Abstract
Objective
To assess the validity of 5 parental stage of change (SOC) measures: (1) providing 5 servings/d of fruits and vegetables (FV), (2) limiting television to 2 hr/d (TV), (3) helping child get 1 hr/d physical activity (PA), (4) limiting sugary drinks to 1 serving/wk (SD), and (5) limiting fruit juice to 4–6 oz/d (FJ).
Design
Cross-sectional instrument development study. Construct validity was evaluated by examining whether parental self-efficacy (SE), parental readiness ladder (ladder), and child’s behavioral levels (e.g., FV consumption) exhibited a theoretically consistent pattern across the SOC.
Setting/Participants
Convenience sample (n=283) of parents of children ages 4–10.
Measures
Survey assessed SOC, ladder and child-behavioral level score for each topic (FV, TV, PA, SD, FJ), and SE for each except TV.
Analysis
Analysis of variance with Tukey-Kramer post hoc tests examined whether variables differed by SOC.
Results
Percentage of parents in the pre-action SOC included 34% (PA), 39% (FV), 42% (SD), 45% (TV) and 63% (FJ). SE, ladder and behavioral level differed significantly by SOC for each topic area (p<.001). Maintenance SOC was significantly higher than pre-action SOC.
Conclusion and Implications
Measured variables exhibited a theoretically consistent pattern across SOC, suggesting construct validity and potential utility for obesity prevention efforts.
Keywords: readiness, measures, parents, nutrition, television, physical activity, vegetables, pediatric obesity, primary health care, health behavior
INTRODUCTION
A third of all children are either overweight or obese,1 putting them at risk for a range of adverse outcomes including diabetes and cardiovascular disease.2,3 Interventions for children are needed to prevent immediate consequences of obesity (e.g., type 2 diabetes) as well as its related risks in adulthood.4 Health care providers including pediatricians, dietitians, nutrition educators and other allied health care professionals (herein called providers) have an important role to play in addressing this problem.5,6 Practice recommendations put forth by the Expert Committee,7 a panel representing major professional health organizations (e.g., American Academy of Pediatrics, Academy of Nutrition and Dietetics, American College of Sports Medicine) urge providers to assess self-efficacy and readiness to change for specific dietary practices and levels of physical and sedentary activity at each well-child visit.7 However, there is a lack of validated measures available to assess a parent’s readiness to support their child’s healthful eating and activity behaviors.
Readiness to change a behavior, also known as stage of change (SOC), is the central organizing construct of the transtheoretical model (TTM), a behavior change framework that explains the processes and principles of health behavior change.8,9 The TTM categorizes readiness into sequential stages: (1) precontemplation (PC), the person is not intending to change behavior to meet a specified behavioral criterion such as consuming > 5 servings of fruit and vegetables a day; (2) contemplation (C), thinking about making a change to meet the criterion in the next 6 months; (3) preparation (PR), intending to change and meet the criterion in the next month; (4) action (A), meeting the health criterion but for less than 6 months; and (5) maintenance (M), meeting the health criterion for more than 6 months. The TTM posits that individuals progress through the stages on their way to making a long term behavior change, and this movement is produced to a greater or lesser extent by the model’s independent variables: decisional balance; self-efficacy; and the processes of change.8,9 SOC is often assessed repeatedly so that the intervention for a particular person is adjusted (i.e., stage-based) to promote movement from the person’s current stage to the next higher stage and to prevent the person from moving backwards to an earlier SOC.10,11
The present study evaluated the validity of 5 separate stage of change measures for parental readiness to help their children in meeting the following health recommendations:6,7 (1) providing the child with 5 servings of fruits and vegetables daily (FV); (2) limiting television time (TV) to 2 hours or less every day; (3) promoting 1 hour of moderate intensity physical activity (PA) every day; (4) avoiding sugary drinks (SD); and (5) limiting fruit juice (FJ) to 4–6 oz a day. Four studies have examined parental readiness to help their children with healthful behavior changes.12–15 None used validated behavioral measures to assess parent helping behaviors. This study addressed this gap.
There were 3 hypotheses for the present study based on the extant literature8,16–22 and the theoretical framework of the TTM. The first hypothesis was that parents in stages A and M report that their children engaged in healthier levels of the behavior than those in pre-action stages (PC, C, PR). More specifically, FV and PA behaviors were hypothesized to increase across the stages while TV, SD and FJ were hypothesized to decrease. The second hypothesis was that self-efficacy (SE) for meeting the criterion increases across the SOC. 8–9,18,22 The third hypothesis was that the 2 measures of parental readiness, i.e., SOC and the readiness ladder, correspond to each other such that ladder scores increase across the SOC.
METHODS
Sample
Passive methods were used to recruit this convenience sample. Flyers were posted in health and community centers in the city of Boston and advertisements were posted in local newspapers and online on Craig’s List. Parents or legal guardians (herein called parents) were eligible for the study if they 1) self-identified as the principal care giver of a child who was 4–10 years old, 2) attended the child’s last 2 well-child annual exams, 3) spoke and read English, and 4) were willing to bring their child into the study office for assessments.
Overview of the Procedures
This study was approved by the institutional review boards at UMass Boston and Boston University Medical Campus. The first study procedure was to review the literature for existing SOC measures and for the researchers to develop a draft of the parental SOC measures using guidelines outlined by Reed and colleagues.17 Six content experts were mailed the survey draft and a follow-up phone call was performed to discuss their feedback. The expert feedback, including input on wording, was incorporated into the revised SOC measures and the resulting measures were pilot tested with 6 parents of children aged 4–10 years. The parents were interviewed about their understanding of the meaning of the SOC measures. These cognitive testing results were used to maximize comprehension, through edits to the wording. The next step was a cross-sectional survey study using a convenience sample of parents with children aged 4–10 years. Informed written consent was obtained from the parent and verbal assent was obtained from the children. Parents completed a paper-pencil survey that included demographics, psycho-social, PA, TV, and dietary questionnaires. Parent and child height and weight were measured. Parents received a $20 gift card incentive. Survey data were collected at research offices from August 2009 to August 2011.
Measures
Stage of Change
The 5 SOC measures created for the study are displayed in Supplemental Materials. The structure of the measure included a specific behavioral criterion based on public health guidelines.17 A 5-item response format was used for each behavior except for SD and FJ as content experts proposed that the survey distinguished between those parents in M whose child used to consume these unhealthy beverages but stopped doing so and those parents in M whose child never consumed these beverages. Each response option corresponded to a single stage: 1 = PC; 2 = C; 3 = PR; 4 = A; 5 = M.8
Readiness Ladder
A readiness ladder was created for each target behavior (Supplemental Materials). Readiness ladders have been used as an alternate method of assessing readiness to change.17 These measures used the same behavioral criterion as the corresponding stage measure combined with the stem, “how ready are you to”, and the response options, “on a scale from 0 to 10?” Participants were asked to circle a number from 0 (not ready) to 10 (very ready) or the option “already do [criterion behavior]”. Each number was equally spaced across the page. The response, “already do it,” was coded as 11. The scale was divided into categories, 0–2, 3–4, 5–6, 7–8, 9–10 and 11 (already do it) for ease of interpretation.
Self-efficacy (SE)
SE was defined as a parent’s confidence in his or her ability to help their child engage in the healthful behavior under a variety of difficult situations.23 The present study authors developed SE scales for FV, PA, SD and FJ, (inadvertently a scale for TV was not developed for this study).24 Each scale included 4 items that reflected a range of difficult situations. All scales used the same stem, “how sure are you that you could,” which was followed by the criteria for the target behavior. For example, “how sure you are that you could help your child get 1 hour of moderate intensity physical activity every day, when there are too many other things to worry about.” Items were rated 1=not sure to 5=extremely sure. A sum score for each of the 4 scales was calculated. Cronbach’s alphas for these SE scales24 were .80 (PA), .84 (FV), .86 (FJ), and .87 (SD), which are comparable to alphas for adolescent and adult SE scales for FV (.86) 20, 21 and PA (.82) 22 and a similar parental SE scale developed for fruit and vegetable consumption (.70).25
Physical activity (PA)
Parents were asked to report on whether their child participated in a list of 20 different physical activities in the past 7 days, the number of days each activity was done and minutes each time.26 Parents were given the option to report other physical activities not on the list. Metabolic equivalents were assigned to each of the 20 physical activities and any other activities reported using the youth compendium.27 Metabolic equivalent hours (MET hr/d) then were calculated to estimate the child’s level of physical activity.
Television Time (TV)
A reliable 12-item proxy measure of recreational time was used to assess TV time.28, 29 Parents reported the time their child spent in leisure time activities during the previous day (e.g., TV, computer, reading).
Dietary intake
FV and average daily calories from SD were assessed with the Block Dietary Data Systems Kids Food Screener version 2, which asked about the number of days in the last week 39 items were consumed and the portion size eaten for each item.30 Parents completed the screener for their child. Because the Block combines fruit juice in the fruit CE, a separate question was used to assess FJ consumption. The question asked “how much 100% pure fruit juice with no added sugar does your child drink on a typical day?” and provided some examples such as “100% orange, apple, grape or Juicy Juice”. The response options were, 0=none, 1=less than 6 ounces (less than 1 juice box), 2=about 6 ounces (1 juice box), 3=about 12 ounces (2 juice boxes), 4=about 24 ounces (3 juice boxes) and 5=more than 24 ounces (4 juice boxes).
Anthropometrics
Child’s and parent’s height and weight were measured by a trained research assistant using a portable stadiometer (Seca model 214) and scale (Seca model 882). Participants were asked to remove shoes and heavy garments (coats, sweaters, and belts) prior to the measurement. Body Mass Index (BMI) was calculated (kg/m2) and compared against adult standards for the parents, and norms for BMI percentile for age and gender for children.31
Data Analysis
There are a number of ways to define validity and approach validation.32 The present study used a construct-validation approach that assumed observed variables (e.g., dietary intake) are indicators of the construct (i.e., SOC). Construct validation also depends on the relationship with other constructs in a theoretical context (i.e., TTM). Convergent validity, a form of construct validity, is the convergence of different methods designed to measure the same construct.32 This convergence provides some confirmation that the construct measures what it purports to measure. The readiness ladder was defined as an alternate form of SOC.17 Both measures ask the respondent how ready they are to meet a healthful criterion but the readiness ladder used a visual analogue scale from 0 to 10 whereas the SOC used a 5-item response format that includes a time frame (Supplemental Materials).
Means, standard deviations and frequencies were used to describe the sample. The study hypotheses were tested using analysis of variance (ANOVA) with Tukey-Kramer post hoc analyses to examine pair-wise stage comparisons for all analyses. The Tukey-Kramer tests used adjusted robust standard errors that corrects for non-normal or heteroscedastic data.33 SOC for FV and PA had a small number of participants in PC and C (n=3 and n=12 participants, respectively) thus PC and C were collapsed for these analyses. For the SD and FJ analyses, the sixth category of “my child does not drink [sugary drinks/fruit juice]” was collapsed with the M stage. Effect size estimates were calculated as Eta2 (η2). A variance of 1%, 6% or 14% indicated a small, medium or large effect, respectively.34 For all analyses, the alpha level was set at p <.05. IBM SPSS Statistics for Windows, Version 20.0 released 2011 (Armonk, NY) was used for all analyses except the Tukey-Kramer post hoc tests, which is not available in SPSS. R open source software (http://CRAN.R-project.org/) was used for the post hoc tests.
RESULTS
Of the 319 parents who indicated interest in participating, 304 (95%) completed the survey. Six percent (n= 21) of the 304 were not included because of missing data, language or comprehension issues for a final sample of n=283. Table 1 displays demographic characteristics of the parents. No racial group was in the majority, and the distribution of Black/African American was higher than the Boston urban population. The majority of parents were single (56.9%) and reported an income less than $40,000 (57.8%), which is less than Boston’s median household income of $51,739. About 72% of the parents and 44% of the children were overweight or obese (adults BMI ≥ 25; children BMI ≥ 85th percentile for age and gender).
Table 1.
Anthropometric and Socioeconomic Data for the Sample of Parents and their Children Aged 4–10 years.
| Variable | % | Mean | (SD) | Sample reporting (n) |
|---|---|---|---|---|
| Parent | ||||
| Age | 37.5 | 8.3 | 239 | |
| Sex (% female) | 88.3 | 265 | ||
| Married | 43.1 | 276 | ||
| Income level (<$40,000) | 57.8 | 277 | ||
| Employment (full-time) | 39.7 | 277 | ||
| Education level | 277 | |||
| High school or less | 20.2 | |||
| Some college or trade school | 38.6 | |||
| College degree or more | 41.1 | |||
| Hispanic/Latino Origin | 18.7 | 278 | ||
| Race | 269 | |||
| Black/African American | 42.8 | |||
| White | 39.8 | |||
| Mixed | 7.1 | |||
| BMI | 30.4 | 7.7 | 252 | |
| BMI % overweight < obese | 26.6 | |||
| BMI % obese | 45.6 | |||
| Number of children at home | 2.1 | 1.1 | 279 | |
| Child | ||||
| Age | 6.6 | 2.1 | 251 | |
| Gender (% female) | 53.6 | 252 | ||
| BMI 85th%tile–94th%tile | 22.0 | |||
| BMI 95th%tile and above | 21.6 | 250 | ||
BMI indicates Body Mass Index; BMI % overweight < obese indicated adults with a BMI between 25–29.9; BMI % obese indicated adults with a BMI > 30; BMI 85th%tile–94th%tile indicates children who are at or above the 85th%tile but less than the 95th%tile for age and gender which is considered overweight; BMI 95th%tile and above indicates children at or above the 95th %tile for age and gender which is considered obese.
Table 2 displays distribution of participants’ responses to the stage of change and readiness measures. The percentage of the sample in pre-action stages was 34% (PA), 39% (FV), 42% (SD), 45% (TV) and 63% (FJ). For the readiness ladder, the highest proportion of responses fell in the 8–10 category for most behaviors. Less than 8% of the sample used the lower end of the ladder for FV, PA, TV and SD. Table 2 also provides a mean for the ladder which was calculated by removing those who responded “already do it’ in order to display a mean that was more representative of how the question is typically asked (on 1–10 or 0–10 scale).17
Table 2.
Distribution of the Parent’s Responses to the Stage of Change (SOC) and Readiness Questions.
| Stage of Change % |
Readiness % |
Mean (sd)* | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Behavioral Criterion | n | PC | C | PR | A | M | Already Do It | n | 0–2 | 3–4 | 5–6 | 7–8 | 9–10 | Already Do It | |
| Fruits and Vegetables | 282 | 1.1 | 10.3 | 27.7 | 12.1 | 48.9 | NA | 285 | 0.4 | 1.1 | 4.9 | 22.8 | 47.0 | 23.9 | 8.8 (1.5) |
| TV | 278 | 10.4 | 16.9 | 17.3 | 12.9 | 42.4 | NA | 282 | 5.7 | 7.1 | 12.8 | 14.5 | 34.5 | 25.5 | 7.3 (2.9) |
| TVBed | NA | 279 | 25.1 | 5.7 | 13.3 | 5.4 | 14.7 | 35.8 | 4.4 (3.9) | ||||||
| Physical Activity | 281 | 3.6 | 9.6 | 21.0 | 20.6 | 45.2 | NA | 283 | 0.7 | 2.1 | 8.5 | 13.8 | 53.7 | 21.2 | 8.7 (1.9) |
| Sugary Drinks | 280 | 8.2 | 20.4 | 13.2 | 18.6 | 21.4 | 18.2 | 283 | 4.2 | 7.4 | 14.1 | 13.4 | 36.4 | 24.4 | 7.5 (2.8) |
| Fruit Juice | 283 | 23.0 | 21.9 | 17.7 | 14.1 | 18.7 | 4.6 | 284 | 7.7 | 10.6 | 23.6 | 20.8 | 28.5 | 8.8 | 6.7 (2.8) |
NA indicates that it was not asked; PC, Precontemplation Stage; C, Contemplation Stage; PR, Preparation Stage; A, Action Stage; M, Maintenance Stage; Behavioral criterion for fruit and vegetables was to provide your child with 5 servings of fruits and vegetables every day; TV, limit your child to 2 hr or less of TV every day; TVBed, readiness to remove TV from the bedroom; physical activity, help your child get 1 hour of moderate intensity physical activity; sugary drinks, limit your child to 1 serving per week of sugary drinks; fruit juice, limit your child’s juice intake to no more than 6 ounces of 100% fruit pure juice each day.
Mean (SD) excludes the ‘already do it’ response option.
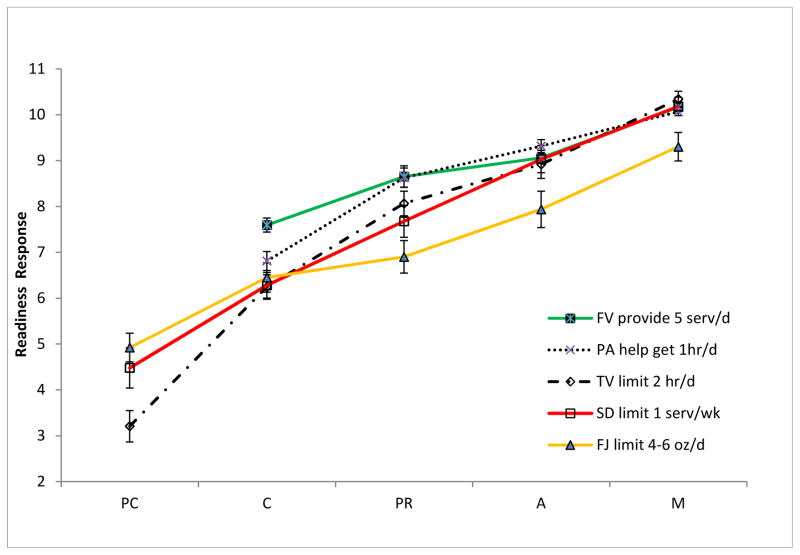
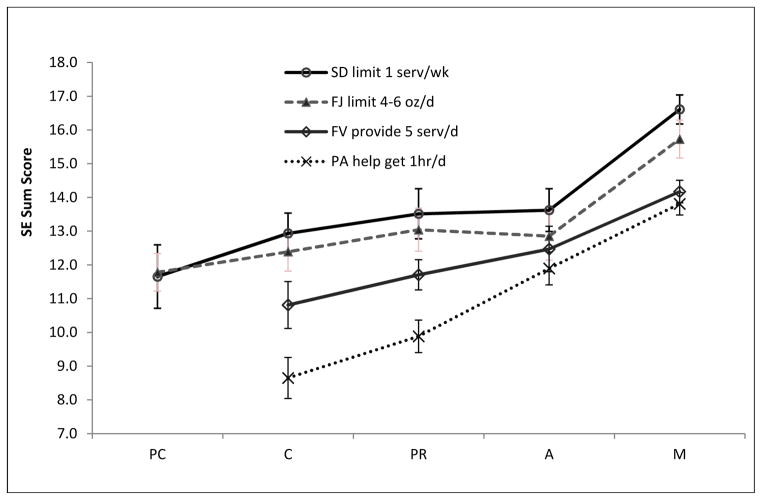
Table 3 displays the means and standard deviations of the variables used to assess construct validity for each SOC measure and the results of the ANOVAs and Tukey-Kramer post hoc analyses and effect size estimates (η2). All omnibus ANOVAs were significant at p<.001. M was significantly different from the pre-action stages for all post hoc comparisons. There were medium to large effect sizes for all behavioral comparisons by SOC (η2 ranged from .08–.16), large effect sizes for all readiness ladder comparisons by SOC (η2 ranged from .28–.62), and medium to large effect sizes for the SE comparisons by SOC (η2 ranged from .10 to .23). Figures 1 and 2 display the readiness ladder and self-efficacy scores and standard error of the mean across their respective stage measure.
Table 3.
Means and Standard Deviation for Behavior, Readiness Ladder and Self-Efficacy Scores across their Corresponding Stage of Change Measure.
| Stage of Change | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | PC | C | PR | A | M | ||||||||||
|
| |||||||||||||||
| n | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | F*** | df | Tukey-Kramera | Eta2 | |
|
|
|||||||||||||||
| Behavior | |||||||||||||||
| FV consumed (cup equivalent) | 254 | * | * | 1.85 | 0.89 | 2.15 | 1.11 | 2.82 | 1.48 | 2.83 | 1.48 | 6.97 | 3,250 | PC/C, PR < M; PC/C < A | .08 |
| TV watched (min/d) | 274 | 188.13 | 80.15 | 207.81 | 104.04 | 203.78 | 145.09 | 165.07 | 109.69 | 106.74 | 85.95 | 11.27 | 4,269 | PC, C, PR, A > M | .14 |
| PA (met hrs/d) | 243 | * | * | 47.19 | 51.36 | 57.38 | 54.89 | 113.39 | 83.09 | 136.54 | 147.77 | 9.16 | 3,239 | PC/C, PR < A, M | .10 |
| SD sugary beverage total kcal/d | 252 | 44.24 | 57.19 | 40.32 | 54.12 | 30.05 | 34.38 | 26.36 | 68.63 | 7.12 | 22.35 | 6.15 | 4,247 | PC, C, PR > M | .09 |
| 100% FJ (servings/d) | 282 | 1.95 | .98 | 1.89 | .91 | 1.88 | .98 | 1.74 | .88 | .97 | .76 | 13.17 | 4,277 | PC, C, PR, A > M | .16 |
| Readiness Ladder | |||||||||||||||
| FV to provide 5 servings/d | 282 | * | * | 7.59 | 1.98 | 8.65 | 1.59 | 9.06 | 0.98 | 10.17 | 1.08 | 42.14 | 3,278 | PC/C < PR, A < M | .31 |
| TV to limit to 2 hr/d | 275 | 3.21 | 2.68 | 6.24 | 2.17 | 8.07 | 2.32 | 8.92 | 1.79 | 10.34 | 1.06 | 108.61 | 4,270 | PC < C <PR, A < M | .62 |
| PA to help get 1 hr/d | 279 | * | * | 6.81 | 2.50 | 8.63 | 1.81 | 9.32 | 1.43 | 10.06 | 1.16 | 42.62 | 3,275 | PC/C < PR, A <M | .32 |
| SD to limit to 1 servings/wk | 278 | 4.48 | 3.20 | 6.28 | 2.55 | 7.68 | 2.35 | 9.03 | 1.86 | 10.18 | 1.53 | 56.03 | 4,273 | PC, C, PR < A < M; PC < PR | .45 |
| FJ to limit to 4–6 oz/d | 283 | 4.92 | 3.21 | 6.45 | 1.96 | 6.90 | 2.50 | 7.94 | 2.48 | 9.30 | 2.19 | 27.17 | 4,278 | PC < C, PR, A < M; C < A | .28 |
| Self-efficacy Score | |||||||||||||||
| FV providing 5 servings/day | 281 | * | * | 10.81 | 3.19 | 11.71 | 3.99 | 12.47 | 4.29 | 14.17 | 3.96 | 10.32 | 3,277 | C, PR < M | .10 |
| PA helping child get 1 hr/day | 278 | * | * | 8.65 | 2.89 | 9.88 | 3.16 | 11.89 | 4.07 | 13.81 | 3.95 | 26.57 | 3,274 | C, PR, A < M; C, PR < A | .23 |
| SD limit 1 serving/wk | 278 | 11.65 | 4.71 | 12.94 | 4.41 | 13.51 | 4.34 | 13.62 | 4.39 | 16.61 | 4.62 | 11.29 | 4,273 | PC, C, PR, A <M | .14 |
| FJ to limit to 4–6 oz/d | 275 | 11.78 | 4.83 | 12.39 | 3.94 | 13.04 | 4.49 | 12.85 | 4.10 | 15.73 | 4.66 | 7.30 | 4,270 | PC, C, PR, A <M | .10 |
FV indicates fruits and vegetables; TV, television; PA, physical activity; SD, sugary drinks, FJ, 100% fruit juice servings with 1 serving equivalent to 4–6 oz/d. PC indicates Precontemplation Stage; C, Contemplation Stage; PR, Preparation Stage; A, Action Stage; M, Maintenance Stage. Behavioral criterion for the FV stage was to provide your child with 5 servings of fruits and vegetables every day; TV, to limit your child to 2 hr or less of TV every day; PA, to help your child get 1 hour of moderate intensity physical activity. SD, to limit your child to 1 serving per week of sugary drinks. FJ, to limit your child’s juice intake to no more than 6 ounces of 100% fruit pure juice each day. Eta2 (η2) is the estimate of the effect size.
PC/C combined because there were so few participants in PC (3 for FV and 12 for PA);
All omnibus comparisons are significant, p<.001.
Tukey-Kramer post hoc comparisons presented only for significant differences at p<.05.
Figure 1.
Readiness Scores across the Corresponding Stages of Change Measure for the Parent Sample (n=283).
FV indicates fruits and vegetables; TV, television; PA, physical activity; SD, sugary drinks, FJ, 100% fruit juice servings with 1 serving equivalent to 4–6 oz/d. PC indicates Precontemplation Stage; C, Contemplation Stage; PR, Preparation Stage; A, Action Stage; M, Maintenance Stage. Behavioral criterion for the FV stage was to provide your child with 5 servings of fruits and vegetables every day; TV, to limit your child to 2 hr or less of TV every day; PA, to help your child get 1 hour of moderate intensity physical activity. SD, to limit your child to 1 serving per week of sugary drinks. FJ, to limit your child’s juice intake to no more than 6 ounces of 100% fruit pure juice each day. PC and C were collapsed for FV and PA.
Figure 2.
Self-Efficacy Scores across the Corresponding Stages of Change Measure for the Parent Sample (n=281).
FV indicates fruits and vegetables; PA, physical activity; SD, sugary drinks, FJ, 100% fruit juice servings. PC indicates Precontemplation Stage; C, Contemplation Stage; PR, Preparation Stage; A, Action Stage; M, Maintenance Stage. Behavioral criterion for the FV stage was to provide your child with 5 servings of fruits and vegetables every day; PA, to help your child get 1 hour of moderate intensity physical activity. SD, to limit your child to 1 serving per week of sugary drinks. FJ, to limit your child’s juice intake to no more than 6 ounces of 100% fruit pure juice each day. PC and C were collapsed for FV and PA. SE indicates self-efficacy. The SE sum score is the sum of the 4 items for the scale (range 4–20).
DISCUSSION
This study assessed the construct validity of 5 SOC measures on parental readiness to help their children engage in healthful behaviors associated with preventing childhood obesity. The findings from this study provide evidence for the validity of SOC measures that are congruent with the behavioral criteria. Overall, levels of behavior and theoretical constructs examined across their respective SOC measure produced the expected patterns based on theory.8,9
Few studies have reported on parental SOC and no studies have been done with the intention of establishing validation. Hildebrand and Betts12 developed a parental SOC for serving more FV and asked experts to assess its face validity. They reported that 43% of low-income mothers with children ages 1–5 were in the PC/C stages for serving more FV, 29% in PR and 28% in A/M. In comparison, the present study had fewer parents who reported being in the pre-action stages of PC/C (11% vs. 43%) and many more who reported A/M (61% vs.28%), although PR was similar (28% vs. 29%). These differences may be due to the criterion used to assess SOC [serving more FV (no amount specified) vs. providing 5 servings of FV/d], the different target population (parents with children 1–5 vs. 4–10 years of age), and demographic characteristics (e.g., 50% vs. 20% who reported high-school education, respectively). It also is possible that the awareness of FV recommendations has increased over time which could affect the degree of socially desirable responding in the present study. Three other studies have developed either a readiness ladder or SOC algorithm to assess parental readiness; however, those measures were designed for weight management behaviors in general (e.g., readiness to make lifestyle changes to help your child lose weight14) and were administered to parents whose children attended a weight management clinic.13–15
The TTM posits that levels of the healthful behavior improve across the stages.8,9 While generally behaviors trended in this direction, the hypothesis that parents in the action stages (A and M) report behavioral levels that are healthier (i.e., closer to the recommended level) than those in the pre-action stages was not supported. Only those parents in M reported significantly healthier levels of the target behavior than the pre-action stages. Often SOC studies collapse stages12,13,18,20,21 making direct comparisons across studies impossible. For example, Hildebrand et al. reported that the higher stages (A/M) were different from the lower stages (PC/C) for parents providing FV.12 Our findings are similar to a study that examined the behavioral validation evidence of PA SOC in 9 adult studies.19 Only 3 of 9 studies found that both A and M had significantly higher PA levels than PC, C, and PR, and 2 other studies found only M was higher than the earlier stages. While more research is needed, A and M could have distinct behavioral profiles.
In the present study, behavioral profiles do not seem to be as strong in A as in M. The behavioral levels in the A stage, generally, were not different from the earlier stages except for the behaviors of FV and PA. Although A and M were generally not significantly different from each other, there is a clear distinction between M and the other stages. Possibly parents with intentions to achieve the health criterion may provide more socially desirable responses resulting in no difference between PR and A for the behavioral levels except for FV and PA. Similarly, underreporting of behavioral levels of TV, SD, and FJ may explain the lack of differentiation between A and the earlier stages. It is possible that parents who are in maintenance have different characteristics than those in the earlier stages suggesting that A and M should not be combined. Studies by Rhee et al. in parents of overweight children found that parental factors were related to stage classification.14,15 More recently they found that parents with a higher income were more likely to be in the A/M stage for improving their child’s physical activity, and parents who viewed their own weight as a health problem were less likely to be in A/M for helping their child eat healthier foods.15 Demographic factors such as income, education and weight status have been associated with misreporting of dietary intake,35 suggesting that if parents in M are different, then those characteristics also could influence the accuracy of their reporting.
Examining the construct of self-efficacy across the SOC is consistent with the expected pattern (Figure 2) of an increase in SE across the stages;8,9 however, only M stage had significantly higher confidence scores. Other studies have found that SE increases across SOC with significant differences between most stages,18,21,22 although as mentioned previously, most studies compare collapsed stages finding action stages higher than pre-action stages.12,20,21 While the present study is cross-sectional, there is some indication that those who are in M have a strong profile (higher self-efficacy, higher readiness, better behavioral levels) that may have implications for focusing intervention or counseling efforts on early stages including A.
A strength of this study is the assessment of convergent validity, a subcategory of construct validity. Figure 1 depicts the linear correspondence between the readiness ladder and SOC measures. The data suggest that responses ranging from 3–5 corresponded with PC whereas responses of 6–7 corresponded to C and 7–8 to PR.
There are limitations to the study including its cross-sectional design, use of a convenience sample and the self-report format. Given that parents reported on their child’s behavioral levels, the reports are likely overestimates of PA and FV and underestimates of TV and SD. The accuracy of parent-reported FJ is more difficult to ascertain. Although the measure’s stem provided a definition of 100% FJ, parents still may not be able to distinguish fruit-flavored beverages (fruit drink) resembling 100% FJ from 100% FJ. The present findings could be a result of parents not ready to reduce 100% FJ or not ready to reduce fruit drink.
As suggested previously, the parents may have given socially desirable responses to the measures, which may be one reason for the lack of distinction between the pre-action stages. The measures were phrased to understand how ready a parent was to help a child engage in healthful behaviors. Parents may be reluctant to report that they are not ready to help a child with a healthful habit. Obesity prevention efforts such as the 5-2-1-0 campaign36 are becoming increasingly more common in clinical practice; therefore, it is possible that parents are more aware of what is recommended. This response bias could intensify if parents are asked face-to-face by a provider, rather than on paper or a Website. These limitations emphasize the need for objective measures of behavior to provide better estimates of the validity of the SOC measures.
There are other possible limitations that may have influenced the findings. One caveat is that the behavioral measures used in this study have not been validated with parents of 4–5 year olds. Another limitation to consider is that the study took place over a period of 2 years in varying seasons, which may have influenced diet and physical activity patterns. Lastly, a possible limitation is the inclusion of parents with children 4–10 years of age, a range that includes varying parent-child relationships and diet and physical activity levels. Nonetheless, the stage measure mused a criterion consistent with the health recommendations for all 4–10 year olds. While a parent of a 4-year-old may have different issues than a parent of a 10-year-old, the purpose of the stage measure is to assess parental readiness to meet the specified recommendation.
Implications
Health promotion advocates, including dietitians, nutrition educators, and researchers can use these measures in efforts to assist families. The measures in this study may have a broader appeal for use in that they do not assume a focus on weight management but rather assess healthful lifestyle behaviors. Dietitians and other health care providers may find the measures useful because they assess issues that providers are encouraged to address regularly.7, 35 The measures may help them provide stage appropriate advice when they are working with parents. Health program planners and researchers should consider using these measures when designing tailored interventions for families with children aged 4–10 years. While future validation of the measures are needed, the readiness ladder may be a good alternative to SOC measures with the caveat that face-to-face administration as opposed to paper-based may lead to overestimation of readiness. Future research should consider examining the validity of the readiness ladder to provide an additional, and perhaps easier, tool to use.
Supplementary Material
Supplementary Table. The Stages of Change (SOC)8 and Readiness Measures as Presented on the Parent Survey.
Practice Points.
Health promotion advocates, including dietitians, nutrition educators, and researchers can use these measures in their work to assist families.
Assessing readiness to change can be done using these brief, validated, measures.
These stage of change measures can be used to provide stage appropriate advice when counseling parents.
Acknowledgments
This study was supported by K07CA113643.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. Epub 2012 Jan 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels SR. Complications of obesity in children and adolescents. Int J Obes (Lond) 2009;33S:S60–5. doi: 10.1038/ijo.2009.20. [DOI] [PubMed] [Google Scholar]
- 3.Steinberger J, Daniels SR, Eckel RH, et al. Progress and challenges in metabolic syndrome in children and adolescents: A scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2009;119:628–47. doi: 10.1161/CIRCULATIONAHA.108.191394. [DOI] [PubMed] [Google Scholar]
- 4.Dietz WH, Robinson TN. Clinical practice: Overweight children and adolescents. N Engl J Med. 2005;352:2100–9. doi: 10.1056/NEJMcp043052. [DOI] [PubMed] [Google Scholar]
- 5.Polacsek M, Orr J, Letourneau L. Impact of a primary care intervention on physician practice and patient and family behavior: Keep ME Healthy---the Maine Youth Overweight Collaborative. Pediatrics. 2009;123:S258–66. doi: 10.1542/peds.2008-2780C. [DOI] [PubMed] [Google Scholar]
- 6.American Heart Association. Dietary recommendations for children and adolescents: A guide for practitioners. Pediatrics. 2006;117:544–59. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 7.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 8.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 9.Prochaska JO, Johnson S, Lee P. The Transtheoretical model of behavior change. In: Shumaker S, Ockene JK, Riekert KA, editors. The Handbook of Health Behavior Change. 3. New York, NY: Springer; 2009. pp. 59–84. [Google Scholar]
- 10.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133:673–93. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 11.Velicer WF, Prochaska JO, Redding CA. Tailored communications for smoking cessation: past successes and future directions. Drug Alcohol Rev. 2006;25:49–57. doi: 10.1080/09595230500459511. [DOI] [PubMed] [Google Scholar]
- 12.Hildebrand DA, Betts NM. Assessment of stage of change, decisional balance, self-efficacy, and use of processes of change of low-income parents for increasing servings of fruits and vegetables to preschool-aged children. J Nutr Educ Behav. 2009;41:110–9. doi: 10.1016/j.jneb.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Campbell M, Benton JM, Werk LN. Parent perceptions to promote a healthier lifestyle for their obese child. Soc Work Health Care. 2011;50:787–800. doi: 10.1080/00981389.2011.597316. [DOI] [PubMed] [Google Scholar]
- 14.Rhee KE, De Lago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics. 2005;116:94–101. doi: 10.1542/peds.2004-2479. [DOI] [PubMed] [Google Scholar]
- 15.Rhee KE, McEachern R, Jelalian E. Parent readiness to change differs for overweight child dietary and physical activity behaviors. J Acad Nutr Diet. 2014;114:1601–1610. doi: 10.1016/j.jand.2014.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marcus BH, Simkin LR. The stages of exercise behavior. J Sports Med Phys Fitness. 1993;33:83–8. [PubMed] [Google Scholar]
- 17.Reed GR, Velicer WF, Prochaska JO, Rossi JS, Marcus BH. What makes a good staging algorithm: examples from regular exercise. Am J Health Promot. 1997;12:57–66. doi: 10.4278/0890-1171-12.1.57. [DOI] [PubMed] [Google Scholar]
- 18.Marshall SJ, Biddle SJ. The transtheoretical model of behavior change: a meta-analysis of applications to physical activity and exercise. Ann Behav Med. 2001;23:229–46. doi: 10.1207/S15324796ABM2304_2. [DOI] [PubMed] [Google Scholar]
- 19.Hellsten LA, Nigg C, Norman G, et al. Accumulation of behavioral validation evidence for physical activity stage of change. Health Psychol. 2008;27:S43–53. doi: 10.1037/0278-6133.27.1(Suppl.).S43. [DOI] [PubMed] [Google Scholar]
- 20.Di Noia J, Schinke SP, Prochaska JO, Contento IR. Application of the transtheoretical model to fruit and vegetable consumption among economically disadvantaged African-American adolescents: preliminary findings. Am J Health Promot. 2006;20:342–8. doi: 10.4278/0890-1171-20.5.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma J, Betts NM, Horacek T, Georgiou C, White A, Nitzke S. The importance of decisional balance and self-efficacy in relation to stages of change for fruit and vegetable intakes by young adults. Am J Health Promot. 2002;16:157–66. doi: 10.4278/0890-1171-16.3.157. [DOI] [PubMed] [Google Scholar]
- 22.Marcus BH, Selby VC, Niaura RS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63:60–6. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Self-efficacy: The Exercise of Control. New York, NY: W.H. Freeman and Co; 1997. [Google Scholar]
- 24.Wright JA, Adams WG, Laforge RG. Assessing parental self-efficacy for obesity prevention related behaviors. Int J Behav Nutr Phys Act. 2014;22:53. doi: 10.1186/1479-5868-11-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cullen KW, Baranowski T, Rittenberry L, Cosart C, Hebert D, de Moor C. Child-reported family and peer influences on fruit, juice and vegetable consumption: reliability and validity of measures. Health Educ Res. 2001;16:187–200. doi: 10.1093/her/16.2.187. [DOI] [PubMed] [Google Scholar]
- 26.Sallis JFTW, Dowda M, Freedson PS, Taylor WC, Sirard JR, Trost SG. Correlates of vigorous physical activity for children in grades 1 through 12: Comparing parent-reported and objectively measured physical activity. Ped Exerc Sci. 2002;14:30–44. [Google Scholar]
- 27.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. Int J Behav Nutr Phys Act. 2008;5:45. doi: 10.1186/1479-5868-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borzekowski D, Robinson TN. Viewing the viewers: ten video cases of children’s television viewing behaviors. J Broadcast Electr Media. 2005;43:506–28. [Google Scholar]
- 29.Robinson TNKJ. Ethnic and gender differences in the relationship between television viewing and obesity, physical activity and dietary fat intake. J School Health. 1995;26:91–8. [Google Scholar]
- 30.Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the block kids questionnaire among youth aged 10 to 17 years. J Am Diet Assoc. 2008;108:862–6. doi: 10.1016/j.jada.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 31.Kuczmarski RJ, Ogden CL, Guo SS. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;246:1–190. [PubMed] [Google Scholar]
- 32.Pedhazur EJ, Schmelkin LP. Measurement, design and analysis: An integrative approach. New York, NY: Taylor and Francis; 1991. [Google Scholar]
- 33.Herberich E, Sikorski J, Hothorn T. A robust procedure for comparing multiple means under heteroscedasticity in unbalanced designs. PLoS ONE. 2010;5:e9788. doi: 10.1371/journal.pone.0009788.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical Power Analyses for the Behavioral Sciences. 2. Hillsdale, New Jersey: Hove and London; 1988. [Google Scholar]
- 35.Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc. 2010;110:1501–1510. doi: 10.1016/j.jada.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 36.NICHQ. [Accessed February 12 2013];Obesity Prevention Messages. http://www.nichq.org/areas_of_focus/childhood_obesity_topic.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table. The Stages of Change (SOC)8 and Readiness Measures as Presented on the Parent Survey.