Abstract
Background and Aims
Obesity is associated with increased risks of cardiovascular disease, type 2 diabetes, and other chronic diseases. Prevalence estimates for metabolic disorders are well documented in many populations, but Alaska Native groups are understudied. The Western Alaska Tribal Collaborative for Health Study combines data from three Alaska Native study cohorts to assess differences in obesity prevalence and associations with cardiometabolic risk factors by sex.
Methods and Results
Analyses were based upon a sample of 3985 adult Yup’ik and Inupiat participants with a mean age of 40 years. Prevalence of obesity and metabolic risk factors was assessed according to nationally recognized guidelines. Regression analysis was used to evaluate the association between obesity and cardiometabolic risk factors, including lipids, blood pressure and glucose. The prevalence of obesity (BMI ≥ 30) was significantly higher in women (40%) than men (20%). Only 18.6% of men had a waist circumference (WC) >102cm, while 58% of women had a WC >88cm (p<0.001). Women had higher mean HDL-C and triglyceride levels compared to men, while systolic and diastolic blood pressure, LDL-C, and glucose means were higher in men than in women. In multivariate analyses, BMI and WC were significantly associated with all of the cardiometabolic risk factors, although these associations were more pronounced in men than women.
Conclusion
The high prevalence of obesity and central adiposity among AN women is an important public health concern. Differences in associations between obesity and cardiometabolic risk factors by sex warrants further investigation to develop effective intervention programs.
Keywords: Alaska Native, obesity, cardiometabolic, diabetes
INTRODUCTION
Obesity is associated with an increased risk of cardiovascular disease (CVD), type 2 diabetes (T2D), certain types of cancer, and other chronic diseases (1,2,3). Although the prevalence of obesity and obesity-related comorbidities is high among most ethnic groups, significant disparities exist in the United States. In particular, black, Hispanic, and American Indian groups are at higher risk for the development of obesity, CVD and T2D (4,5). While prevalence of obesity is well documented in European (non-Hispanic) Americans, black and Mexican American populations (5, 6), Alaska Native (AN) groups are understudied. A few reports have noted that the prevalence of obesity among indigenous people living in the circumpolar regions of Alaska, Canada, and Greenland is a growing health concern (7,8,9). One study of AN people conducted almost two decades ago in the Norton Sound region of western Alaska found that the prevalence of obesity was 32.8% for women and 15.6% for men, less than in American Indian populations, although the prevalence of overweight, 27.9% for women and 36.2% for men, was high (9,10).
Abdominal obesity has been observed among Canadian Inuit people, and Inuit women have a higher prevalence of obesity and central body fat than men (11). Since abdominal obesity is highly correlated with metabolic diseases, efforts to increase physical activity and reduce or prevent the deposition of intra-abdominal body fat might serve to reduce or prevent the onset of obesity, CVD and T2D among Arctic populations. However, the relationship between obesity and disease risk has not been fully explored in western Alaska Native peoples.
Over 120,000 Alaska Native people live in Alaska and belong to one of approximately 230 federally recognized tribes (12). The Western Alaska Tribal Collaborative for Health (WATCH) study seeks to rigorously assess prevalence and incidence of obesity, CVD and T2D and their risk factors in western AN people residing in the Norton Sound (NS) and Yukon-Kuskokwim (YK) regions of Alaska (13). In this manuscript, we report the prevalence of overweight, obesity, and cardiometabolic risk factors, and the relationship between obesity and these risk factors, by sex and by cohort, in the WATCH study population.
METHODS
The WATCH study was approved by the Alaska Area Institutional Review Board (IRB) and the Alaska Native Tribal Health Consortium, as well as by the IRBs of all participating institutions and tribal community review boards from the NS and YK regions.
Study Population
The WATCH study combines four large cohort studies in AN communities from the NS and YK regions of Alaska. Together, the four studies comprise a cohort of more than 4,500 individuals living mostly in remote communities in western and southwestern Alaska (14).
The analyses presented here are based on data from 3,985 adult participants (≥ 18 years of age) from the three most recently recruited WATCH study cohorts. The study methods have been previously published (13,14). The Center for Alaska Native Health Research (CANHR) study (15,16) is a longitudinal community-based participatory study recruited from 2003 until 2010. The Alaska Education and Research Toward Health (EARTH) study (17) is a multi-center community-based observational study recruited between 2004 and 2006. These two studies were conducted in the YK region with participants predominantly of Yup’ik descent. The Genetics of Coronary Artery Disease in Alaska Natives (GOCADAN) study (18) was conducted between 2000 and 2004 in the Norton Sound region of Alaska; participants were predominantly of Inupiat descent. All participants who were non-pregnant, and self-reported AN descent, including those individuals reporting a mixed AN ancestry, were included in the analysis.
Study Procedures and Data Consolidation
Age, gender, and ethnicity were self-reported at baseline, defined as first clinic visit after enrollment in the study. In all three cohorts, body composition and blood pressure were assessed by physical exam (13, 15–18). Height and waist circumference (WC) were calculated from the two of three measurements that were the most similar. In CANHR and GOCADAN studies, weight, was measured with bioimpedence analyzers (TANITA TBF-300A, Tanita Corporation of America Inc., Arlington Hills, Illinois; Impedance Meter #BIA101, RJL Equipment Company, respectively). In EARTH, weight was measured by using a Tanita digital scale (BWP800/BWP627A; Tanita Corporation of America Inc., Arlington Hills, Illinois). BMI was calculated using weight (kg)/height (meters)2. In the GOCADAN study, WC was measured supine, while in EARTH and CANHR it was measured erect. In all studies, resting blood pressure was measured three times after a 5-minute rest period with participants in a seated position. CANHR and EARTH studies used the Omron HEM-907® (Omron Healthcare, Kyoto, Japan) automated blood pressure system; the GOCADAN study obtained blood pressures with a mercury sphygmomanometer. An average of the last two of the three blood pressure readings were used for this analysis.
Blood lipids and blood glucose were determined from fasting blood samples. GOCODAN and CANHR used venous blood samples to measure LDL-cholesterol (LDL-C), triglycerides, HDL-cholesterol (HDL-C), and plasma glucose levels. EARTH used capillary blood from a finger stick for lipids and glucose analysis. Both CANHR and EARTH determined lipid and glucose values using the Cholestech LDX Analyzer (Hayward, USA) on site. GOCODAN used a conventional enzymatic chemistry analyzer to assess blood lipids and glucose from a venous blood sample; fasting glucose was assessed using the Accu-Chek Advantage. For CANHR and GOCODAN cohorts, lab values from frozen stored samples were used for analyses; Cholestech LDX Analyzer values were used for the EARTH cohort. Consolidation and harmonization procedures have been described in detail in a previous publication (13). Clinical, anthropometric and laboratory measurements used in this report required minimal harmonization because they were determined with identical or comparable approaches and equipment. Any variable that was too dissimilar to be combined or harmonized was excluded.
Statistical Analysis
For comparisons, the measurements were categorized based on clinically relevant body mass index (BMI) cut-points per National Heart, Lung and Blood Institute; (19): underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2). Due to sample size considerations, underweight participants were grouped in the normal weight category. Cutpoints for central obesity, blood pressure, LDL-C and HDL-C, and triglycerides were categorized by gender according to Adult Treatment Panel (ATP) III guidelines (20,21). Central obesity was defined by WC (>102 cm for men; >88 cm for women). Elevated blood pressure was defined as a blood pressure ≥130/≥85 mm Hg or taking antihypertensive medication based on ATP III guidelines for metabolic syndrome. LDL-C was defined as elevated if ≥130 mg/dl or taking lipid-lowering medications. Medication was assessed using self-report and medical chart abstraction. HDL-C was categorized as low using a cutpoint of <40 mg/dl in men or <50 mg/dl in women. Triglycerides were classified as high or borderline high if ≥150 mg/dl for both men and women. Elevated fasting plasma glucose was classified according to guidelines by the American Diabetes Association Executive Summary: Standards of Medical Care in Diabetes – 2010 (22), with glucose ≥100 mg/dl defined as elevated. Participants who were taking diabetes medications were categorized as having elevated fasting glucose.
Statistical analyses were performed using SAS® version 9.3 (SAS Institute, Cary NC). Differences in the prevalence of risk factors by group were assessed using chi-square tests. Data from the National Health and Nutrition Examination Survey (NHANES) 2007–2008 were used for comparison of overweight and obesity prevalence by gender (23). This nationally representative sample of the US population consists of 5555 adult men and women aged 20 years or older. Associations between the measures of obesity (BMI and WC) and the cardiometabolic risk factors were first evaluated individually using univariate regression analysis stratified by sex and by cohort. Then, multivariate regression analysis of all WATCH study participants was performed with adjustment for age and sex. These models also included an obesity×sex interaction term to determine if the associations differed by sex.
RESULTS
In all three cohorts, and the total WATCH study, there were slightly more women than men (54% vs. 46%) (Table 1). Mean ages in the three cohorts ranged from 38 to 41 years in men and 39 to 42 years in women. In all cohorts, mean ages of women were somewhat older than men. In the total WATCH cohort, 61.7 percent of the women reported having ever smoked cigarettes compared to 80.5 percent of the men (data not shown).
Table 1.
Sample size (percent), Mean values ± SD for Age and Cardiometabolic Risk Factors, by Study and Sex, and for the total WATCH cohort
| CANHR | EARTH | GOCADAN | WATCH | |
|---|---|---|---|---|
| Sample Size | ||||
| Men | 542 (47%) | 699 (47%) | 604 (45%) | 1,845 (46%) |
| Women | 615 (53%) | 794 (53%) | 731 (55%) | 2,140 (54%) |
| Age (years) | ||||
| Men | 37.8 ± 16.3 | 38.0 ± 15.6 | 41.2 ± 16.0 | 39.0 ± 16.0 |
| Women | 39.4 ± 16.3 | 40.7 ± 16.2 | 42.0 ± 16.5 | 40.8 ± 16.3 |
| Body Mass Index | ||||
| Men | 26.2 ± 4.7 | 26.9 ± 5.1 | 26.3 ± 5.1 | 26.5 ± 5.0 |
| Women | 29.2 ±6.7 | 29.7 ± 6.8 | 28.3 ± 6.2 | 29.1 ± 6.6 |
| Waist Circumference (cm) | ||||
| Men | 90.0 ± 13.6 | 93.7 ± 13.8 | 87.0 ± 12.4 | 90.5 ± 13.6 |
| Women | 91.6 ± 15.5 | 97.5 ± 15.4 | 88.3 ± 14.2 | 92.7 ± 15.3 |
| Systolic Blood Pressure (mmHg) | ||||
| Men | 121.9 ± 12.7 | 122.0 ± 12.1 | 120.6 ± 12.9 | 121.5 ± 12.6 |
| Women | 116.0 ± 15.7 | 115.5 ± 15.5 | 116.9 ± 15.6 | 116.1 ± 15.6 |
| Diastolic Blood Pressure (mmHg) | ||||
| Men | 70.2 ± 9.7 | 73.8 ± 10.4 | 77.5 ± 9.3 | 73.9 ± 10.3 |
| Women | 69.6 ± 10.7 | 71.9 ± 10.2 | 73.9 ± 9.2 | 71.9 ± 10.2 |
| LDL-C (mg/dl) | ||||
| Men | 137.7 ± 39.3 | 123.9 ± 39.1 | 116.0 ± 35.7 | 125.6 ± 39.1 |
| Women | 135.2 ± 37.6 | 118.9 ± 35.5 | 114.4 ± 35.2 | 122.2 ± 37.1 |
| HDL-C (mg/dl) | ||||
| Men | 57.7 ± 15.8 | 54.2 ± 16.7 | 55.0 ± 17.6 | 55.5 ± 16.8 |
| Women | 66.1 ± 18.4 | 62.8 ± 17.7 | 63.2 ± 18.2 | 63.9 ± 18.1 |
| Triglycerides (mg/dl) | ||||
| Men | 85.2 ± 53.2 | 101.2 ± 71.5 | 124.3 ± 75.3 | 103.7 ± 69.5 |
| Women | 83.0 ± 44.7 | 105.8 ± 64.4 | 128.1 ± 89.9 | 106.6 ± 71.8 |
| Fasting Glucose (mg/dl) | ||||
| Men | 93.4 ± 10.9 | 100.6 ± 28.7 | 94.0 ± 19.5 | 96.3 ± 22.0 |
| Women | 92.8 ± 15.5 | 96.4 ± 17.8 | 93.8 ± 15.7 | 94.5 ± 16.5 |
Mean values for cardiometabolic risk factors by cohort and for the total WATCH cohort are shown in Table 1. Overall mean BMI for women was higher than for men (29.1 vs. 26.5, respectively), and sex differences were similar in all cohorts. Women had higher mean values for WC, HDL-C, and triglycerides levels compared to men, while mean systolic and diastolic blood pressure, LDL-C, and glucose were higher in men than in women.
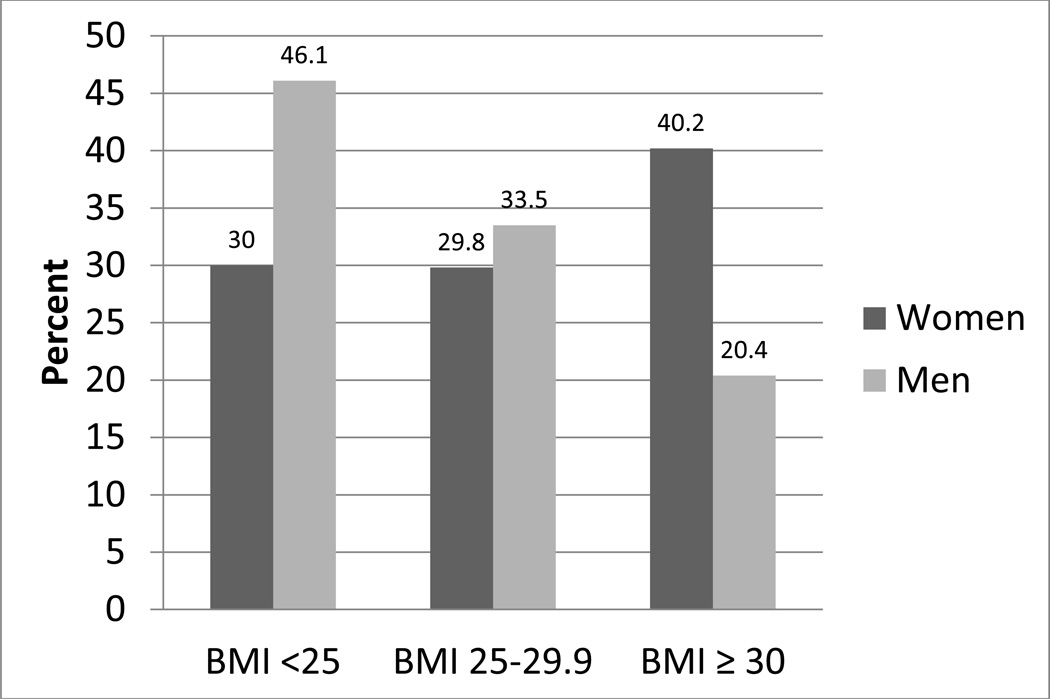
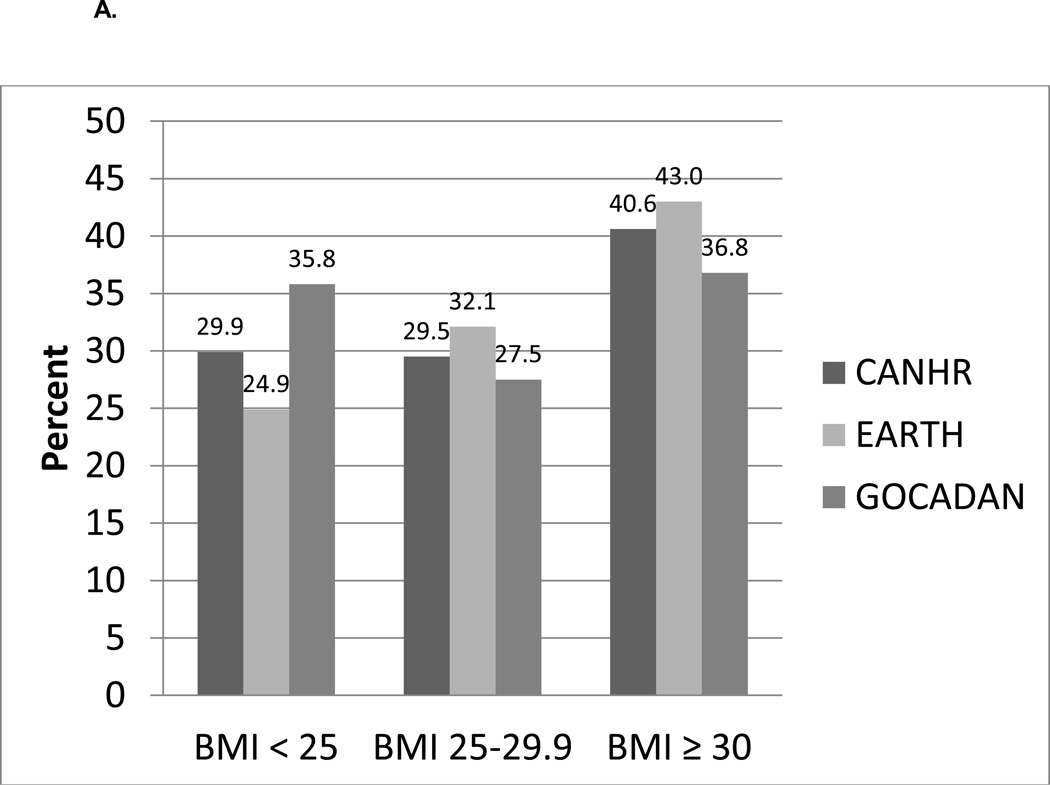
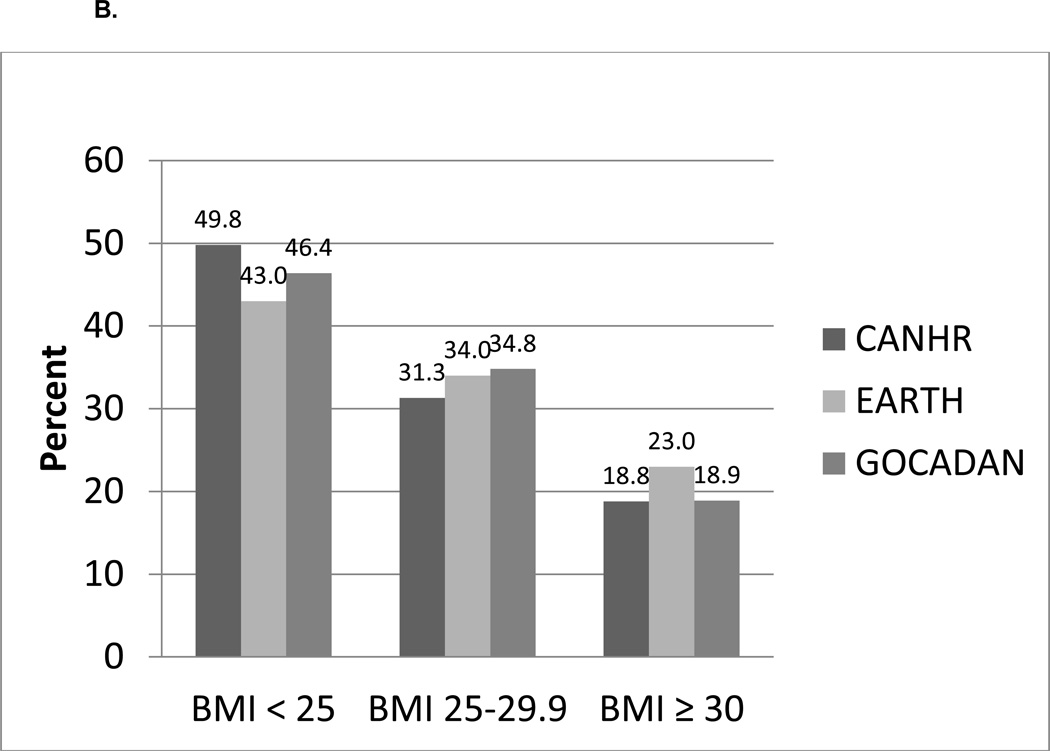
Figure 1 shows the distribution of BMI in the overall WATCH study cohort by sex. More than 40% of women were classified as obese (BMI ≥ 30), compared to 20% of men. The percentages of men and women who were overweight (BMI 25 to 29.9) were similar (33.5 and 29.8, respectively); however, the percentage of men with a BMI < 25 was considerably higher than in women. Similar results were seen in each of the study samples (Figures 2A and 2B).
Figure 1.
Distribution of Body Mass Index (BMI) in the total WATCH cohort by sex
Figure 2.
A. Distribution of Body Mass Index (BMI) in Women by WATCH Study
B. Distribution of Body Mass Index (BMI) in Men by WATCH Study
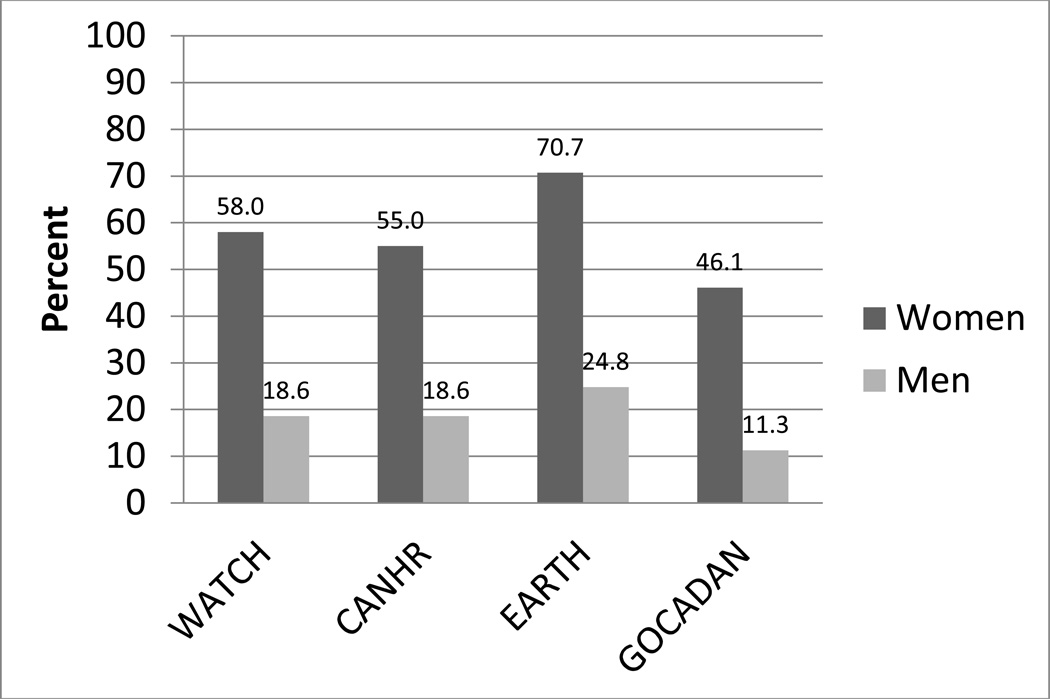
Sex differences in central obesity were even more striking (Figure 3). In the overall WATCH cohort, the prevalence of central obesity was 58% in women compared to 19% in men (p<0.001). Similar results were seen in each of the studies, and the differences between men and women were significantly different in each cohort (p<0.001).
Figure 3.
Prevalence (percent) of central obesity (> 88 cm in women, >102 cm in men) in the total WATCH cohort and each WATCH study by sex
In contrast to the obesity results, the prevalence of elevated blood pressure was significantly lower in women than men in the combined WATCH cohort (Supplementary Table 1A), due primarily to the difference between men and women in the GOCADAN cohort (38% vs. 29%, respectively) and the EARTH cohort (26% vs. 22%, respectively), while the prevalence of elevated blood pressure was similar among men and women in the CANHR cohort. As shown in Supplementary Table 1B, the prevalence of elevated LDL-C was similar among men and women in the overall WATCH cohort. In each study, and in the combined WATCH cohort, women had a significantly higher prevalence of low HDL-C than men (Supplementary Table 1C). There were no significant differences in the percentage of men and women with elevated triglycerides (Supplementary Table 1D). In all studies and the overall WATCH cohort, a greater percentage of men had either fasting plasma glucose ≥ 100 mg/dl or were taking diabetes medications (Supplementary Table 1E).
As shown in Table 2A, systolic blood pressure (SBP), diastolic blood pressure (DBP), LDL-C, triglycerides and fasting glucose were significantly positively associated, and HDL-C was significantly negatively associated, with both BMI and WC in univariate analyses for both men and women. BMI was more strongly associated (larger beta values) with DBP, HDL-C, and triglycerides in men than women. We ran the univariate association analyses by study cohort (CANHR, GOCADAN, EARTH) and by region. The results did not differ substantially by cohort. In multivariate analyses, significant BMI × risk factors interactions were observed for the same risk factors, DBP, HDL-C and triglycerides, confirming that the BMI – risk factor associations were stronger in men than women. In univariate analysis of WC (Table 2B), WC was more strongly associated with LDL-C and triglycerides in men than women, while SBP was less strongly associated among men than women. The significant WC×risk factor interaction term for these risk factors confirms the sex differences in these associations. Thus, for several risk factors, the association of obesity with cardiometabolic risk factors was less pronounced in women than men, despite the higher levels of obesity among women.
Table 2.
Univariate and Multivariate Regression Analysis for Associations of Body Mass Index and Waist Circumference with Cardiometabolic Risk Factors for the total WATCH cohort
| A. Body Mass Index (BMI) | ||||||
|---|---|---|---|---|---|---|
| Univariate | Multivariate | |||||
| BMI Beta Coefficient | BMI Beta Coefficient (p-value) |
Age Beta Coefficient (p-value) |
Sex Beta Coefficient (p-value) |
BMI × sex interaction coefficient (p-value) |
||
| Men (p-value) |
Women (p-value) |
|||||
| Systolic BP | 0.58 | 0.50 | 0.45 | 0.29 | 5.99 | 0.04 |
| (mmHg) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.005) | (0.592) |
| Diastolic BP | 0.64 | 0.48 | 0.48 | 0.03 | −0.85 | 0.16 |
| (mmHg) | (<0.001) | (<0.001) | (<0.001) | (0.001) | (0.585) | (0.005) |
| LDL-C | 1.16 | 0.82 | 0.71 | 0.61 | −0.32 | 0.25 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.957) | (0.254) |
| HDL-C | −1.11 | −0.87 | −0.91 | 0.32 | −0.25 | −0.29 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.341) | (0.001) |
| Triglycerides | 5.40 | 3.37 | 3.33 | 0.24 | −46.51 | 1.99 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (<0.001) |
| Fasting Glucose | 0.81 | 0.75 | 0.70 | 0.28 | 3.68 | 0.02 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.213) | (0.882) |
| B. Waist Circumference (WC) | ||||||
|---|---|---|---|---|---|---|
| Univariate | Multivariate | |||||
| WC Beta Coefficient | WC Beta Coefficient (p-value) |
Age Beta Coefficient (p-value) |
Sex Beta Coefficient (p-value) |
WC × sex interaction coefficient (p-value) |
||
| Men (p-value) |
Women (p-value) |
|||||
| Systolic BP | 0.21 | 0.25 | 0.20 | 0.27 | 12.82 | −0.07 |
| (mmHg) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.016) |
| Diastolic BP | 0.20 | 0.20 | 0.19 | 0.01 | 2.22 | 0.002 |
| (mmHg) | (<0.001) | (<0.001) | (<0.001) | (0.137) | (0.271) | (0.904) |
| LDL-C | 0.63 | 0.39 | 0.30 | 0.57 | −10.91 | 0.18 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.156) | (0.033) |
| HDL-C | −0.34 | −0.35 | −0.41 | 0.37 | −5.61 | 0.35 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.086) | (0.321) |
| Triglycerides | 1.81 | 1.45 | 1.44 | 0.08 | −30.93 | 0.35 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (0.224) | (0.027) | (0.021) |
| Fasting Glucose | 0.36 | 0.34 | 0.30 | 0.25 | 4.14 | −0.01 |
| (mg/dl) | (<0.001) | (<0.001) | (<0.001) | (<0.001) | (0.276) | (0.738) |
DISCUSSION
While obesity is associated with poor health outcomes in most adult populations worldwide, it is important to understand the complex relationship between obesity and cardiometabolic risk factors among AN people. In this large cohort, based on harmonized data from three cohort studies of AN people, the prevalence of obesity, based on both BMI and WC was substantially higher in women than men. The 2007–2008 NHANES survey reported 36.2% of women and 32.6% of men were obese (BMI ≥ 30) (23). Compared to NHANES, the percentage of obese women in the CANHR and EARTH cohorts were significantly higher (p=0.024 and p<0.001, respectively), while the percentage of obese women in GOCADAN was approximately the same as in NHANES. The percentage of obese men were significantly lower than the percentage of obese men in NHANES (p<0.001). These findings demonstrate important differences in the prevalence of obesity between AN women and men.
Similar results have been found in other smaller studies in circumpolar indigenous populations. In a Canadian cross-sectional study, conducted in 2007–2008, the prevalence of overweight and obesity in Inuit adults was 28% and 36%, respectively (24), similar to the results presented here. A study among Greenland Inuit in 2005–2010 suggested that the prevalence of general and central obesity is increasing, especially among women (25). The percentage of women in that study with central obesity was 54%, similar to WATCH study results.
In contrast, less substantial differences in cardiometabolic risk factors were seen between men and women. For example, the prevalence of elevated LDL-C and high triglycerides was not significantly different between men and women. Elevated blood pressure was not significantly different by sex in the CANHR cohort, although differences were seen in the GOCADAN and EARTH studies and the presence of elevated blood pressure was significantly higher in men than women. Other environmental factors, including tobacco use and physical activity, may contribute to this gender difference and need further exploration. However, in all three cohorts and in the overall WATCH cohort, women had a significantly higher prevalence of low HDL-C compared to male study participants. This may indicate increased risk for cardiovascular disease among women. Despite the lower prevalence of obesity in men, the prevalence of elevated fasting plasma glucose (or taking diabetes medications) was higher in men than women in each cohort and the overall WATCH study.
All of the cardiometabolic risk factors were associated with measures of obesity among men and women and in all the study cohorts, although these relationships were stronger for men than for women for several of the risk factors. Similarly, in a study among circumpolar Inuit, Young et al. found that while mean values of metabolic risk factors increased with levels of obesity, these values were lower than those found in Euro-Canadians (26). Further exploration into the complex relationship between central obesity and metabolic risk factors is needed to determine if there is the same degree of cardiometabolic risk in this population studied here.
Participants in all three studies that comprise the WATCH cohort reside in small rural communities that engage in a subsistence lifestyle that includes hunting, fishing, and gathering. This lifestyle is physically active and provides a diet rich in omega 3 fatty acids, which have been indicated in previous studies to be protective for CVD (27,28). However, physical activity patterns vary by gender. In a CANHR study of 179 AN participants, 47% of the women were sedentary compared to 9% of men (29), possibly contributing to the differences in obesity seen in this analysis by sex. A subsistence lifestyle in rural AN communities often involves moderate to vigorous physical activity such as hunting and fishing, hauling water, and gathering wood, activities primarily performed by men. Rural AN women engage in more sedentary activities like food preparation and crafts, including knitting, basket making, and sewing. Moreover, Westernization in Inuit communities with more cash-based jobs and increasing use of motorized transportation (snow machines, 4-wheelers, and boats) has led to decreased physical activity and may increase cardiometabolic risk among both men and women in AN communities by increasing the prevalence of obesity (30).
Differences in methods, including measurement of WC (erect vs. supine), could influence differences seen between cohorts and could be a limitation of the study. However, we made a direct comparison of WC measured in an erect vs supine position in a subset of 50 CANHR participants and the results were indistinguishable (unpublished). Additional clinical, anthropometric and laboratory variables were measured using comparable methods (e.g., body weight, blood pressure, blood glucose and lipids) and were therefore combined directly and variable keys were used to note differences in methods between studies (13). Another limitation is the use of WC as a simple and indirect measure of visceral adiposity as there was no abdominal computed tomography (CT), MRI or DXA available in the WATCH study communities. However, anthropometry and bioimpedance compare reasonably well with more refined body composition methods (31). Other limitations include the lack of ethnic-specific criteria for cardiometabolic risk factors, and that we can only examine prevalence cross-sectionally with the data currently available. We also cannot definitively state the degree to which the study populations are genetic clusters because we have not genotyped participants from all three cohorts using an extensive set of the same genetic markers. A major strength of this study is the large sample size representing three representative cohorts of AN people from western Alaska. This is the first consolidated study of multiple cohorts of AN people to examine obesity prevalence and cardiometabolic risk factors.
CONCLUSION
The high prevalence of obesity and central adiposity in AN women in the WATCH study is a serious health concern. Similar to other populations, these levels are associated with increases in cardiometabolic risk factors among both men and women. The multivariate analyses, however, suggest that obesity may have less impact on cardiometabolic risk factors among women than among men, but additional research with a more refined measurement of visceral fat is necessary. Future research is needed to investigate gender-specific cardiometabolic factors and obesity prevalence, with the goal of developing culturally relevant and effective interventions to reduce cardiometabolic disease risk.
Supplementary Material
Highlights.
We assessed differences in obesity and cardiometabolic risk factors by sex.
Alaska Native women had more obesity and central adiposity than Alaska Native men.
The women had higher HDL-C and triglycerides than the men.
Men had higher blood pressure, LDL-C, and glucose than the women.
Cardiometabolic risk factors in women were less strongly associated with obesity.
ACKNOWLEDGEMENTS
SEH, KRK, JGU, BVH, and BBB were involved in study design of the WATCH study. SEH, CK, KRK and BBB collected data. All authors were involved in data analysis and interpretation, writing the paper, and had final approval of the submitted and published versions. The WATCH study was funded in part by an American Recovery and Reinvestment Act Administrative Supplement to a grant funded by the National Center for Research Resources (NCRR) at the National Institutes of Health (P20 RR16430-08S2). The Center for Alaska Native Health Research (CANHR) was funded through the NCRR COBRE [P20 RR016430 and R01 DK074842] mechanisms. Alaska Education and Research Toward Health (EARTH) was funded by the National Cancer Institute [CA88958 and CA96095]. Genetics of Coronary Artery Disease in Alaska Natives (GOCADAN) was funded by the National Heart, Lung, and Blood Institute [U01 HL64244]. Additional Federal funds (Grant # UL1RR031975) from the NCRR and the National Center for Advancing Translational Sciences, NIH, through the Clinical and Translational Science Awards Program, a trademark of the U.S. Department of Health and Human Services, part of the Roadmap Initiative, “Re-Engineering the Clinical Research Enterprise; with funds from the National Institute of Diabetes and Digestive and Kidney Diseases (DK097307) and with funds made available by the President of the University of Alaska from unrestricted donations by British Petroleum and ConocoPhillips.
Abbreviations
- AN
Alaska Native
- ATP
Adult Treatment Panel
- BMI
body mass index
- CANHR
Center for Alaska Native Health Research
- CVD
cardiovascular disease
- DBP
diastolic blood pressure
- EARTH
Alaska Education and Research Toward Health
- GOCADAN
Genetics of Coronary Artery Disease in Alaska Natives
- HDL-C
HDL-cholesterol
- IRB
Institutional Review Board
- LDL-C
LDL cholesterol
- NHANES
National Health and Nutrition Examination Survey
- NS
Norton Sound
- SBP
systolic blood pressure
- T2D
type 2 diabetes
- WATCH
Western Alaska Tribal Collaborative for Health
- WC
waist circumference
- YK
Yukon-Kuskokwim
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests: the authors have no competing interests.
REFERENCES
- 1.Caballero B. The Global Epidemic of Obesity: An Overview. Epidemiologic Reviews. 2007;29:1–5. doi: 10.1093/epirev/mxm012. [DOI] [PubMed] [Google Scholar]
- 2.Baskin ML, Ard J, Franklin F, Allison DB. Prevalence of obesity in the United States. Obes Rev. 2005;6:5–7. doi: 10.1111/j.1467-789X.2005.00165.x. [DOI] [PubMed] [Google Scholar]
- 3.Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd-Jones D, Sowers J. Obesity-related hypertension: Pathogenesis, cardiovascular risk, and treatment-A position paper of the TheObesity Society and the American Society of Hypertension. Obesity (Silver Spring) 2012 Dec 20; doi: 10.1111/jch.12049. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Chen X. How much of racial/ethnic disparities in dietary intakes, exercise, and weight status can be explained by nutrition- and health-related psychosocial factors and socioeconomic status among US adults? J Am Diet Assoc. 2011 Dec;111(12):1904–1911. doi: 10.1016/j.jada.2011.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC. Differences in Prevalence of Obesity Among Black, White, and Hispanic Adults --- United States, 2006--2008. MMWR. 58(27):740–744. http://www.cdc.gov/features/dsobesityadults/index.html. [PubMed] [Google Scholar]
- 6.Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D. Changing Trends in the Prevalence and Disparities of Obesity and Other Cardiovascular Disease Risk Factors in Three Racial/Ethnic Groups of USA Adults. Adv Prev Med. 2012;2012:172423. doi: 10.1155/2012/172423. PMCID: PMC3518078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young TK. Obesity, central fat patterning, and their metabolic correlates among the inuit of the central Canadian Arctic. Hum Biol. 1996;68:245–263. [PubMed] [Google Scholar]
- 8.Bjerregaard P, Jorgensen ME, Andersen S, Mulvad G, Borch-Johnsen K. Decreasing overweight and central fat patterning with Westernization among the Inuit in Greenland and Inuit migrants. Int J Obes Relat Metab Disord. 2002;26:1503–1510. doi: 10.1038/sj.ijo.0802082. [DOI] [PubMed] [Google Scholar]
- 9.Risica PM, Schraer C, Ebbesson SO, Nobmann ED, Caballero B. Overweight and obesity among alaskan eskimos of the bering straits region: the alaska siberia project. Int J Obes Relat Metab Disord. 2000;24:939–944. doi: 10.1038/sj.ijo.0801259. [DOI] [PubMed] [Google Scholar]
- 10.Risica PM, Ebbesson SO, Schraer CD, Nobmann ED, Caballero BH. Body fat distribution in Alaskan Eskimos of the Bering Straits region: the Alaskan Siberia Project. Int J Obes Relat Metab Disord. 2000;24:171–179. doi: 10.1038/sj.ijo.0801103. [DOI] [PubMed] [Google Scholar]
- 11.Young TK, Bjerregaard P, Dewailly E, Risica PM, Jorgensen ME, Ebbesson SE. Prevalence of obesity and its metabolic correlates among the circumpolar inuit in 3 countries. Am J Public Health. 2007;97:691–695. doi: 10.2105/AJPH.2005.080614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Conference of State Legislatures. Federal and State Recognized Tribes. 2013 http://www.ncsl.org/issues-research/tribal/list-of-federal-and-state-recognized-tribes.aspx. [Google Scholar]
- 13.Koller KR, Wolfe AW, Metzger JS, Austin MA, Hopkins SE, Kaufmann C, Jolly SE, Ebbesson SOE, Umans JG, Howard BV, Boyer BB. Utilizing Harmonization and Common Surveillance Methods to Consolidate Four Cohorts: The Western Alaska Tribal Collaborative for Health (WATCH) Study. Int J Circumpolar Health. 2013;72:20572. doi: 10.3402/ijch.v72i0.20572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howard BV, Metzger JS, Koller KR, Jolly SE, Asay ED, Wang H, Wolfe AW, Hopkins SE, Kaufmann C, Raymer TW, Trimble B, Provost EM, Ebbesson SOE, Austin MA, Howard WJ, Umans JG, Boyer BB. All-Cause, Cardiovascular, and Cancer Mortality in Western Alaska Native People: Western Alaska Tribal Collaborative for Health (WATCH) American Journal of Public Health. doi: 10.2105/AJPH.2013.301614. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyer BB, Mohatt GV, Lardon C, et al. Building a community-based participatory research center to investigate obesity and diabetes in Alaska Natives. Int J Circumpolar Health. 2005;64:281–290. doi: 10.3402/ijch.v64i3.18002. [DOI] [PubMed] [Google Scholar]
- 16.Mohatt GV, Plaetke R, Klejka J, et al. The Center for Alaska Native Health Research Study: a community-based participatory research study of obesity and chronic disease-related protective and risk factors. Int J Circumpolar Health. 2007;66:8–18. doi: 10.3402/ijch.v66i1.18219. [DOI] [PubMed] [Google Scholar]
- 17.Slattery ML, Schumacher MC, Lanier AP, Edwards S, Edwards R, Murtaugh MA, et al. A prospective cohort of American Indian and Alaska Native people: study design, methods, and implementation. Am J Epidemiol. 2007;166(5):606–515. doi: 10.1093/aje/kwm109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howard BV, Devereux RB, Cole SA, Davidson M, Dyke B, Ebbesson SO, et al. A genetic and epidemiologic study of cardiovascular disease in Alaska natives (GOCADAN): design and methods. Int J Circumpolar Health. 2005;64(3):206–221. doi: 10.3402/ijch.v64i3.17985. [DOI] [PubMed] [Google Scholar]
- 19.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 20.Chobanian AV, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 21.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106;(25):3143–3421. [PubMed] [Google Scholar]
- 22.Excecutive Summary: Standards of Medical Care in Diabetes-2010. Diabetes Care. 2010 Jan;33(Supplement 1) doi: 10.2337/dc10-S004. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National HEalth and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007–2008. http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/ [Google Scholar]
- 24.Zienczuk N, Young TK, Zhirong RC, Egeland GM. Dietary correlates of an at-risk BMI among Inuit adults in the Canadian high arctic: cross-sectional international polar year Inuit health survey, 2007–2008 2012. Nutrition Journal. 2012;11:73. doi: 10.1186/1475-2891-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bjerregaard P, Jørgensen ME The Greenland Population Study Group. Prevalence of Obesity Among Inuit in Greenland and Temporal Trend by Social Position. Am J Hum Biol. 2013 Feb 5; doi: 10.1002/ajhb.22372. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Young TK, Bjerregaard P, Dewailly E, Risica PM, Jorgensen ME, Ebbesson SEO. Prevalence of Obesity and Its Metabolic Correlates Among the circumpolar Inuit in 3 Countries. American Journal of Public Health. 2007 Apr;97(4):691–5. doi: 10.2105/AJPH.2005.080614. Epub 2007 Feb 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Makhoul Z, Kristal AR, Gulati R, Luick B, Bersamin A, O’Brien D, Hopkins SE, Stephensen CB, Stanhope KL, Havel PJ, et al. Associations of obesity with triglycerides and C-reactive protein are attenuated in adults with high red blood cell eicosapentaenoic and docosahexaenoic acids. Eur. J. Clin. Nutr. 2011;65:808–817. doi: 10.1038/ejcn.2011.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bersamin A, Luick BR, Ruppert E, Stern JS, Zidenberg-Cherr S. Nutrient intakes are associated with adherence to a traditional diet among Yup’ik Eskimos living in remote Alaska Native Communities: The CANHR Study. International Journal of Circumpolar Health. 2007;66(1):62–70. doi: 10.3402/ijch.v66i1.18228. [DOI] [PubMed] [Google Scholar]
- 29.Bersamin A, Wolsko C, Luick B, Boyer B, Lardon C, Hopkins S, Stern J, Zidenberg-Cherr S. Enculturation, Perceived Stress, and Physical Activity: Implications for Metabolic Risk among the Yup’ik. Ethnicity and Health. 2014 Jun;19(3):255–269. doi: 10.1080/13557858.2012.758691. Epub 2013 Jan 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jørgensen ME, Moustgaard H, Bjerregaard P, Borch-Johnsen K. Gender differences in the association between westernization and metabolic risk among Greenland Inuit. Eur J Epidemiol. 2006;21(10):741–748. doi: 10.1007/s10654-006-9063-4. Epub 2006 Nov 1. [DOI] [PubMed] [Google Scholar]
- 31.Boyer BB, Heo M, Allison DB, Liebenstein NT, Cho IS, Wang Z, Heymsfield SB. Comparison of body composition methodologies: determining what is most practical for the hospital, research laboratory or remote field study. International Journal of Body Composition Research. 2004;2(3):115–124. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.