Abstract
Background
Understanding patterns and predictors of engagement could improve the efficacy of Internet interventions.
Purpose
The purpose of the study was to characterize engagement in a multi-component Internet intervention for cancer survivors with distress.
Methods
Data were derived from 296 cancer survivors provided with access to the Internet intervention and included self-report measures and directly-measured engagement with each component of the intervention.
Results
Over 12 weeks, average total engagement was 7.3 h (sd=11.7), and 42% of participants spent >3 h on the website. Participants spent more time using social networking components than structured intervention content. Greater early and total engagement was associated with previous chemotherapy, being female, and being recruited via the Internet. Early engagement was associated with greater fatigue and more social constraints.
Conclusions
For many users, engagement with an Internet intervention was quite high. Reducing attrition and tailoring content to better meet the needs of those who do not engage should be a focus of future efforts.
Keywords: Cancer, Distress, Internet, Recruitment, Randomized controlled trial
Introduction
Internet-based interventions targeting mood [1, 2], health behavior change [3, 4], and adjustment to cancer and other chronic diseases [5, 6] are being tested in a variety of populations. Although such interventions have the potential to reach large groups of individuals, their efficacy remains uncertain for cancer survivors. Some Internet-based interventions for cancer survivors produce positive effects for the sample [7, 8] or for subsets of participants [9], whereas others evidence null or even negative effects [10, 11]. Internet interventions for cancer survivors also vary markedly with respect to intervention design (e.g., selection and recruitment) and treatment elements, such as types of intervention components that are offered, whether the intervention is self-guided, peerfacilitated or professionally-facilitated, or whether the intervention is provided to individuals or groups. It is likely that design features and characteristics of participants influence how participants use a given intervention. The purpose of the current study was to identify both design features and participant characteristics that predicted engagement across time in an Internet-based intervention for cancer-related distress.
Understanding how users engage with Internet-based interventions is likely to be central to improving outcomes [12–14]. Engagement refers to the ways in which participants use an intervention and can be measured in many ways, such as time spent using the intervention, number, length, and quality of messages posted by participants, use of the intervention across time, and use of specific treatment elements. In several cancer-specific Internet interventions, engagement is positively associated with treatment outcomes [7, 9, 15, 16]. Similar relationships have been observed in studies of Internet-based intervention for health behavior change [17, 18]. Understanding engagement is central not only to improving outcomes (i.e., efficacy), but also to improving the likelihood of “real life” adoption (i.e., effectiveness) of innovative online interventions [19]. Whether Internet-based interventions provide an adequate dose of treatment, and how to maximize engagement in these types of interventions, remain open and pressing questions.
Early efforts to measure engagement with Internet-based interventions used general engagement measures, such as number of messages posted [7, 10, 20-24], number of logins [7, 9, 24-26], number of page views [5, 27], and time on the study website [9, 24, 28, 29]. Number of logins is one of the most commonly reported types of engagement across Internet-based interventions for health [30–32]. Among Internet-based interventions specific to cancer, average logins per week has been remarkably stable, ranging from 2.5 logins per week [24] to 2.9 logins per week [9, 25, 26]. Another marker of engagement is whether participants actively contribute, by posting messages or responses, to a study website. In some studies, estimates of average number of active contributions have ranged from 0.7 messages per week across a 12-week intervention [23] to 0.9 messages per week across a 16-week intervention [20, 21]. These estimates of general engagement with Internet-based interventions, though remarkably consistent across studies, suggest relatively low levels of overall engagement and certainly suggest room for improvement.
In general, low levels of engagement are characteristic of many types of Internet-based interventions, not just those for cancer survivors [14, 19]. Engagement also tends to decline substantially over time [33], a phenomenon described by Eysenbach's “Law of Attrition” [19]. In a randomized controlled trial of diabetics [34–36], 70 % of participants logged into the site weekly during the initial 6 weeks of the study, but this number dropped to 47 % of participants during the final 6 weeks of the study. In a randomized controlled trial of an online support group for breast cancer patients, Han et al. [22] reported that 23 % of participants never logged on to the site, and another 32 % of participants logged on to the site but never actively posted to the group. Internet-based interventions are often accessed only once or twice by participants, and only a small proportion of participants use the intervention consistently across the duration of a study [19, 37–40].
Understanding lack of uptake and patterns of attrition over time will inform the development of subsequent trials. Additionally, few studies in the cancer literature have reported detailed measures of engagement, such as attrition curves, or individual-level characteristics that might be associated with engagement in Internet-based interventions. In the only study to date that has evaluated predictors of engagement in Internet-based interventions for cancer, higher engagement with the Comprehensive Health Enhancement and Support Study (CHESS) intervention for women with breast cancer was associated with being Caucasian, younger, living alone, having less social support, having greater need for information, and having lower self-efficacy for obtaining health information [22]. Internet-based interventions in other populations have produced mixed results. In some studies, engagement has been linked with being female [41] or older [41, 42], whereas other studies have shown no associations between key demographic factors and engagement [43]. For cancer survivors, understanding who uses an intervention is an important step towards being able to identify subgroups whose needs are not met by these types of interventions and being able to tailor interventions more effectively to specific subgroups.
There is also a need to understand how users engage with specific components of Internet interventions (e.g., facilitation, group interaction, educational information, discussion board) so that researchers may use this information to increase treatment efficacy. Research reveals that tailoring intervention content [18], personal messaging and feedback [18, 44, 45], self-monitoring [44], facilitation and professional support [44, 45], social networking (e.g., viewing other participants’ profiles, sending messages to participants, peer support; [41, 45]), and receiving updates regarding the intervention [45] are associated with higher participant engagement. However, few studies have tested engagement with specific treatment elements within an intervention. The present study evaluates the extent to which users engage with a variety of distinct treatment elements, such as a community discussion board, professionally-facilitated chat, personal pages, and structured intervention content. While many studies attempt to provide “everything but the kitchen sink” in order to maximize effects, development time and resources could be greatly reduced by focusing Internet interventions on those treatment elements that are actually used by participants.
An advantage of Internet-based interventions is their ability to measure an individual's use of the website and to do so with extraordinary detail. A precise analysis of behavioral engagement is necessary for designing interventions that are clinically efficacious and have potential for real-world adoption. Understanding engagement with the intervention is key to improving effect sizes in subsequent trials and represents a critical first step towards maximizing the impact of Internet-based interventions for cancer survivors. Accordingly, the aims of the present study were (1) to characterize levels of engagement with a social networking intervention for cancer-related distress; (2) to describe engagement with specific treatment components of the intervention; (3) to evaluate patterns of attrition across time; and (4) to identify design, demographic, medical, and psychosocial factors that are associated with engagement.
Methods
Participants
Following human subjects approval, participants were recruited through the Loma Linda University tumor registry, as well as a number of online websites. The online websites included cancer-related forums, Facebook, and cancer-related websites. The websites had members with a range of cancer types. Recruitment took place from July 2009 through June 2012, and approximately two-thirds of the sample was recruited through online efforts. Those individuals recruited through the Loma Linda tumor registry were mailed a letter describing the study, with the option of learning more about the study, as well as opting out of future contact. Potential participants who did not opt out were contacted by phone, provided additional information, and, if interested, screened for eligibility. Through online recruitment efforts, a brief description of the study was posted, along with a link for more information, as well as the option to screen for eligibility.
Eligibility
Participants were required to be at least 18 years of age, have consistent Internet access, be able to read and write in English, and have a minimum score of a 4 on the Distress Thermometer [46, 47].
Procedures
After enrolling in the study, participants completed an online consent form and a baseline questionnaire. Upon completion of this questionnaire, participants were randomized to receive either immediate access to the intervention (treatment condition) or a 12-week wait-list condition (control group; ClinicalTrials.gov #NCT01976949). All those assigned to the treatment condition were informed that the intervention would last 12 weeks, and each participant's progression through the study was clearly indicated on the study homepage. Twelve weeks after completing the baseline questionnaire, participants completed a follow-up questionnaire, which included all items in the baseline questionnaire, aside from demographic and medical characteristics. With participants being randomized upon completion of the baseline questionnaire, new participants joined the group on a rolling basis. With the completion of each questionnaire, participants were given a US $10 Amazon giftcard.
Study Design
This randomized controlled trial was a 12-week distress management intervention (health-space.net) that included multiple components. Each group contained approximately 20–25 people and two facilitators. Facilitators were advanced PhD and PsyD students enrolled in a clinical psychology doctoral program. Facilitators received specific training for leading online support groups and received weekly supervision from two of the investigators (JO, EB), one of whom is a licensed clinical psychologist. Primary components of health-space.net were weekly guidance modules; a live weekly facilitated chat; a discussion board; personal profiles; and webmail (i.e., confidential private messaging with other group members or facilitators via the study website). Weekly guidance modules contained 10 to 12 pages of educational materials and activities for participants, such as quizzes and exercises in which a participant was asked to describe ways in which they were currently engaging with each weekly guidance module. Each week, participants were offered a new guidance module topic, such as self and body image, relationships, self-efficacy, goal setting, and relaxation. Because participants joined the group on a rolling basis, modules were created so that it was not a requirement to have learned the information from a previous week in order to make use of subsequent guidance modules.
In addition to the guidance modules, a 90-min, facilitated weekly chat was offered. During that time, the facilitator reviewed the weekly guidance module and conducted an exercise around that theme, as well as invited current concerns of group members for discussion and problem solving. A goal during this 90-min session was to explore and use emotion as a way to facilitate change. Participants were also encouraged to use the chat room outside of the scheduled weekly chat session.
The discussion board was a way for members to stay connected to the facilitators and other group members and was actively monitored by the group facilitator. Participants and facilitators were invited to post messages to the group at any time to solicit feedback, update other members about their current situation, or follow up on activities that were assigned during the weekly chat session. A webmail feature was also included in health-space.net, where participants had the option to email the entire group or select members. Participants were also encouraged to create a profile in which they could describe themselves and their experience with cancer and upload pictures, as a way of facilitating group cohesion. Participants were discouraged from sharing identifying information (e.g., email address, name) and were encouraged to select a confidential name for their profile. Typical profile names were “cancermom” or “fighter” or a first name. Many, but not all, participants elected to share personal photos on their pages. As supported by research [48, 49], our rationale for encouraging anonymous communication was that it would be easier for participants to engage in distress-relevant self-disclosure and address psychological concerns.
Measures
Demographic and Medical Characteristics
Participants were asked to self-report their age, gender, ethnicity, and cancer type. In addition, participants also reported level of education (in years), annual household income, current employment, marital status, time since diagnosis, cancer stage, days per month activities were restricted due to cancer, and the frequency of Internet use.
Psychosocial Characteristics
Measures of quality of life, psychological well-being, and social support were included in both the baseline and follow-up questionnaire.
Quality of life was measured with the 27-item Functional Assessment of Cancer Therapy (FACT-G), which asks participants to indicate functioning on a 5-point Likert scale to create subscales of social well-being, psychological well-being, functional well-being, and an overall quality of life score [50]. This instrument has adequate internal consistency (overall α=0.90, subscale α's=0.63–0.86) and good concurrent validity [51]. In addition to the FACT-G, the EuroQol-5D Quality of Well-Being Scale was used to measure overall selfrated health [52] by rating their health on a scale of 0–100, with 0 representing “least desirable state of health you can imagine” and 100 being “perfect health.” This measure has good test-retest reliability, concurrent validity, and sensitivity to change [53].
Measures of distress, trauma symptoms, and mood were used to assess psychological well-being. The Distress Thermometer [47] asks participants to rate their level of distress on a 0–10 scale, with higher numbers indicating more distress. A cut-off score of 4 or higher has been demonstrated to provide the optimal balance between sensitivity and specificity for identifying significant clinical concerns in those with cancer [46, 54]. In order to measure trauma symptoms, the Impact of Events Scale-Revised (IES-R) was used. The IES-R is a 22-item, Likert-type scale that measures intrusive and avoidant symptoms of cancer-related thoughts and stimuli [55]. This scale is sensitive to the effects of psychosocial intervention and has good internal consistency (Cronbachs α=0.79–0.92; [56]). Total mood disturbance was measured with the Profile of Mood States (POMS-SF; [57]). The POMS-SF requires participants to identify, on a 5-point Likert scale, the extent to which they have experienced each of 37 distinct mood states in the previous week, ranging from “not at all” to “extremely.” The total mood disturbance score (α=0.91) was used in this study, as was the 5-item fatigue subscale (α=0.90; [57]). Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D; [58]), which is a 20-item measure that asks respondents to indicate how often they have experienced symptoms of depression within the past week, on a 4-point Likert scale, ranging from “rarely or none of the time” to “most or all of the time.” The CES-D is reliable and has been validated within cancer populations [57, 59].
The Yale Social Support Index [60] was used to measure positive and negative experiences of emotional support [61]. Respondents rated the amount and quality of emotional support they have received from family and friends (α=0.73). Social support needs that were unmet were measured using the Social Constraints Scale [62]. This 15-item measure asks respondents to rate the extent to which a significant other or close friend has been receptive to their expression of feelings and concerns about their cancer experience. This measure has excellent reliability (α=0.88) for cancer survivors and good test-retest reliability and validity [63].
Measures of Behavioral Engagement
Engagement was measured objectively via server-side scripting that provided time spent using the intervention, time spent using specific parts of the intervention, and active posting of content to the study website. Consistent with previous literature [64], exposures to specific pages that lasted longer than 30 min were assumed to be periods of inactivity and were not included in totals of time spent using the intervention, and time data were verified against the period of time during which the chat component of the intervention would have been available to participants who participated in the chat sessions. In addition to measuring exposure in time, we also measured engagement associated with actively contributing content to the social networking intervention (i.e., active engagement). For each week of the intervention, participants were considered to be actively engaged if they spent more than 60 seconds in the facilitated chat, posted an original message or reply message to the discussion board, created a blog of more than 10 words, or composed a mail message of more than 10 words.
Statistical Analysis
To address aims 1 and 2, average engagement, measured in minutes, was calculated for overall use of the study website and use of each specific component of the study website. To further characterize findings associated with engagement, clinical cut-points were used to identify three distinct engagement groups: those who spent fewer than 10 min using the study website (Non-Engaged), those who spent more than 10 min but fewer than 3 h (Low-Engaged), and those who spent more than 3 h (Moderately/Highly Engaged) Cut-points were derived based on a minimum exposure to ensure familiarity with the contents of the intervention (10 min) and a minimum anticipated beneficial dose (3 h across 12 weeks; [65]). Overall use and use of specific components were calculated separately for each of the three engagement groups and tested for between-group differences using ANOVA models. ANOVA and chi-square models were also employed to evaluate differences between engagement groups with respect to key demographic and medical characteristics. In order to evaluate attrition across time for aim 3, active engagement (i.e., actively posting content to the study website) was assessed for each week of the 12-week intervention. For any given week, participants were characterized as being active (i.e., posted content to the study website) or inactive. Repeated measures ANOVA was used to test the effect of time and the time x engagement group interaction on active engagement across the 12-weeks of intervention. To address aim 4, we tested univariate associations between design, demographic, medical, and psychosocial characteristics and overall engagement (i.e., total time) with the study website. Characteristics identified as univariate predictors of engagement were then included in a multivariate regression model predicting total engagement. Predictors of early (week 1) and late (weeks 9–12) active engagement with the intervention (i.e., demographic, design, medical, and psychosocial characteristics) were standardized and tested using logistic regression models. Significant univariate predictors were then entered simultaneously in a multivariate logistic regression model predicting either early or late active engagement with the intervention.
Results
Characteristics of the Sample
The full sample consisted of 296 cancer survivors (see Table 1), who were primarily middle-aged (x̄=54 years, sd= 10.8, range=29–88), female (78 %), and White (87 %). With respect to cancer type, the sample appeared to overrepresent women with breast cancer relative to the US Surveillance Epidemiology and End Results Data (SEER, 2009), but provided a reasonable approximation of other cancer types. Nearly 25 % (n=73) of the sample reported having regional or distant metastases, suggesting advanced disease, whereas 58.1 % (n=172) reported confined, early stages of disease, and 17.2 % (n=51) reported early disease with some evidence of limited spread (e.g., involved lymph nodes).
Table 1. Demographic and medical characteristics of participants, by engagement group.
| Non-engaged users (n=59) | Low-engaged users (n=113) | Moderate-highly engaged users (n=124) | All users combined (n=296) | Between-group differences | |
|---|---|---|---|---|---|
| Age, x̄years (SD) | 56.1 (10.8) | 53.0 (11.9) | 53.5 (9.8) | 53.8 (10.8) | ns |
| Sex, n (%) | |||||
| Female | 46 (78.0 %) | 81 (71.7 %) | 103 (83.1 %) | 230 (77.7 %) | ns |
| Male | 13 (22.0 %) | 32 (28.3 %) | 21 (16.9 %) | 66 (22.3 %) | |
| Ethnicity, n (%) | |||||
| White (%) | 54 (91.5 %) | 101 (89.4 %) | 103 (83.1 %) | 258 (87.2 %) | ns |
| Latino (%) | 2 (3.4 %) | 5 (4.4 %) | 7 (5.6 %) | 14 (4.7 %) | |
| African-American (%) | 1 (1.7 %) | 4 (3.5 %) | 6 (4.8 %) | 11 (3.7 %) | |
| Other (%) | 2 (3.4 %) | 3 (2.7 %) | 8 (6.5 %) | 13 (4.4 %) | |
| Education, years (SD) | 15.4 (3.3) | 15.6 (2.5) | 16.0 (2.7) | 15.7 (2.7) | ns |
| Annual household income, dollars/year (SD) | 95,500 (120,884) | 92,400 (81,940) | 93,000 (94,240) | 93,270 (95,670) | ns |
| Cancer type, n (%) | ns | ||||
| Breast | 28 (47.5 %) | 47 (41.6 %) | 59 (47.6 %) | 134 (45.3 %) | |
| Prostate | 7 (11.9 %) | 20 (17.7 %) | 14 (11.3 %) | 41 (13.9 %) | |
| Colorectal | 4 (6.8 %) | 4 (3.5 %) | 4 (3.2 %) | 12 (4.1 %) | |
| Female reproductive | 2 (3.4 %) | 6 (5.3 %) | 10 (8.1 %) | 18 (6.1 %) | |
| Hematologic | 1 (1.7 %) | 6 (5.3 %) | 3 (2.4 %) | 10 (3.4 %) | |
| Urinary | 1 (1.7 %) | 0 (0 %) | 0 (0 %) | 1 (0.3 %) | |
| Melanoma | 1 (1.7 %) | 2 (1.8 %) | 4 (3.2 %) | 7 (2.4 %) | |
| Lung | 1 (1.7 %) | 0 (0 %) | 1 (0.8 %) | 2 (0.7 %) | |
| Other | 9 (15.3 %) | 22 (19.5 %) | 19 (15.3 %) | 50 (16.9 %) | |
| Multiple cancers | 5 (8.5 %) | 6 (5.3 %) | 10 (8.1 %) | 21 (7.1 %) | |
| Cancer spread | |||||
| No spread (%) | 30 (50.8 %) | 71 (62.8 %) | 71 (57.3 %) | 172 (58.1 %) | ns |
| Spread to lymph tissue (%) | 10 (16.9 %) | 22 (19.5 %) | 19 (15.3 %) | 51 (17.2 %) | |
| Regional metastasis (%) | 7 (11.9 %) | 8 (7.1 %) | 15 (12.1 %) | 30 (10.1 %) | |
| Distant metastasis (%) | 12 (20.3 %) | 12 (10.6 %) | 19 (15.3 %) | 43 (14.5 %) | |
ns=not significant
Engagement with the Intervention
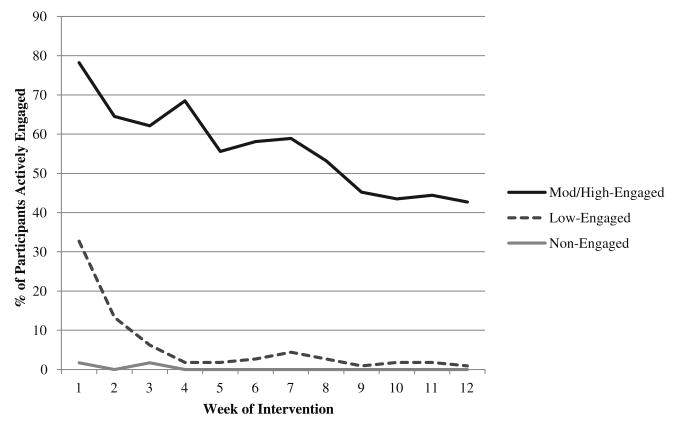
Average duration of engagement with the study website over the course of the 12-week intervention was 7.3 h (sd=11.7), equivalent to 2.4 h per month. Nearly 20 % (n=59) were characterized as Non-Engaged, 38.2 % (n=113) as Low-Engaged, and 41.9 % (n=124) as Moderately-to-Highly Engaged (see Table 1). Total time spent using the healthspace.net intervention averaged 3.1 min in the Non-Engaged group, 58.8 min in the Low-Engaged group, and 991 min in the Moderately to Highly Engaged group (see Table 2). Participants averaged 277 min using the social networking components of the website, compared with 122 min for the structured intervention components. Time spent using each feature of the intervention is shown in Table 2. With respect to use of the intervention website across time, 55.7 % (n=146) actively engaged during the first month of the intervention. By month 2, 37.2 % (n=110) participants were actively engaged with the intervention website, and 30.1% (n=89) were actively engaged during month 3. There was a significant linear decline in active engagement across time, F (11, 8.6)=13.2, p<0.001. There was also a significant time X engagement group interaction, F (22, 17.2)=4.3, p<0.001, suggesting that the rates of decline in active engagement differed considerably across engagement groups (see Fig. 1). Non-engaged participants hardly engaged with the website at all, even at the beginning of the intervention. However, most moderate-highly engaged participants (78.2 %) were actively engaged within the first week of the intervention, and engagement rates declined at a relatively slow and stable rate across the 12-week intervention, culminating at 42.7 % (see Fig. 1). Across all participants, 25.7 % (n=76) were actively engaged in the intervention during each and every week of the 12-week intervention.
Table 2. Mean engagement with key components of the intervention by engagement group, in minutes.
| Non-engaged users (n=59) | Low-engaged users (n=113) | Moderate-highly engaged users (n=124) | All users combined (n=296) | Between-group differences | |
|---|---|---|---|---|---|
| Social networking components | |||||
| Discussion board | 2.2 (2) | 29.8 (28) | 312.9 (300) | 142.9 (243) | *** |
| Personal pages | 0.5 (1) | 17.6 (20) | 300.0 (303) | 132.4 (243) | *** |
| Webmail | 0 (0) | 0.1 (0.6) | 4.1 (9.1) | 1.8 (6.2) | *** |
| Structured intervention components | |||||
| Guidance modules | 0.3 (1) | 8.3 (14) | 96.0 (82) | 43.4 (70) | *** |
| Facilitated chat | 0.1 (0.4) | 2.9 (12) | 278 (305) | 117.7 (240) | *** |
| Total time using intervention | 3.1 (3) | 58.8 (45) | 991.0 (808) | 438.2 (703) | *** |
Standard deviations appear in parentheses
p<0.001
Fig. 1.
Proportion of participants engaged in active use of the intervention website across the 12-week duration of the study. Note. Active engagement defined as >60 s in the facilitated chat, posting an original message or reply message to the discussion board, creating a blog of more than 10 words, or writing a mail message of more than 10 words
Design and Demographic Predictors of Total Engagement Time
Total time spent using the intervention website was not associated with randomization condition (i.e., treatment vs. waitlist). Engagement time was associated with recruitment source, t (274.1)=2.59, p=0.01, with significantly higher use among those recruited from the Internet (x̄=507 min) relative to those recruited from the cancer registry (x̄= 309 min). In subsequent analyses, recruitment source was considered as a covariate. In unadjusted models, engagement time was not associated with age, education, income, ethnicity, or marital status. Sex was significantly associated with engagement time, t (194.8)=3.81, p<0.001, with females spending x̄=499 (756)min engaged with the intervention compared with x̄=226 (419)min in males, but this difference was no longer significant after adjustment for recruitment source. Engagement time was not associated with frequency of Internet use, previous use of support groups, or previous use of online support groups.
Medical, Psychosocial, and Multivariate Predictors of Total Engagement Time
With respect to medical characteristics, engagement time was not associated with degree of tumor spread, clinical stage, previous surgery, previous radiation treatment, functional impairments due to cancer, or other health-related conditions. Engagement time was associated with having undergone chemotherapy, t (277.0)=2.55, p=0.01, and remained significant in a covariate-adjusted model, F (1, 293)=3.9, p=0.05. Participants who had previously received chemotherapy exhibited significantly higher engagement time, x̄=546 min (sd=759), than those who had not, x̄=388 min (sd=633). Additionally, cancer type was associated with engagement time, F (6, 289)=2.76, p=0.01 and remained significant after adjustment for date of entry and recruitment source, F (6, 288) =2.89, p=0.006. Relative to the grand mean (x̄=438), engagement time was significantly higher among those with a female reproductive cancer, x̄=735 min (sd=889), and those with multiple cancers, x̄=815 min (sd=1,344).
None of the psychosocial predictors were significantly associated with engagement. Engagement time was not associated with perceived social support, social constraints, or emotional suppression. Similarly, engagement time was not associated with depressive symptoms, cancerrelated trauma symptoms, or fatigue. A combined multivariate model, consisting of each univariate predictor of engagement time (recruitment source, gender, previous chemotherapy treatment, and cancer type) significantly predicted engagement time, F (9, 286)=3.1, p=0.001, but explained only a small proportion of variability, R2=0.09. In the multivariate model, cancer type was the strongest overall predictor of engagement, F (6, 286)=2.7, p=0.01, ΔR2=0.05.
Predictors of Early (Week 1) Active Engagement with the Intervention
Given the high rates of attrition among Non-Engaged and Low-Engaged participants between weeks 1 and 2, post hoc tests were used to compare those who actively used the intervention in week 1 with those who did not use the intervention in week 1. One hundred thirty-five participants (45.6 %) actively engaged in the intervention during the first week of access to the study website. These “Early Users” were compared with the 161 participants (54.4 %) who did not make early use of the study website on previously tested design, demographic, medical, and psychosocial characteristics (see Table 3).
Table 3. Predictors of early and late use of the study website among all participants (n=296).
| Early use of the study website among all participants (week 1) |
Late use of the study website among all participants (weeks 9–12) |
|||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Odds ratio | (95 % CI) | p value | Odds ratio | (95 % CI) | p value | |
| Design characteristics | ||||||
| Immediate treatment vs wait-list control | 2.50 | (1.5–4.0) | *** | 1.32 | (0.8–2.2) | ns |
| Recruitment source (web vs registry recruitment) | 1.4 | (0.9–2.3) | ns | 1.8 | (1.0–3.1) | * |
| Demographic characteristics | ||||||
| Age | 0.92 | (0.7–1.2) | ns | 1.1 | (0.9–1.4) | ns |
| Education | 1.24 | (1.0–1.6) | ns | 1.2 | (0.9–1.5) | ns |
| Income | 1.13 | (0.3–1.1) | ns | 1.0 | (0.8–1.3) | ns |
| Gender (female vs male) | 1.63 | (0.9–2.9) | ns | 2.6 | (1.3–5.2) | ** |
| Medical characteristics | ||||||
| Chemotherapy | 2.02 | (1.3–3.2) | ** | 1.8 | (1.1–3.0) | * |
| Surgery | 1.00 | (0.6–1.7) | ns | 1.6 | (0.7–2.1) | ns |
| Radiation | 0.95 | (0.6–1.5) | ns | 0.9 | (0.5–1.5) | ns |
| Psychosocial characteristics | ||||||
| Depression | 1.11 | (0.9–1.4) | ns | 0.9 | (0.7–1.2) | ns |
| Anxiety | 1.19 | (0.9–1.5) | ns | 1.0 | (0.7–1.2) | ns |
| Fatigue | 1.39 | (1.1–1.8) | ** | 1.1 | (0.8–1.4) | ns |
| Social support | 1.04 | (0.8–1.3) | ns | 1.2 | (0.9–1.5) | ns |
| Social constraints | 1.28 | (1.0–1.6) | * | 1.00 | (0.8–1.3) | ns |
ns=not significant
p<0.05;
p<0.01;
p<0.001
Being an Early User was not associated with recruitment source, age, education, income, ethnicity, marital status, gender, frequency of Internet use, tumor spread, previous surgery or radiation, or cancer type. With respect to psychosocial variables, early use of the intervention was not associated with depression, anxiety, or social support. Early Use was significantly associated with being randomized to the immediate treatment group, OR=2.50 (95 % CI=1.5–4.0), p<0.001; having previously undergone chemotherapy treatment, OR= 2.02 (95 % CI=1.3–3.2), p=0.003; having higher levels of fatigue, OR=1.40 (95 % CI=1.1–1.8), p=0.006; and having higher social constraints, OR=1.28 (95 % CI=1.0–1.6), p= 0.04. A combined multivariate model consisting of randomization group, previous chemotherapy, fatigue, and social constraints was significant, χ2(4)=27.0, p<0.001, but resulted in a small 8.4 % improvement in classification over the null model.
Predictors of Late (Weeks 9–12) Active Engagement with the Intervention
Next, we sought to identify attributes of users who persisted in using the intervention across time (n=89; 30.1 % of the full sample). Persistent users were defined as those who were actively engaged with the intervention during the final 4 weeks of the 12-week trial. As shown in Table 3, persistent users were more likely to be female, OR=2.6 (95 % CI=1.3–5.2), p=0.009; to have undergone chemotherapy, OR=1.8 (95 % CI =1.1–3.0), p=0.02; and to have been recruited via the Internet, OR=1.8 (95 % CI=1.0–3.1), p=0.04. No other characteristics were associated with persistent active engagement with the intervention. A multivariate model consisting of Internet recruitment, gender, and previous chemotherapy was significant, χ2(3)=10.3, p=0.02, but resulted in no improvement in classification over the null model.
Discussion
On average, participants spent a considerable amount of time using the study website (144 min/month), a rate that appears to be superior to a number of other prominent (and considerably better funded) social networking sites, including Pinterest (89 min/month), Twitter (21 min/month), LinkedIn (17 min/month), MySpace (8 min/month), and Google+ (3 min/month; [66, 67]). Sites such as Facebook command very high rates of participation (405 min/month; [67]), but our intervention was successful by social networking standards and could be improved with additional testing. With respect to clinical standards, only 42 % of participants used the study website at a level that we anticipated might be necessary for observing changes in distress and other outcomes (i.e., 60 min/month). However, engagement levels were consistent with levels reported by other group-based Internet interventions for cancer survivors, such as Webchoice (138 min/month; [28]).
Understanding how to better meet the needs of the 58 % who reported high levels of cancer-related distress, yet made little use of the intervention, is an important next step. Distress is clearly multi-factorial, manifested by emotional concerns for many, but also by physical problems, disruptions to family and other social relationships, and practical concerns [68, 69]. Although the health-space intervention was designed to provide some assistance with each of these types of concerns, greater specificity to each participants’ particular type of distress may be needed. Future interventions of this type need to address three key shortcomings of the present study. First, additional efforts to refine social networking strategies and large sample sizes would be useful for helping participants connect with specific others who share similar concerns (e.g., individuals with the same cancer type, treatment trajectory, and distress-related concerns). Second, specific coping-skills intervention materials need to be tailored to participants’ specific concerns (e.g., emotional problems, physical symptoms), as determined either by responses to self-report measures or participant preferences related to delivery of the intervention [70]. Third, the first week of the intervention is a particularly critical and sensitive period for connecting participants with an Internet intervention. In order to promote early adoption, additional efforts to understand how effectively to time the delivery of tailored social networking and intervention elements are needed.
When given free access to all parts of the intervention website, participants spent the majority of their time using the social networking features. Although social networking engagement was significantly associated with engagement with the structured intervention components (i.e., guidance exercises and facilitated chat), using social networking features may have interfered with participants’ use of the structured intervention components. Engagement with the structured intervention components was considerably lower than that for social networking, and the one structured component that was predominately used (facilitated chat) provided both guidance exercises and social networking with other survivors and facilitators. It is our belief that social networking and strong professional facilitation in particular, has the potential to enhance participation rates and levels of engagement, but this hypothesis has not yet formally been tested, and understanding the role and importance of social networking is still an open question.
Three specific factors were linked with greater engagement with the intervention: being recruited via the Internet, having previously undergone chemotherapy, and having female reproductive or multiple cancers. Those recruited from the Internet may have been more comfortable being online and spending time with an Internet-based intervention, may have self-selected based on interest and suitability for the intervention, and may have been more motivated to participate [71]. Those who had certain cancer types or had undergone chemotherapy may have shared other unmeasured characteristics, such as concerns related to mortality, dealing with side effects or physical concerns, active efforts to manage symptoms, or greater sense of personal identification with a cancer survivor role. Indeed, early adoption of the intervention was linked specifically with both previous chemotherapy and the presence of fatigue. Early adopters also reported feeling more constrained by their social environment in talking about their cancer-related feelings than did non-adopters. These findings suggest a pattern of “fit” between the intervention and participants’ goals for using the intervention. The health-space.net intervention was designed to provide social connections for survivors and to address symptom-related concerns. The intervention was also intended to address emotion-related concerns. Although engagement was not predicted by levels of emotional functioning, all participants met an eligibility criterion for cancer-related distress.
There were several limitations of the present study. First, results of this study are specific to a professionally-facilitated, coping skills-training, mixed diagnosis, social networking intervention. Internet-based interventions for cancer survivors are quite heterogenous with respect to whether they are self-guided or professionally-facilitated, whether they are specific to breast or other cancers, whether they provide structured intervention content (e.g., guidance exercises), whether they target only those with distress or other specific problems (e.g., fatigue), and whether they are individual, group-based, and/or provide social networks. Additional research is needed to evaluate engagement and outcomes associated with each of these types of intervention modalities. Second, our sample was somewhat better educated, wealthier, and disproportionately represented by women with breast cancer than the general population of cancer survivors, and it is unclear whether this is due to sampling bias or because these are subgroups most likely to use and benefit from these types of interventions. We have previously suggested improvements to Internet-based recruitment that could improve generalizability of Internet-based interventions to the population of cancer survivors in the USA, including the use of stratified sampling designs and supplemental registry-based recruitment strategies [71]. Third, it is worth noting that it is impossible to perfectly measure time spent using a website. We attempted to estimate time spent engaged with the intervention conservatively, but no standards currently exist for capturing time-stamp data in behavioral Internet interventions. Finally, our models accounted for 9 % of the variability in engagement, suggesting that additional important predictors of engagement exist. Such predictors might include expectations and attitudes about privacy or social disclosure related to cancer, quantity and quality of interactions with facilitators and other participants, expectations about the intervention, perceived and actual usability of the study website, or degree of fit between the intervention and the participant.
This study provides one of the most detailed reports characterizing engagement with an Internet-based intervention for cancer survivors. Given the relatively short period of time over which Internet-based interventions have been developed and tested, the results of this study demonstrate that these types of interventions are feasible and can provide substantial treatment doses to at least 42 % of those with cancer-related distress. Analysis of engagement patterns provides a valuable opportunity for better understanding and mitigating poor engagement or declines in participation across time. Intervention researchers may need to better anticipate and accommodate expected declines in participation across time, for example by delivering the most effective intervention components earlier in treatment, employing more sophisticated systems for monitoring participant engagement, or identifying and potentially addressing participants’ concerns and expectations for the intervention as early as possible. Future studies will need to decompose the effects of primary intervention modalities (e.g., individual vs group, social networks vs without, facilitated vs non-facilitated) on both engagement measures and outcomes. Detailed, objective measures of engagement provide a necessary foundation for identifying and testing ways to improve both engagement and outcomes of this new generation of interventions for those living with cancer.
Footnotes
Conflicts of Interest: Jason Owen, Annette Stanton, Amanda Gorlick, and Erin Bantum declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Contributor Information
Jason E. Owen, Email: jason.owen@va.gov, Department of Psychology, Loma Linda University, Loma Linda, CA, USA; Veterans Affairs Palo Alto Health Care System, National Center for PTSD, Menlo Park, CA, USA.
Erin O. Bantum, University of Hawai’i Cancer Center, Cancer Prevention and Control Program, University of Hawai’i at Manoa, Honolulu, HI, USA.
Amanda Gorlick, Department of Psychology, Loma Linda University, Loma Linda, CA, USA.
Annette L. Stanton, Departments of Psychology and Psychiatry/Biobehavioral Sciences, University of California, Los Angeles, CA, USA.
References
- 1.Andersson G, Bergström J, Hollandare F, et al. Internet-based selfhelp for depression: Randomised controlled trial. Br J Psychiatry. 2005;187:456–461. doi: 10.1192/bjp.187.5.456. [DOI] [PubMed] [Google Scholar]
- 2.Mohr DC, Duffecy J, Jin L, et al. Multimodal e-mental health treatment for depression: A feasibility trial. J Med Internet Res. 2010;12:e48. doi: 10.2196/jmir.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leykin Y, Aguilera A, Torres LD, et al. Interpreting the outcomes of automated internet-based randomized trials: Example of an International Smoking Cessation Study. J Med Internet Res. 2012;14:e5. doi: 10.2196/jmir.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wangberg SC, Nilsen O, Antypas K, et al. Effect of tailoring in an Internet-based intervention for smoking cessation: Randomized controlled trial. J Med Internet Res. 2011;13:e121. doi: 10.2196/jmir.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schover LR, Yuan Y, Sui D, et al. A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer. 2011;118:500–509. doi: 10.1002/cncr.26308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawkins RP, Pingree S, Shaw B, et al. Mediating processes of two communication interventions for breast cancer patients. Patient Educ Couns. 2010;81:S48–S53. doi: 10.1016/j.pec.2010.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winzelberg AJ, Classen C, Alpers GW, et al. Evaluation of an internet support group for women with primary breast cancer. Cancer. 2003;97:1164–1173. doi: 10.1002/cncr.11174. [DOI] [PubMed] [Google Scholar]
- 8.McTavish FM, Gustafson DH, Owens BH, et al. CHESS: An interactive computer system for women with breast cancer piloted with an underserved population. J Ambul Care Manag. 1995;18:35–41. doi: 10.1097/00004479-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Owen JE, Klapow JC, Roth DL, et al. Randomized pilot of a selfguided internet coping group for women with early-stage breast cancer. Ann Behav Med. 2005;30:54–64. doi: 10.1207/s15324796abm3001_7. [DOI] [PubMed] [Google Scholar]
- 10.Hoybe MT, Dalton SO, Deltour I, et al. Effect of Internet peer-support groups on psychosocial adjustment to cancer: A randomised study. Br J Cancer. 2010;102:1348–1354. doi: 10.1038/sj.bjc.6605646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salzer MS, Palmer SC, Kaplan K, et al. A randomized, controlled study of Internet peer-to-peer interactions among women newly diagnosed with breast cancer. Psycho-Oncology. 2009;19:441–446. doi: 10.1002/pon.1586. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Executive Summary National Cancer Control Programmes: Policies and managerial guidelines. 2nd. Geneva: World Health Organization; 2002. p. XII. [Google Scholar]
- 13.Ritterband LM, Thorndike FP, Cox DJ, et al. A behavior change model for internet interventions. Ann Behav Med. 2009;38:18–27. doi: 10.1007/s12160-009-9133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Danaher BG, Seeley JR. Methodological issues in research on webbased behavioral interventions. Ann Behav Med. 2009;38:28–39. doi: 10.1007/s12160-009-9129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw B, Han JY, Hawkins RP, et al. Doctor-patient relationship as motivation and outcome: Examining uses of an interactive cancer communication system. Int J Med Inform. 2007;76:274–82. doi: 10.1016/j.ijmedinf.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Wise M, Han J, Shaw B, et al. Effects of using online narrative and didactic information on healthcare participation for breast cancer patients. Patient Educ Couns. 2008;70:348–356. doi: 10.1016/j.pec.2007.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danaher BG, Smolkowski K, Seeley JR, et al. Mediators of a successful web-based smokeless tobacco cessation program. Addiction. 2008;103:1706–1712. doi: 10.1111/j.1360-0443.2008.02295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strecher VJ, McClure J, Alexander G, et al. The role of engagement in a tailored web-based smoking cessation program: Randomized controlled trial. J Med Internet Res. 2008;10:e36. doi: 10.2196/jmir.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eysenbach G. The law of attrition. J Med Internet Res. 2005;7:e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han JY, Shah DV, Kim E, et al. Empathic exchanges in online cancer support groups: Distinguishing message expression and reception effects. Health Commun. 2011;26:185–197. doi: 10.1080/10410236.2010.544283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim E, Han JY, Moon TJ, et al. The process and effect of supportive message expression and reception in online breast cancer support groups. Psycho-Oncology. 2012;21:531–40. doi: 10.1002/pon.1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han JY, Kim JH, Yoon HJ, et al. Social and psychological determinants of levels of engagement with an online breast cancer support group: Posters, lurkers, and nonusers. J Health Commun. 2012;17:356–371. doi: 10.1080/10810730.2011.585696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Classen CC, Chivers ML, Urowitz S, et al. Psychosexual distress in women with gynecologic cancer: A feasibility study of an online support group. Psycho-Oncology. 2012;22:930–35. doi: 10.1002/pon.3058. [DOI] [PubMed] [Google Scholar]
- 24.Vilhauer RP, McClintock MK, Matthews AK. Online support groups for women with metastatic breast cancer: A feasibility pilot study. J Psychosoc Oncol. 2010;28:560–586. doi: 10.1080/07347332.2010.504504. [DOI] [PubMed] [Google Scholar]
- 25.Duffecy J, Sanford S, Wagner L, et al. Project onward: An innovative e-health intervention for cancer survivors. Psycho-Oncology. 2012;22:947–51. doi: 10.1002/pon.3075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.David N, Schlenker P, Prudlo U, et al. Internet-based program for coping with cancer: A randomized controlled trial with hematologic cancer patients. Psycho-Oncology. 2012;22:1064–72. doi: 10.1002/pon.3104. [DOI] [PubMed] [Google Scholar]
- 27.Kazer MW, Bailey DE, Sanda M, et al. An Internet intervention for management of uncertainty during active surveillance for prostate cancer. Oncol Nurs Forum. 2011;38:561–568. doi: 10.1188/11.ONF.561-568. [DOI] [PubMed] [Google Scholar]
- 28.Ruland CM, Jeneson A, Andersen T, et al. Designing tailored Internet support to assist cancer patients in illness management. AMIA Proceedings. 2007:635–639. [PMC free article] [PubMed] [Google Scholar]
- 29.Gustafson DH, Hawkins R, Pingree S, et al. Effect of computer support on younger women with breast cancer. J Gen Intern Med. 2001;16:435–445. doi: 10.1046/j.1525-1497.2001.016007435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Couper MP, Alexander GL, Zhang N, et al. Engagement and retention: Measuring breadth and depth of participant use in an online intervention. J Med Int Res. 2010;4:e52. doi: 10.2196/jmir.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McClure JB, Shortreed SM, Bogart A, et al. The effect of program design on engagement with an internet-based smoking intervention: Randomized factorial trial. J Med Int Res. 2013;3:e69. doi: 10.2196/jmir.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Donkin L, Christensen H, Naismith SL, et al. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011;3:e52. doi: 10.2196/jmir.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Couper MP, Alexander GL, Zhang N, et al. Engagement and retention: Measuring breadth and depth of participant use of an online intervention. J Med Internet Res. 2010;12:e52. doi: 10.2196/jmir.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glasgow RE, Kutz D, King D, et al. Outcomes of minimal and moderate support versions of an Internet-based diabetes selfmanagement support program. J Gen Intern Med. 2010;25:1315–22. doi: 10.1007/s11606-010-1480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glasgow RE, Christiansen SM, Kurz D, et al. Engagement in a diabetes self-management website: Usage patterns and generalizabil-ity of program use. J Med Internet Res. 2011;13:e9. doi: 10.2196/jmir.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glasgow RE, Kurz D, King D, et al. Twelve-month outcomes of an internet-based diabetes self-management support program. Patient Educ Couns. 2012;87:81–92. doi: 10.1016/j.pec.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wangberg SC, Bergmo TS, Johnsen JAK. Adherence in Internet-based interventions. Patient Prefer Adherence. 2008;2:57–65. [PMC free article] [PubMed] [Google Scholar]
- 38.Strecher V, Shiffman S, West R. Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction. 2005;100:682–688. doi: 10.1111/j.1360-0443.2005.01093.x. [DOI] [PubMed] [Google Scholar]
- 39.Glasgow RE, Nelson CC, Kearney KA, et al. Reach, engagement, and retention in an Internet-based weight loss program in a multi-site randomized controlled trial. J Med Internet Res. 2007;9:e11. doi: 10.2196/jmir.9.2.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ybarra ML, Eaton WW. Internet-based mental health interventions. Ment Health Serv Res. 2005;7:75–87. doi: 10.1007/s11020-005-3779-8. [DOI] [PubMed] [Google Scholar]
- 41.Murray E, White IR, Varagunam M, et al. Attrition revisited: Adherence and retention in a web-based alcohol trial. J Med Internet Res. 2013;15:e162. doi: 10.2196/jmir.2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davies C, Corry K, Van Itallie A, et al. Prospective associations between intervention components and website engagement in a publicly available physical activity website: The case of 10,000 Steps Australia. J Med Internet Res. 2012;14:e4. doi: 10.2196/jmir.1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Glasgow RE, Christiansen SM, Kurz D, et al. Engagement in a diabetes self-management website: Usage patterns and generalizability of program use. J Med Internet Res. 2011;13:e9. doi: 10.2196/jmir.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schubart JR, Stuckey HL, Ganeshamoorthy A, et al. Chronic health conditions and internet behavioral interventions: A review of factors to enhance user engagement. Comput Inform Nurs. 2011;29:81–92. doi: 10.1097/NCN.0b013e3182065eed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brouwer W, Kroeze W, Crutzen R, et al. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J Med Internet Res. 2011;13:e2. doi: 10.2196/jmir.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494–1502. doi: 10.1002/cncr.20940. [DOI] [PubMed] [Google Scholar]
- 47.Roth AJ, Kornblith AB, Batel-Copel L, et al. Rapid screening for psychological distress in men with prostate carcinoma: A pilot study. Cancer. 1998;82:1907–1908. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 48.Joinson AN. Self-disclosure in computer-mediated communication: The role of self-awareness and visual anonymity. Eur J Soc Psychol. 2001;31:177–192. [Google Scholar]
- 49.Tidwell LC, Walther JB. Computer-mediated communication effects on disclosure, impressions, and interpersonal evaluations: Getting to know one another a bit at a time. Hum Comm Res. 2002;28:317–48. [Google Scholar]
- 50.Cella D. F A C I T Manual. Chicago, IL: Center on outcomes, research, and education, Evanston Northwestern Healthcare and Northwestern University; 1997. [Google Scholar]
- 51.Brady MJ, Cella DF, Mo F, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15:974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- 52.Brooks R. EuroQuol: The current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 53.Llach XB, Herdman M, Schiaffino A. Determining correspondence between scores on the EQ-5D “Thermometer” and a 5-point categorical rating scale. Med Care. 1999;37:671–677. doi: 10.1097/00005650-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 54.Ransom S, Jacobsen PB, Booth-Jones M. Validation of the Distress Thermometer with bone marrow transplant patients. Psycho-Oncology. 2006;15:604–612. doi: 10.1002/pon.993. [DOI] [PubMed] [Google Scholar]
- 55.Weiss D, Marmar C. The impact of event scale- revised. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. New York: Guildford; 1997. [Google Scholar]
- 56.Edgar L, Rosberger Z, Nowlis D. Coping with cancer during the first year after diagnosis. Cancer. 1992;69:817–828. doi: 10.1002/1097-0142(19920201)69:3<817::aid-cncr2820690334>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 57.Baker F, Denniston M, Zabora J, et al. POMS short form for cancer patients: Psychometric and structural evaluation. Psycho-Oncology. 2002;11:273–81. doi: 10.1002/pon.564. [DOI] [PubMed] [Google Scholar]
- 58.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;3:385–401. [Google Scholar]
- 59.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) J Psychosom Res. 1999;46:437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 60.Seeman TE, Berkman LF. Structural characteristics of social networks and their relationship with social support in the elderly: Who provides support. Soc Sci Med. 1988;26:737–49. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]
- 61.Butler LD, Koopman C, Classen C, et al. Traumatic stress, life events, and emotional support in women with metastatic breast cancer: Cancer-related traumatic stress symptoms associated with past and current stressors. Health Psychol. 1999;18:555–60. doi: 10.1037//0278-6133.18.6.555. [DOI] [PubMed] [Google Scholar]
- 62.Lepore SJ. A social-cognitive processing model of emotional adjustment to cancer. In: Baum A, Andersen B, editors. Psychosocial interventions for cancer. Washington, DC: American Psychological Association; 2001. pp. 99–118. [Google Scholar]
- 63.Lepore SJ, Ituarte PHG. Optimism about cancer enhances mood by reducing negative social interactions. Cancer Res Ther Control. 1999;8:165–174. [Google Scholar]
- 64.Danaher BG, Boles SM, Akers L, et al. Defining participant exposure measures in web-based health behavior change programs. J Med Internet Res. 2006;3:e15. doi: 10.2196/jmir.8.3.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gorlick A, Bantum EO, Owen JE. Internet-based interventions for cancer-related distress: Exploring the experiences of those whose needs are not met. Psycho-Oncol. 2014;23:452–8. doi: 10.1002/pon.3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McGee M. Google+Users Spend 3 Minutes Per Month There, ComScore Tells WSJ. [Last accessed on Nov 26, 2012]; http://marketingland.com/google-users-spend-3-minutes-per-month-there-6960.
- 67.Wagstaff K. Social networking: The average user spent only 3 minutes on Google+last month. [Last accessed on Nov 26, 2012];Time Magazine, published feb 28, 2012. http://techland.time.com/2012/02/28/the-average-user-spent-only-three-minutes-on-google-last-month/
- 68.Boyes AW, Girgis A, D’Este C, et al. Prevalence and correlates of cancer survivors’ supportive care needs 6 months after diagnosis: A population-based cross-sectional study. BMC Cancer. 2012;12:150. doi: 10.1186/1471-2407-12-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Giese-Davis J, Waller A, Carlson LE, et al. Screening for distress, the 6th vital sign: Common problems in cancer outpatients over one year in usual care: Associations with marital status, sex, and age. BMC Cancer. 2012;12:441. doi: 10.1186/1471-2407-12-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carlson LE, Doll R, Stephen J, et al. Randomized control trial of Mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. J Clin Oncol. 2013;31:3119–26. doi: 10.1200/JCO.2012.47.5210. [DOI] [PubMed] [Google Scholar]
- 71.Owen JE, Bantum EO, Criswell K, Bazzo J, Gorlick A, Stanton AL. Representativeness of two sampling procedures for an Internet intervention targeting cancer-related distress: A comparison of convenience and registry samples. J Behav Med. doi: 10.1007/s10865-013-9509-6. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]