Abstract
Objective
The presence of anxiety disorders is associated with poorer alcohol use disorder treatment outcomes, but little is known about the impact of alcohol use problems on anxiety disorder treatment outcomes despite their high comorbidity. The current study examined the impact of alcohol use symptom severity on anxiety disorder treatment outcomes in a multi-site primary care effectiveness study of anxiety disorder treatment.
Method
Data came from the Coordinated Anxiety Learning and Management (CALM) effectiveness trial. Participants (N = 1004) were randomized to an evidence-based anxiety intervention (including cognitive behavioral therapy and medications) or usual care in primary care. Participants completed measures of alcohol use, anxiety, and depression a baseline, 6-mo, 12-mo, and 18-mo follow-up periods. Patients with alcohol dependence were excluded.
Results
There were no significant moderating (Treatment Group x Alcohol Use Severity) interactions. The majority of analyses revealed no predictive effects of alcohol use severity on outcome; however, alcohol problems at baseline were associated with somewhat higher anxiety and depression symptoms at the 18-mo follow-up.
Conclusions
These data indicate that patients with alcohol problems in primary care can be effectively treated for anxiety disorders. Baseline alcohol problems were associated with some poorer long-term outcomes, but this was evident across CALM and usual care. These findings provide preliminary evidence that there may be no need to postpone treatment of anxiety disorders until alcohol problems are addressed, at least among those who have mild to moderate alcohol problems. Replication with more severe alcohol use disorders is needed.
Keywords: Alcohol use, anxiety disorders, predictors of treatment outcome
Anxiety disorders are highly prevalent in addiction treatment settings (1–6). Anxiety disorder comorbidity is associated with poorer alcohol use disorder (AUD) outcomes (e.g., greater percentage of patients relapsing compared to those with no comorbid anxiety disorder; see 7 for a review). In contrast, the effects of alcohol use problems among those seeking treatment for anxiety disorders are not well understood. The available studies sometimes report on presence of comorbid AUD but not its associated effects (8). One exception found that in those treated for an anxiety disorder, AUDs were associated with a greater likelihood of anxiety recurrence over a follow-up period (9). The paucity of data may be due in part to the common AUD exclusionary criteria in anxiety disorder treatment studies. In community practices, the presence of AUDs may not preclude someone from seeking treatment for anxiety disorders; yet it is unclear how alcohol use disorders affect treatment outcomes for anxiety.
Given the high comorbidity (e.g., 10), clinical settings providing treatment for anxiety disorders likely have a significant proportion of patients with AUDs or alcohol use problems. Indeed, hazardous drinking estimates in primary care range from 4–29% (see 11). Estimates of AUD in primary care are lower, ranging from 3% to 14% (12, 13), likely due to two factors: 1) the lower prevalence overall of AUDs compared to mild-moderate alcohol problems (14–16); and 2) Most patients with comorbid anxiety and AUD are more likely to receive treatment for their addiction in a substance abuse specialty clinic than for their anxiety disorder in another (e.g., primary care, mental health clinic) setting (17).
It remains unclear whether alcohol problems typically present in primary care interfere with treatment for anxiety disorders. Understanding whether alcohol use severity (AUS) in this population predicts outcomes can provide important prognostic information to clinicians. If AUS predicts poorer outcomes, identification of alcohol use problems may be important in order to make treatment decisions (18, 19)
However, if alcohol use symptoms do not affect outcomes, then individuals can seek treatment for their anxiety disorders while alcohol problems are present. Common practice typically encourages patients with comorbid substance use and mental health problems to seek addiction treatment first, a practice that may lead to untreated mental health problems (17). Recent models suggest that treating anxiety and alcohol use disorders in an integrated approach may be preferable both from clinical (7, 20–22) and public health perspectives, as this model is in line with recommendations from the Affordable Care Act (23–25).
The current study examines the impact of AUS on anxiety treatment outcomes in a large effectiveness trial of anxiety disorder treatment in primary care. The effectiveness trial (Coordinated Anxiety Learning and Management; CALM) was conducted in primary care and utilized clinicians with minimal mental health training. Participants were randomized to usual care (UC) or the CALM intervention, which included cognitive behavioral therapy (CBT) and medications. Given that many community providers are not likely to conduct a formal diagnostic assessment of AUD, a brief dimensional screening measure of AUS may have broader applicability to clinical practice. Thus, the current study examines whether scores on a dimensional measure of AUS predict anxiety treatment outcomes. We examined both prescriptive effects (i.e., whether AUS predicts anxiety outcomes differentially between CALM and UC) and prognostic effects (i.e., if prescriptive effects are not observed, whether AUS predict anxiety outcomes generally across conditions). Based on the limited previous research, we expected that greater AUS would be associated with poorer anxiety outcomes in both the UC and CALM arms of the study. We had no specific hypothesis about whether AUS would moderate outcomes. Thus, although we conducted a moderator analysis, our prediction was that AUS would serve as a prognostic predictor of outcome.
Methods
Participants
Adult primary care English or Spanish-speaking patients who met criteria for panic, social anxiety, generalized anxiety, or post-traumatic stress disorder and scored at least an 8 (moderate and clinically significant anxiety symptoms) on the Overall Anxiety Severity and Impairment Scale (OASIS; 26) were recruited from clinics across four sites. Exclusion criteria included unstable medical conditions, cognitive impairment, active suicidality, bipolar I disorder, psychotic disorders, current enrollment in CBT. Alcohol and marijuana abuse (but not dependence) were permitted. Abuse and dependence of other drugs were exclusionary. The sample (N =1004) was 71.2% female (mean age 43.47; SD=13.44). Participants were 56.57% White, 19.52% Hispanic/Latino, 11.55% Black/African-American, and 12.35 % other race.
In the CALM arm of the study, participants completed 7 CBT sessions on average (SD=4.1). Of the 482 participants in the CALM arm, 166 (34%) had only CBT. A small proportion of subjects (69/482 [14%]) also had an in-person visit with the study psychiatrist. See Roy-Byrne et al. (27) for detailed descriptions of the procedures and a flowchart of participation throughout the study. See Table 1 for information about attrition over the follow-up period.
Table 1.
Attrition over the study
| CALM | UC | |||
|---|---|---|---|---|
| Time-point | Number of assessments administered | Percentage drop-out | Number of assessments administered | Percentage drop-out |
| Baseline | 503 | 0.00 | 501 | 0.00 |
| 6 Months | 446 | 11.33 | 430 | 14.17 |
| 12 Months | 410 | 18.49 | 403 | 19.56 |
| 18 Months | 409 | 18.69 | 395 | 21.16 |
Note: Table 1 includes data on the number of participants who completed assessment at baseline and each of the follow-up time-points.
Measures
Diagnostic Measure
Mini International Neuropsychiatric Interview (MINI; 28)
The MINI Neuropsychiatric Interview is a concise structured diagnostic interview designed to assess for psychiatric diagnoses in multicenter clinical trials (28). When compared with the SCID-P (29) kappa values for the majority of the psychiatric diagnoses were .70 or above. Five of the diagnoses had kappa values between .60 and .70 (30). Interviewers were trained to 80% reliability before independently conducting assessments.
Putative Predictor: Alcohol Use Symptom Measure
Alcohol Use Disorders Identification Test (AUDIT; 31)
The AUDIT is a brief (10-item) gold standard alcohol use disorder screening measure that has shown excellent psychometric properties across several countries. The intraclass correlation on this measure is high (.95), and it is highly sensitive (range= .70 to .97) and specific (range= .88–.98; 32, 33). The questions assess alcohol consumption, alcohol dependence, and alcohol-related problems. AUDIT scores are typically categorized by four “Risk Zones” that indicate to providers the level of care needed at the time of screening.
Outcome Measures
All outcome measures were completed at baseline, 6, 12, and 18-monthsafter baseline. Twelve and 18-month outcomes were included in the analyses because some participants were still in treatment at 6-months.
Primary: Brief Symptom Inventory-12 (BSI-12; 34)
The BSI measures symptoms of psychiatric and medical patients (35), and this study used two subscales (psychic and somatic anxiety), which resulted in the 12-item BSI subscales for anxiety and somatization. The BSI has high test-restest reliability and high validity (36).
Primary: Anxiety Sensitivity Index (ASI; 37)
The ASI is a 16-item measure of beliefs that anxiety symptoms are being harmful. Items measure physical, social, and mental concerns about physical anxiety symptoms. The ASI shows sensitivity to change after CBT for anxiety disorders (e.g., 38) and has demonstrated good reliability and is distinct from other anxiety measures (39).
Secondary: Patient Health Questionnaire (PHQ-8; 40)
The PHQ-9 is a measure of depression symptoms, including each of the DSM -IV diagnostic criteria for depression ranging from 0 (not at all) to 3 (nearly every day). The suicide item was removed, reducing the scale to 8 items. PHQ-9 has excellent internal reliability with a Cronbach’s α = .89 and a correlation of r = .84 between the self-report and clinician-administered PHQ-9.
Procedures
This study was approved by the Institutional Review Boards at all sites. Referrals were made through primary care providers. Referred patients met with an Anxiety Clinical Specialist (ACS), who was usually a nurse or social worker, to determine eligibility. Eligible participants were randomized to the CALM intervention or UC. See Roy -Byrne et al. (27), for randomization details as well as further details about the treatment conditions described in brief below.
CALM
Patients in the CALM arm received CBT, medication, or both, depending on their preference. Patients with multiple anxiety disorders were asked to identify the disorder that caused the most distress or impairment as the focus of CBT. CBT was delivered weekly by the ACS, who was guided by a computer program. Primary care providers prescribed medications (with psychiatric consultation available). After the acute phase of treatment, patients entered the “continued care” phase in which they received monthly phone calls by the ACS for up to 12 months. All ACSs received weekly supervision by a psychiatrist and psychologist.
UC
Participants in the UC condition received usual care in their primary care clinics. This included counseling that was available as part of standard clinic care, as well as continued contact with their primary care physician and medication as indicated. Contact with study personnel was limited to that required for assessment.
Statistical Analyses
Two-level hierarchical linear models (HLM 6; 41) were conducted with the outcome measures (i.e., BSI, ASI, and PHQ-8) entered as dependent variables (DV) in a separate series of models with Time (12-and 18 -month follow-ups) as the level 1 predictor. Level 2 included the baseline score of the outcome variable, baseline score on the AUDIT, Group (ITV or UC), and a series of covariates. The covariates included age, gender, ethnicity (White v. non-White), presence of health insurance coverage, employment status (working v. not working), number of medical conditions, use of medication, family income level, and highest year of education completed. In the first model with each DV, covariates were examined to see if they were significantly associated with outcome. If they were not, they were removed and a simpler model with fewer covariates was run.
We first examined Group x AUDIT x Time interactions. A significant interaction indicated that significant moderation of AUDIT by condition changed overtime, in which case we would recode Time to cross-sectionally examine the moderating effect at 12-month and 18-months. Aiken & West’s (42) approach to post hoc testing was used to examine the nature of the interaction by centering the moderator (AUDIT) at high, medium, and low levels to identify between-group (CALM v. UC) differences at each level of the moderator. If Time was non-significant (i.e., no significant AUDIT x Group x Time interaction), it was removed from the model and the Group x AUDIT moderating effect was examined (with the same post-hoc testing to examine the nature of significant interactions described above). A significant effect with Time removed represented the effects collapsed across Time (12 and 18 month follow-ups), with follow-up points with more data weighted more heavily. If there was no significant Group x AUDIT effect, interaction terms were removed and main effects of AUDIT (and treatment group) were examined. A main effect of AUDIT suggests that AUDIT scores significantly predict outcome across treatment groups. Similar approaches have been taken in published moderator papers (e.g., 43, 44–46).
Because of the non-normal distribution of AUDIT scores in the sample (in part due to what we would expect epidemiologically with regard to AUS in the population, but also likely due to alcohol dependence exclusion), we conducted secondary analyses using a dichotomous variable of alcohol problems v. no problems as a predictor instead of the continuous AUDIT score. To increase sensitivity and capture more alcohol problems in this sample with relatively low AUS, alcohol problems were operationalized as an AUDIT score of 7 or higher (31). Participants with AUDIT scores below 7 were categorized as having no alcohol problems. These secondary findings are presented when they differ from the findings including the full sample.
Results
AUDIT Scores
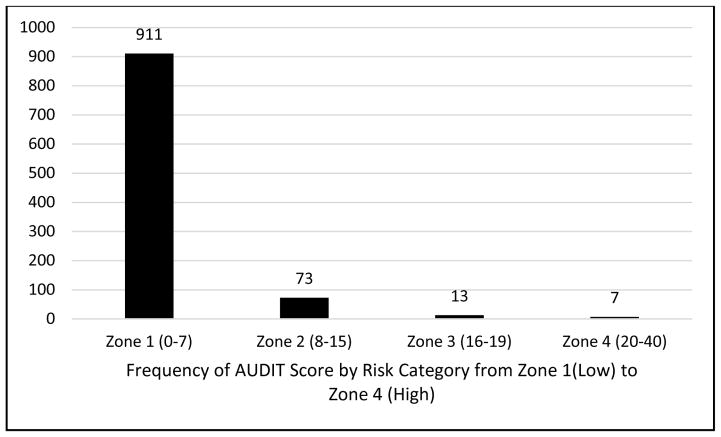
Participants were excluded if they met criteria for alcohol dependence (but not abuse). The mean AUDIT score was 2.69 (SD = 3.79), with 9.3% of AUDIT scores exceeding the cutoff for significant alcohol problems (8 or above). When lowering the cutoff to 7 or above (as recommended for increased sensitivity; 31), 11.3% of the sample exceeded the cutoff indicating significant alcohol problems. Figure 1 shows the frequencies in this sample of each Risk Zone (31).. Zone 1 indicates education only; Zones 2 and 3 indicate brief intervention (with continued monitoring in Zone 3) and Zone 4 indicates a need for a specialty addiction treatment referral (31). As shown in the table, the prevalence of alcohol problems is consistent with what would be expected of a primary care sample (see 11 for a review), and in particular has few cases in Zones 3 and 4, given that alcohol dependence was an exclusionary criterion.
Figure 1.
Frequency of AUDIT Scores by Risk Zone in the CALM Sample
Note: Zone categories were not used to classify patients in any of the statistical analyses, but are presented in order to provide a meaningful descriptive summary of the level of alcohol severity seen in this primary care sample.
AUDIT Scores as Moderators of Anxiety Treatment Outcome
BSI
Significant covariates in the first model included insurance status, number of medical conditions, and BSI score at baseline. The covariates were retained in all models with BSI as the DV. Time did not interact with the AUDIT x Group interaction (p = .45), so Time was removed from the model. The new model revealed no significant AUDIT x Group interaction (p = .95).
Because no moderation was observed, a set of models was run to examine main effects. There was a significant AUDIT x Time interaction, b = .14, t (673) = 2.07, p < .05, indicating that there was a significant change from 12-mo to 18-mo follow-ups in the way AUDIT scores predicted BSI scores. Post hoc tests examined the effect of AUDIT scores cross-sectionally at each of the follow-up periods. The effect of AUDIT at the intercept represented effects at 12-mo follow-up. At the 12-mo follow-up, AUDIT scores did not significantly predict BSI scores (p = .88). Time was then recoded so that the intercept represented effects at 18-mo. At the 18-mo follow-up, higher baseline AUDIT scores were associated with higher BSI scores, but the finding did not attain statistical significance, b = .13, t (770) = 1.94, p = .053.
Secondary analyses with the dichotomous alcohol problem variable were largely similar, with one important difference: The alcohol problem x Time interaction was not significant (p = .45). Thus, a model was run without Time to examine the main effect of the presence of an alcohol problem on BSI scores. The presence of an alcohol problem did not affect BSI outcomes (p = .60).
ASI
Employment status and baseline ASI scores were covariates significantly associated with outcome and were retained in all models including ASI as the DV. There was no effect of Time in the interaction model (i.e., no AUDIT x Group x Time interaction, p = .55). Time was thus removed from the model to examine the AUDIT x Group interaction. There was no significant moderating effect (AUDIT x Group interaction; p = .67).
Simplified models examining the main effect of AUDIT on ASI outcomes were conducted. No significant AUDIT x Time interaction was observed (p = .16), indicating that the effect of AUDIT on ASI did not change from 12 to 18-mo. Thus, Time was removed from the model and a simplified model with only the main effect terms was conducted. There was no effect of AUDIT score on ASI outcomes (p = .78). As expected, a main effect of intervention status was observed, b = −4.74, t (771) = −6.36, p < .001, with CALM outperforming UC.
The secondary analyses examining the effects of problem alcohol use v. no problem alcohol use were identical to the findings with the continuous AUDIT scores as the predictor.
PHQ
Number of medical conditions, the presence of social phobia, and baseline PHQ scores were the covariates in the first model that were significantly associated with PHQ outcomes and were thus retained in all models with PHQ as the DV. Identical to findings described for BSI and ASI, there was no significant AUDIT x Group x Time interaction (p = .46). A model removing Time and collapsing across the 12 and 18-mo follow-up periods found no significant AUDIT x Treatment Group interaction (p = .13). Simplified models were then conducted to examine main effects by excluding the interaction term. There was no significant Time x AUDIT interaction (p = .17), indicating that the effect of AUDIT on PHQ outcomes did not change over time. Thus, main effects were examined without Time in the model. There was no main effect of AUDIT score on PHQ outcomes (p = .19) and there was a significant effect of intervention, b = −2.06, t (770) = −6.11, p < .001, with CALM outperforming UC.
Some differences emerged when using the dichotomous alcohol problems variable as a predictor of PHQ outcomes. Neither a Time x Group x Alcohol Problems interaction nor Group x Alcohol Problems interaction emerged (ps > .21). However, there was a significant Time x Alcohol Problems interaction, b = 1.21, t (673) = 2.15, p < .05, indicating that the prognostic, main effect of alcohol problems on PHQ changed over the follow-up period. Thus, main effects of alcohol problems were examined cross-sectionally at 12 and 18-mo follow-ups. There was no significant effect of alcohol problems on PHQ outcomes at 12-mo follow-up (p = .99). In contrast, the presence of an alcohol problem at baseline was associated with higher PHQ scores at the 18-mo follow-up, b = 1.20, t (770) = 1.98, p < .05.
Discussion
This study examined whether AUS either moderated anxiety disorder treatment outcomes or predicted anxiety disorder outcomes regardless of treatment. No moderating effects were observed, indicating that the presence or degree of alcohol problems did not predict outcome differentially between the CALM intervention and usual care. Moreover, the majority of analyses revealed no general prognostic effects of alcohol use severity on outcomes. Importantly, as already reported elsewhere (27), CALM outperformed usual care robustly on all outcomes, regardless of alcohol use. These data largely suggest that alcohol problems minimally influence the nature or direction of the effects of evidence-based care for anxiety disorder (or usual care) on anxiety and depression.
A few exceptions to the overall findings were observed: By the 18-mo follow-up, there were general prognostic effects of alcohol use severity on anxiety and depression symptoms across both conditions. Regardless of the intervention, individuals being treated in primary care (either with or without evidence-based, focused treatment for anxiety disorders) who had both alcohol and anxiety problems showed trends for higher anxiety and higher depression scores on some outcome measures at the long-term assessment.
These findings indicate that, contrary to popular clinical practice, it may be unnecessary to postpone treatment for an anxiety disorder until an alcohol problem has been treated, particularly in patients whose alcohol problems do not reach the criteria for alcohol dependence, as seen in this sample. Mounting evidence suggests that the high comorbidity between anxiety and alcohol use disorders can be explained in many cases by the self-medication hypothesis that individuals who use alcohol (or other drugs) to cope with negative affect (e.g., anxiety) may develop substance use problems (47–50). Providing treatment for the underlying negative affect may prevent alcohol problems from persisting and worsening. This is an area of growing research attention, which has led to the development of models aiming to treat alcohol and anxiety concurrently (20–22). Still, ongoing efforts have focused on providing joint treatment to patients primarily seen as alcohol patients in alcohol treatment settings. Almost no research to our knowledge has focused on bringing alcohol treatment to patients presenting with anxiety disorders in primary care, psychiatric, or other clinical settings who have comorbid alcohol problems. The current findings suggest that anxiety treatment works similarly whether an individual has alcohol problems or not (with some longer-term exceptions indicating somewhat higher anxiety and depression). A remaining question is whether the addition of integrated alcohol treatment among those who seek treatment for anxiety disorders may improve those long-term anxiety and depression outcomes (in addition to improving alcohol use severity). This area of future research has direct clinical and organizational/systems implications.
Despite these robust findings with a large sample, caution is needed in interpreting findings that do not reject a null hypothesis. Even with a large sample, it is possible that the study lacked sufficient power to detect small effects. A significant limitation of the study was the exclusion of patients with substance dependence. Findings may have differed if more patients with severe alcohol problems were included. Possibly, the CALM intervention would not have been as beneficial to those with alcohol dependence as it was for those without alcohol dependence. It is possible that the discrepancy between these findings and previous work is due to the inclusion of alcohol dependence in other studies (9), a methodological difference that precludes direct comparisons. However, it is important to note that patient responses to our dimensional measure of alcohol problems ranged from no to severe alcohol problems. Thus, even if patients did not meet full diagnostic criteria for alcohol dependence using DSM-IV criteria, there were some patients represented in this sample who experienced severe alcohol problems (albeit few compared to those with no or mild to moderate alcohol problems). Future research should examine whether these findings can be replicated with an anxiety disorder sample receiving evidence-based treatment for anxiety disorders in primary care when including those with alcohol dependence. Given that problems with alcohol were not directly addressed in this intervention, if a study that includes those with alcohol dependence does not produce similar results this may suggest that individuals with comorbid anxiety and alcohol dependence in primary care may benefit from integrated evidence-based treatment for both problems. Taken together, this study indicates that typical alcohol problems seen in primary care populations do not appear to negatively affect evidence-based treatment for anxiety disorders.
Acknowledgments
This work was supported by the following National Institute of Mental Health grants: U01 MH070018, U01 MH058915, U01 MH057835, UO1 MH057858, U01 MH070022, K24 MH64122, and K24 MH065324.
References
- 1.Fals-Stewart W, Angarano K. Obsessive-Compulsive Disorder Among Patients Entering Substance Abuse Treatment: Prevalence and Accuracy of Diagnosis. Journal of Nervous & Mental Disease. 1994;182:715–9. doi: 10.1097/00005053-199412000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addictive Behaviors. 1999;13:115–22. [Google Scholar]
- 3.Bakken K, Landheim AS, Vaglum P. Substance-dependent patients with and without social anxiety disorder: Occurrence and clinical differences: A study of a consecutive sample of alcohol-dependent and poly-substance-dependent patients treated in two counties in Norway. Drug and Alcohol Dependence. 2005;80:321–8. doi: 10.1016/j.drugalcdep.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 4.McGovern MP, Xie H, Segal SR, Siembab L, Drake RE. Addiction treatment services and co-occurring disorders: Prevalence estimates, treatment practices, and barriers. Journal of Substance Abuse Treatment. 2006;31:267–75. doi: 10.1016/j.jsat.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Bakken K, Landheim AS, Vaglum P. Axis I and II disorders as long-term predictors of mental distress: a six-year prospective follow-up of substance-dependent patients. BMC Psychiatry. 2007:7. doi: 10.1186/1471-244X-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith JP, Book SW. Comorbidity of Generalized Anxiety Disorder and Alcohol Use Disorders among Individuals Seeking Outpatient Substance Abuse Treatment. Addictive Behavior. 2010;35:42–5. doi: 10.1016/j.addbeh.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolitzky-Taylor K, Operskalski J, Ries R, Craske MG, Roy-Byrne P. Understanding and Treating Comorbid Anxiety Disorders in Substance Users: Review and Future Directions. Journal of Addiction Medicine. 2011;5:233–47. doi: 10.1097/ADM.0b013e31823276d7. [DOI] [PubMed] [Google Scholar]
- 8.Otto MW, Pollack MH, Sachs GS, O’Neil CA, Rosenbaum JF. Alchohol dependence in panic disorder patients. Journal of Psychiatric Research. 1992;26:29–38. doi: 10.1016/0022-3956(92)90013-e. [DOI] [PubMed] [Google Scholar]
- 9.Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, et al. Influence of Psychiatric Comorbidity on Recovery and Recurrence in Generalized Anxiety Disorder, Social Phobia, and Panic Disoder: A 12-Year Prospective Study. American Journal of Psychiatry. 2005;162:1179–87. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 11.Reid MC, Fiellin DA, O’Connor PG. Hazardous and Harmful Alcohol Consumption in Primary Car. The Journal of the American Medical Association Internal Medicine. 1999;159:1681–9. doi: 10.1001/archinte.159.15.1681. [DOI] [PubMed] [Google Scholar]
- 12.Volk RJC, SB, Steinbauer JR, Cass AR. Alcohol Use Disorders, Consumption Patterns, and Health-Related Quality of Life in Primary Care Patients Alcoholism. Clinical and Experimental Research. 1997;21:899–905. [PubMed] [Google Scholar]
- 13.Adams WL, Barry KL, Fleming MF. Screening for Problem Drinking in Older Primary Care Patients. The Journal of American Medical Association. 1996;68:378–88. [PubMed] [Google Scholar]
- 14.Hilton ME. Drinking Patterns and Drinking Problems in 1984: Results from a General Population Survey. Alcoholism: Clinical and Experimental Research. 1987;11:167–75. doi: 10.1111/j.1530-0277.1987.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 15.Archer L, Grant BF, Dawson DA. What if Americans drank less? The Potential Effect on the Prevalence of Alcohol Abuse and Dependence. American Journal of Public Health. 1995;85:61–6. doi: 10.2105/ajph.85.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hingson RW, Zha W. Age of Drinking Onset, Alcohol Use Disorders, Frequent Heavy Drinking, and Unintentionally Injurying Oneself and Others after Drinking. Pediatrics. 2009;123:1477–84. doi: 10.1542/peds.2008-2176. [DOI] [PubMed] [Google Scholar]
- 17.Havassy BE, Alvidrez J, Mericle AA. Disparities in Use of Mental Health and Substance Abuse Services by Persons with Co-occurring Disorders. Psychiatric Services. 2009;60:217–23. doi: 10.1176/appi.ps.60.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ziedonis DM. Integrated treatment of co-occurring mental illness and addiction: clinical intervention, program, and system perspectives. CNS spectrums. 2004;9:892–904. doi: 10.1017/s1092852900009718. [DOI] [PubMed] [Google Scholar]
- 19.Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT) Substance Abuse. 2007;3:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 20.Stewart SH, Conrod P. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York, NY: Springer; 2008. [Google Scholar]
- 21.Najavits LM. Seeking Safety: Therapy for Trauma and Substance Abuse. Corrections Today. 2002;64:136–41. [Google Scholar]
- 22.Kushner M, Donahue C, Sletten S, Thuras P, Abrams K, Peterson J, et al. Cognitive behavioral treatment of comorbid anxiety disorder in alcoholism treatment patients: Presentation of a prototype program and future directions. Journal of Mental Health. 2006;15:697–707. [Google Scholar]
- 23.Barry CL, Huskamp HA. Moving beyond Parity — Mental Health and Addiction Care under the ACA. The New England Journal of Medicine. 2011;365:973–5. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pating DR, Miller MM, Goplerud E, Martin J, Ziedonis DM. New systems of care for substance use disorders: Treatment, finance, and technology under health care reform. Psychiatric Clinics of North America. 2012;35:327–56. doi: 10.1016/j.psc.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Patient Protection and Affordable Care Act, (March 23, 2010, 2010).
- 26.Norman SB, Cissell SH, Means-Christensen AJ, Stein MB. Development and validation of an Overall Anxiety Severity And Impairment Scale (OASIS) Depression and Anxiety. 2006;12:245–9. doi: 10.1002/da.20182. [DOI] [PubMed] [Google Scholar]
- 27.Roy-Byrne P, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, et al. Delivery of Evidence-Based Treatment for Multiple Anxiety Disorders in Primary Care. The Journal of the American Medical Association. 2010;303(19):1921–8. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheehan DV, Lecrubier Y, KHS, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structures diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Supplement 20):22–33. [PubMed] [Google Scholar]
- 29.Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R, Patient Edition/Non-patient Edition (SCID-P/SCID-NP) Washington, DC: American Psychiatric Press, Inc; 1990. [Google Scholar]
- 30.Sheehan DV, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–41. [Google Scholar]
- 31.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2. Geneva, Switzerland: World Health Organization: Department of Mental Health and Substance Dependence; 2001. [Google Scholar]
- 32.Gache P, Michaaud P, Landry U, Accietto C, Arfaoui S, Wenger O, et al. The Alcohol Use Disorders Identification Test (AUDIT) as a Screening Tool for Excessive Drinking in Primary Care: Reliability and Validity of a French Version. Alcoholism: Clinical and Experimental Research. 2005;29:2001–7. doi: 10.1097/01.alc.0000187034.58955.64. [DOI] [PubMed] [Google Scholar]
- 33.Dybek I, Bischof GJG, Reinhardt S, Meyer C, Hapke U, et al. The Reliability and Validity of the Alcohol Use Disorders Identification Test (AUDIT) in a German General Practice Population Sample. Journal of Studies on Alcohol. 2006;67:473–81. doi: 10.15288/jsa.2006.67.473. [DOI] [PubMed] [Google Scholar]
- 34.Derogatis LR. BSI Brief Symptom Inventory: Administration, Scoring, and Procedure Manual. 4. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 35.Derogatis LR. Symptom Checklist-90-R (SCL-90-R): Administration, scoring, and procedures manual. Minneapolis, MN: NCS; 1994. [Google Scholar]
- 36.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- 37.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behavior research and therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 38.Smits JA, Powers MBCY, Telch MJ. Mechanism of change in cognitive-behavioral treatment of panic disorder: evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology. 2004;72:646–52. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- 39.Peterson RA, Heilbronner RL. The anxiety sensitivity index: Construct validity and factor analytic structure. Journal of Anxiety Disorders. 1987;1:117–21. [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:601–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raudenbush SW, Bryk AS, Congdon R. HLM 6 for Windows. Skokie, IL: Scientific Software International, Inc; 2004. [Google Scholar]
- 42.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, CA: SAGE Publications; 1991. [Google Scholar]
- 43.Wolitzky-Taylor K, Arch JJ, Rosenfield D, Craske MG. Moderators and non-specific predictors of treatment outcome for anxiety disorders: A comparison of cognitive behavioral therapy to acceptance and commitment therapy. Journal of Consulting and Clinical Psychology. 2012;80:786–99. doi: 10.1037/a0029418. [DOI] [PubMed] [Google Scholar]
- 44.Arch JJ, Ayers CR. Which treatment worked better for whom? Moderators of group cognitive behavioral therapy versus adapted mindfulness based stress reduction for anxiety disorders. Behaviour Research and Therapy. 2013;51:434–42. doi: 10.1016/j.brat.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 45.Smits JA, Rosenfield D, Otto MW, Powers MB, Hofmann SG, Telch MJ, et al. D-Cycloserine Enhancement of Fear Extinction is Specific to Successful Exposure Sessions: Evidence from the Treatment of Height Phobia. Biological Psychiatry. 2013;73:1054–8. doi: 10.1016/j.biopsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Kleine RA, Hendriks G, Smits JAJ, Broekman TG, van Minnen A. Prescriptive variables for d-cycloserine augmentation of exposure therapy for posttraumatic stress disorder. Journal of Psychiatric Research. 2014;48:40–6. doi: 10.1016/j.jpsychires.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 47.Conger JJ. Alcoholism: Theory, Problem and Challenge: Reinforcement theory and the Dynamics of Alcoholism. Quarterly Journal of Studies on Alcohol. 1956;13:296–305. [PubMed] [Google Scholar]
- 48.Khantzian EJ. The Self-Medication Hypothesis of Addictive Disorders: Focus on Heroin and Cocaine Dependence. American Journal of Psychiatry. 1985;142:1259–64. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- 49.Greeley J, Oei T. In: Alcohol and Tension Reduction. Leonard KE, Blane HT, editors. New York, NY: Guilford Press; 1999. [Google Scholar]
- 50.Kushner M, Krueger R, Frye B, Peterson J. Epidemiological Perspectives on Co-Occurring Anxiety Disorder and Substance Use Disorder. In: Stewart AL, Conrod PJ, editors. Anxiety and Substance Use Disorders. New York, NY: Springer Publisher; 2008. [Google Scholar]