment of the osseous structure whereby magnetic resonance imaging (MRI) is used to evaluate the soft tissues, especially the integrity of the rotator cuff and its degree of fatty degeneration. These imaging techniques are usually combined upon availability.
Although MRI nowadays is the reference standard for the diagnosis of a rotator cuff lesion, it is expensive, time-consuming and not always available. Also, there are patients that suffer from claustrophobia and do not sustain the examination, other have MRI contraindications, such as pacemakers or cochlea implants. A recent study showed a similar diagnostic performance of CT Arthrography in comparison to a 1.5 T MRI with respect to full thickness and partial thickness supraspinatus tears.1 Examination of the shoulder by ultrasound (US) has so far only been established as an additional diagnostic tool in the preoperative assessment.
Up to date studies of US for detection of rotator cuff lesions showed controversial results.2,3 Especially in older patients with chronic and degenerative changes the results were not satisfying.4 A recent meta-analysis reported that on present level of knowledge MRI has the best sensitivity and comparable specificity for the detection of full- and partial-thickness tears of the rotator cuff.5 This encouraged us to explore the accuracy of US in comparison to MRI as gold standard for detection of supraspinatus, infraspinatus and subscapularis tears as well as pathologies of the long head biceps tendon. As 1.5 T MRI has already shown high accuracy in the investigation of rotator cuff tears, we considered 3 T MRI with higher resolution to be the appropriate gold standard for this study.6 To our knowledge this is the first study to evaluate if US can substitute the MRI before total shoulder replacement with regard to the supraspinatus, infraspinatus and subscapularis tendon as well as the long biceps tendon.
2. Patients and methods
Patients with osteoarthritis of the glenohumeral joint and scheduled joint replacement were prospectively enrolled after giving their written informed consent. Exclusion criteria were contraindications to MRI such as pacemakers and ICD implants, metal fragments, vascular clips, cochlear implants, claustrophobia, pregnancy during the first trimester and large tattoos at the shoulder girdle, chest or the neck.
Within a six months period 45 consecutive patients were prospectively included (28 women, 17 men; mean age 68.3 years, range 49–81 years). 25 patients had right-sided and 20 patients left-sided shoulder osteoarthritis (Table 1). Before surgery, all study patients received both a dedicated US and MRI examination of the affected shoulder. Derived from the Snyder classification the tendons of supraspinatus, infraspinatus and subscapularis tendons were classified into full-thickness tears, partial-thickness tears, or intact. The same criteria were applied for the US and MRI assessment. The localization of partial-thickness tears was additionally evaluated (articular- vs. bursal-sided). Pathologies of the long biceps tendon were classified into tendovaginitis, rupture, dislocation, or normal condition.
Table 1.
Study population.
| Included patients | 45 | Female 28 Male 17 |
| Age (years) | Mean 68.3 |
Range 49–81 |
| Localization of osteoarthritis | Left 20 |
Right 25 |
| Handedness | Left 20 |
Right 25 |
| Prosthesis type | Total arthroplasty 29 |
Hemi-arthroplasty 16 |
| Prosthesis design | Anatomical 17 |
Reversed 12 |
Reverse prostheses were implanted in case of a complete supraspinatus rupture in preoperative MRI. All other patients received anatomical prostheses, of which hemi-prostheses were used in shoulders with an intact glenoid. In total 16 hemi-prostheses and 29 total shoulder prostheses were implanted of which 17 patients received an anatomical prosthesis and 12 patients a reverse prosthesis.
2.1. Ultrasound
The US examination was performed by the same consultant orthopedic surgeon with over ten years of experience in US of the shoulder without knowledge of the MRI results. All US examinations were performed with a 10 MHz linear transducer on the same US system (Logiq P5, GE Healthcare, Munich/Germany). This transducer is best suitable to detect any type of rotator cuff tear.7 Patients were placed on a chair in line of sight of the device monitor. During the standardized dynamic US examination the arm was passively rotated in the shoulder with the elbow flexed at 90°. Six standard planes (anterior, lateral and posterior, longitudinal and transverse) were used to assess the tendons of the rotator cuff and the long biceps as recommended by the ESSR US guidelines (www.essr.com).
A criterion for a tear of the rotator cuff was a hypoechoic area which persisted in two different planes. A full-thickness tear was defined by a continuous hypoechoic area from the bursal space to the articular surface, thus a complete absence of the tendon. A partial-thickness tear was diagnosed by a defect on the bursal side of the cuff or a hypoechoic, respectively a mixed hypoechoic and hyperechoic area on the articular sided cuff portions.8,9 A tendovaginitis of the long biceps tendon showed a hypoechoic, fluid filled area around the tendon. The criterion for a rupture was the absence of the tendon in the intertubercular groove. In case of dislocation, the tendon was always found medial to the groove.
2.2. Magnetic resonance imaging
MRI examinations were performed on the same 3 T whole-body MR system (MAGNETOM Verio, Siemens Healthcare, Erlangen/Germany). The rotator cuff and biceps tendon were evaluated using three imaging planes including two proton-density-weighted fat-saturated turbo-spin-echo (PD TSE) sequences (in coronal and axial orientation), a coronal T1-weighted spin-echo sequence, and a T2-weighted TSE sequence in sagittal and axial orientation. MRI has been reported to be highly sensitive and specific for the detection of full-thickness and partial-thickness tears of the supraspinatus tendon.10 The evaluation of the MRI scans was performed by a consultant musculoskeletal radiologist with 13 years of experience in the diagnostic investigation of MRI of the shoulder. The classification and the diagnostic results were obtained using all available sequences and imaging planes.
The criteria for a rotator cuff tear were increased signal intensity in association with a discontinuity or irregularity of the tendon on T2- and PD TSE-weighted images. A full thickness tear was diagnosed by a continuous tendon gap that connects the bursal space with the articular surface. A partial-thickness tear showed a high signal intensity in T2-weighting and fat suppressed PD-weighted images within the tendon substance without retraction of the tendon.11 Tendovaginitis of the long biceps tendon was diagnosed when increased signal was present within the tendon sheath on T2-weighted sequences. The biceps tendon was primarily evaluated on the transverse planes.
2.3. Statistics
Descriptive statistics (mean, standard deviation, median, range) were provided where appropriate. The empirical distribution of age was reported with mean, standard deviation (SD) and range, with absolute and relative frequencies in case of categorical variables. Agreement of the scores measured with different methods was evaluated using Kappa statistic and McNemar-test (Bowker-test in case of more than two categories). In all statistical tests, an effect was considered to be statistically significant if the p-value was 0.05 or less. P-values were not adjusted for multiple testing and interpretation of p-values was explorative.
To evaluate the sensitivity and specificity of the US for detection of any supraspinatus, infraspinatus or subscapularis tendon damage we pooled full-thickness-tears and partial-thickness-tears to one entity. To compare the classification of supraspinatus, infraspinatus and subscapularis tendons in US and MRI to intraoperative findings we also pooled full-thickness and partial-thickness tears to one entity. To calculate the sensitivity and specificity of US for the detection of long biceps pathologies we pooled tendovaginitis, dislocation and ruptures. Data analysis and statistical evaluation were performed with SPSS, version 18 (SPSS Inc., Somers, NY).
3. Results
The statistical analysis of the box tables showed a high level of agreement between MRI and US with kappa-values >0.57. The p-value served as a measure of symmetry of the panels, p-values >0.05 indicated high symmetry values and argued against a tilting of the panel (Table 2).
Table 2.
Kappa and p-values for the comparison of US with MRI.
| Comparison | Kappa | p |
|---|---|---|
| Supraspinatus rupture | 0.85 | 0.26 |
| Supraspinatus partial-thickness tear localization | 0.85 | 0.68 |
| Infraspinatus rupture | 0.71 | 0.39 |
| Subscapularis rupture | 0.57 | 0.88 |
| Long biceps tendon integrity | 0.75 | 0.32 |
The comparison of MRI and US showed the following results with high kappa- and p-values:
3.1. Supraspinatus tendon
MRI revealed 22 (48.89%) full-thickness tears and seven (15.56%) partial-thickness tears (Table 3). US revealed 24 full-thickness tears (53.33%) and three partial-thickness tears (6.67%). Full-thickness tears were classified similarly in 22 patients (Fig. 1). Two tendons, which seemed to be totally torn in US, manifested in MRI as partial-thickness tears. In three cases partial-thickness tears were similarly classified by US and MRI. US consistently assessed the supraspinatus tendon to MRI in 41/45 cases (accuracy of US when using MRI as reference = 91.1%, kappa = 0.85, p = 0.26).
Table 3.
Comparison of supraspinatus tear-type in US with MRI.
| Supraspinatus tendon | ||||
|---|---|---|---|---|
| US |
MRI |
Total | ||
| n (%) | No tear | Partial-thickness tear | Full-thickness tear | |
| No tear | 16 (35.56) | 2 (4.44) | 0 | 18 (40.00) |
| Partial-thickness tear | 0 | 3 (6.67) | 0 | 3 (6.67) |
| Full-thickness tear | 0 | 2 (4.44) | 22 (48.89) | 24 (53.33) |
| Total | 16 (35.56) | 7 (15.56) | 22 (48.89) | 45 (100.00) |
Fig. 1.
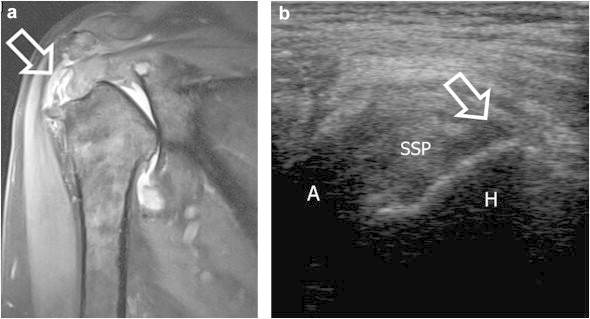
Full-thickness supraspinatus tear. Coronal PD-TSE-weighted MRI plane (a) and transverse US image (b). The arrows point out the rupture, hyperintense in the MRI and hypoechoic in the US. A = Acromion; H = Humerus; SSP = Supraspinatus tendon.
When using US no supraspinatus full-thickness-tear was missed, but the number of full-thickness tears was slightly overestimated. For the diagnosis of intact supraspinatus tendons, 16 matches of US and MRI were observed. Furthermore, two tendons which were unsuspicious in US inspection were classified as partial-thickness tear in MRI.
Sensitivity of US for detection of any supraspinatus tendon damage was 0.93 and specificity was 1. For full-thickness tears only, sensitivity was 1 and specificity was 0.91, for partial-thickness tears sensitivity was 0.43 and specificity was 1.
With regard to the localization of the partial-thickness tears, MRI showed five patients (US: two patients) with an articular-sided tear, two patients (US: one patient) with a bursal-sided tear and 22 patients (US: 24 patients) with a full-thickness tear of the supraspinatus tendon (Table 4). The accuracy of US when using MRI as reference for the localization of partial-thickness tears was 91.1%, kappa = 0.85, p = 0.68.
Table 4.
Comparison of supraspinatus tear localization in US with MRI.
| Supraspinatus tendon | |||||
|---|---|---|---|---|---|
| US |
MRI |
Total | |||
| n (%) | Intact | Articular-sided tear | Bursal-sided tear | Full-thickness tear | |
| Intact | 16 (35.56) | 1 (2.22) | 1 (2.22) | 0 | 18 (40.00) |
| Articular-sided tear | 0 | 2 (4.44) | 0 | 0 | 2 (4.44) |
| Bursal-sided tear | 0 | 0 | 1 (2.22) | 0 | 1 (2.22) |
| Full-thickness tear | 0 | 2 (4.44) | 0 | 22 (48.89) | 24 (53.33) |
| Total | 16 (35.56) | 5 (11.11) | 2 (4.44) | 22 (48.89) | 45 (100.00) |
We compared both the US and the MRI diagnosis of any supraspinatus tendon damage to the intraoperative findings. There were 39 matches to be found with MRI (86.7%) and 41 (91.1%) with US, intraoperatively diagnosed full-thickness tears were neither missed in US nor MRI.
3.2. Infraspinatus tendon
MRI revealed six full-thickness (13.33%) and ten partial-thickness tears (22.22%) (Table 5). The US examination indicated nine full-thickness tears (20%) and nine partial-thickness tears (20%). The tendons were estimated similarly by the two imaging methods in 38/45 cases (accuracy 84.4%; kappa = 0.71, p = 0.39). While six full-thickness tears were judged correspondingly on both imaging modalities, one partial-thickness tear and two intact tendons diagnosed by MRI were identified as full-thickness tears in US. There was similar assessment of the status of the tendon in seven patients with partial-thickness tear of the infraspinatus tendon. Two healthy tendons in the MRI assessment appeared partially torn in US. The intact tendons had 25 analogies in US and MRI, but two tendons without signs of tear in US showed a partial-thickness tear in MRI.
Table 5.
Comparison of infraspinatus tear-type in US with MRI.
| Infraspinatus tendon | ||||
|---|---|---|---|---|
| US |
MRI |
Total | ||
| n (%) | No tear | Partial-thickness tear | Full-thickness tear | |
| No tear | 25 (55.56) | 2 (4.44) | 0 | 27 (60.00) |
| Partial-thickness tear | 2 (4.44) | 7 (15.56) | 0 | 9 (20.00) |
| Full-thickness tear | 2 (4.44) | 1 (2.22) | 6 (13.33) | 9 (20.00) |
| Total | 29 (64.44) | 10 (22.22) | 6 (13.33) | 45 (100.00) |
No full-thickness tear of the infraspinatus tendon was missed in US. One partial-thickness tear and two intact tendons were misclassified as full-thickness tears.
Sensitivity of US for detection of any infraspinatus tendon damage was 0.88 and specificity was 0.86. For full-thickness tears only a sensitivity of 1 and a specificity of 0.92, for partial-thickness tears only a sensitivity of 0.7 and a specificity of 0.94 was observed.
We compared both the US and the MRI diagnosis of any infraspinatus tendon damage to the intraoperative findings. There were 39 matches to be found with MRI (86.7%) and 41 (91.1%) with US, intraoperatively diagnosed full-thickness tears were neither missed in US nor MRI.
3.3. Subscapularis tendon
MRI detected four full-thickness (8.89%) and 14 partial-thickness tears (31.11%; Table 6). US performance was as follows: Four full-thickness tears (8.89%) and twelve partial-thickness tears (26.67%). Both imaging modalities showed the condition of the tendon consistently in 35/45 patients (accuracy 77.8%, kappa = 0.57, p = 0.88). Eight partial-thickness tears were similarly rated in MRI and US (Fig. 2). Also, two patients with intact tendons and two patients with full-thickness tear of the subscapularis in MRI were diagnosed having partial-thickness tear in US. For intact subscapularis tendons 25 matches in US and MRI were observed. In four patients with partial-thickness tear in MRI, US detected no evidence of rupture.
Table 6.
Comparison of subscapularis tear-type in US with MRI.
| Subscapularis tendon | ||||
|---|---|---|---|---|
| US |
MRI |
Total | ||
| n (%) | No tear | Partial-thickness tear | Full-thickness tear | |
| No tear | 25 (55.56) | 4 (8.89) | 0 | 29 (64.44) |
| Partial-thickness tear | 2 (4.44) | 8 (17.78) | 2 (4.44) | 12 (26.67) |
| Full-thickness tear | 0 | 2 (4.44) | 2 (4.44) | 4 (8.89) |
| Total | 27 (60.00) | 14 (31.11) | 4 (8.89) | 45 (100.00) |
Fig. 2.
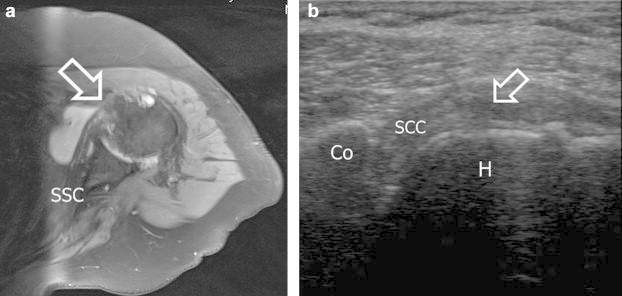
Partial-thickness subscapularis tear. Axial PD-TSE-weighted MRI plane (a) and transverse US image (b). The arrows show the focal defect with a thinned-out tendon. Co = Coracoid; H = Humerus, ISP = Infraspinatus tendon, S = Scapula; SSC = Subscapularis tendon.
We noticed that no MRI-rated full-thickness tear of the subscapularis tendon was classified as an intact tendon in US.
The evaluation of the pooled ruptures of the subscapularis tendons showed the following results for US: sensitivity = 0.78 and specificity = 0.93. For full-thickness tears only the sensitivity was 0.5 and specificity was 0.95. For partial-thickness tears only US had a sensitivity of 0.57 and a specificity of 0.87.
We compared both the US and the MRI diagnosis of any subscapularis tendon damage to the intraoperative findings. There were 36 matches to be found with MRI (80%) and 34 (75.6%) with US. One intraoperatively diagnosed full-thickness tear was missed in US, while one intraoperatively diagnosed intact subscapularis tendon was classified as torn in MRI.
3.4. Long biceps tendon
MRI examination revealed 14 ruptures (31.11%), one dislocation (2.22%), 25 tendovaginitis (55.56%) and five intact long biceps tendons (11.11%) (Table 7). In US we had 18 ruptures (40%), two dislocations (4.44%), 19 tendovaginitis (42.22%) and six normal findings (13.33%). When comparing the different findings in MRI and US we observed 39/45 (accuracy 86.7%) analogical corresponding results between the two diagnostic modalities (kappa = 0.75, p = 0.32). All of the 14 in MRI diagnosed ruptures could be found in US as well. In four patients who only had tendovaginitis in MRI there was a false classification as “rupture” in US. There was only one dislocation found in MRI which could equally be seen in US. One inconspicuous tendon in MRI was diagnosed as “dislocation” in US. The tendovaginitis was assessed analogically in 19 cases (Fig. 3). An intact long biceps tendon was consistently evaluated in four cases. Two patients with tendovaginitis in MRI had no signs of inflammatory changes of the long biceps tendon in US.
Table 7.
Comparison of long biceps tendon disorders in US with MRI.
| Long biceps tendon | |||||
|---|---|---|---|---|---|
| US |
MRI |
Total | |||
| n (%) | No pathology | Tendinitis | Dislocation | Rupture | |
| No pathology | 4 (8.89) | 2 (4.44) | 0 | 0 | 6 (13.33) |
| Tendinitis | 0 | 19 (42.22) | 0 | 0 | 19 (42.22) |
| Dislocation | 1 (2.22) | 0 | 1 (2.22) | 0 | 2 (4.44) |
| Rupture | 0 | 4 (8.89) | 0 | 1431.11 | 18 (40.00) |
| Total | 5 (11.11) | 25 (55.56) | 1 (2.22) | 14 (31.11) | 45 (100.00) |
Fig. 3.
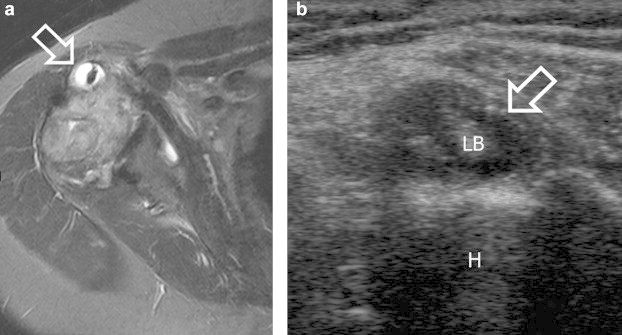
Tendovaginitis of the long biceps tendon. Axial T2-weighted MRI plane (a) and transverse US image (b). The hyperintense effusion in the tendon sheath is marked (arrow). Similarly the arrow in the US image points out the hypoechogenity that surrounds the long biceps tendon. H = Humerus, LB = Long biceps tendon.
A sensitivity of 0.95 and a specificity of 0.8 for any biceps pathology were calculated. The US had a sensitivity of 1 and a specificity of 0.87 for detection of a rupture, a sensitivity of 1 and a specificity of 0.97 for detection of a dislocation and a sensitivity of 0.58 and a specificity of 0.63 for diagnosis of a long biceps tendovaginitis.
4. Discussion
In the present study, we could demonstrate that with US the detection of rotator cuff and biceps tendon integrity and damage before shoulder joint replacement is comparable to MRI. There are no previous studies to evaluate US in comparison to MRI in patients with osteoarthritis before shoulder joint replacement with regard to rotator cuff and long biceps tendon pathologies.
In the literature review almost all studies that compare US to arthroscopic findings refer to the rotator cuff as a whole and do not distinguish between partial and complete tears of the individual tendons. Some studies suggest that US is less sensitive than MRI to detect complete and especially partial tears12,13 while other authors see no relevant difference.14,15 Zehetgruber et al retrospectively examined US and intraoperative findings in 332 patients without osteoarthritis of the shoulder.16 In contrast to our study sensitivities and specificities were only calculated for the supraspinatus tendon alone or in combination with the infraspinatus and subscapularis tendon but never individually for the latter two.
4.1. Supraspinatus tendon
In our study all MRI-diagnosed full-thickness tears of the supraspinatus tendon were also detected in US. Yet, not all of the seven partial tears were consistently described in US as two were classified as healthy tendons and another two as full-thickness tears. This inconsistency in the evaluation of partial-thickness tears has likewise been reported by other authors.5,12,13 Small partial-thickness tears can be missed whereas large focal defects over 50% of the tendon mimic full-thickness tears.8 In conclusion, the exact size of the partial tear should be measured to ascertain that partial-thickness tears are frequently missed due to the dimension of the injury.
Nevertheless, in our study US agreement to MRI for the supraspinatus tendon assessment was 91.1% so that US can equally be used to rule out complete supraspinatus tears, especially in patients that are not apt to receive MRI.
Both US and MRI detected all of the full-thickness supraspinatus tears that were seen intraoperatively, although not all of the partial-thickness tears that were found in US and MRI could be seen during the operation. One of the reasons could be the impaired visibility of partial-thickness ruptures in open surgery compared to arthroscopy.
4.2. Infraspinatus tendon
As in the evaluation of the supraspinatus tendons no full-thickness tears were missed in US, but one partial-thickness tear and two intact tendons were falsely classified as completely torn tendon. False positive US-classifications of infraspinatus tears could be caused by muscle atrophy which simulates a partial rupture of the tendons. Therefore, it might be beneficial to measure the tendon thickness in US and MRI and compare them to each other.
Seven out of ten partial-thickness tears were adequately classified. Again, sensitivity and specificity for detection of full-thickness tears was high whereas diagnosis of partial-thickness tears was less consistent. One of the reasons seems to be the wide variety of partial-thickness tears. Further reasons for an impaired sonographic visibility of the infraspinatus tendon are excessive osteophytes that can usually be seen in patients with osteoarthritis of the shoulder.
There are very few studies that focused on isolated tears of the infraspinatus tendon. Zehetgruber et al could not detect any isolated infraspinatus tears.16 Our study had similar results. In all cases of an infraspinatus tear, there could also be found a supraspinatus injury. Equal to the comparison of US and MRI detection of supraspinatus tears to the intraoperative findings, all full-thickness infraspinatus tears seen during surgery were also found preoperatively in US and MRI. Partial-thickness tears were less frequently observed during surgery than anticipated in US and MRI. Arthroscopic evaluation before joint replacement could have clarified this bias, but was not included in the Ethical committee's approval.
Young et al investigated secondary rotator cuff dysfunction following total shoulder arthroplasty in a multicenter study.17 They concluded that a fatty infiltration of the infraspinatus tendon preoperatively promoted secondary rotator cuff dysfunction. These results encourage us to compare additional signs of fatty infiltration in US and MRI in further studies, so that we will be able to diagnose influencing factors of postoperative complications in US and achieve the best outcome for patients with total shoulder replacement.
4.3. Subscapularis tendon
Comparison of US and MRI showed that no full-thickness tears were classified as intact, but two of the four complete tears were underestimated as partial-thickness tears and two intact tendons false-positively as partially torn. Four partial-thickness tears were not seen in US.
Sensitivities for US-detection of any tear (0.78) or full-thickness tears (0.5) were remarkably lower than US-assessment of supra- and infraspinatus tendon damages. Hence, the US evaluation of subscapularis tears prior to joint replacement seems more challenging.
Gerber and Farin analyzed traumatically induced isolated ruptures of subscapularis tendons and reported that intraoperative assessment completely matched preoperative diagnosis in US and MRI.18,19 Farin et al described similar results in patients with ongoing shoulder pain. They were able to detect 82% of the subscapularis tendon ruptures preoperatively in US. They further differentiated between partial- and full-thickness tears and assessed sensitivities of only 67% and 86% for the latter ones.19 In our study 75.6% of the ruptures diagnosed in US could be observed intraoperatively. These results once more demonstrate a low accuracy for detection of partial-thickness tears in US.
However, in the two studies of Gerber and Farin the US-assessment of the subscapularis tendon was more accurate than in our study. The main reason for this discrepancy is the different patient cohort. While Gerber and Farin examined patients with isolated subscapularis ruptures, in our study only patients with osteoarthritis of the shoulder were included. For the US-evaluation of the subscapularis tendon, it is essential to externally rotate to a maximum and visualize the tendon under traction.19 Patients with osteoarthritis usually suffer from an impaired or even lost ability to externally rotate. Even more, a medialization of the humeral head is often present so that the interval of the subscapularis between the coracoid process and the lesser tuberosity is diminished. Therefore, it can be more demanding or even impossible to visualize the subscapularis tendon by dynamic US in patients with osteoarthritis of the shoulder.
A recent study emphasized the importance of an intact subscapularis tendon after joint replacement. A deficient subscapularis promotes an upward migration of the humeral head by an increase of the middle portion of the deltoid and the supraspinatus tendon. The integrity of the subscapularis tendon is therefore crucial for the long term stability of a total shoulder arthroplasty.20
4.4. Long biceps tendon
None of the 14/45 ruptures of the long biceps tendon have been overlooked in US. Six tendovaginitis were not identified because four of them appeared as ruptured and two intact. The only dislocation found in MRI could also be seen in US.
Likewise to our study results, Armstrong et al could detect all ruptures in US.21 Armstrong additionally tried to differ between partial- and full-thickness tears in which US was not able to do so. Farin et al earlier emphasized on the difficult differentiation between partial- and full-thickness tears.22 We did not split up these two entities because of its lacking consequence for joint replacement.
With regard to sonographic detection of dislocated long biceps tendons Armstrong described a high sensitivity and specificity. Ptasznik and Hennessy described that dislocations are typically associated with full-thickness supraspinatus tears.23 This association could be confirmed in our study (in MRI and US). More interesting is the coincidence of dislocations with subscapularis tendon injuries, as the long biceps tendon usually dislocates medially and therefore gradually bruises the subscapularis tendon. In our study one biceps tendon dislocation was diagnosed by MRI. This patient showed a subscapularis partial-thickness tear.
Consequently, US of the long biceps tendon proved to be reliable compared to MRI. Misinterpretations are caused by thinned out tendons which can be poorly visualized and which are commonly seen in osteoarthritis of the shoulder.
5. Limitation
Only patients with osteoarthritis of the shoulder were included so that the number of patients is limited. Further studies with higher patient numbers are desirable to reassure our statements.
6. Conclusion
Examination of the rotator cuff with US is highly competitive to MRI as it is inexpensive, quick, easily available, dynamic, without radiation exposure, and can be performed at bedside and thus is ideal for the patients' comfort.24,25 On the other hand, US depends considerably on the examiner's experience26–28 and a constituted standard of examination.29,30 For patients with limited ROM especially external rotation, US is less consistent with MRI in the diagnosis of subscapularis tears. In our opinion, US is especially advantageous for the preoperative assessment of the rotator cuff and the long biceps tendon in revision cases where MRI quality is often reduced due to metallic implants. In particular patients with claustrophobia, pacemakers or other MRI exclusion criteria benefit from US diagnosis of the rotator cuff.
Conflicts of interest
All authors have none to declare.
Ethical approval
Approved by:
Ethical Committee, Alte Glockengießerei 11/1, University of Heidelberg, Germany, Study number: S-305/2007.
References
- 1.Omoumi P., Bafort A.C., Dubuc J.E., Malghem J., Vande Berg B.C., Lecouvet F.E. Evaluation of rotator cuff tendon tears: comparison of multidetector CT arthrography and 1.5-T MR arthrography. Radiology. 2012;264:812–822. doi: 10.1148/radiol.12112062. [DOI] [PubMed] [Google Scholar]
- 2.de Jesus J.O., Parker L., Frangos A.J., Nazarian L.N. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192:1701–1707. doi: 10.2214/AJR.08.1241. [DOI] [PubMed] [Google Scholar]
- 3.Levine B.D., Motamedi K., Seeger L.L. Imaging of the shoulder: a comparison of MRI and ultrasound. Curr Sports Med Rep. 2012;11:239–243. doi: 10.1249/JSR.0b013e31826b6baa. [DOI] [PubMed] [Google Scholar]
- 4.Zanetti M., Hodler J. Imaging of degenerative and posttraumatic disease in the shoulder joint with ultrasound. Eur J Radiol. 2000;35:119–125. doi: 10.1016/s0720-048x(00)00227-8. [DOI] [PubMed] [Google Scholar]
- 5.Lenza M., Buchbinder R., Takwoingi Y., Johnston R.V., Hanchard N.C., Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;9:CD009020. doi: 10.1002/14651858.CD009020.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iannotti J.P., Zlatkin M.B., Esterhai J.L., Kressel H.Y., Dalinka M.K., Spindler K.P. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg Am. 1991;73:17–29. [PubMed] [Google Scholar]
- 7.Smith T.O., Back T., Toms A.P., Hing C.B. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol. 2011;66:1036–1048. doi: 10.1016/j.crad.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Teefey S.A., Hasan S.A., Middleton W.D., Patel M., Wright R.W., Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498–504. [PubMed] [Google Scholar]
- 9.van Holsbeeck M.T., Kolowich P.A., Eyler W.R. US depiction of partial-thickness tear of the rotator cuff. Radiology. 1995;197:443–446. doi: 10.1148/radiology.197.2.7480690. [DOI] [PubMed] [Google Scholar]
- 10.Magee T., Williams D. 3.0-T MRI of the supraspinatus tendon. AJR Am J Roentgenol. 2006;187:881–886. doi: 10.2214/AJR.05.1047. [DOI] [PubMed] [Google Scholar]
- 11.Naredo A.E., Aguado P., Padron M. A comparative study of ultrasonography with magnetic resonance imaging in patients with painful shoulder. J Clin Rheumatol. 1999;5:184–192. doi: 10.1097/00124743-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Nelson M.C., Leather G.P., Nirschl R.P., Pettrone F.A., Freedman M.T. Evaluation of the painful shoulder. A prospective comparison of magnetic resonance imaging, computerized tomographic arthrography, ultrasonography, and operative findings. J Bone Joint Surg Am. 1991;73:707–716. [PubMed] [Google Scholar]
- 13.Martin-Hervas C., Romero J., Navas-Acien A., Reboiras J.J., Munuera L. Ultrasonographic and magnetic resonance images of rotator cuff lesions compared with arthroscopy or open surgery findings. J Shoulder Elbow Surg. 2001;10:410–415. doi: 10.1067/mse.2001.116515. [DOI] [PubMed] [Google Scholar]
- 14.Teefey S.A., Rubin D.A., Middleton W.D., Hildebolt C.F., Leibold R.A., Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86-A:708–716. [PubMed] [Google Scholar]
- 15.Vlychou M., Dailiana Z., Fotiadou A., Papanagiotou M., Fezoulidis I.V., Malizos K. Symptomatic partial rotator cuff tears: diagnostic performance of ultrasound and magnetic resonance imaging with surgical correlation. Acta Radiol. 2009;50:101–105. doi: 10.1080/02841850802600764. [DOI] [PubMed] [Google Scholar]
- 16.Zehetgruber H., Lang T., Wurnig C. Distinction between supraspinatus, infraspinatus and subscapularis tendon tears with ultrasound in 332 surgically confirmed cases. Ultrasound Med Biol. 2002;28:711–717. doi: 10.1016/s0301-5629(02)00508-2. [DOI] [PubMed] [Google Scholar]
- 17.Young A.A., Walch G., Pape G., Gohlke F., Favard L. Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am. 2012;94:685–693. doi: 10.2106/JBJS.J.00727. [DOI] [PubMed] [Google Scholar]
- 18.Gerber C., Krushell R.J. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73:389–394. doi: 10.1302/0301-620X.73B3.1670434. [DOI] [PubMed] [Google Scholar]
- 19.Farin P., Jaroma H. Sonographic detection of tears of the anterior portion of the rotator cuff (subscapularis tendon tears) J Ultrasound Med. 1996;15:221–225. doi: 10.7863/jum.1996.15.3.221. [DOI] [PubMed] [Google Scholar]
- 20.Terrier A., Larrea X., Malfroy Camine V., Pioletti D.P., Farron A. Importance of the subscapularis muscle after total shoulder arthroplasty. Clin Biomech (Bristol, Avon) 2013;28:146–150. doi: 10.1016/j.clinbiomech.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Armstrong A., Teefey S.A., Wu T. The efficacy of ultrasound in the diagnosis of long head of the biceps tendon pathology. J Shoulder Elbow Surg. 2006;15:7–11. doi: 10.1016/j.jse.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 22.Farin P.U. Sonography of the biceps tendon of the shoulder: normal and pathologic findings. J Clin Ultrasound. 1996;24:309–316. doi: 10.1002/(SICI)1097-0096(199607/08)24:6<309::AID-JCU5>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 23.Ptasznik R., Hennessy O. Abnormalities of the biceps tendon of the shoulder: sonographic findings. AJR Am J Roentgenol. 1995;164:409–414. doi: 10.2214/ajr.164.2.7839979. [DOI] [PubMed] [Google Scholar]
- 24.Middleton W.D., Payne W.T., Teefey S.A., Hildebolt C.F., Rubin D.A., Yamaguchi K. Sonography and MRI of the shoulder: comparison of patient satisfaction. AJR Am J Roentgenol. 2004;183:1449–1452. doi: 10.2214/ajr.183.5.1831449. [DOI] [PubMed] [Google Scholar]
- 25.Mack L.A., Gannon M.K., Kilcoyne R.F., Matsen R.A. Sonographic evaluation of the rotator cuff. Accuracy in patients without prior surgery. Clin Orthop Relat Res. 1988:21–27. [PubMed] [Google Scholar]
- 26.Sonnabend D.H., Hughes J.S., Giuffre B.M., Farrell R. The clinical role of shoulder ultrasound. Aust N Z J Surg. 1997;67:630–633. doi: 10.1111/j.1445-2197.1997.tb04612.x. [DOI] [PubMed] [Google Scholar]
- 27.O'Connor P.J., Grainger A.J., Morgan S.R., Smith K.L., Waterton J.C., Nash A.F. Ultrasound assessment of tendons in asymptomatic volunteers: a study of reproducibility. Eur Radiol. 2004;14:1968–1973. doi: 10.1007/s00330-004-2448-4. [DOI] [PubMed] [Google Scholar]
- 28.O'Connor P.J., Rankine J., Gibbon W.W., Richardson A., Winter F., Miller J.H. Interobserver variation in sonography of the painful shoulder. J Clin Ultrasound. 2005;33:53–56. doi: 10.1002/jcu.20088. [DOI] [PubMed] [Google Scholar]
- 29.Rutten M.J., Jager G.J., Blickman J.G. From the RSNA refresher courses: US of the rotator cuff: pitfalls, limitations, and artifacts. Radiographics. 2006;26:589–604. doi: 10.1148/rg.262045719. [DOI] [PubMed] [Google Scholar]
- 30.Jacobson J.A. Shoulder US: anatomy, technique, and scanning pitfalls. Radiology. 2011;260:6–16. doi: 10.1148/radiol.11101082. [DOI] [PubMed] [Google Scholar]


