Abstract
Introduction
Families of children with Autism Spectrum Disorder (ASD) endure significant financial and employment burden due to their children's numerous needed services. The study objective is to describe additional impact on families of children with intellectual disability (ID) in addition to ASD.
Methods
The study is a secondary data analysis of the 2009-2010 National Survey of Children with Special Health Care Needs. Children whose parents answered “yes” when asked if their child had ASD or ID were classified as having ASD alone (unweighted n=2406), ID alone (unweighted n=1363), or both ASD/ID (unweighted n=620). Bivariate and multivariate analyses compared study outcomes of family financial and caregiver burden using ASD as the reference group. All analyses were weighted using person-level estimates.
Results
Of children with ASD, 24% also had ID. Over half of caregivers of children with ASD/ID reported financial difficulty (52%) and having to stop work to care for their child (51%). Compared to ASD alone, caregivers of children with both ASD/ID were more likely to report financial difficulty (aOR 1.65, 95% CI 1.10-2.46), cutting work hours (aOR 1.43, 95% CI .98-2.08), and stop working (aOR 2.32, 95% CI 1.57-3.43). No differences were found between caregivers of children with ASD only and ID only.
Conclusions
We conclude that having ID in addition to ASD may be associated with greater negative impact on family financial and employment burden. Recognition of ID in addition to ASD is important to tailor the clinical approach and sufficiently support families.
Keywords: Autism Spectrum Disorder, intellectual disability, financial, caregiver burden
Introduction
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by (1) persistent deficits in social communication and social interaction across multiple contexts and (2) restricted and repetitive patterns of behavior, interests, and activities (American Psychiatric Association, 2013). The prevalence of ASD is thought to have steadily increased, from one in 2000 children between 1960 and 1980, to one in 68 in 2010 (Autism and Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators, 2014; Kogan, Blumberg, Schieve, Boyle, Perrin, et al., 2009). ASD impacts children's learning, social skills, communication, and behavior. This often requires children to need special education and related support services, raises the stress level of those caring for them, and increases financial burden on the family (Järbrink, Fombonne, Knapp, 2003; Montes and Halterman, 2008; Mugno, Ruta, D'Arrigo, Mazzone, 2007; Xiong, Yang, Yu, Hou, Li, et al., 2011).
A significant subset with ASD also has intellectual disability (ID) (US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau, 2013). ID, previously called mental retardation, is characterized by significant limitations in cognitive functioning and adaptive behavior and is defined as “a disorder with the onset during the developmental period that includes both intellectual and adaptive functioning deficits in conceptual, social and practical domains” (American Psychiatric Association, 2013). ASD and ID can present similarly, as children with either disorder may demonstrate difficulty with communication, social skills, and behavior (Johnson and Walker, 2006). If appropriately supported, children with ASD only may be able to participate in regular education classes with their peers, while a child with both ASD/ID requires a higher level of support. Between 30 and 60% of children with ASD also have ID (Schieve, Baio, Rice, Durkin, Kirby, et al., 2010).
Caregivers of children with ASD may experience significant financial and employment burden compared to caregivers of children with special health care needs who do not have ASD (Kogan, Strickland, Blumberg, Singh, Perrin, et al., 2008). The cost of caring for a person with ASD during his or her lifetime has been estimated to be $1.4 million in the United States (Buescher, Cidav, Knapp, Mandell, 2014). Mothers of children with ASD earned significantly less than mothers of children with other health limitations, were less likely to be employed, and that those who were employed worked fewer hours per week when compared to mothers of children with no health limitations (Cidav, Marcus, Mandell, 2012).
Preliminary research suggests that the coexistence of ASD and ID may be important to recognize because of the heightened family financial and employment burden due to managing multiple conditions. While Brown, Ouelette-Kuntz, Hunter, Kelley, and Cobigo's (2010) study suggested this finding in children ages 6-13 years old from 5 study regions in Canada, this finding has not been described on a broader scale. A better understanding of the scale of potential additional family burden in the setting of a concomitant ASD and ID may tailor our clinical approach and inform policy recommendations to achieve best developmental outcomes. With this study, we utilize a nationally representative data set to 1) describe the level of financial and employment burden for families of children who have autism and 2) examine how family financial and employment burden may vary with different levels of intellectual functioning.
Methods
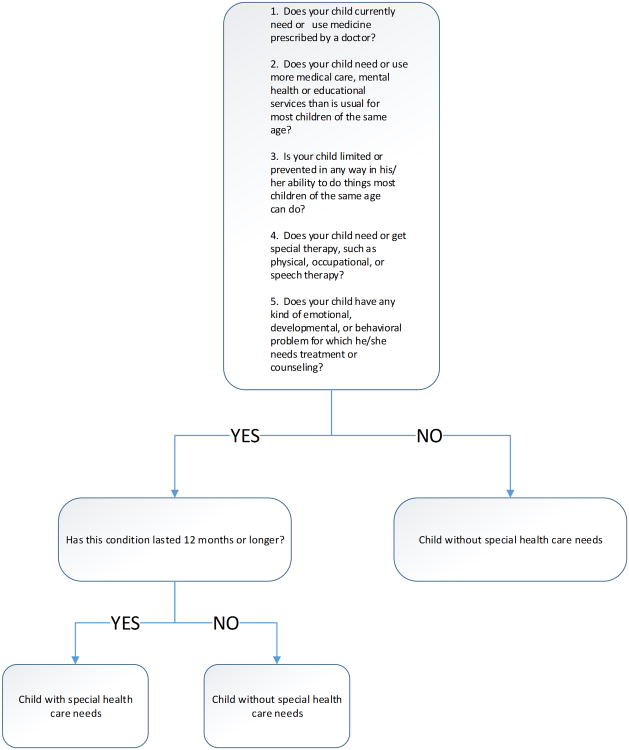
This study is a secondary analysis of the 2009-10 National Survey of Children with Special Health Care Needs (NS-CSHCN), a telephone survey of parents of a national random sample of non-institutionalized CSHCN in the United States. A total of 372,698 children in 196,159 households were screened for special health care needs using a health care needs screener developed using the Maternal and Child Health Bureau definition of CSHCN (Bethell, Read, Stein, Blumberg, Wells, et al., 2002). Five screening questions addressed medication use, need for medical and educational services, limits on the child's ability, need for various therapy services, and the presence of developmental or behavioral problems (Figure 1).
Figure 1. Special Health Care Needs Screener.
Children were regarded as having special needs if they were positive for at least one of the screening questions due to a condition lasting at least 12 months. One child with special health care needs was randomly selected from each CSHCN-reporting household to be the target child for the interview. This resulted in 40,242 household interviews, with at least 750 interviews conducted in each state and the District of Columbia. Each interview covered a range of topics addressing health care services and quality of life of the child and family, such as the child's health and functional status, access to care, and access to community-based services.
The overall weighted response rate was 25.5%, which reflects the proportion of completed interviews based on calculations of eligible sampling units due to nonresponse at various stages of screening for eligibility. However, for study subjects that completed the screening process and began the interview, the interview completion rate was 80.8%. Informed consent was obtained from all survey participants. Because the survey data is publically available and does not contain identifiers, use of this data set for research was determined to be exempt from review by our Institutional Review Board.
Study Population
All study respondents were asked if their child had any of 20 non-mutually exclusive health conditions. Children were included for further analyses if they had at least one of three reported conditions: ASD, ID, or asthma. Children with ASD were self-identified by their parents when asked about Autism, Asperger's Disorder, pervasive developmental disorder, or other autism spectrum disorder. ID was identified by parents asked about the presence of intellectual disability or mental retardation. Severity was assessed by parent report.
Asthma was identified based on positive parental response. We included asthma in our analyses to illustrate the significant difference with regard to the nature, impairment, and treatment of neurodevelopmental versus non-neurodevelopmental conditions. We chose to use asthma due to the high prevalence of this condition and the relatively low level of severity in most children. Study subjects were then classified as having ASD only, ID only, both ASD/ID or asthma.
Study Variables
Family financial burden was examined by families reporting that they accrued out-of-pocket costs (dichotomized at $1000 for their child's medical care in the last 12 months) and had any financial difficulty in the last 12 months. Family employment burden was measured by whether the study respondent reported a family member stopped working or cut work hours due to the child's health. The number of hours spent on care coordination and hours per week devoted to providing care for the child by a family member were measured. Some continuous variables were dichotomized at the median for use in logistic regression analyses. Demographic variables examined to control for confounding relationships were gender, ethnicity, family income, health insurance coverage and type of health insurance.
Statistical Analyses
We performed descriptive analyses to examine the total number of children with ASD only, ID only, both ASD/ID, and asthma. Bivariate associations with demographic variables were examined by chi-square among children with either ASD only, ID only, and ASD/ID. Tests of significance were calculated for study subjects exclusive of asthma to examine the relationship between having ASD, ID, and ASD/ID together. We conducted chi-square for categorical variables, median non-parametric tests for skewed continuous variables, and logistic and multivariate logistic regression analyses adjusting for significant demographics at the <.05 level. The reference group in regression analyses was ASD alone. Additional analyses by chi-square were conducted to examine whether increasing severity of ASD, ID, or ASD/ID together was associated with an increased level of family financial and caregiver burden. Asthma was included in the logistic regression models as a comparison group to illustrate the relative burden of a relatively low-impact condition. All variables were forced in. Unless otherwise indicated, all analyses were weighted using person-level estimates to account for the complex sampling design. Analyses were conducted using STATA 11.0.
Results
There were 40242 (unweighted) US children in the 2009-10 NS-CSHCN. Among those children, 2406 had ASD only, 1363 had ID only and 620 had both ASD/ID; 12121 had asthma without ASD or ID. Of all CSHCN nationally, 5.7% (weighted) had ASD only, 3.7% had ID only, 1.8% had ASD/ID together, and 30.1% had asthma exclusive of ASD or ID. Of children with ASD, 23.6% (weighted) also had ID.
Demographics for the study sample can be found in Table 1. Children with ASD only were more likely to be male (81.6%) compared to children with ID only (58.1%) (p<.001). Children with ASD only were more likely to be White (66.1%) compared to ID only (52.9%) and ASD/ID combined (51.7%) (p<.001). Children with ASD only were more likely to have family income at or greater than 400% federal poverty level (FPL) (29.1%) compared to children with ID only (21.3%) and ASD/ID combined (21.2%) (p<.05). Children with ASD were more likely to have private or combined insurance (67.8%) compared to ID only (51.1%) and ASD/ID combined (55.0%) (p<.001). No additional demographic associations were seen between children with ASD alone or ID alone.
Table 1. Demographics of the Study Subjects.
| Variable | Autism Spectrum Disorder (ASD) only | Intellectual Disability (ID) only | ASD with ID | p-value | asthma |
|---|---|---|---|---|---|
| N (unweighted) | 2406 | 1363 | 620 | 12121 | |
| Child age | |||||
| 0-5 years | 19.9% | 13.5% | 12.4% | <.001 | 20.0% |
| 6-11 years | 46.9% | 35.5% | 45.0% | 41.6% | |
| 12-17 years | 33.3% | 51.1% | 42.7% | 38.4% | |
| Child gender | |||||
| Male | 81.6% | 58.1% | 77.6% | <.001 | 59.2% |
| Female | 18.4% | 42.9% | 22.4% | 37.2% | |
| Child ethnicity | |||||
| Non-Hispanic White | 66.1% | 52.9% | 51.7% | <.001 | 50.4% |
| Non-Hispanic Black | 9.4% | 18.2% | 13.5% | 23.0% | |
| Hispanic | 16.4% | 22.6% | 16.7% | 17.7% | |
| Other/Mixed race | 8.1% | 6.3% | 18.1% | 8.9% | |
| Family income | |||||
| 0-99% FPL* | 17.9% | 27.0% | 21.1% | <.05 | 24.6% |
| 100-199% FPL | 20.8% | 26.2% | 22.8% | 21.8% | |
| 200-299% FPL | 17.3% | 16.6% | 18.1% | 15.9% | |
| 300-399% FPL | 14.9% | 8.9% | 16.9% | 12.6% | |
| 400%+ FPL | 29.1% | 21.3% | 21.2% | 25.2% | |
| *Federal poverty level | |||||
| Health insurance coverage | |||||
| Insured full year* | 91.9% | 88.2% | 91.8% | .29 | 89.9% |
| Ever uninsured during year | 8.1% | 11.8% | 8.3% | 10.1% | |
| *Year = past 12 months before the survey | |||||
| Type of health insurance | |||||
| Private/combined | 67.8% | 51.1% | 55.0% | <.001 | 59.9% |
| Public only | 29.5% | 46.2% | 42.4% | 36.1% | |
| Uninsured | 2.7% | 2.7% | 2.6% | 4.0% |
NOTE: Percents are columns. All figures weighted unless otherwise indicated. P value by chi square comparing ASD, ID, and ASD versus ID only.
Study outcomes for family financial difficulties are reported in Table 2. About one-third of caregivers of children with ASD only (34.1%) and ASD/ID (31.3%) reported paying at least $1000 in annual out-of-pocket costs. By comparison, 21.5% of caregivers of children with ID and 18.7% of caregivers of children with asthma reported paying at least $1000 in annual out-of-pocket costs. Neither ID nor ASD/ID combined was associated with higher out-of-pocket costs compared to ASD. Over half (52.0%) of caregivers of children with ASD/ID reported financial difficulty. Compared to caregivers of children with ASD only, caregivers of children with both ASD/ID were more likely to report having financial difficulty (aOR 1.65, 95%CI 1.10-2.46). No association with financial difficulty was noted for children with ID only (35.6%; aOR .88, 95% CI .63-1.21) compared to ASD only (40.1%). Only 18.1% of caregivers of children with asthma reported having financial difficulty.
Table 2. Association of ID with Family Financial Burden.
| Study Group | >$1000 out of pocket costs | OR | aOR | Family experience financial difficulty | OR | aOR |
|---|---|---|---|---|---|---|
| ASD only | 34.1% | Ref | Ref | 40.1% | Ref | Ref |
| ID only | 21.5% | .53 (.41-.70) | .66 (.49-.89) | 35.6% | .83 (.61-1.11) | .88 (.63-1.21) |
| ASD with ID | 31.3% | .88 (.62-1.26) | 1.10 (.70-1.72) | 52.0% | 1.62 (1.13-2.32) | 1.65 (1.10-2.46) |
| Asthma with no other condition | 18.7% | .45 (.38-.52) | .48 (.40-.58) | 18.1% | .33 (.28-.39) | .33 (.28-.40) |
All figures weighted. Analyses controlled for age group, gender, race/ethnicity, income level, and type of insurance at time of interview.
Hours spent on care coordination and home care can be found in Table 3. Caregivers of children with ASD/ID combined and ID only reported a median of 2 hours a week providing care coordination, compared to a median of 1 for the other two groups (p<.001). Over half of caregivers of children with ID, ASD/ID, and asthma reported that a family member provided any kind of home health care in the past 12 months. Of those caregivers that reported providing home health care, ASD/ID was associated with the highest median hours per week (11), compared to ID only (7), ASD only (5), and asthma (1).
Table 3. Hours Spent on Care Coordination and Home Care.
| Study Group | Median # hours providing care coordination | Dichotomized at 1 hour, OR | Dichotomized at 1 hour, AOR | % reporting provided home care | If provided home care: median hours | Home care, dichotomized at 2 hours, OR | Home care, dichotomized at 2 hours, AOR |
|---|---|---|---|---|---|---|---|
| ASD only | 1 | Ref | Ref | 48.9% | 5 | Ref | Ref |
| ID only | 2 | 1.20 (.90-1.59) | 1.04 (.76-1.43) | 62.7% | 7 | 1.16 (.77-1.77) | 1.11 (.65-1.88) |
| ASD with ID | 2 | 1.68 (1.03-2.74) | 1.46 (.90-2.37) | 66.6% | 11 | 2.43 (1.53-3.86) | 2.36 (1.40-3.99) |
| Asthma with no other condition | 1 | .38 (.32-.45) | .32 (.26-.38) | 61.5% | 1 | .32 (.25-.40) | .26 (.21-.33) |
All figures weighted. Analyses controlled for age group, gender, race/ethnicity, income level, and type of insurance at time of interview.
Caregiver burden findings are reported in Table 4. Compared to caregivers of children with ASD only, caregivers of children with both ASD/ID were more likely to stop working to care for their child (51.1%; aOR 2.32, 95% CI 1.57-3.43). No such relationship with children with ID only (34.5%; aOR .89, 95%CI .64-1.23) compared to ASD only (36.8%) was noted for cutting work hours. Moreover, no relationship for having to stop working was noted for children with ID only (35.3%; aOR 1.04, 95%CI .76-1.43) compared to ASD only (34.1%). Among caregivers of children with asthma, the need for cutting work hours (13.8%; aOR .26, 95%CI .22-.31) and to stop working (12.4%, aOR .26, 95%CI .21-.31) was significantly less than the other three groups. No associations were noted in any study outcomes for children who had different levels of severity of ASD, ID, or ASD/ID with both diagnostic categories of outcomes.
Table 4. Association of ID with Caregiver Burden.
| Study Group | Caregiver cut work hours to care for child (unweighted N=18770) | OR | aOR | Caregiver stopped working to care for child (N=18779) | OR | aOR |
|---|---|---|---|---|---|---|
| ASD only | 36.8% | Ref | Ref | 34.1% | Ref | Ref |
| ID only | 34.5% | .90 (.66-1.23) | .89 (.64-1.23) | 35.3% | 1.06 (.80-1.39) | 1.04 (.76-1.43) |
| ASD with ID | 44.4% | 1.37 (.94-2.00) | 1.43 (.98-2.08) | 51.1% | 2.02 (1.40-2.91) | 2.32 (1.57-3.43) |
| Asthma with no other condition | 13.8% | .27 (.23-.33) | .26 (.22-.31) | 12.4% | .27 (.23-.33) | .26 (.21-.31) |
All figures weighted. Analyses controlled for age group, gender, race/ethnicity, income level, and type of insurance at time of interview.
Discussion
Children with both ASD/ID have a greater negative impact on the family's financial and employment burden compared to children who have ASD alone. Of study respondents, almost one-third of caregivers of children with both ASD/ID reported having at least $1000 out of pocket costs to provide care for their children. Over half of caregivers reported having financial difficulty and having to stop work to care for their child within the twelve months prior to the study. By comparison, just over one-third of caregivers of children with ASD only and ID only reported the latter burdens.
To our knowledge this is the first study that describes on a national level how the co-existence of ASD and ID is associated with both a substantially greater negative impact on family stress and economics. Our finding is consistent with literature suggesting the coexistence of ID with mental health and developmental diagnoses increases the financial and employment burden felt by families. A recent study by Ouyang, Grosse, Riley, Bolen, Bishop, et al. (2014) found that families of children with fragile X syndrome and ID had higher financial and employment burden than those who had fragile X without ID. A study regarding ID and co-existing mental disorders indicated that ID co-existing with a mental disorder causes higher levels of family burden than ID alone (Irazábal, Marsá, García, Gutiérrez-Recacha, Martorell, et al., 2012). Caregivers of children with neurodevelopmental disorders may exhibit a greater number of health and psychosocial problems, which may contribute to this burden (Lach, L.M., Kohen, D.E., Garner, R.E., Brehaut, J.C., Miller, A.R., et al., 2009).
Caregivers of children with ASD and ID alone reported similar rates of financial difficulty, having to stop working altogether, and cutting work hours if continuing to work. Similarities in family burden were found despite the two groups having substantially different overall demographic profiles. We also note that children in the ASD only group tended to be more advantaged demographically, which could explain why children with ID and ASD/ID appeared to have higher family burden and why caregivers in the ASD only group did not view the high out of pocket costs as causing financial hardship for the family. Our study found that caregivers of children with ASD/ID together had the highest reported prevalence of financial difficulty despite having similar out-of-pocket costs to ASD and ID alone. These findings persisted in both adjusted and unadjusted analyses and after controlling for gender, ethnicity, family income, and type of health insurance.
There may be other unmeasured variables that contribute to family burden such as genetic diagnoses, medical complexity, and SES/demographic variables that are associated with ID and may contribute to increased family burden (Kuo, Cohen, Agrawal, Berry, and Casey, 2011). Although different levels of ASD and ID individually did not show significant increase in family burden, we suggest that it remains important for clinicians to be aware that the co-morbidity of ID with ASD may be particularly burdensome to families.
Our findings are striking for the overall burden associated with the presence of ASD and ID, either independently or together, when compared to asthma. We found that caregivers of children with asthma and no other condition were less likely to report high out of pocket costs to provide care for their child. In fact, less than one-fifth of caregivers of children with asthma reported out of pocket costs of $1000 or more, and almost half of such caregivers reported out of pocket costs less than $250 for the year prior to the study [data not shown]. Few caregivers of children with asthma reported having financial difficulty in the 12 months prior to being surveyed. There is likely variation in the severity of health needs within the asthma group, and we did not examine the asthma subgroup further for presence of additional medical complexity. Nevertheless, substantial family burden with asthma appears to be the exception rather than the rule.
We found that about one-fourth of children with ASD also have ID. This is comparable to the rate of co-existence found by Peacock, Amendah, Ouyang, and Gross (2012) but is less than some previous studies have reported (Mandell, Novak, Zubritsky, 2005). This finding may be an underestimate, as it is possible some children with ASD have not had ID properly diagnosed. The question regarding ID diagnosis in the 2009-10 NS-CSHCN may also be more specific and less sensitive than prior surveys. In the 2005-06 NS-CSHCN, for example, survey respondents were asked whether the child had “mental retardation or developmental delay,” while the 2009-10 respondents were asked for the presence of “intellectual disability or mental retardation.” Another reason for the lower prevalence is diagnostic substitution, where children with ID are now being classified as having another diagnosis (Shattuck, 2006). These findings may have resulted in the remaining children with ID having a particularly severe form, which could have exaggerated our study findings of increased burden in the presence of ID. However, at a minimum, a substantial proportion of children with ASD continue to have ID.
Consideration should be given to thoroughly screen for the existence of ID at the time of diagnosis of ASD, and vice versa, because of the potential additive stressors on the family. The substantial proportion of concomitant diagnoses means that regularly screening for ID when a diagnosis of ASD is made will frequently result in a positive screen. The routine use of an abbreviated IQ measure and measure of adaptive functioning may allow the clinician to know if further cognitive assessment is warranted. These assessments can be performed by early intervention providers, school psychologists/psychometrists, or other appropriately trained clinicians and should be added to diagnostic/assessment protocols used by all early intervention, public school, and medical specialty providers. Medical providers evaluating children during well-child visits should be screening for developmental delays and ASD as per the American Academy of Pediatrics guidelines and should refer any child with a positive screen to one of the providers mentioned above for further evaluation (American Academy of Pediatrics, 2006; Johnson and Myers, 2007).
Our findings support the importance of recognizing the presence of ID in addition to ASD, as this can help tailor the clinical approach and better support families. If properly identified, families of children with both ASD/ID can be counseled regarding resources available to help with care of their children. Available resources such as supplemental Medicaid and home and community waiver services can be based on specific diagnoses, and when children have multiple diagnoses, such as ASD/ID, they are more likely to receive the appropriate services. It has been noted that children with existing special health care needs are socially underprivileged and disproportionately poor (Newacheck, Strickland, Shonkoff, Perrin, McPherson, et al., 1998). Resources most often utilized by families of children with developmental disabilities are those provided by/funded through the state and federal government, i.e. Medicaid, waiver services, SSI, etc. By getting these families enrolled in appropriate programs for which they qualify, the families' financial and employment burden may be decreased.
Our study has some limitations. First, the NS-CSHCN is based on parent interview, thus the prevalence of specific diagnoses is based on parent report. Estimates of physician-diagnosed ASD may be different than parent-reported ASD. However, there is high reliability regarding parent report of ASD with other methods of collecting estimates (Schieve, Rice, Boyle, Visser, Blumberg, 2006). It is not clear if parent report of ID is as reliable as physician diagnosis. Second, a response rate to the survey higher than 25.5% of eligible sampling units may have given a more accurate picture of CSHCN in the United States. However, the high interview completion rate and the person-level weights support the validity of the findings. Third, while the survey addresses financial, employment, and caregiver burden, there are likely other variables that also affect a family's burden. These may include things such as other family members with a disability, parental mental health conditions, parental marital status, etc. The information in the data set is related only to the sample child, and not any other family member. Fourth, while we looked at ASD only and ID only, we did not exclude other co-existing conditions, which could affect a family's financial and employment burden as well. We recognize the fact that children with ASD/ID are more likely to have comorbid disorders such as genetic syndromes that could affect a family's financial burden. Other than Down syndrome, the NS-CSHCN does not list specific genetic disorders for analysis. Other co-existing conditions sometimes seen in children with ASD include GI dysfunction, seizure disorders, sleep disturbances, food allergies/intolerance, and psychiatric illnesses, which could all affect family burden. Finally, this study is cross-sectional; no causality or mechanism for family stressors can be derived.
Despite these limitations, our study had some major strengths. The NS-CSHCN is a nationally representative sample of children. The survey also allows for comparisons between different groups of children based on diagnosis. Our methodology allows for nationally representative estimates of burden prevalence.
Our study suggests that having ID in addition to ASD is associated with high caregiver financial and employment burden. Compared to ASD and ID alone, the presence of ASD and ID together may be associated with a negative impact on the family's financial and employment burden. Timely recognition of ID in addition to ASD is important to tailor the clinical approach and sufficiently support families.
Acknowledgments
Dr. Tilford received support from grant # R01MH089466 from the National Institute of Mental Health. Drs. Kuo and Tilford received support from grant # UL1TR000039 from the National Center for Advancing Translational Science through the Translational Research Institute at the University of Arkansas for Medical Sciences. The funding bodies had no role in design or conduct of the study; collection, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Abbreviations
- ASD
Autism Spectrum Disorder
- ID
intellectual disability
- NS-CSHCN
National Survey of Children with Special Health Care Needs
References
- American Academy of Pediatrics. Identifying infants and young children with developmental disorders in the medical home: an algorithm for surveillance and screening. Pediatrics. 2006;118(1):405–420. doi: 10.1542/peds.2006-1231. Retrieved from http://pediatrics.aappublications.org/content/118/1/405. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth. Arlington, VA: American Psychiatric Association; 2013. DSM-5. [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators; Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders: Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. MMWR Surveillance Summaries. 2014;63(SS02):1–21. Retrieved from http://www.cdc.gov/mmwr/ [PubMed] [Google Scholar]
- Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. Retrieved from http://www.sciencedirect.com/science/article/pii/S1530156705600810. [DOI] [PubMed] [Google Scholar]
- Brown H, Ouellette-Kuntz H, Hunter D, Kelley E, Cobigo V, Lam M. Beyond an autism diagnosis: children's functional independence and parents' unmet needs. Journal of Autism and Developmental Disorders. 2010;41(10):1291–1302. doi: 10.1007/s10803-010-1148-y. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Buescher AS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics. 2014;168(8):721–728. doi: 10.1001/jamapediatrics.2014.210. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Cidav Z, Marcus SC, Mandell DS. Implications of childhood autism for parental employment and earnings. Pediatrics. 2012;129(4):617–623. doi: 10.1542/peds.2011-2700. Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irazábal M, Marsá F, García M, Gutiérres-Recacha P, Martorell A, Salvador-Carulla L, Ochoa S. Family burden related to clinical and functional variables in people with intellectual disability with and without a mental disorder. Research in Developmental Disabilities. 2012;33(3):796–803. doi: 10.1016/j.ridd.2011.12.002. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Järbrink K, Fombonne E, Knapp M. Measuring the parental, service, and cost impacts of children with autistic spectrum disorder: a pilot study. Journal of Autism and Developmental Disorders. 2003;33(4):395–402. doi: 10.1023/a:1025058711465. Retrieved from http://link.springer.com/journal/10803. [DOI] [PubMed] [Google Scholar]
- Johnson CP, Walker WO. Mental retardation: management and prognosis. Pediatrics in Review. 2006;27(7):249–255. doi: 10.1542/pir.27-7-249. Retrieved from http://pedsinreview.aappublications.org/ [DOI] [PubMed] [Google Scholar]
- Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215. doi: 10.1542/peds.2007-2361. Retrieved from http://pediatrics.aappublications.org/content/120/5/1183.full.html. [DOI] [PubMed] [Google Scholar]
- Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005-2006. Pediatrics. 2008;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. Retrieved from http://www.pediatrics.org/cgi/content/full/122/6/e1149. [DOI] [PubMed] [Google Scholar]
- Kogan MD, Blumberg SJ, Schieve LA, Boyle CA, Perrin JM, Ghandour RM, Singh GK, Strickland BB, Trevathan E, van Dyck PC. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009;124(5):1395–1403. doi: 10.1542/peds.2009-1522. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Archives of Pediatrics and Adolescent Medicine. 2011;165(11):1020–1026. doi: 10.1001/archpediatrics.2011.172. Retrieved from http://archpedi.jamanetwork.com/article.aspx?articleid=1107633&resultClick=3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lach LM, Kohen DE, Garner RE, Brehaut JC, Miller AR, Klassen AF, Rosenbaum PL. The health and psychosocial functioning of caregivers of children with neurodevelopmental disorders. Disability and Rehabilitation. 2009;31(8):607–618. doi: 10.1080/09638280802242163. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Novak MM, Zubritsky CD. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116(6):1480–1486. doi: 10.1542/peds.2005-0185. Retrieved from http://pediatrics.aappublications.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montes G, Halterman JS. Association of childhood autism spectrum disorders and loss of family income. Pediatrics. 2008;121(4):e821–e826. doi: 10.1542/peds.2007-1594. Retrieved from. doi:10.1542/peds.2007 1594. [DOI] [PubMed] [Google Scholar]
- Mugno D, Ruta L, D'Arrigo VG, Mazzone L. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health and Quality of Life Outcomes. 2007;5(22) doi: 10.1186/1477-7525-5-22. Retrieved from http://www.hqlo.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newacheck PW, Strickland B, Shonkoff JP, Perrin JM, McPherson M, McManus M, Lauver C, Fox H, Arango P. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1):117–123. doi: 10.1542/peds.102.1.117. Retrieved from http://pediatrics.aappublications.org/ [DOI] [PubMed] [Google Scholar]
- Ouyang L, Grosse SD, Riley C, Bolen J, Bishop E, Raspa M, Bailey DB. A comparison of family financial and employment impacts of fragile x syndrome, autism spectrum disorders, and intellectual disability. Research in Developmental Disabilities. 2014;35(7):1518–1527. doi: 10.1016/j.ridd.2014.04.009. Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock G, Amendah D, Ouyang L, Gross SD. Autism spectrum disorders and health care expenditures: the effects of co-occurring conditions. Journal of Developmental and Behavioral Pediatrics. 2012;33(1):2–8. doi: 10.1097/DBP.0b013e31823969de. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Schieve LA, Rice C, Boyle C, Visser SN, Blumberg SJ. Mental health in the United States: parental report of diagnosed autism in children aged 4-17 – United States, 2003-2004. MMWR Weekly. 2006;55(17):481–486. Retrieved from http://www.cdc.gov/mmwr/mmwr_wk.html. [PubMed] [Google Scholar]
- Schieve LA, Baio J, Rice CE, Durkin M, Kirby RS, Drews-Botsch C, Miller LA, Nicholas JS, Cunniff CM. Risk for cognitive deficit in a population-based sample of U.S. children with autism spectrum disorders: variation by perinatal health factors. Disability and Health Journal. 2010;3(3):202–212. doi: 10.1016/j.dhjo.2009.12.001. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Shattuck PT. The contribution of diagnostic substitution to the growing administrative prevalence of autism in US special education. Pediatrics. 2006;117(4):1028–1037. doi: 10.1542/peds.2005-1516. Retrieved from http://pediatrics.aappublications.org/ [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. The National Survey of Children with Special Health Care Needs Chartbook 2009-2010. Rockville, Maryland: U.S. Department of Health and Human Services; 2013. [Google Scholar]
- Xiong N, Yang L, Yu Y, Hou J, Li J, Li Y, Liu H, Zhang Y, Jiao Z. Investigation of raising burden of children with autism, physical disability and mental disability in China. Research in Developmental Disabilities. 2011;32(1):306–311. doi: 10.1016/j.ridd.2010.10.003. Retrieved from. [DOI] [PubMed] [Google Scholar]