Abstract
Purpose
The etiology of an ischemic stroke remains undetermined in 20–35% of cases and many patients do not have any of the conventional risk factors. Increased visceral adipose tissue (VAT) is a suggested new risk factor for both carotid artery atherosclerosis (CAA) and atrial fibrillation (AF), but its role in the remaining stroke population is unknown. We assessed the amount of VAT in patients with embolic stroke of undetermined source (ESUS) after excluding major-risk cardioembolic sources, occlusive atherosclerosis, and lacunar stroke.
Methods
Altogether 58 patients (mean age 57.7±10.2 years, 44 men) with ischemic stroke of unknown etiology but without CAA, known AF or small vessel disease underwent computed tomography angiography and assessment of VAT. For comparison VAT values from three different reference populations were used. Conventional risk factors (smoking, hypertension, diabetes, increased total and LDL-cholesterol, decreased HDL-cholesterol) were also registered.
Results
Mean VAT area was significantly higher in stroke patients (205±103 cm2 for men and 168±99 cm2 for women) compared to all reference populations (P<0.01). 50% of male and 57% of female patients had an increased VAT area. In male patients, VAT was significantly higher despite similar body mass index (BMI). Increased VAT was more common than any of the conventional risk factors.
Conclusion
Increased VAT was found in over half of our patients with ESUS suggesting it may have a role in the pathogenesis of thromboembolism in this selected group of patients.
Introduction
Stroke is the leading cause of long-term disability, the second leading cause of death and a major consumer of healthcare resources worldwide [1–4]. Ischemic stroke accounts for 80% of all strokes in the Western countries and is mostly caused by atheroma of the cervical arteries, embolization from intracardiac sources, or by microvascular disease [5]. In 20–35% of the cases the etiology of stroke remains undetermined (cryptogenic) despite profound investigations [6, 7]. Patients with embolic stroke of undetermined source (ESUS) are a subset of patients with cryptogenic stroke who have embolic strokes and sufficient diagnostic assessment to exclude major-risk cardioembolic sources, occlusive atherosclerosis, and lacunar stroke [8].
Obesity is a well-known risk factor for all cardiovascular diseases and stroke, and it increases the risk of all-cause mortality [9]. A traditional way to define obesity is to measure body mass index (BMI) [10, 11]. Recently, more attention has been paid to the distribution of the adipose tissue in the body. The increased visceral fat type in particular has been stated to increase the risk of stroke and other cardiovascular diseases [12–16]. Adults with visceral adiposity tend to manifest insulin resistance, hypertension and dyslipidemia more often when compared to those who are equally obese with lower levels of visceral fat [17, 18]. The aforementioned metabolic changes have been postulated to cause a hypercoagulable state both in the arterial and venous system and, consequently, play a role in the pathogenesis of stroke [19]. Visceral fat can be measured accurately with computed tomography (CT) [20, 21]. To the best of our knowledge, no previous study has investigated the prevalence of VAT in a population with ESUS, i.e. in which atherosclerosis, small vessel disease or known AF are excluded as stroke etiologies.
Materials and Methods
The study was approved by the Kuopio University Hospital Research Ethics Board and all clinical investigations have been conducted according to the principles expressed in the Declaration of Helsinki. Prior to participation in the study, written informed consent was obtained from the patient or the patient's legally authorized representative.
Study patients and reference populations
Study patients
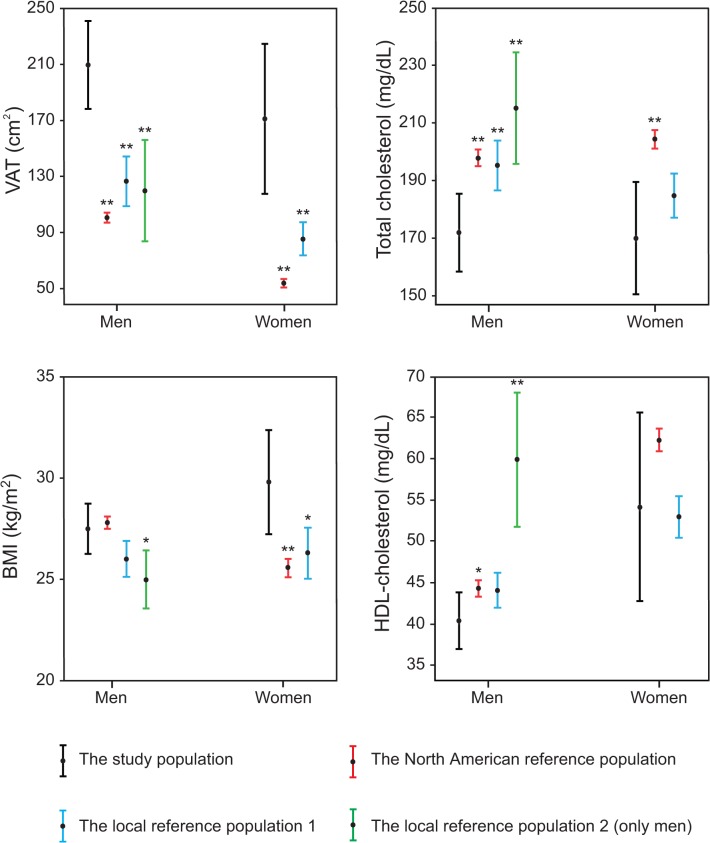
A flow chart describing the formation of the study population is presented in Fig. 1. Patients with ischemic stroke or transient ischemic attack (TIA) admitted to Kuopio University Hospital between March 2005 and October 2008 were evaluated as candidates for the study (EMBODETECT) [22, 23]. A total of 162 patients with stroke/TIA of undetermined or suspected cardioembolic etiology other than atrial fibrillation were recruited by the neurologists involved in the study as a part of their daily clinical work. The suspicion of cardiogenic etiology was based on the characteristic clinical symptoms and/or primary clinical signs, i.e., simultaneous or sequential strokes/TIAs in different arterial territories, hemorrhagic transformation, simultaneous emboli in other organs, decreased consciousness at stroke/TIA onset, isolated aphasia, or isolated visual-field defect. Patients with chronic or other previously known atrial fibrillation (AF) were excluded. Of 162 originally recruited patients the VAT measurements were performed on 118 patients. Furthermore, 60 patients were excluded due to a defined etiology for stroke (n = 54) or technically unsuccessful assessment of stroke etiology (n = 6). We modified the TOAST classification for cardioembolism, applying the more recent European Association of Echocardiography (EAE) recommendations for defining cardiac sources of embolism [24, 25]. Accordingly, 26 patients were found to have cardiogenic stroke. Large artery atherosclerosis was found in nine patients, small vessel occlusion in eight patients and other determined etiology in 11 patients. After profound etiologic investigations of stroke etiology, 58 patients fulfilled the criteria for ESUS and formed the final study population.
Fig 1. Flow chart of patient recruitment.
Neurologists recruited consecutive patients with acute ischemic stroke/TIA with undetermined etiology or a suspicion of cardiogenic etiology. Stroke/TIA patients with atrial fibrillation were excluded. Patients who had undergone the assessment of visceral adipose tissue were included in the current study. Six patients were excluded from the study due to technically unsuccessful assessment of stroke etiology. The remaining patients were further categorized according to the modified TOAST classification, denoting five subtypes of ischemic stroke: 1) large-artery atherosclerosis, 2) cardioembolism, 3) small-vessel occlusion, 4) stroke of other determined etiology, and 5) embolic stroke of undetermined source (ESUS). The classification was updated by applying the more recent EAE recommendations for defining cardiac sources of embolism.
Reference population
We used three different reference populations. The first one was a large North American population published previously (n = 1160) [26], where the area of VAT was measured from a single CT slice at the level of the umbilicus. The ethnicity of the subjects in this reference population was 88% non-Hispanic white, 10% Hispanic and the remainder either Asian or African-American. The second reference population was a previously published local population from Kuopio University Hospital area consisting of healthy non-Hispanic white offspring of type 2 diabetic patients (n = 129) [27, 28]. In this study the area of VAT was measured from a single CT slice at the level of the fourth lumbar vertebra (L4). Both previously published reference studies used an attenuation range from −30 to −190 Hounsfield Units (HU) to measure adipose tissue. The third reference population is an unpublished local group of 18 healthy male subjects from the Kuopio University Hospital area. The VAT area was measured at the level of the L4 vertebra using an attenuation range of −30 to −190 HU. Increased VAT was defined as VAT above the mean+2SD in the North American reference population (>122.8 cm2 for females and >188.4 cm2 for men).
Detailed statistical comparison of the reference populations is presented in S1 Table. Noteworthy, men in the North American reference population and the local reference population 2 were coeval and had similar VAT area, whereas the local population 1 consisted of younger individuals with higher VAT when compared to the North American ones. Women in the North American reference population were older and had smaller VAT areas than in the local reference population 1 but there was no difference in BMI.
Measurement of VAT
VAT was measured with CT (Sensation 16; Siemens Medical Solutions, Forchheim, Germany). Scanning was performed at 120 kV, 190 mAs with a slice thickness of 10 mm. The radiation dose was calculated by the dose length product and it was 0.2 mSv, which equals around 8% of annual background radiation [29]. The image quality for the assessment of VAT was sufficient in all patients. The subjects were examined in the supine position with their arms stretched above their heads. The fourth lumbar vertebra was identified on the scout image and one axial slice from that level was obtained [30]. The VAT area was calculated by drawing a line within the muscle wall delineating the abdominal cavity and then computing the adipose tissue surfaces with an attenuation range from −30 to −190 HU [31]. All VAT area measurements were done by the same investigator (A.M.) guided by an experienced radiologist (J.M.). The measurement is illustrated in Fig. 2.
Fig 2. The image illustrates how the area of visceral adipose tissue (VAT) within the abdominal cavity (white line) was determined by CT scanning.

Pixels with the density of adipose tissue between −30 and −190 Hounsfield Units (HU) were included in the VAT area calculated automatically by the CT software. In the illustrative case, the VAT area is 110 cm2.
Assessment of conventional risk factors
Subjects were dichotomized as never-smokers or as current/former smokers according to their self-reported smoking status. Subjects were dichotomized to have hypertension or diabetes if they were diagnosed either previously or during their hospital stay. BMI was determined by measuring the height and weight from lightly clothed patients without shoes. Based on BMI patients were categorized as normal weight (BMI <25 kg/m2), overweight (25 kg/m2 ≤ BMI <30 kg/m2) and obese (BMI ≥30 kg/m2). The fasting total cholesterol, high density lipoprotein (HDL)-cholesterol, low density lipoprotein (LDL)-cholesterol and triglyceride measurements were obtained the next morning after hospital admission. Body surface area (BSA) was calculated using the Mosteller’s formula [32].
Statistical analysis
The associations between sex, smoking, hypertension, diabetes and VAT were studied using Independent Samples T-test. The effect size between aforementioned variables was studied using Cohen’s d (d) [33]. Pearson’s correlation coefficient was used to study correlations between VAT and age, total cholesterol, LDL-cholesterol, HDL-cholesterol, triglycerides, and BMI. Correlates that associated with VAT were included in the multiple regression analysis. Of the continuous variables, HDL-cholesterol, triglycerides and BMI were not normally distributed so they were log transformed for statistical analyses. Continuous variables are expressed as mean ± one standard deviation. In comparative analyses, age adjusted values were used. Categorical variables are presented as absolute values and percentages of the study population. p≤0.05 was considered statistically significant. SPSS 19.0 (1989−2010, SPSS Inc, Chicago, USA) and R version 2.14.0 (2011, The R Foundation for Statistical Computing) software were used for the statistical analyses.
Results
The clinical characteristics of the stroke patients and the reference populations are summarized in Table 1. Over 75% of the patients with ESUS were men. Fifty-two percent and 21% of men, and 50% and 36% of women were overweight and obese, respectively. Eleven patients (19%) were on cholesterol-lowering medication. Women had higher mean HDL-cholesterol than men, 54 mg/dL (1.40 mmol/L) vs. 40 mg/dL, (1.04 mmol/L), d = 0.79, p = 0.037).
Table 1. Clinical characteristics of the study population and the reference populations.
| The study population | The North American reference population 26 | The local reference population 1 27, 28 | The local reference population 2 | |||||
|---|---|---|---|---|---|---|---|---|
| Subjects, n | 58 | 1160 | 129 | 18 | ||||
| Sex | 75.9% men | 55.2% men | 45.7% men | 100% men | ||||
| Ethnicity | 100% non-Hispanic white | 88% non-Hispanic white | 100% non-Hispanic white | 100% non-Hispanic white | ||||
| Men (n = 44) | Women (n = 14) | Men (n = 640) | Women (n = 520) | Men (n = 59) | Women (n = 70) | Men (n = 18) | Women (n = 0) | |
| Age, years | 57.0±10.4 | 60.1±9.4 | 56.0±11.4 | 57.0±11.2 | 34.9±6.2 ** | 36.4±6.4 ** | 53.4±3.2 * | NA |
| VAT area, cm2 | 205.3±103.0 | 168.0±99.1 | 99.6±44.4 ** | 54.2±34.3 ** | 125.1±67.8 ** | 85.0±11.9 ** | 118.3±75.9 ** | NA |
| BMI, kg/m2 | 27.5±4.2 | 29.8±4.9 | 27.8±3.9 | 25.6±4.8 ** | 26.0±3.5 | 26.3±5.4 * | 25.0±3.1 * | NA |
| Total cholesterol, mg/dl | 172.0±45.6 | 170.1±37.1 | 197.9±37.3 ** | 204.3±37.1 ** | 195.3±34.4 ** | 184.8±33.3 | 215.1±41.8 ** | NA |
| HDL-cholesterol, mg/dl | 40.4±11.6 | 54.2±21.8 | 44.3±12.8 * | 62.3±16.0 | 44.1±8.5 | 53.0±10.8 | 59.9±17.6 ** | NA |
| LDL-cholesterol, mg/dl | 114.5±42.2 | 103.9±33.9 | NA | NA | NA | NA | 136.5±35.5 * | NA |
| Triglycerides, mg/dl | 122.5±88.0 | 105.8±54.8 | NA | NA | 119.6±62.0 | 86.8±43.4 | 92.2±45.8 | NA |
| Diabetes mellitus, n (%) | 4 (9.1) | 2 (14.3) | 19 (3.0) | 8 (1.5) | 0 (0.0) | 0 (0.0) | NA | NA |
| Hypertension, n (%) | 24 (54.5) | 8 (57.1) | 225 (35.6) | 146 (27.6) | NA | NA | NA | NA |
| Current or former smoker, n (%) | 16 (26.3) | 3 (21.4) | 290 (45.3) | 218 (41.9) | NA | NA | NA | NA |
VAT, visceral adipose tissue; BMI, body mass index; HDL, high density lipoprotein; LDL, low density lipoprotein
* statistically significant difference at level p<0.05 compared to the same gender group in study population
** statistically significant difference at level p<0.01 compared to the same gender group in study population
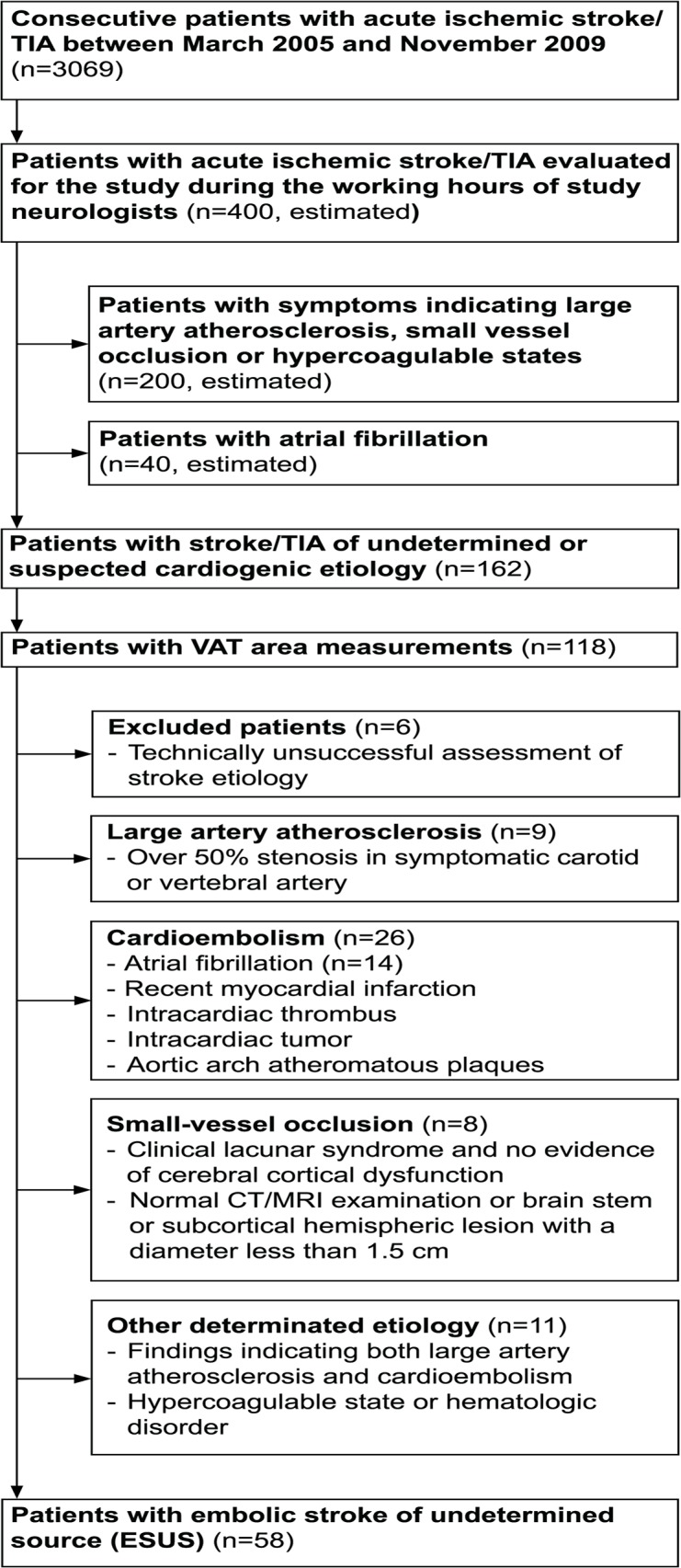
Fig. 3 shows the differences in VAT, BMI, total cholesterol and HDL-cholesterol between patients with ESUS and the reference populations. In both male and female patients with ESUS the VAT area was almost or over twofold when compared to all the reference populations. In women, BMI was higher in the study population compared to both reference populations whereas in men there was a significant difference only when compared to the second local reference population. Unexpectedly, the mean total cholesterol of both men and women was lower in our study patients when compared to all three reference populations. Male stroke patients had significantly lower HDL-cholesterol compared to all reference populations whereas in the female group there was a significant difference only in comparison to the North American reference population.
Fig 3. Age adjusted mean values and their 95% confidence intervals of visceral adipose tissue (VAT) and the conventional risk factors in patients with ESUS compared to the three control populations.
Statistically significant differences between patients with ESUS and reference populations are marked by * (p<0.05) and ** (p<0.01).
Half of the male patients and 57% of female patients had VAT area increased over the set upper limit of normality. Almost 80% of normal weight patients (BMI <25 kg/m2) and only 7% of obese (BMI ≥30 kg/m2) patients had normal VAT area. Though, 48% of male patients and 71% of female patients with overweight BMI (25 kg/m2 ≤ BMI <30 kg/m2) had normal VAT area. Patient examples of normal and increased VAT are presented in Fig. 4.
Fig 4. Patient examples with the same body mass index (BMI) and normal or increased (>188.4 cm2 for men) areas of visceral adipose tissue (VAT).
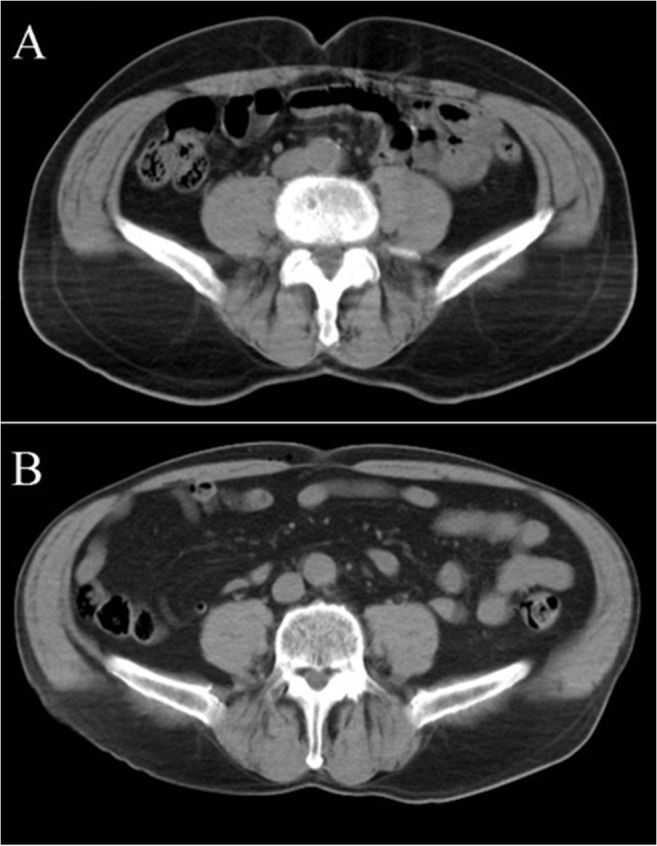
(A) Male, age 69 years, BMI 25 kg/m2, VAT area 80 cm2. (B) Male, age 71 years, BMI 25 kg/m2, VAT area 230 cm2.
There were moderate positive correlations between VAT and BMI (r = 0.562, p<0.001) and VAT and BSA (r = 0.453, p<0.001). The number of patients with diabetes was small (n = 6) but this group of patients had larger VAT areas when compared to non-diabetics (319 cm2 vs. 182 cm2, d = 1.85, p = 0.001). In study patients, the VAT area was not associated with age or any of the cholesterols or triglycerides.
Discussion
Our main finding was that over half of the patients with embolic stroke of undetermined source had increased VAT, and the mean VAT in the whole group was two-fold larger when compared to three different reference populations, one Northern American and two local ones. Moreover, increased VAT was more commonly found than any single conventional risk factor for stroke. Interestingly, in male patients, VAT was significantly higher compared to all of the reference populations although BMI didn’t show similar trend. Patients were determined to have acute ESUS after exclusion of CAA, AF or other high risk sources for cardiogenic embolism. To the best of our knowledge, the area of VAT has not been previously studied in this patient group.
Our results indicate that the increased amount of visceral type fat might be a risk factor for ESUS. The pathophysiology of ESUS is largely unknown and the role of conventional risk factors is less clear than in stroke of a defined etiology [34]. Similarly, many of our patients were lacking all conventional risk factors and only moderate positive correlations were found between VAT and diabetes, BMI, decreased HDL cholesterol, and BSA. There was no difference in the BMI between men in our study populations and two reference populations even if a highly significant difference in VAT was found. Moreover, more than a half of the overweight patients had a normal VAT area. Therefore, VAT measurements cannot be replaced by BMI. BMI is not sensitive to the differentiation of body fat/muscle ratio [35] or the variable distribution of visceral and subcutaneous fat.
The importance of body fat distribution has been recognized for more than 60 years [36]. Individuals with upper abdominal, central or android obesity are at a greater risk of cardiovascular diseases than those with gluteofemoral or peripheral obesity. It has been shown that the response to insulin and other hormones differs between visceral and subcutaneous adipose tissue, and that VAT is metabolically more active than subcutaneous adipose tissue. It secretes several pro- and anti-inflammatory factors that are associated with endothelial damage [37], modulates the inflammatory state and procoagulant response via increased secretion of procoagulant mediators such as plasminogen activator inhibitor-1 (PAI-1), an endogenous inhibitor of fibrinolysis [38–41], tissue factor (TF) [40–42], and via enhanced platelet activity [43]. The potential role of enhanced procoagulative tendency is further strengthened by the fact that increased epicardial fat, which has been shown to have a strong correlation with the amount of visceral adipose tissue, has been reported to be strongly associated with idiopathic venous thrombosis (VTE), even after adjustment for the established risk factors for atherosclerosis [44]. VTE and intracardiac thrombosis are known to share similar constituents (predominantly fibrin and erythrocytes with fewer platelets) and pathogenic factors (stasis, altered vessel wall and increased activity of coagulation).
VAT also predisposes patients to atherosclerosis [45, 46] and it has been shown to be independently associated with paroxysmal and persistent atrial fibrillation [47]. In our study, patients with CAA, previously known AF or AF diagnosed by telemetry or 24-h Holter recording during or immediately after hospital stay were excluded, but the presence of silent atrial fibrillation cannot be totally ruled out. In conclusion, the increased visceral adipose tissue could expose a subject to the risk of ESUS both by 1) promoting an inflammatory and prothrombotic state and 2) predisposing to latent atrial fibrillation.
We used a single CT slice for VAT area assessments because it has been shown to be an accurate quantitative estimate of VAT [48]. CT is the most reproducible method for the assessment of the adipose tissue area along with MRI [48, 49]. The reproducibility of CT-assessed VAT has been shown to be excellent with an error of reproducibility of less than 1% [49–51]. Ultrasound imaging is a radiation-free method but it yields inconsistent results [52]. MRI also enables radiation-free assessment of the VAT area, however, with poorer availability and higher costs. The clinical value of VAT in the risk stratification of stroke remains to be evaluated in future. Determination of the VAT might improve risk stratification and the allocation of secondary prevention resources, the benefit of which could exceed the harm caused by the small amount of radiation (0.2 mSv) caused by VAT CT imaging.
There are limitations of the present study. The most important limitation is the reference population. Only two small local reference populations (n = 129 and n = 18) with similar VAT quantification methods were available due to radiation-related restrictions. These two control populations consisted of healthy individuals from the Kuopio University Hospital area. The latter consisted only of males, who were considerably younger than our patients. Additionally, a large population from North America (n = 1160) was used as a reference. In this North American population the distribution of age and sex was similar, but the ethnicity was somewhat different (88% non-Hispanic white, 10% Hispanic and the remaining two percent either Asian or African-American vs. 100% non-Hispanic white in our homogenous patient group). However, in previous studies no difference in the VAT area at the level of L4/L5 vertebra has been found between Hispanic and non-Hispanic white populations [53] and the vast majority of non-Hispanic whites in Northern America trace their origins to the Northwestern Europe [54]. Most importantly, the main results were similar regardless of which of these three populations was used. Secondly, in the North American reference population, the area of VAT was measured from a single CT slice at the level of the umbilicus, whereas in our study and in the local reference studies a skeletal landmark was used. Practically, these two landmarks are at the same position as shown in a previous study [55]. However, regarding to the North American reference population we had access only to the published data so a profound methodological comparison of VAT measurement could not be performed. Thirdly, 19% of our patients were on cholesterol-lowering medication, which could interfere the interpretation of the role of blood lipids as risk factor. However, the share of patients using cholesterol-lowering medication in the North American reference population was similar [56]. Information about the use of cholesterol-lowering medication in the local reference populations was not available. The fourth limitation concerns the relatively small number of patients with ESUS and especially the number of female patients. This is due to the strict criteria of including only patients with ESUS after excluding CAA or a cardiogenic source for stroke.
In conclusion, patients with ESUS have highly increased VAT compared to unmatched reference population. Increased VAT may serve as a pathogenic organ for promoting the formation of thrombus and may thus contribute to the etiology of the current stroke and increase the risk of future strokes in this selected stroke population. Recognizing individuals with an increased amount of VAT could theoretically help in preventing stroke recurrence if appropriate treatment is launched. Further clinical studies are needed to clarify whether a reduction in VAT could also decrease the risk of recurrent stroke.
Supporting Information
(PDF)
Acknowledgments
We thank Dr Nick Hayward for proofreading and MSc Marja-Leena Hannila for help with statistical analyses.
Data Availability
Based on legal restrictions, data cannot be made available in the paper, the supplemental files, or a public repository. Readers may contact Antti Muuronen to request the data. Data are also available from the Kuopio University Hospital Ethics Committee for researchers who meet the criteria for access to confidential data.
Funding Statement
This study was supported by the Kuopio University Hospital (grant number 5063519—URL: http://www.psshp.fi/). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006;367: 1747–1757. [DOI] [PubMed] [Google Scholar]
- 2. Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Stroke 2006;37: 577–617. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. World health statistics 2012 Geneva, Switzerland: World health organization; 2012. [Google Scholar]
- 4. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012;125: e2–220. 10.1161/CIR.0b013e31823ac046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ay H, Furie KL, Singhal A, Smith WS, Sorensen AG, Koroshetz WJ. An evidence-based causative classification system for acute ischemic stroke. Ann Neurol 2005;58: 688–697. [DOI] [PubMed] [Google Scholar]
- 6. Guercini F, Acciarresi M, Agnelli G, Paciaroni M. Cryptogenic stroke: time to determine aetiology. J Thromb Haemost. 2008;6: 549–54. 10.1111/j.1538-7836.2008.02903.x [DOI] [PubMed] [Google Scholar]
- 7. Arboix A, Alió J. Cardioembolic stroke: clinical features, specific cardiac disorders and prognosis. Curr Cardiol Rev. 2010;6: 150–61 10.2174/157340310791658730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hart RG, Diener HC, Coutts SB, Easton JG, Granger CB, O'Donnell MJ, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13: 429–38. 10.1016/S1474-4422(13)70310-7 [DOI] [PubMed] [Google Scholar]
- 9. Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet 2009;373: 1083–1096. 10.1016/S0140-6736(09)60318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chronic Dis 1972;25: 329–343. [DOI] [PubMed] [Google Scholar]
- 11. Quetelet LA. A treatise on man and the development of his faculties. 1842. Obes Res 1994;2: 72–85. [DOI] [PubMed] [Google Scholar]
- 12. Jensky NE, Criqui MH, Wright CM, Wassel CL, Alcaraz JE, Allison MA. The association between abdominal body composition and vascular calcification. Obesity 2011;19: 2418–2424. 10.1038/oby.2011.70 [DOI] [PubMed] [Google Scholar]
- 13. Bodenant M, Kuulasmaa K, Wagner A, Kee F, Palmieri L, Ferrario MM, et al. MORGAM Project. Measures of abdominal adiposity and the risk of stroke: The MOnica risk, genetics, archiving and monograph (MORGAM) study. Stroke 2011;42: 2872–2877. 10.1161/STROKEAHA.111.614099 [DOI] [PubMed] [Google Scholar]
- 14. Nicklas BJ, Penninx BW, Ryan AS, Berman DM, Lynch NA, Dennis KE. Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Diabetes Care 2003;26: 1413–1420. [DOI] [PubMed] [Google Scholar]
- 15. Wiklund P, Toss F, Weinehall L, Hallmans G, Franks PW, Nordström A, et al. Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J Clin Endocrinol Metab. 2008;93: 4360–4366. 10.1210/jc.2008-0804 [DOI] [PubMed] [Google Scholar]
- 16. Toss F, Wiklund P, Franks PW, Eriksson M, Gustafson Y, Hallmans G, et al. Abdominal and gynoid adiposity and the risk of stroke. Int J Obes. 2011;35: 1427–1432. 10.1038/ijo.2011.9 [DOI] [PubMed] [Google Scholar]
- 17. Yudkin JS, Juhan-Vague I, Hawe E, Humphries SE, di Minno G, Margaglione M, et al. Low-grade inflammation may play a role in the etiology of the metabolic syndrome in patients with coronary heart disease: The HIFMECH study. Metabolism 2004;53: 852–857. [DOI] [PubMed] [Google Scholar]
- 18. Ridker PM, Cook N. Clinical usefulness of very high and very low levels of C-reactive protein across the full range of framingham risk scores. Circulation 2004;109: 1955–1959. [DOI] [PubMed] [Google Scholar]
- 19. Nieuwdorp M, Stroes ES, Meijers JC, Buller H. Hypercoagulability in the metabolic syndrome. Curr Opin Pharmacol 2005;5: 155–159. [DOI] [PubMed] [Google Scholar]
- 20. Rossner S, Bo WJ, Hiltbrandt E, Hinson W, Karstaedt N, Santago P, et al. Adipose tissue determinations in cadavers—a comparison between cross-sectional planimetry and computed tomography. Int J Obes 1990;14: 893–902. [PubMed] [Google Scholar]
- 21. Schoen RE, Thaete FL, Sankey SS, Weissfeld JL, Kuller LH. Sagittal diameter in comparison with single slice CT as a predictor of total visceral adipose tissue volume. Int J Obes Relat Metab Disord 1998;22: 338–342. [DOI] [PubMed] [Google Scholar]
- 22. Sipola P, Hedman M, Onatsu J, Turpeinen A, Halinen M, Jäkälä P, et al. Computed tomography and echocardiography together reveal more high-risk findings than echocardiography alone in the diagnostics of stroke etiology. Cerebrovasc Dis. 2013;35: 521–530. 10.1159/000350734 [DOI] [PubMed] [Google Scholar]
- 23. Taina M, Vanninen R, Hedman M, Jäkälä P, Kärkkäinen S, Tapiola T, et al. Left atrial appendage volume increased in more than half of patients with cryptogenic stroke. PLoS One. 2013;8: e79519 10.1371/journal.pone.0079519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24: 35–41. [DOI] [PubMed] [Google Scholar]
- 25. Pepi M, Evangelista A, Nihoyannopoulos P, Flachskampf FA, Athanassopoulos G, Colonna P, et al. European Association of Echocardiography. Recommendations for echocardiography use in the diagnosis and management of cardiac sources of embolism: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr. 2010;11: 461–76. 10.1093/ejechocard/jeq045 [DOI] [PubMed] [Google Scholar]
- 26. DiTomasso D, Carnethon MR, Wright CM, Allison MA. The association between visceral fat and calcified atherosclerosis are stronger in women than men. Atherosclerosis 2010;208: 531–536. 10.1016/j.atherosclerosis.2009.08.015 [DOI] [PubMed] [Google Scholar]
- 27. Salmenniemi U, Ruotsalainen E, Vänttinen M, Vauhkonen I, Pihlajamäki J, Kainulainen S, et al. High amount of visceral fat mass is associated with multiple metabolic changes in offspring of type 2 diabetic patients. Int J Obes. 2005;29: 1464–70. [DOI] [PubMed] [Google Scholar]
- 28. Salmenniemi U, Ruotsalainen E, Pihlajamäki J, Vauhkonen I, Kainulainen S, Punnonen K, et al. Multiple Abnormalities in Glucose and Energy Metabolism and Coordinated Changes in Levels of Adiponectin, Cytokines, and Adhesion Molecules in Subjects With Metabolic Syndrome. Circulation. 2004;110: 3842–8. [DOI] [PubMed] [Google Scholar]
- 29. United Nations Scientific Committee on the Effects of Atomic Radiation (2010). Sources and effects of ionizing radiation, vol. 1 United Nations; Available: http://www.unscear.org/docs/reports/2008/09-86753_Report_2008_Annex_A.pdf. [Google Scholar]
- 30. Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Visceral adipose tissue: Relations between single-slice areas and total volume. Am J Clin Nutr 2004;80: 271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K, et al. Abdominal fat: Standardized technique for measurement at CT. Radiology 1999;211: 283–286. [DOI] [PubMed] [Google Scholar]
- 32. Mosteller RD. Simplified calculation of body-surface area. N Engl J Med 1987;317: 1098 [DOI] [PubMed] [Google Scholar]
- 33. Cohen J. Statistical Power Analysis for the Behavioral Sciences (second ed.). Lawrence Erlbaum Associates; 1998. pp. 273–88. [Google Scholar]
- 34. Karttunen V, Alfthan G, Hiltunen L, Rasi V, Kervinen K, Kesäniemi YA, et al. Risk factors for cryptogenic ischaemic stroke. Eur J Neurol. 2002;9: 625–32. [DOI] [PubMed] [Google Scholar]
- 35. Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes 2008;32: 959–966. 10.1038/ijo.2008.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vague J. The degree of masculine differentiation of obesities: A factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr 1956;4: 20–34. [DOI] [PubMed] [Google Scholar]
- 37. Hanzu FA, Palomo M, Kalko SG, Parrizas M, Garaulet M, Escolar G, et al. Translational evidence of endothelial damage in obese individuals: inflammatory and prothrombotic responses. J Thromb Haemost. 2011;9: 1236–1245. 10.1111/j.1538-7836.2011.04285.x [DOI] [PubMed] [Google Scholar]
- 38. Alessi MC, Peiretti F, Morange P, Henry M, Nalbone G, Juhan-Vague I. Production of plasminogen activator inhibitor 1 by human adipose tissue: Possible link between visceral fat accumulation and vascular disease. Diabetes 1997;46: 860–867. [DOI] [PubMed] [Google Scholar]
- 39. Mertens I, Van der Planken M, Corthouts B, Wauters M, Peiffer F, De Leeuw I, et al. Visceral fat is a determinant of PAI-1 activity in diabetic and non-diabetic overweight and obese women. Horm Metab Res 2011;33: 602–607. [DOI] [PubMed] [Google Scholar]
- 40. Uchida Y, Takeshita K, Yamamoto K, Kikuchi R, Nakayama T, Nomura M, et al. Stress augments insulin resistance and prothrombotic state: role of visceral adipose-derived monocyte chemoattractant protein-1. Diabetes. 2012;61: 1552–1561. 10.2337/db11-0828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Starr ME, Hu Y, Stromberg AJ, Carmical JR, Wood TG, Evers BM, et al. Gene expression profile of mouse white adipose tissue during inflammatory stress: age-dependent upregulation of major procoagulant factors. Aging Cell. 2013;12: 194–206. 10.1111/acel.12040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89: 2548–2556. [DOI] [PubMed] [Google Scholar]
- 43. Davi G, Guagnano MT, Ciabattoni G, Basili S, Falco A, Marinopiccoli M, et al. Platelet activation in obese women: role of inflammation and oxidant stress. J Am Med Assoc. 2002;288: 2008–2014. [DOI] [PubMed] [Google Scholar]
- 44. Mazzoccoli G, Copetti M, Dagostino MP, Grilli M, Fontana A, Pellegrini F, et al. Epicardial adipose tissue and idiopathic deep venous thrombosis: an association study. Atherosclerosis. 2012;223: 378–383. 10.1016/j.atherosclerosis.2012.05.033 [DOI] [PubMed] [Google Scholar]
- 45. Gautier A, Bonnet F, Dubois S, Massart C, Grosheny C, Bachelot A, et al. Associations between visceral adipose tissue, inflammation and sex steroid concentrations in men. Clin Endocrinol 2013;78: 373–378. 10.1111/j.1365-2265.2012.04401.x [DOI] [PubMed] [Google Scholar]
- 46. Karcher HS, Holzwarth R, Mueller HP, Ludolph AC, Huber R, Kassubek J, et al. Body fat distribution as a risk factor for cerebrovascular disease: an MRI-based body fat quantification study. Cerebrovasc Dis. 2013;35: 341–348. 10.1159/000348703 [DOI] [PubMed] [Google Scholar]
- 47. Al Chekakie MO, Welles CC, Metoyer R, Ibrahim A, Shapira AR, Cytron J, et al. Pericardial fat is independently associated with human atrial fibrillation. J Am Coll Cardiol. 2010;56: 784–788. 10.1016/j.jacc.2010.03.071 [DOI] [PubMed] [Google Scholar]
- 48. Klopfenstein BJ, Kim MS, Krisky CM, Szumowski J, Rooney WD, Purnell JQ. Comparison of 3 T MRI and CT for the measurement of visceral and subcutaneous adipose tissue in humans. Br J Radiol 2012;85: 826–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sjostrom L, Kvist H, Cederblad A, Tylen U. Determination of total adipose tissue and body fat in women by computed tomography, 40K, and tritium. Am J Physiol 1986;250: 736–745. [DOI] [PubMed] [Google Scholar]
- 50. Thaete FL, Colberg SR, Burke T, Kelley DE. Reproducibility of computed tomography measurement of visceral adipose tissue area. Int J Obes Relat Metab Disord 1995;19: 464–467. [PubMed] [Google Scholar]
- 51. Chowdhury B, Sjostrom L, Alpsten M, Kostanty J, Kvist H, Löfgren R. A multicompartment body composition technique based on computerized tomography. Int J Obes Relat Metab Disord 1994;18: 219–234. [PubMed] [Google Scholar]
- 52. Berker D, Koparal S, Isik S, Pasaoglu L, Aydin Y, Erol K, et al. Compatibility of different methods for the measurement of visceral fat in different body mass index strata. Diagn Interv Radiol 2010;16: 99–105. 10.4261/1305-3825.DIR.2749-09.1 [DOI] [PubMed] [Google Scholar]
- 53. Carroll JF, Fulda KG, Chiapa AL, Rodriquez M, Phelps DR, Cardarelli KM, et al. Impact of race/ethnicity on the relationship between visceral fat and inflammatory biomarkers. Obesity 2009;17: 1420–1427. 10.1038/oby.2008.657 [DOI] [PubMed] [Google Scholar]
- 54.American FactFinder. Available: http://factfinder2.census.gov.
- 55. Kuhns LR, Borlaza GS, Seigel R, Thornbury JR. External anatomic landmarks of the abdomen related to vertebral segments: Applications in cross-sectional imaging. Am J Roentgenol 1978;131: 115–117. [DOI] [PubMed] [Google Scholar]
- 56. Arnett DK, Jacobs DR Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: The minnesota heart survey, 1980–1982 to 2000–2002. Circulation 2005;112: 3884–3891. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
Based on legal restrictions, data cannot be made available in the paper, the supplemental files, or a public repository. Readers may contact Antti Muuronen to request the data. Data are also available from the Kuopio University Hospital Ethics Committee for researchers who meet the criteria for access to confidential data.