Abstract
Severe sepsis is a leading cause of long-term morbidity in the United States. Up to half of severe sepsis is treated in non-intensive care unit (ICU) settings, making it applicable to hospitalist practice. Evidence has demonstrated benefits from physical therapy (PT) in myriad conditions; whether PT may benefit severe sepsis patients either within or outside the ICU is unknown. Therefore, we conduct a review of the literature to understand whether early mobilization improves outcomes in patients with severe sepsis in non-ICU settings. We summarize the pathophysiology of functional decline in severe sepsis, the efficacy of PT in other patient populations, and the potential rationale for PT interventions in patients with severe sepsis. Multiple databases were searched for keywords including length of stay, mortality, costs, mobilization and PT. Two authors (SG and VC) independently determined the eligibility of each study. A secondary review including studies of any infectious pathology with PT interventions or sepsis patients within the ICU was also conducted. Our search did not yield any primary literature regarding the impact of mobilization on severe sepsis outcomes in non-ICU settings. Only one retrospective study showed potential benefit of therapy in sepsis patients in the ICU. Similarly, in non-ICU settings, only one study that included patients with bacterial pneumonia reported outcomes after implementing an intervention consisting of early mobilization. These findings suggest that scant data regarding the efficacy of early mobilization following severe sepsis exists. Since hospitalists often care for this patient population, an opportunity for research in this area exists.
Keywords: sepsis, mobilization, physical therapy, outcomes, review
INTRODUCTION
Severe sepsis, defined as an infection leading to systemic inflammatory response and acute organ dysfunction, is a significant cause of morbidity and mortality.1–3 Although it has been a condition classically attributed to patients in intensive care units (ICU), accumulating data suggest that a substantial proportion of patients with severe sepsis are managed by hospitalists and floor teams in non-ICU, general ward-settings.1,4,5 Although the incidence of severe sepsis continues to rise both in the United States and other developed nations,2,6,7 advances in early recognition, management, and care of this condition have resulted in improved rates of survival.8 The resultant increase in a “severe sepsis survivor population”6 make the long-term sequelae of this condition an important public health problem.9
In both the ICU and on general wards, severe sepsis survivors suffer from decreased functional status, worsened quality of life, increased cognitive dysfunction, and sarcopenia.4,6,10–14 Not surprisingly, many such patients are discharged to long term care facilities for physical rehabilitation,15 with escalating utilization of resources16 and cost.17,18 Inexpensive interventions that improve outcomes following sepsis would thus be welcomed.
It is well known that physical therapy (PT) and early mobilization are beneficial in mitigating functional decline in a number of conditions.19–22 PT can improve outcomes in several ways: prevention of bed rest deconditioning; mitigation of mechanisms that lead to sarcopenia; increased pulmonary and tissue aerobic capacity; and improved sense of wellbeing. Indeed, among the population cared for in ICU-settings, early mobility and PT lead to more ventilator-free days, better functional status at discharge, shorter duration of delirium, and even a potentially reduced risk of CLABSI.23,24 However, whether initiating early PT can improve outcomes in patients with severe sepsis treated by either intensivists or hospitalists/floor teams outside the ICU is unknown.
Therefore, in order to better understand this phenomenon, we systematically reviewed and integrated the literature regarding early mobilization and PT for severe sepsis outside the ICU. In order to be more inclusive, a secondary review including populations with any infectious etiology and severe sepsis treated within the ICU was also conducted. Our review begins by providing an overview of the pathophysiology behind functional decline in severe sepsis, along with existing evidence on early mobilization efficacy in other patient populations. We then proceed with a review of the extant literature on the aforementioned topic. We conclude with an evaluation of the current evidence on the subject, along with assertions regarding future research in the area.
PATHOPHYSIOLOGY OF DISABILITY FOLLOWING HOSPITALIZATION FOR SEVERE SEPSIS
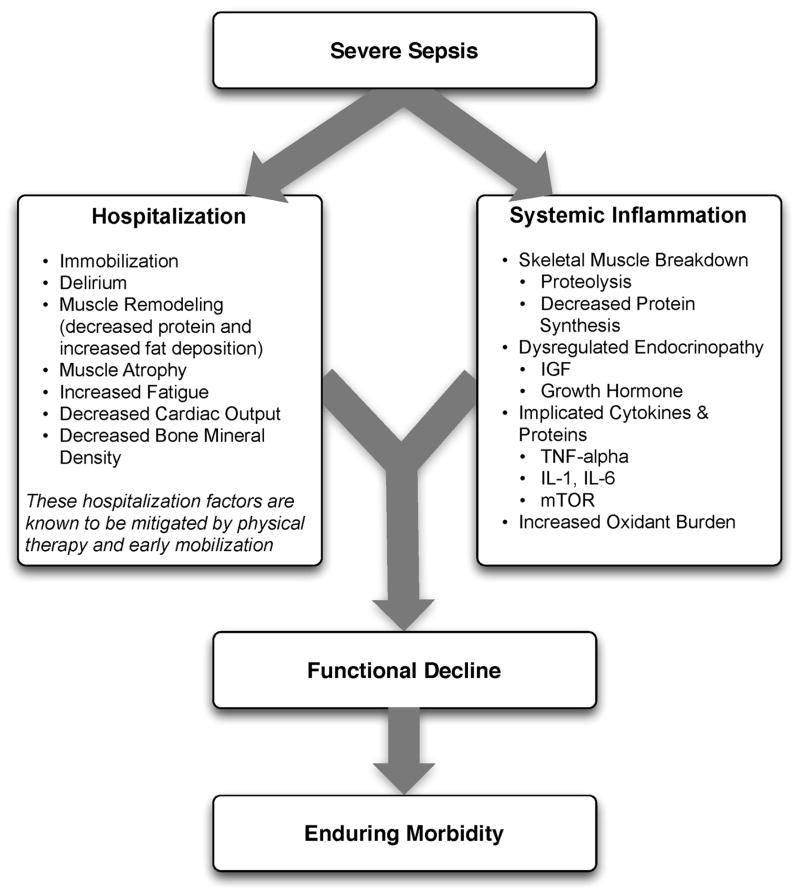
The pathophysiology behind functional decline in patients hospitalized with severe sepsis is multifactorial (Figure 1). During hospitalization, it is well known that patients suffer from restricted mobility25 and that this impediment is linked to poor functional outcomes.26 Described as far back as Hippocrates,27 more recent studies have elucidated how prolonged bed rest leads to a multitude of physiological changes that promote deconditioning.28 Specifically, skeletal muscle atrophy and decreased protein synthesis, independent of ongoing disease processes and acute illness, have been demonstrated in both animal and human models of prolonged inactivity.29,30 Additionally, bed-rest leading to insensible fluid losses, a decline in stroke volume and effective cardiac output, bone loss, and decreased insulin sensitivity has been reported.28,31 There is little doubt that the aforementioned issues pertain to severe sepsis patients outside the ICU; in fact, nearly all of the acute mechanisms driving Creditor’s “Hazards of Hospitalization” are noted among patients with severe sepsis.32
FIGURE 1.
Sepsis and Functional Decline Diagram
Further, several factors preceding hospitalization may increase risk of disability. For example, Covinsky et al. described a number of risk factors such as comorbid conditions, cognitive impairment, and various psychosocial aspects such as depression and limited social support as being associated with increased risk of functional decline.33 Thus, both in-hospital and pre-hospital factors likely combine within an individual patient’s context to determine risk of physical decline.
On this backdrop and the inherent immobilization associated with hospitalization, sepsis and inflammation catalyze physiologic changes that further propagate deconditioning.7 Implicated pathways and proteins for this process include the mammalian target of rapamycin (MTor), human growth hormone, insulin-like growth factors, interleukin-1, and tumor necrosis factor-alpha. Through several metabolic alterations, sepsis independently promotes skeletal muscle breakdown and impairs skeletal muscle synthesis.34–36 Inflammation associated with sepsis also increases oxidant burden, further leading to muscle dysfunction and dysregulation.7,31,37,38
EFFECTS OF PHYSICAL THERAPY AND MOBILIZATION ON CLINICAL OUTCOMES
In patients with non-sepsis conditions who are at risk for functional decline, the effectiveness of physical therapy has been studied in multiple settings with positive outcomes. For example, in hospitalized elderly patients with general deconditioning, PT-based interventions have demonstrated reductions in length of hospital stay.39 Additionally, exercise in healthy subjects who have been subjected to bed rest has been shown to attenuate physiological changes, maintain plasma and red cell volume and work capacity.40 Adequate safety and improved outcomes have also been demonstrated in the general population of critically ill patients who receive early PT and mobilization: improved functional capacity at discharge, decreases in duration of delirium, increased ventilator-free days, decreased risk for CLABSI, and a better general sense of wellbeing following these interventions have been widely reported in the literature.14,19,23,24,41–45 Interestingly, critically ill patients may have a dose- and time-dependent response to PT; that is, high intensity and early onset mobility-based interventions are often associated with more ventilator free time and improved functional outcomes, resulting in shorter ICU and hospital length of stay.42,46–48
Moderate intensity exercise has also been shown to improve 6-minute walking distance in patients convalescing from coronary artery bypass grafting surgery.49 Furthermore, in the post-operative setting, patients suffering traumatic hip fractures are known to benefit from physical and occupational therapies with shorter time to ambulation and improved locomotion in the recovery period.21,50,51 Among patients with stroke, PT and gait training has led to improvements in speed, gait, independence during walking, activities of daily living, and extended activities of daily living.52–54 A recent meta-analysis also suggested that extra PT compared to regular treatment in patients with acute and subacute conditions such as stroke and post-operative states improved mobility and quality of life, while reducing length of hospital stay.22
Although this evidence suggests potential benefits for PT and mobilization, it is important to note that the effect of these treatments in dissimilar populations is unknown and may not necessarily be positive. For example, a recent study examining PT and its impact on patients with hip osteoarthritis showed no clinical benefit.55 Mobilizing patients in severe illness may be associated with important risks, including falls, worsening of their clinical status or moral discouragement in the setting of limited capacity. Therefore, understanding which elements of mobilization efforts create the greatest impact in the context of delivery of the intervention is critical to assessing the risk, benefit and efficacy of PT-based interventions.
EARLY PHYSICAL THERAPY FOR SEVERE SEPSIS OUTSIDE THE ICU: LITERATURE REVIEW
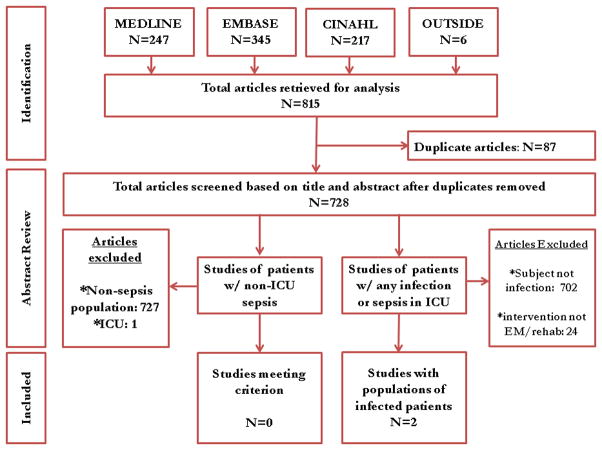
Given the functional decline associated with severe sepsis and the evidence of PT efficacy in other populations, we reviewed the current literature for studies evaluating physical therapy in severe sepsis patients outside the ICU. With the assistance of medical reference librarians, we searched MEDLINE via PubMed (1950-present), EMBASE (1946-present), Cochrane CENTRAL Register of Controlled Trials, and the Cochrane Database of Reviews of Effectiveness (1960-present, via Ovid). The search was last updated in June 2014. Detailed search criteria are available in the appendix.
We searched for studies that (a) involved human patients ≥ 18 years of age; (b) included patients with a primary diagnosis of sepsis or severe sepsis being treated outside the ICU; (c) featured a primary intervention that included PT or an early mobilization-based initiative; and (d), reported a primary clinical or functional outcome of interest. “Early” was defined based on the included studies’ definition. In order to be fully inclusive, we also conducted a secondary review with inclusion criteria expanded to studies of either any infectious pathology or severe sepsis patient in the ICU that employed PT interventions.
Our electronic search retrieved 815 records (Figure 2). Despite this approach, no publications met our primary inclusion criteria as we found no study that implemented a mobility intervention directed towards patients with sepsis treated outside the ICU. Our expanded secondary review included patients with any infectious pathology or those with severe sepsis in the ICU treated with PT; in this review, two studies met eligibility criteria.56 In a 2003 cluster-randomized trial, Mundy and colleagues randomized patients admitted with pneumonia to receive early PT or usual care. The outcomes of interest were hospital length of stay, mortality, number of chest radiographs, emergency department visits, and readmissions at 30 and 90 days after hospital admission. Although the study has important limitations (including patient-level difference between trial arms, subjective definition of early mobilization), the authors found a significant decrease in length of stay among patients with pneumonia who received early PT compared to controls (5.8 vs. 6.9 days, absolute difference 1.1 days, 95% CI 0–2.2 days). The study also reported a substantial decrease in adjusted mean hospital charges for the early mobilization group vs. the usual care group ($10,159 per patient vs. $12,868 per patient, p=0.05). In the second study, Sossdorf et al. retrospectively evaluated a cohort of 999 patients with severe sepsis and septic shock and assessed whether onset and frequency of PT-based interventions was associated with clinical benefit. After multivariate analysis, the authors reported a small mortality benefit associated with the relative number of PT interventions (HR 0.982, P< 0.001).45
Figure 2.
EXPLAINING THE VOID
Our integrative review of the current literature reveals a gap in our understanding of the role of early mobilization in severe sepsis both within and beyond the ICU. Given the promise of PT-based interventions and the toll of severe sepsis, one must ask: why may this be so?
First, the understanding that severe sepsis leads to significant, long-term consequences for survivors has only been identified recently. Thus, it is possible that the burden and consequences related to this condition have not been fully recognized in clinical settings, leading to a paucity of research and interventions. Although the association between sepsis and mortality has been known since the 1990s,57 long-term complications and enduring morbidity of this disease continue to be realized. Indeed, many studies delineating the longer-term effects of sepsis have been only recently published.6,10–13
Second, it is likely that many clinicians ascribe to the viewpoint that severe sepsis is an ICU-only condition, a myth that has been discounted by multiple studies.1,4,5 While our study shows a paucity of evidence in both ICU and non-ICU based severe sepsis, almost half of severe sepsis occurs outside the ICU, carrying with it many of the same clinical implications. Additionally, increased morbidity, mortality, and resource utilization are known to be true in all patients with severe sepsis, irrespective of where they receive treatment in the hospital.4–6 Recent evidence has also shown that severe sepsis treated on the floor may be clinically, epidemiologically, and even prognostically unique from its ICU counterpart.5,58,59 Therefore, it appears that research domains with tailored interventions to both ICU and non-ICU severe sepsis patients are important areas of inquiry for clinicians. Such research may serve the purpose of assessing impact of early mobilization and unmasking any treatment heterogeneity that may exist when dealing with severe sepsis. Though trials of PT in ICU-based severe sepsis are underway,60 it is prudent that these also extend beyond the ICU-setting.
Third, variability in early mobility practices and billing documentation for severe sepsis patients exist, adding barriers to performing high-quality research on this topic. In fact, administrative billing records for PT offer insufficient granularity about services provided or therapies administered—particularly in the crucial domains of distinguishing early mobility from “initial evaluation” or chest physiotherapy, and about the timing and intensity of such therapy.61
Finally, many hospitalists may believe that patients with severe sepsis are simply “too sick” for early mobilization or PT —possibly limiting their participation in clinical or research-based interventions. This perception has been well described in ICU populations, where it has been well studied and shown to be false.41–43 Nevertheless, if severe sepsis patients are viewed as relatively “sick” hospitalized patients, it is plausible that resistance against early mobilization interventions may exist.62 Understanding these biases and being mindful of such barriers when conducting studies in this area would be important.
CONCLUSION AND FUTURE DIRECTIONS
The cost burdens of severe sepsis are substantial: Elixhauser et al. suggest that it is currently the single most expensive cause of acute hospitalization in the United States.63 Importantly, a large proportion of patients with severe sepsis receive care from hospitalists and/or floor teams on the general wards. Our integrative review has demonstrated a knowledge gap when it comes to rigorous assessments of PT and mobilization treatments in patients with severe sepsis within and beyond the ICU. Existing evidence provides a strong rationale for why functional decline occurs in patients with severe sepsis. A reasonable argument for PT-based interventions to mitigate functional decline in this subset exists, but rigorous evaluation of such interventions is necessary. Physical and mobilization-based treatments are routinely available and efficacious in several other settings and populations. It could be rapidly deployed and potentially improve outcomes in those with severe sepsis. Research would be welcomed to establish optimal dosing, efficacy, and cost effectiveness of PT and early mobilization for severe sepsis, particularly in patients treated on the general wards by hospitalists and floor teams
How may such a research agenda be launched? A balanced multi-pronged approach is necessary. First, large-scale epidemiological data to understand variation in practice is needed. Focused studies carried out by community and academic hospitalists on septic patients treated outside the ICU are the call of the hour. These data, in turn, can help create registries that assess for risk factors, quality of treatment, and long term outcomes among survivors of this condition. Second, evaluation and improvement of the coding and precision of physical and occupational therapy billing records is necessary so that their added value can be assessed and tracked using administrative data. Third, targeted prospective studies and clinical trials to directly evaluate the effect of PT in well-defined patient populations with sepsis outside the ICU are needed. In this arena, hospitalist expertise and trained physical therapists will be crucial. The focus of this work should be directed towards both short-term and long-term functional outcomes, as well as mortality and morbidity assessments. Fourth, these patient-centered efforts should loop back and inform the foundational biology of severe sepsis, thus illuminating patient-centered endpoints, from biomarker analysis to physiometric measurements in basic and translational research.
In conclusion, this review sheds light on the fact that interventions that may mitigate the functional and cognitive decline in survivors of severe sepsis appear underdeveloped. Although the precise benefit of such interventions remains unclear, the low-cost, widespread availability and generalizability of PT-based interventions make it a worthy candidate for future research. As the numbers of survivors of sepsis expand, an unmet public health need for interventions to improve the long-term outcomes of this population exists. Hospitalists and intensivists caring for severe sepsis patients must rise to meet this need. Together, we can help improve the lives of patients afflicted with severe sepsis, wherever they may receive care in the hospital.
Acknowledgments
This work was supported by U.S. National Institutes of Health – K08, HL091249 (TJI) and VA HSR&D IIR-11-109 (TJI).
We would like to acknowledge the efforts of medical research librarians Andy Hickner, MSI and Marissa Conte, MSI on this project.
Footnotes
The views expressed here are the authors’ own and do not necessarily represent the view of the U.S. Government or the Department of Veterans’ Affairs.
The authors have no other conflicts of interest to disclose.
References
- 1.Angus DC, Wax RS. Epidemiology of sepsis: an update. Crit Care Med. 2001;29:S109–116. doi: 10.1097/00003246-200107001-00035. [DOI] [PubMed] [Google Scholar]
- 2.Kumar G, Kumar N, Taneja A, et al. Nationwide trends of severe sepsis in the 21st century (2000–2007) Chest. 2011;140:1223–1231. doi: 10.1378/chest.11-0352. [DOI] [PubMed] [Google Scholar]
- 3.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 4.Odden AJ, Rohde JM, Bonham C, et al. Functional outcomes of general medical patients with severe sepsis. BMC Infect Dis. 2013;13:588. doi: 10.1186/1471-2334-13-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rohde JM, Odden AJ, Bonham C, et al. The epidemiology of acute organ system dysfunction from severe sepsis outside of the intensive care unit. J Hosp Med. 2013;8:243–247. doi: 10.1002/jhm.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iwashyna TJ, Cooke CR, Wunsch H, et al. Population burden of long-term survivorship after severe sepsis in older Americans. J Am Geriatr Soc. 2012;60:1070–1077. doi: 10.1111/j.1532-5415.2012.03989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fink H, Helming M, Unterbuchner C, et al. Systemic inflammatory response syndrome increases immobility-induced neuromuscular weakness. Crit Care Med. 2008;36:910–916. doi: 10.1097/CCM.0B013E3181659669. [DOI] [PubMed] [Google Scholar]
- 8.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 9.Angus DC. The lingering consequences of sepsis: a hidden public health disaster? JAMA. 2010;304:1833–1834. doi: 10.1001/jama.2010.1546. [DOI] [PubMed] [Google Scholar]
- 10.Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iwashyna TJ, Netzer G, Langa KM, et al. Spurious inferences about long-term outcomes: the case of severe sepsis and geriatric conditions. Am J Respir Crit Care Med. 2012;185:835–841. doi: 10.1164/rccm.201109-1660OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karlsson S, Ruokonen E, Varpula T, et al. Long-term outcome and quality-adjusted life years after severe sepsis. Crit Care Med. 2009;37:1268–1274. doi: 10.1097/CCM.0b013e31819c13ac. [DOI] [PubMed] [Google Scholar]
- 13.Winters BD, Eberlein M, Leung J, et al. Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med. 2010;38:1276–1283. doi: 10.1097/CCM.0b013e3181d8cc1d. [DOI] [PubMed] [Google Scholar]
- 14.Hopkins RO, Suchyta MR, Farrer TJ, et al. Improving post-intensive care unit neuropsychiatric outcomes: understanding cognitive effects of physical activity. Am J Respir Crit Care Med. 2012;186:1220–1228. doi: 10.1164/rccm.201206-1022CP. [DOI] [PubMed] [Google Scholar]
- 15.Lagu T, Rothberg MB, Shieh MS, et al. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2012;40:754–761. doi: 10.1097/CCM.0b013e318232db65. [DOI] [PubMed] [Google Scholar]
- 16.Kahn JM, Benson NM, Appleby D, et al. Long-term acute care hospital utilization after critical illness. JAMA. 2010;303:2253–2259. doi: 10.1001/jama.2010.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dick A, Liu H, Zwanziger J, et al. Long-term survival and healthcare utilization outcomes attributable to sepsis and pneumonia. BMC Health Serv Res. 2012;12:432. doi: 10.1186/1472-6963-12-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weycker D, Akhras KS, Edelsberg J, et al. Long-term mortality and medical care charges in patients with severe sepsis. Crit Care Med. 2003;31:2316–2323. doi: 10.1097/01.CCM.0000085178.80226.0B. [DOI] [PubMed] [Google Scholar]
- 19.Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009;37:2499–2505. doi: 10.1097/CCM.0b013e3181a38937. [DOI] [PubMed] [Google Scholar]
- 20.Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011:CD001800. doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoenig H, Rubenstein LV, Sloane R, et al. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157:513–520. [PubMed] [Google Scholar]
- 22.Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med Rehabil. 2011;92:1490–1500. doi: 10.1016/j.apmr.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Hunter A, Johnson L, Coustasse A. Reduction of intensive care unit length of stay: the case of early mobilization. Health Care Manag (Frederick) 2014;33:128–135. doi: 10.1097/HCM.0000000000000006. [DOI] [PubMed] [Google Scholar]
- 24.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 26.Zisberg A, Shadmi E, Sinoff G, et al. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59:266–273. doi: 10.1111/j.1532-5415.2010.03276.x. [DOI] [PubMed] [Google Scholar]
- 27.Chadwick JaWNM. The Medical Works of Hippocrates. Oxford: Blackwell; 1950. [Google Scholar]
- 28.Convertino VA, Bloomfield SA, Greenleaf JE. An overview of the issues: physiological effects of bed rest and restricted physical activity. Med Sci Sports Exerc. 1997;29:187–190. doi: 10.1097/00005768-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Ferrando AA, Lane HW, Stuart CA, et al. Prolonged bed rest decreases skeletal muscle and whole body protein synthesis. Am J Physiol. 1996;270:E627–633. doi: 10.1152/ajpendo.1996.270.4.E627. [DOI] [PubMed] [Google Scholar]
- 30.Stein TP, Wade CE. Metabolic consequences of muscle disuse atrophy. J Nutr. 2005;135:1824S–1828S. doi: 10.1093/jn/135.7.1824S. [DOI] [PubMed] [Google Scholar]
- 31.Winkelman C. Inactivity and inflammation in the critically ill patient. Crit Care Clin. 2007;23:21–34. doi: 10.1016/j.ccc.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 33.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA. 2011;306:1782–1793. doi: 10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- 34.Breuille D, Voisin L, Contrepois M, et al. A sustained rat model for studying the long-lasting catabolic state of sepsis. Infect Immun. 1999;67:1079–1085. doi: 10.1128/iai.67.3.1079-1085.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vary TC. Regulation of skeletal muscle protein turnover during sepsis. Curr Opin Clin Nutr Metab Care. 1998;1:217–224. doi: 10.1097/00075197-199803000-00013. [DOI] [PubMed] [Google Scholar]
- 36.Lang CH, Frost RA, Vary TC. Regulation of muscle protein synthesis during sepsis and inflammation. Am J Physiol Endocrinol Metab. 2007;293:E453–459. doi: 10.1152/ajpendo.00204.2007. [DOI] [PubMed] [Google Scholar]
- 37.Couillard A, Prefaut C. From muscle disuse to myopathy in COPD: potential contribution of oxidative stress. Eur Respir J. 2005;26:703–719. doi: 10.1183/09031936.05.00139904. [DOI] [PubMed] [Google Scholar]
- 38.Macdonald J, Galley HF, Webster NR. Oxidative stress and gene expression in sepsis. Br J Anaesth. 2003;90:221–232. doi: 10.1093/bja/aeg034. [DOI] [PubMed] [Google Scholar]
- 39.Fisher SR, Kuo YF, Graham JE, et al. Early ambulation and length of stay in older adults hospitalized for acute illness. Arch Intern Med. 2010;170:1942–1943. doi: 10.1001/archinternmed.2010.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greenleaf JE. Intensive exercise training during bed rest attenuates deconditioning. Med Sci Sports Exerc. 1997;29:207–215. doi: 10.1097/00005768-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35:139–145. doi: 10.1097/01.CCM.0000251130.69568.87. [DOI] [PubMed] [Google Scholar]
- 42.Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36:2238–2243. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 43.Kress JP. Clinical trials of early mobilization of critically ill patients. Crit Care Med. 2009;37:S442–447. doi: 10.1097/CCM.0b013e3181b6f9c0. [DOI] [PubMed] [Google Scholar]
- 44.Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300:1685–1690. doi: 10.1001/jama.300.14.1685. [DOI] [PubMed] [Google Scholar]
- 45.Sossdorf M, Otto GP, Menge K, et al. Potential effect of physiotherapeutic treatment on mortality rate in patients with severe sepsis and septic shock: a retrospective cohort analysis. J Crit Care. 2013;28:954–958. doi: 10.1016/j.jcrc.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 46.Chiang LL, Wang LY, Wu CP, et al. Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys Ther. 2006;86:1271–1281. doi: 10.2522/ptj.20050036. [DOI] [PubMed] [Google Scholar]
- 47.Martin UJ, Hincapie L, Nimchuk M, et al. Impact of whole-body rehabilitation in patients receiving chronic mechanical ventilation. Crit Care Med. 2005;33:2259–2265. doi: 10.1097/01.ccm.0000181730.02238.9b. [DOI] [PubMed] [Google Scholar]
- 48.Nava S. Rehabilitation of patients admitted to a respiratory intensive care unit. Arch Phys Med Rehabil. 1998;79:849–854. doi: 10.1016/s0003-9993(98)90369-0. [DOI] [PubMed] [Google Scholar]
- 49.Hirschhorn AD, Richards D, Mungovan SF, et al. Supervised moderate intensity exercise improves distance walked at hospital discharge following coronary artery bypass graft surgery--a randomised controlled trial. Heart Lung Circ. 2008;17:129–138. doi: 10.1016/j.hlc.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 50.Chudyk AM, Jutai JW, Petrella RJ, et al. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil. 2009;90:246–262. doi: 10.1016/j.apmr.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 51.Penrod JD, Boockvar KS, Litke A, et al. Physical therapy and mobility 2 and 6 months after hip fracture. J Am Geriatr Soc. 2004;52:1114–1120. doi: 10.1111/j.1532-5415.2004.52309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brazzelli M, Saunders DH, Greig CA, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2011:CD003316. doi: 10.1002/14651858.CD003316.pub4. [DOI] [PubMed] [Google Scholar]
- 53.Veerbeek JM, Koolstra M, Ket JC, et al. Effects of augmented exercise therapy on outcome of gait and gait-related activities in the first 6 months after stroke: a meta-analysis. Stroke. 2011;42:3311–3315. doi: 10.1161/STROKEAHA.111.623819. [DOI] [PubMed] [Google Scholar]
- 54.Kwakkel G, van Peppen R, Wagenaar RC, et al. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke. 2004;35:2529–2539. doi: 10.1161/01.STR.0000143153.76460.7d. [DOI] [PubMed] [Google Scholar]
- 55.Bennell KL, Egerton T, Martin J, et al. Effect of physical therapy on pain and function in patients with hip osteoarthritis: a randomized clinical trial. JAMA. 2014;311:1987–1997. doi: 10.1001/jama.2014.4591. [DOI] [PubMed] [Google Scholar]
- 56.Mundy LM, Leet TL, Darst K, et al. Early mobilization of patients hospitalized with community-acquired pneumonia. Chest. 2003;124:883–889. doi: 10.1378/chest.124.3.883. [DOI] [PubMed] [Google Scholar]
- 57.Quartin AA, Schein RM, Kett DH, et al. Magnitude and duration of the effect of sepsis on survival. Department of Veterans Affairs Systemic Sepsis Cooperative Studies Group. JAMA. 1997;277:1058–1063. [PubMed] [Google Scholar]
- 58.Sundararajan V, Macisaac CM, Presneill JJ, et al. Epidemiology of sepsis in Victoria, Australia. Crit Care Med. 2005;33:71–80. doi: 10.1097/01.ccm.0000150027.98160.80. [DOI] [PubMed] [Google Scholar]
- 59.Esteban A, Frutos-Vivar F, Ferguson ND, et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med. 2007;35:1284–1289. doi: 10.1097/01.CCM.0000260960.94300.DE. [DOI] [PubMed] [Google Scholar]
- 60.Kayambu G, Boots RJ, Paratz JD. Early rehabilitation in sepsis: a prospective randomised controlled trial investigating functional and physiological outcomes The i-PERFORM Trial (Protocol Article) BMC Anesthesiol. 2011;11:21. doi: 10.1186/1471-2253-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carol LH, Sue B, Rinaldo B, et al. ICU. B104. ICU WEAKNESS ON THE RUN: EXERCISE, ELECTRICAL STIMULATION, AND PHARMACOTHERAPY. American Thoracic Society; 2013. TEAM: A Prospective Multi-Centre Cohort Study Of Early Activity And Mobilisation; pp. A3625–A3625. [Google Scholar]
- 62.Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40:502–509. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 63.Elixhauser A, Friedman B, Stranges E. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): 2006. Septicemia in U.S. Hospitals, 2009: Statistical Brief #122. [Google Scholar]