Abstract
Background:
National guidelines call for exercise of at least moderate intensity; however, recommending self-paced exercise may lead to better adherence, particularly among overweight and obese adults.
Purpose:
Test proof-of-concept for recommending self-paced exercise among overweight adults.
Methods:
Fifty-nine healthy, low-active (exercise <60 min/week), overweight (Body Mass Index: 25.0-39.9) adults (18-65) received a six-month print-based exercise promotion program with the goal of walking 30-60 min/day. Participants were surreptitiously randomly assigned to receive a recommendation for either self-paced (n=30) or moderate (64-76% maximum heart rate; n=29) intensity exercise. All participants used electronic diaries and heart rate monitors to track exercise frequency, duration, and intensity.
Results:
The self-paced condition reported more min/week of walking (f2=0.17, p=.045) and a trend toward greater exercise-related energy expenditure/week (f2=0.12; p=0.243), corresponding to approximately 26 additional min/week and 83 additional kcals/week over six months.
Conclusions:
Explicit recommendation for self-paced exercise may improve adherence to exercise programs among overweight and obese adults.
Approximately 70% of U.S. adults are overweight or obese [1]. Despite the benefits of regular exercise among this population, only 28% meet the minimum national recommendation of 1000 kcals/week of exercise-related energy expenditure (EEE) [2-4]. Thus, there is an urgent need to improve adherence to exercise programs for overweight adults.
Consistent with self-determination theory [5, 6], some researchers have argued that adherence to exercise programs may improve if exercise guidelines and individual prescriptions emphasized self-selected intensity (i.e., self-paced) exercise instead of the current recommendation for moderate intensity exercise [7-9]. Indeed, several studies conducted in a laboratory setting have shown that self-paced exercise results in greater feelings of perceived autonomy, a more positive immediate affective (i.e., hedonic) response, and, using analogue measures of exercise behavior (e.g., behavioral choice procedures), greater preference for self-paced relative to imposed moderate intensity exercise [10-15]. Moreover, these effects are more pronounced among overweight adults [10] who often experience moderate intensity exercise as aversive [16].
Despite preliminary support from laboratory studies, no study to date has compared the relative effects of prescribing self-paced versus moderate intensity exercise in the context of a field-based exercise promotion program. Accordingly, the present study employed a randomized design in a preliminary comparison of the effects of recommending self-paced versus moderate intensity (i.e., 64-76% of heart rate (HR) maximum) exercise on adherence to a six-month walking program among previously low-active overweight adults. Primary outcomes were minutes per week of exercise and EEE over the six-month program. Secondary outcomes were mean intensity of exercise sessions and changes in aerobic fitness.
Methods
Participants
Participants were 59 healthy, low-active (< 60 min/week of structured exercise), overweight and obese (body mass index (BMI): 25.0-39.9), community-dwelling adults (ages 18-65) from the greater Providence, RI area. Participants were predominantly female (88%), with mean age of 47.71 years (SD=11.06) and body mass index 31.93 kg/m2 (SD=3.99). A majority of participants were employed (85%), reported household income ≥ $50,000/year (54%), and self-identified as Non-Hispanic White (76%). There were no between-group differences in baseline demographics (p>.05).
Procedures
Participants were recruited via newspaper, internet, radio, and brochures distributed throughout the community. The stated purpose of the study was to test an exercise promotion program focusing on purposeful walking for exercise. All participants were instructed to target one 30-60-min walking session at least five days per week, for a goal of 150-300 min/week of walking, consistent with national guidelines [2, 4]. Walking was emphasized in order to reduce potential between-condition variability in mode of exercise, and because it is preferred among the general population [17] and among overweight and obese adults [18, 19]. In order to help them overcome barriers to regular exercise, all participants received a six-month print-based exercise promotion program (for more details on this program see [20]).
To test the study question, participants were surreptitiously randomly assigned to receive a recommendation for either self-paced or moderate intensity walking. Specifically, participants randomized to the moderate intensity condition were given the following instructions:
We want you to walk at a pace that achieves a heart rate range of _____to _____ [64-76% of maximal HR (i.e., 220-age)]. For safety and study purposes, we ask that you not exceed a heart rate of _____ [76% of age-predicted maximal HR]. During the first few weeks of the study, we recommend starting out slowly to achieve a heart rate at the lower end of your prescribed range. You should then gradually increase your pace but always stay within the prescribed range for the entire session.
Participants in the self-paced condition were given the following instructions:
We want you to select your own pace when walking for exercise. For safety and study purposes, we ask that you not exceed a heart rate of _____ [76% of age-predicted maximal HR].
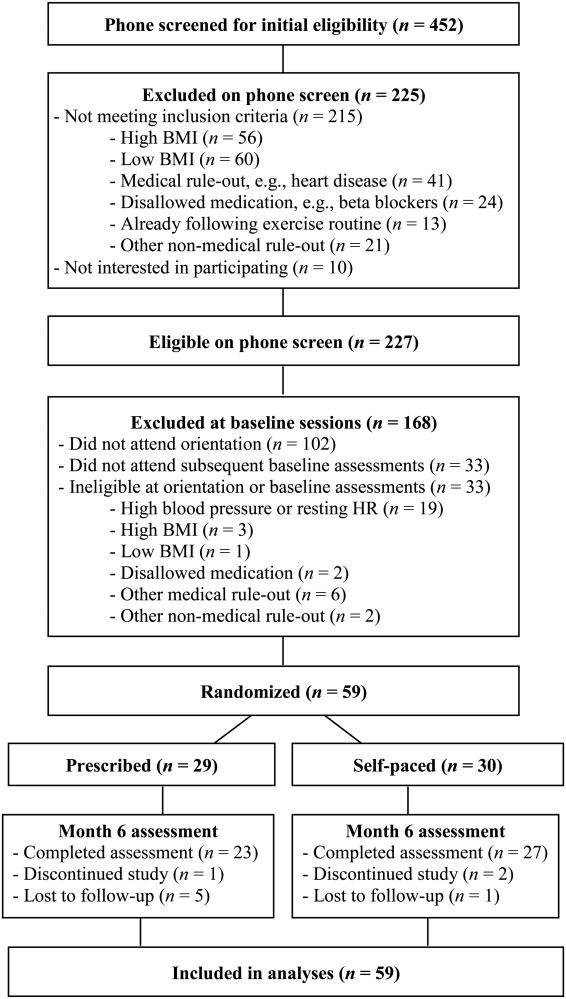
In order to reduce expectancy effects, participants were blinded to the true purpose of the study (i.e., comparison of self-paced versus prescribed moderate intensity), as confirmed by post-study debriefings. The study protocol was approved by the Brown University IRB. Figure 1 illustrates participant flow through the study.
Figure 1.
Participant Flow
Measures
Exercise behavior
Participants used handheld electronic diaries (HP iPAC 111) to complete ecological momentary assessment (EMA) over the course of the six-month intervention. Participants were instructed to indicate, in real time, each time they began and ended a session of structured walking-for-exercise. When available, these real-time data reports were used to compute number of minutes of exercise for each session. Additionally, each morning participants were asked to indicate whether they had exercised the previous day and, if so, whether they had reported the exercise in real time in their e-diary. Participants completed 87% of these daily morning reports over the 6-month study period, with no differences between conditions (p>.05). For 81% of the exercise sessions that participants reported on the daily morning report (i.e., participant indicated that they had exercised the previous day), participants reported completing real-time exercise reports on the previous day at the time of the exercise session (and, in all cases, they had done so), and thus the number of minutes of exercise was computed based on the real-time data. However, for the remaining 19% of exercise sessions reported on the morning report, participants reported that they did not record the exercise in real time (and, in all cases, they had not done so). In these situations, participants were asked to retrospectively report the number of minutes of exercise completed the previous day.
Exercise intensity
HR monitors displayed minimum, maximum, and mean HR for the relevant exercise session, which participants then entered into their e-diary. Using these procedures HR data were collected for 72% of the exercise sessions that were reported in real time over the six-month study period. HR data were used to compute mean exercise intensity across exercise sessions, and, in combination with minutes of exercise, to compute EEE.
Aerobic fitness
Participants completed a one-mile sub-maximal treadmill fitness test at baseline and month six. Peak VO2 (mL/kg/min) was estimated as a function of time taken to complete the one-mile walk, heart rate during the walk, age, body mass index, and gender. In previous research, estimated peak VO2 using this fitness test has shown correlations with observed peak VO2 of r ≥ .85 among community dwelling adults [21, 22].
Statistical Analyses
A single linear mixed effects regression model was used to estimate the treatment effects on min/week of exercise (i=1,2,…,N, j=1,2,…,J where J=total number of weeks of EMA per participant, i=1,…N participants) with a subject-specific intercept included to account for within-subject correlation in the outcome over time. Daily min of exercise was nested within week within participant. A log transformation was used to bring the initially skewed distribution towards normality. Mixed effects models include a likelihood-based approach to estimation and thus make use of all available data (on the intent-to-treat sample) without directly imputing missing outcome values. Similarly, to estimate effects of treatment on intensity (% of maximum heart rate) and EEE mixed effects regression models were used with the outcome variables regressed on time and treatment assignment, including a subject specific intercept, and adjusting standard errors for clustering over time. EEE was calculated as a function of minutes of walking over the six-month intervention weighted by intensity of walking as assessed through mean HR at each exercise bout. Finally, we estimated effects of treatment on within- and between-group changes over time in aerobic fitness (i.e., estimated peak VO2) using a mixed effects model with subject specific intercepts. Analyses were conducted using SPSS 18.0 and SAS 9.3.
Results
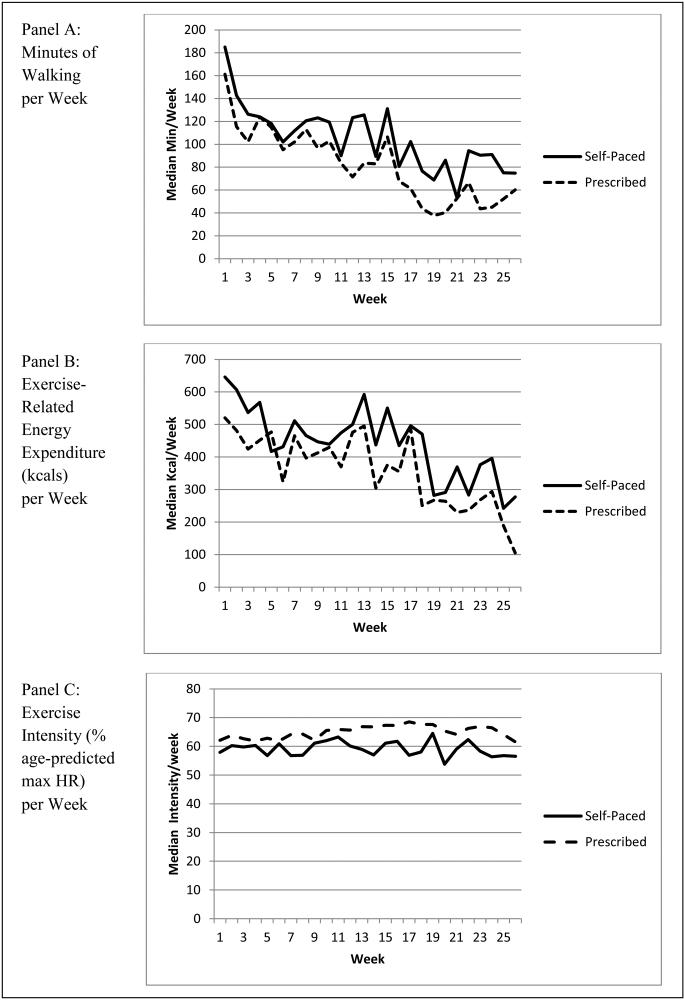
Participants in the self-paced condition reported more walking (b=1.24, se=.64, f2=0.17; p=.045), corresponding to approximately 26 additional min/week during the six-month period or 17% of the minimum recommendation of 150 min/week (Figure 2a). Additionally, participants in the self-paced condition exhibited a non-significant trend toward greater EEE (b=0.02, se=.0.13, f2=0.12; p=.243) than participants in the prescribed moderate intensity condition, corresponding to approximately 83 additional kcals/week on average during the six-month walking program (Figure 2b).
Figure 2.
Unadjusted Median Weekly Minutes of Walking (Panel A), Exercise-related Energy Expenditure (Panel B), and Exercise Intensity (Panel C) During Six-Month Study Period.
Note. Data are unadjusted; see text for analyses.
There was a non-significant trend toward higher intensity of exercise sessions in the prescribed moderate intensity (mean=62.0%, sd=14.3) versus self-paced (mean=57.8%, sd=15.3) conditions, b=−2.74, SE=2.18, f2=0.09, p=.0.21. Finally, there were significant increases in estimated peak VO2 (mL/kg/min) from baseline to month 6 within the self-paced (baseline mean=22.4, sd=7.0; month 6 mean=24.2, sd=4.8; b=2.27, se=0.62, d=0.31, p<.01) and prescribed moderate intensity (baseline mean=23.6, sd=6.2; month 6 mean=26.2, sd=5.9; b=1.78, se=0.69, d=0.42, p=0.01) conditions, but no between-group differences at month six when controlling for baseline values (b=−0.02, se =0.90, p=0.98).
Discussion
Consistent with self-determination theory [5, 6] and recent arguments in favor of recommending self-paced exercise [7-9], overweight adults who were randomly assigned to self-select their walking intensity exercised for more min/week and exhibited a non-significant trend toward greater EEE relative to adults who were prescribed a specific moderate intensity range based on national guidelines. The fact that there was merely a trend toward greater EEE in the self-paced condition despite the greater number of minutes of exercise in that condition is explained by the slightly greater (though statistically non-significant) intensity of exercise among participants in the moderate intensity condition (i.e., EEE is a function of total duration and intensity). That is, although participants in the self-paced condition walked for more minutes/week on average than participants in the moderate intensity condition, the between-group effects on EEE were attenuated by the slightly lower intensity of walking in the self-paced condition.
While the small difference in mean exercise intensity between the two conditions impacted between-group differences in EEE (by definition), this small difference in intensity also suggests that a recommendation for self-paced exercise does not lead to exercise of a significantly lower intensity than from a specific prescription for moderate intensity exercise (i.e., 64-76% of maximum heart rate). In this case, the similar mean intensity in the two conditions was due to the fact that participants in the prescribed moderate intensity condition exercised at an intensity that was, on average, below the prescribed range, which is perhaps not surprising for a group of overweight and previously low-active adults. The greater number of minutes of exercise reported in the self-paced condition, despite the similar mean intensity of exercise in the two conditions, suggests that there is something about being able to choose one’s own intensity—independent of the actual intensity of the exercise performed—that makes people more likely to exercise. The latter is consistent with recent laboratory findings in which both choice of intensity and (actual) lower intensity of exercise contributed to greater preference for self-paced versus imposed higher intensity exercise among previously low-active adults [14, 15].
While participants in both conditions showed mean increases in aerobic fitness, there was no between-group difference in fitness change over the six-month period. This lack of between-group differences is perhaps not surprising, as changes in fitness are largely a function of exercise intensity rather than volume of exercise (i.e., EEE) [23]. Nonetheless, the potential for a greater volume of exercise resulting from self-paced exercise may confer health benefits on overweight and obese adults independent of increased fitness [24]. It should also be noted that the present study used a submaximal fitness test to estimate peak VO2 rather than directly observing peak VO2. Such direct observation of peak VO2, including maximal fitness testing, would be beneficial in determining fitness changes in future research comparing self-paced to prescribed moderate intensity exercise.
Limitations of the present study include the relatively short study period, the small sample size and corresponding lack of statistical power, the predominantly female and relatively affluent participant group, and the high rate of pre-randomization ineligibility.
In summary, this proof-of-concept study provides preliminary evidence that recommending self-paced exercise, as compared to the moderate intensity exercise recommended in national guidelines [2, 4], yields greater adherence (i.e., increased minutes of exercise) to an exercise program among overweight and obese adults. From a theoretical perspective, the present findings support the notion that increased autonomy (operationalized in this study as the explicit recommendation to choose one’s exercise intensity) leads to increases in the target behavior (i.e., exercise). However, there was no significant difference between the two conditions on mean intensity of exercise or EEE (see Figure 2). Nor were there differences between the two conditions in changes in aerobic fitness. Moreover, neither condition came close to the 150 min/week of moderate intensity exercise that is recommended in national guidelines [2, 4]. Thus, despite significantly greater adherence in the self-paced condition, it cannot be concluded—based on the present findings—that a recommendation for self-paced exercise leads to significantly greater health benefits (i.e., increased fitness, EEE) than the current moderate intensity exercise guidelines. Nonetheless, given the significant findings for minutes of exercise and the trend toward greater EEE in the self-paced condition, a larger trial with a more diverse sample of individuals and a longer follow-up period is warranted.
Acknowledgements
This project was funded by the National Cancer Institute (R21CA137211; Williams, PI). We would like to thank Bess Marcus and Beth Bock for the use of their print-based exercise promotion intervention. Special thanks to Jason Frezza for EMA programming, David Upegui and Laura Dionne for data management, and Fred Holloway for research assistance.
Footnotes
Statement of Conflict of Interest and Adherence to Ethical Standards:
David M. Williams, Shira Dunsiger, Robert Miranda Jr., Chad J. Gwaltney, Jessica A. Emerson, Peter M. Monti, and Alfred F. Parisi declare that they have no conflict of interest.
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
References
- 1.National Center for Health Statistics . Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: 2013. [PubMed] [Google Scholar]
- 2.Physical Activity Guidelines Advisory Committee . Physical Activity Guidelines Advisory Committee Report. U.S. Department of Health and Human Services; Washington, DC: 2008. [DOI] [PubMed] [Google Scholar]
- 3.Young DR, Jerome GJ, Chen C, Laferriere D, Vollmer WM. Patterns of physical activity among overweight and obese adults. Prev Chronic Dis. 2009;6(3):A90. [PMC free article] [PubMed] [Google Scholar]
- 4.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 5.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 6.Ryan RM, Williams GC, Partrick H, Deci EL. Self-determination theory and physical activity: the dynamics of motivation in development and wellness. Hellenic Journal of Psychology. 2009;6:107–24. [Google Scholar]
- 7.Ekkekakis P. Let them roam free? Physiological and psychological evidence for the potential of self-selected exercise intensity in public health. Sports Med. 2009;39(10):857–88. doi: 10.2165/11315210-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Parfitt G, Alrumh A, Rowlands AV. Affect-regulated exercise intensity: Does training at an intensity that feels 'good' improve physical health? J Sci Med Sport. 2012;15(6):548–53. doi: 10.1016/j.jsams.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Williams DM. Exercise, affect, and adherence: An integrated model and a case for self-paced exercise. J Sport Exerc Psychol. 2008;30(5):471–96. doi: 10.1123/jsep.30.5.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekkekakis P, Lind E. Exercise does not feel the same when you are overweight: the impact of self-selected and imposed intensity on affect and exertion. Int J Obes. 2006;30(4):652–60. doi: 10.1038/sj.ijo.0803052. [DOI] [PubMed] [Google Scholar]
- 11.Lind E, Ekkekakis P, Vazou S. The affective impact of exercise intensity that slightly exceeds the preferred level: 'pain' for no additional 'gain'. J Health Psychol. 2008;13(4):464–8. doi: 10.1177/1359105308088517. [DOI] [PubMed] [Google Scholar]
- 12.Parfitt G, Rose EA, Burgess WM. The psychological and physiological responses of sedentary individuals to prescribed and preferred intensity exercise. Br J Health Psychol. 2006;11(Pt 1):39–53. doi: 10.1348/135910705X43606. [DOI] [PubMed] [Google Scholar]
- 13.Rose EA, Parfitt G. A quantitative analysis and qualitative explanation of the individual differences in affective responses to prescribed and self-selected exercise intensities. J Sport Exerc Psychol. 2007;29:281–309. doi: 10.1123/jsep.29.3.281. [DOI] [PubMed] [Google Scholar]
- 14.Vazou-Ekkekakis S, Ekkekakis P. Affective consequences of imposing the intensity of physical activity: Does the loss of perceived autonomy matter? Hellenic Journal of Psychology. 2009;6:125–44. [Google Scholar]
- 15.Williams DM, Raynor HA. Disentangling the effects of choice and intensity on affective response to and preference for self-selected-versus imposed-intensity physical activity. Psychol Sport Exerc. 2013;14:767–75. [Google Scholar]
- 16.Mattsson E, Larsson UE, Rossner S. Is walking for exercise too exhausting for obese women? Int J Obes Relat Metab Disord. 1997;21(5):380–6. doi: 10.1038/sj.ijo.0800417. [DOI] [PubMed] [Google Scholar]
- 17.Siegel PZ, Brackbill RM, Heath GW. The epidemiology of walking for exercise: implications for promoting activity among sedentary groups. Am J Public Health. 1995;85(5):706–10. doi: 10.2105/ajph.85.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DiPietro L, Williamson DF, Caspersen CJ, Eaker E. The descriptive epidemiology of selected physical activities and body weight among adults trying to lose weight: the Behavioral Risk Factor Surveillance System survey, 1989. Int J Obes Relat Metab Disord. 1993;17(2):69–76. [PubMed] [Google Scholar]
- 19.MMWR Prevalence of leisure-time physical activity among overweight adults--United States, 1998. Morb Mortal Wkly Rep. 2000;49(15):326–30. [PubMed] [Google Scholar]
- 20.Williams DM, Papandonatos GD, Jennings EG, et al. Does tailoring on additional theoretical constructs enhance the efficacy of a print-based physical activity promotion intervention? Health Psychol. 2011;30:432–441. doi: 10.1037/a0023084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Widrick J, Ward A, Ebbeling C, Clemente E, Rippe JM. Treadmill validation of an over-ground walking test to predict peak oxygen consumption. Eur J Appl Physiol. 1992;64:304–308. doi: 10.1007/BF00636216. [DOI] [PubMed] [Google Scholar]
- 22.Kline GM, Porcari JP, Hintermeister R, et al. Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Med Sci Sports Exerc. 1987;19:253–259. [PubMed] [Google Scholar]
- 23.Meyer T, Auracher M, Heeg K, Urhausen A, Kindermann W. Effectiveness of low-intensity endurance training. Int J Sports Med. 2007;28:33–39. doi: 10.1055/s-2006-924037. [DOI] [PubMed] [Google Scholar]
- 24.Lee IM, Rexrode KM, Cook NR, Manson JE, Buring JE. Physical activity and coronary heart disease in women: Is "no pain, no gain" passe? JAMA. 2001;285:1447–1454. doi: 10.1001/jama.285.11.1447. [DOI] [PubMed] [Google Scholar]