Abstract
Objectives
Though the emergency department (ED) provides essential care for severely ill or injured children, past research has shown that children often visit the ED for potentially preventable illnesses, including asthma. We sought to determine how children’s rate of ED visits for asthma has changed over the last decade, and analyze what factors are associated with a child’s potentially preventable ED visit for asthma.
Methods
We retrospectively analyzed ED visits by children aged 2–17 from 2001–2010 using data from the National Hospital Ambulatory Medical Care Survey. Visits were classified as potentially preventable asthma visits by mapping ICD-9-CM diagnosis codes to the Agency for Healthcare Research and Quality’s asthma pediatric quality indicator. We examined trends in the annual rate of ED visits for asthma per 1000 children using a weighted linear regression model. Finally, we used multivariate logistic regression to determine what demographic, clinical, and structural factors were associated with a child’s ED visit being for a potentially preventable asthma crisis.
Results
The rate of children’s ED visits for asthma increased 13.3% between 2001 and 2010, from 8.2 to 9.3 visits per 1000 children (p=0.26). ED visits by children who were younger, male, racial or ethnic minorities, insured with Medicaid/CHIP, and visiting between 11pm – 7am were more likely to be for potentially preventable asthma crises.
Conclusions
Though the overall rate of potentially preventable ED visits for asthma did not significantly change over the last decade, racial, insurance-based, and other demographic disparities in the likelihood of a preventable asthma-related ED visit persist.
Keywords: asthma, emergency department utilization, National Hospital Ambulatory Medical Care Survey
Introduction
In 2011, 19% of all U.S. children had at least one visit to the emergency department (ED), amounting to a total of 25 million ED visits by children annually.1,2 While the ED represents an essential point of healthcare access for severely ill or injured children, many children seek treatment in the ED for potentially preventable reasons.3
Due to the high cost of ED care and the strained emergency care system, recent focus has been directed towards reducing ED visits that could have been either treated in a primary care setting or prevented by improved access to and quality of primary care.4,5 Children, who account for one in five ED visits nationally, have not been immune to these efforts.2 One condition often highlighted as a driver of preventable ED use is childhood asthma. Asthma can be effectively managed by medication and high-quality primary care,6 but can also quickly escalate into a respiratory crisis requiring emergency care if not controlled.7
Emergency department visits for asthma are often used as an adverse outcome for studies of the effectiveness of different asthma control therapies and practices,7–9 as well as those looking at the influence on the environment on children’s asthma.10,11 However, studies of trends in and predictors of ED visits for asthma as measures of public health or the effectiveness of preventive care at the population level have mainly been limited to cross-sectional,12 purely descriptive,13,14 or more dated analyses.15,16
In the last decade, numerous initiatives and promising advances have been made in efforts to reduce asthma crises and associated preventable acute care use. The National Asthma Education and Prevention Program (NAEPP) of the National Institutes of Health’s National Heart, Lung, and Blood Institute updated guidelines in 1997 and 2007 with scientific evidence describing diagnostic and treatment guidelines for physicians, including long-term strategies for monitoring and controlling asthma and preventing complications.17 There have been federally funded efforts to introduce initiatives to reduce ED visits for asthma, ranging from school asthma control programs to widespread dissemination of evidence-based guidelines.18,19 There have also been extensive state and local efforts to increase preventive medication use for asthma20 and reduce acute care use.9
To see whether these efforts have made an impact on preventable outpatient acute care use, we analyze the trends in ED visits by children for asthma from 2001 to 2010. We also identify the demographic, clinical and structural characteristics associated with pediatric ED visits for a potentially preventable asthma crises over this time period. The trajectory of and factors associated with children’s ED use for asthma can help identify trends in children’s access to and quality of preventive asthma care, and target areas to reduce these potentially preventable ED visits.
Methods
Study Design and Data Sources
We conducted a retrospective analysis of hospital emergency department visits by children using data from the 2001–2010 National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS is a survey of ambulatory care visits to nonfederal, general, short-stay US hospitals conducted annually by the National Center for Health Statistics (NCHS). To generate a national probability sample of ED visits, NHAMCS employs a three-stage sampling design: 112 geographic primary sampling units, approximately 480 hospitals within primary sampling units, and patient visits within EDs at each hospital.21,22
For each sampled visit, US Census Bureau field representatives or hospital staff complete a patient record form based on the patient’s medical record. The data collected includes demographic information as well as clinical variables such as vital signs, cause of injury, diagnoses, medications, and discharge status. SRA International, Inc., Durham, NC performed the data processing. A 10% sample is independently coded for quality assurance; typical error rates found from the resulting comparison are 0.3–0.9%.
The survey data was analyzed using sampled visit weights provided by NCHS. The weights are the product of the sampling fractions at each stage of the design, and take into account non-response rates within geographic region, time of year, demographic oversampling, and urban/rural and ownership designations. The final weighted visit counts represent national estimates of ED visits and associated characteristics. When computing rates of ED use per population, we used corresponding population denominator numbers from the U.S. Census Bureau.
The NCHS Research Ethics Review Board approves the NHAMCS annually. This study was exempt from review by the Committee on Human Research at the University of California San Francisco, as only de-identified data was used.
Sample Selection
We included all ED visits by children 17 years and under. Within this group, we excluded children covered by Medicare (4.5%), as they are typically severely ill and disabled and their ED use is therefore not comparable to our remaining sample. To limit the range of the clinical severity of visits, we also excluded patients who died in the ED (0.01%). Finally, per the specifications of AHRQ’s potentially preventable asthma measure, we excluded patients younger than two years old.
Outcome
Our primary outcome was ED visits by children with a principal ICD-9-CM diagnosis code for asthma, as specified in the Agency for Healthcare Research and Quality’s (AHRQ) asthma pediatric prevention quality indicator.23 While the measure was primarily intended to measure preventable hospitalizations for asthma, the corresponding adult asthma measure has been used with ED visits in the past.24,25 In addition, similar categorizations of asthma diagnoses have been used as a measure of preventable asthma crises requiring acute care in previous studies.26,27
Covariates
We defined numerous demographic and clinical visit characteristics that could be associated with a child’s ED visit was for asthma a priori, based largely on previous literature.12,28 We examined demographics including patient age (2–5, 6–9, 10–13, and 14–17 years old), insurance coverage (private, Medicaid/CHIP, self-pay/uninsured, and other), gender, and race (non-Hispanic White, non-Hispanic Black, Hispanic, and other).12,29 We also examined basic visit characteristics including arrival method (ambulance, walk-in), arrival day (weekend, weekday), arrival time (7am–3pm, 3pm–11pm, 11pm–7am), whether the patient was discharged from hospital within the previous seven days, and whether the patient had been seen at that ED in the last 72 hours. In addition, we examined clinical variables including triage level (need to be seen in <15 min, 15min–1hr, 1–2hrs, 2–24hrs; corresponding to immediate/emergent, urgent, semi-urgent, and non-urgent classifications) as determined by a triage nurse, and if the patient had any abnormal vital signs (pulse rate, blood pressure, temperature, or respiratory rate) given their age.30–32 Finally, we included the hospital’s geographic region (Northeast, Midwest, South, West), and whether the hospital was in a urban or rural Metropolitan Statistical Area (MSA).
Statistical Analysis
Using denominators from the US Census Bureau, we computed annual rates of ED visits for asthma per 1000 US children ages 2–17 and examined trends in the rates descriptively. We then analyzed the change in pediatric ED visit rates for asthma from 2001 to 2010 using a linear regression model weighted for population. Finally, we analyzed the association of the previously described demographic and structural factors with pediatric ED visits for asthma using a multivariate logistic regression model, which also incorporated NHAMCS sampling weights. Analyses were performed using SAS (version 9.2; SAS Institute, Cary, North Carolina) and SUDAAN (version 10.0; RTI International, Research Triangle Park, North Carolina).
Results
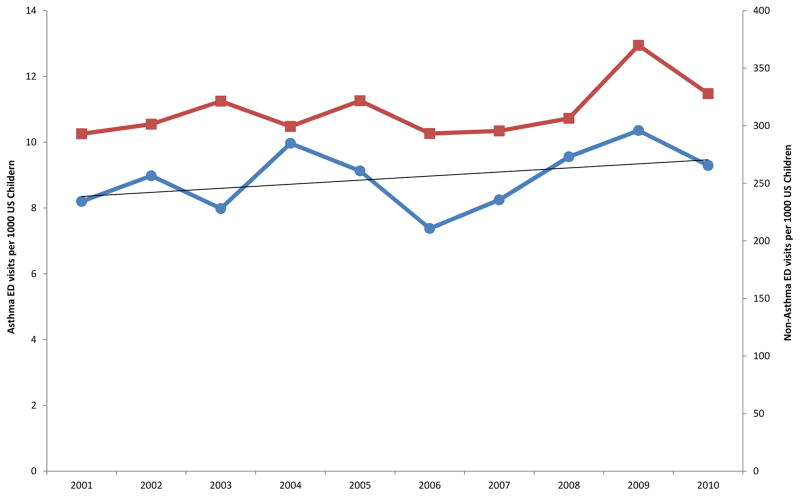
We analyzed 62,849 pediatric ED visits between 2001 and 2010, representing 211 million visits nationally. Just under three percent of the visits were for potentially preventable asthma crises, with the weighted annual count rising 16% from 531,374 visits for asthma in 2001 to 615,958 in 2010. However, when adjusted for population, there was no significant trend in the rate of ED visits for asthma per 1000 children ages 2–17 from 2001 to 2010 (p=0.26). Though the absolute change from 2001 to 2010 was 13.3%, there were significant fluctuations year to year and no definitive direction was noted upon analysis with weighted linear regression (Figure 1). Similarly, the rate of ED visits for non-asthma diagnoses also exhibited no significant trend between 2001 and 2010 (p=0.16).
Figure 1.
Rates ED visits for potentially preventable asthma and non- potentially preventable asthma diagnoses by children ages 2–17, 2001–2010
Legend: Though ED visit rates for potentially preventable asthma diagnoses (blue line) rose from 8.2 per 1000 children in 2001 to 9.3 per 1000 in 2010 (13.3%) and other diagnoses (red line) diagnoses rose from 293 to 323 per 1000 (11.9%), there were many fluctuations and neither was statistically significant (p = 0.26 and 0.16, respectively).
As shown in Table 1, in an unadjusted descriptive comparison visits for asthma were more likely to be by younger, male patients, racial or ethnic minorities, children with Medicaid insurance, children visiting from 11pm–7am and children seen at urban hospitals compared to non-asthma visits. Children presenting with asthma were also more often admitted and had shorter triage times compared with those visiting the ED for another condition.
Table 1.
Characteristics of pediatric ED visits by asthma classification, 2001–2010
| Asthma | Non-Asthma | ||
|---|---|---|---|
| No. of visits (col %) | No. of visits (col %) | p value | |
| Total | 5,841,628 (100%) | 205,232,589 (100%) | |
| Age | |||
| 2–5 years | 2,189,485 (37.5%) | 68,221,554 (33.2%) | <0.01 |
| 6–9 years | 1,534,378 (26.3%) | 41,849,082 (20.4%) | |
| 10–13 years | 1,093,068 (18.7%) | 40,619,837 (19.8%) | |
| 14–17 years | 1,023,697 (17.5%) | 54,542,116 (26.6%) | |
| Gender | |||
| Female | 2,321,433 (39.7%) | 97,888,803 (47.7%) | <0.01 |
| Male | 3,520,195 (60.3%) | 107,343,786 (52.3%) | |
| Race | |||
| NH white | 2,287,741 (39.2%) | 116,309,200 (56.7%) | <0.01 |
| NH black | 2,208,561 (37.8%) | 45,987,147 (22.4%) | |
| Hispanic | 1,172,623 (20.1%) | 36,548,807 (17.8%) | |
| Other | 172,703 (3.0%) | 6,387,435 (3.1%) | |
| Geographic Region | |||
| Northeast | 1,297,980 (22.2%) | 36,502,022 (17.8%) | <0.01 |
| Midwest | 1,415,000 (24.2%) | 47,145,755 (23.0%) | |
| South | 2,320,729 (39.7%) | 86,059,909 (41.9%) | |
| West | 807,919 (13.8%) | 35,524,903 (17.3%) | |
| MSA | |||
| Urban | 5,218,664 (89.3%) | 170,167,814 (82.9%) | <0.01 |
| Rural | 622,964 (10.7%) | 35,064,775 (17.1%) | |
| Insurance | |||
| Private | 2,143,936 (36.7%) | 88,055,285 (42.9%) | <0.01 |
| Medicaid/CHIP | 2,621,898 (44.9%) | 78,519,895 (38.7%) | |
| Self-pay/uninsured | 566,043 (9.7%) | 19,640,080 (9.6%) | |
| Other^ | 180,931 (3.1%) | 7,058,809 (3.4%) | |
| Missing | 328,820 (5.6%) | 10,958,520 (5.3%) | |
| Arrival | |||
| Ambulance | 117,958 (2.0%) | 2,844,930 (1.4%) | 0.29 |
| Walk-in | 1,076,776 (18.4%) | 40,972,632 (20.0%) | |
| Unknown | 4,646,894 (79.5%) | 161,415,027 (78.6%) | |
| Arrival Time | |||
| 7am–3pm | 2,041,342 (34.9%) | 68,148,287 (33.2%) | <0.01 |
| 3pm–11pm | 2,424,912 (41.5%) | 107,944,134 (52.6%) | |
| 11pm–7am | 1,334,589 (22.8%) | 27,214,840 (13.3%) | |
| Unknown | 40,785 (0.7%) | 1,925,328 (0.9%) | |
| Triage | |||
| <15 minutes | 1,236,284 (21.2%) | 21,978,909 (10.7%) | <0.01 |
| 15min–1 hr | 2,511,213 (43.0%) | 68,325,771 (33.3%) | |
| 1hr–2hr | 1,019,028 (17.4%) | 58,182,384 (28.3%) | |
| 2hr–24hr | 266,361 (4.6%) | 25,584,006 (12.5%) | |
| Unknown | 808,742 (13.8%) | 31,161,519 (15.2%) | |
| Arrival Day | |||
| Weekend | 1,886,067 (32.3%) | 63,103,434 (30.7%) | 0.36 |
| Weekday | 3,955,561 (67.7%) | 142,129,155 (69.3%) | |
| Discharged w/in 7 days | |||
| Yes | 35,216 (0.6%) | 1,454,745 (0.7%) | 0.52 |
| No | 2,135,931 (36.6%) | 78,874,421 (38.4%) | |
| Unknown | 3,670,481 (62.8%) | 124,903,421 (38.4%) | |
| Seen Before | |||
| Yes | 112,275 (1.9%) | 4,527,958 (2.2%) | 0.65 |
| No | 4,922,905 (84.3%) | 173,743,578 (84.7%) | |
| Unknown | 806,448 (13.8%) | 26,961,053 (13.1%) | |
| Abnormal Vitalsa | |||
| Any abnormal | 240,260 (4.1%) | 10,443,419 (5.1%) | 0.21 |
| All normal | 5,124,216 (87.7%) | 176,126,614 (85.8%) | |
| Any missing | 477,152 (8.2%) | 12,662,556 (9.1%) | |
| Discharge Status | |||
| Transfer | 79,405 (1.4%) | 2,922,524 (1.4%) | <0.01 |
| Admitted to hospital | 431,009 (7.4%) | 6,452,480 (3.1%) | |
| Discharged/left | 5,291,277 (90.6%) | 193,591,559 (94.4%) | |
| Unknown | 39,937 (0.7%) | 2,215,299 (1.1%) |
The range of normal for breaths per minute is 22 to 34 for those 2 to 5 years old, 18–30 for those 6 to 12 years old, and 12–16 for those older than 12 years. The range of normal for heart beats per minute is 80 to 140 for those 2 to 5 years old, 70 to 120 for those 6 to 12 years old, and 60 to 100 for those older than 12 years. The range of normal systolic blood pressure is 70 to 95 mm Hg for children 2 to 8 years old, and 90 to 140 mm Hg for those older than 8 years. Values that fell outside (above or below) these ranges were considered abnormal. Abnormal temperature was defined as a recorded temperature above 38°C/100.4°F. (see citations # 30 & 31)
Our multivariate logistic regression showed that numerous demographic and clinical visit characteristics increased the odds that a visit was for a potentially preventable asthma crisis, even after adjustment for other influential factors (Table 2). For instance, ED visits by younger children and male children were more likely to be for potentially preventable asthma crises, as were visits by black and Hispanic children compared with white children. In addition, visits by children covered by Medicaid/CHIP had higher odds of being for potentially preventable asthma concerns than visits by privately insured children. Finally, pediatric ED visits with shorter triage times, visits at urban hospitals, visits occurring between 11pm and 7 am, and visits resulting in admission all had higher odds of being for a potentially preventable asthma crisis.
Table 2.
Results of multivariate logistic regression model of factors associated with potentially preventable ED visits for asthma by children ages 2–17, 2001–2010
| Adjusted OR (95% CI) | |
|---|---|
| Age | |
| 2–5 | ref |
| 6–9 | 1.2 (1.1, 1.4) |
| 10–13 | 0.9 (0.8, 1.1) |
| 14–17 | 0.6 (0.5, 0.7) |
| Gender | |
| Female | 0.7 (0.6, 0.8) |
| Male | ref |
| Race | |
| Non-Hispanic white | ref |
| Non-Hispanic black | 2.2 (1.9, 2.6) |
| Hispanic | 1.4 (1.2, 1.7) |
| Other | 1.2 (0.8, 1.7) |
| Geographic region | |
| Northeast | 1.5 (1.2, 1.9) |
| Midwest | 1.4 (1.1, 1.8) |
| South | 1.1 (0.9, 1.4) |
| West | ref |
| MSA | |
| Urban | ref |
| Rural | 0.7 (0.5, 0.9) |
| Insurance | |
| Private | ref |
| Medicaid/CHIP | 1.2 (1.1, 1.4) |
| Self-pay/uninsured | 1.2 (0.9, 1.5) |
| Other | 1.0 (0.6, 1.7) |
| Missing | 1.1 (0.8, 1.5) |
| Arrival | |
| Ambulance | 1.0 (0.6, 1.7) |
| Walk-in | ref |
| Unknown | 0.9 (0.8, 1.5) |
| Arrival time | |
| 7am–3pm | ref |
| 3pm–11pm | 0.8 (0.7, 0.9) |
| 11pm–7am | 1.6 (1.3, 1.9) |
| Unknown | 0.8 (0.4, 1.4) |
| Triage | |
| <15 minutes | 5.5 (3.8, 7.8) |
| 15min–1 hr | 3.6 (2.6, 5.1) |
| 1hr–2hr | 1.7 (1.2, 2.5) |
| 2hr–24hr | ref |
| Unknown | 2.5 (1.7, 3.7) |
| Arrival day | |
| Weekend | 1.1 (0.9, 1.3) |
| Weekday | ref |
| Discharged w/in 7 days | |
| Yes | 0.6 (0.3, 1.4) |
| No | ref |
| Unknown | 1.0 (0.9, 1.2) |
| Seen before | |
| Yes | 0.9 (0.6, 1.4) |
| No | ref |
| Unknown | 1.0 (0.9, 1.3) |
| Abnormal vitals | |
| Any abnormal | 0.9 (0.6, 1.3) |
| All normal | ref |
| Any missing | 0.9 (0.7, 1.2) |
| Discharge status | |
| Transfer | 0.8 (0.5, 1.5) |
| Admitted to hospital | 1.9 (1.5, 2.4) |
| Discharged^ | ref |
| Unknown | 0.6 (0.3, 1.3) |
Includes left without being seen
Discussion
Over the last decade, we found that minority race, Medicaid insurance, younger age, and arrival between 11pm and 7am, for example, were associated with increased odds of an ED visit being for a potentially preventable asthma crisis. Rural residence and female gender, on the other hand, were associated with decreased odds of an ED visit being for a potentially preventable asthma crisis. These results provide updated evidence that disparities continue to persist in access to quality preventive asthma care and preventable acute care use for asthma.
Our findings align with previous literature detailing the higher self-reported rates of ED visits for asthma among Black,33 Hispanic,34 and younger children.16 They also correspond with previous studies showing higher overall ED visits by children with Medicaid insurance,25 as well as lower healthcare use for asthma by girls,16 but stand in contrast to the evidence on worse primary care access for preventive asthma care in rural areas.35
Many of the demographic groups that we find have higher odds of an ED visit being for potentially preventable asthma crises have higher prevalence of asthma, including racial minorities,33 male children,16 children in urban areas,35 and low-income children likely to qualify for Medicaid,14 which likely drives a portion of the higher likelihood of potentially preventable ED visits for asthma.
However, our finding that ED visits by otherwise similar children between 11pm and 7am had higher odds of being for potentially preventable asthma crises than visits occurring during the day suggests that these visits are related to a lack of primary care access, as most physician offices and clinics are closed during these hours. Past research has found that lack of after-hours access to primary care is consistent driver of ED use,36 and that better self or parent-reported after-hours access to care is associated with lower ED use by children and adults.37,38 This evidence suggests continued room for improved asthma care delivery in the primary care setting to reduce potentially preventable acute care use, especially among vulnerable demographic groups.
We also found that visits during 3pm–11pm, during which time many primary care clinics are closed for at least a portion of the time, were significantly less likely to be for asthma than those between 7am and 3pm. This discrepancy could be due to other factors, including slightly extended hours by many clinics and potentially the limited availability of urgent care centers.
Overall, the rate of emergency department use by children ages 2–17 for asthma rose from 8.20 visits per 1000 US children in 2001 to 9.29 visits per 1000 in 2010, but the change was not statistically significant and involved many fluctuations over the decade. A number of factors may have contributed to the generally stable trend. For instance, despite an increase in the prevalence of asthma in children from 8.7% in 2001 to 9.4% in 2010,39,40 the numerous initiatives and promising advances to reduce asthma crises and associated preventable acute care use in this past decade may have had some effect. For example, in 1999 the CDC launched the National Asthma Control Program, which invested over $238 million between 2001 and 2012 in territorial and state asthma control programs, school asthma control programs, national surveillance, and developing and disseminating best practices and evidence based guidelines.18 This huge effort was adapted locally in all states and implemented with different partners and stakeholders,41 and could have potentially affected the trajectory of potentially preventable ED visits for asthma.
In addition, environmental and behavioral trends during our study period, including improvements in air quality,42 and decreasing smoking prevalence,43 should have reduced the prevalence of asthma triggers and the associated number of preventable asthma crises and ED visits. Finally, from 2001–2010 the proportion of children with private insurance dropped from 70% to 60%, while the proportion of children covered by Medicaid and CHIP/SCHIP programs rose from 23% to 36%.44 Given overwhelming evidence that children with Medicaid have more difficulty accessing high-quality primary care than privately insured children,38,45,46 and perhaps the resulting evidence of their higher rate of potentially preventable ED use,25,47 this population-level insurance transition may have driven up the rate of ED use for potentially preventable asthma crises over time.
Limitations
There are several limitations to our study. First, because there is no linkage between visits in NHAMCS, we could not identify multiple visits by the same child. Therefore, our results only reflect rates of ED visits per 1000 children, not the proportion of the population with an ED visit. Second, as with all administrative data, there are limitations in the accuracy and ability to verify clinical data due to a combination of chart abstraction and keying errors.48 However, there is no other nationally representative dataset that allows an analysis over this length of time to be performed. Because the purpose of this study is to present trends reflecting changes in the ability of the pediatric primary care system to prevent the need for ED use, we feel it is an appropriate use of the data.
Conclusion
Though the overall rate of potentially preventable ED visits for asthma by children did not change significantly between 2001 and 2010, ED visits by younger, male children, racial minorities, those enrolled in Medicaid/CHIP programs, and those visiting between the hours of 11pm – 7am had higher odds of being for potentially preventable asthma crises. Our findings that populations vulnerable to poor healthcare access continue to be the most likely to make preventable ED visits for asthma potentially suggest that efforts to decrease barriers to quality preventive care for asthma may be more effective when targeted more specifically at certain sub-populations.
What’s New.
ED visits between 2001 and 2010 by children traditionally vulnerable to poor healthcare access were more likely to be for potentially preventable asthma crises than ED visits by their demographic counterparts, suggesting room for improvements in asthma care delivery.
Acknowledgments
Project Support: This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2 TR000143 (R.Y.H), and the Robert Wood Johnson Foundation Physician Faculty Scholars Program (R.Y.H.). The sponsors had no role in the design and conduct of the study, in the collection, analysis, and interpretation of data, or in the preparation, review, or approval of the manuscript.
We especially thank Judy Maselli, MSPH, for her assistance with data analysis for this project.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- ED
emergency department
- NCHS
National Center for Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
Footnotes
Conflicts of interest: The authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Hyatsville, MD: 2013. [PubMed] [Google Scholar]
- 2.Healthcare Cost and Utlization Project. [Accessed August 12, 2013.];National Emergency Department Dataset. 2010 http://hcupnet.ahrq.gov.
- 3.Fong C. The influence of insurance status on nonurgent pediatric visits to the emergency department. Acad Emerg Med. 1999;6(7):744–748. doi: 10.1111/j.1553-2712.1999.tb00446.x. [DOI] [PubMed] [Google Scholar]
- 4.Massachusetts Division of Health Care Finance and Policy. Efficiency of Emergency Department Utilization in Massachusetts. 2012 Document No. 12-236-HCF- 05. [Google Scholar]
- 5.Adams JG. Emergency department overuse: Perceptions and solutions. JAMA. 2013;309(11):1173–1174. doi: 10.1001/jama.2013.2476. [DOI] [PubMed] [Google Scholar]
- 6.Homer CJ, Szilagyi P, Rodewald L, et al. Does quality of care affect rates of hospitalization for childhood asthma? Pediatrics. 1996;98(1):18–23. [PubMed] [Google Scholar]
- 7.Adams RJ, Fuhlbrigge A, Finkelstein JA, et al. Impact of Inhaled Antiinflammatory Therapy on Hospitalization and Emergency Department Visits for Children With Asthma. Pediatrics. 2001;107(4):706–711. doi: 10.1542/peds.107.4.706. [DOI] [PubMed] [Google Scholar]
- 8.Lieu TA, Quesenberry CP, Capra AM, Sorel ME, Martin KE, Mendoza GR. Outpatient management practices associated with reduced risk of pediatric asthma hospitalization and emergency department visits. Pediatrics. 1997;100(3):334–341. doi: 10.1542/peds.100.3.334. [DOI] [PubMed] [Google Scholar]
- 9.Cloutier MM, Hall CB, Wakefield DB, Bailit H. Use of asthma guidelines by primary care providers to reduce hospitalizations and emergency department visits in poor, minority, urban children. J Pediatr. 2005;146(5):591–597. doi: 10.1016/j.jpeds.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Norris G, Young Pong SN, Koenig JQ, Larson TV, Sheppard L, Stout JW. An association between fine particles and asthma emergency department visits for children in Seattle. Environ Health Perspect. 1999;107(6):489. doi: 10.1289/ehp.99107489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villeneuve PJ, Chen L, Rowe BH, Coates F. Outdoor air pollution and emergency department visits for asthma among children and adults: a case-crossover study in northern Alberta, Canada. Environ Health. 2007;6(1):40. doi: 10.1186/1476-069X-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friday GA, Jr, Khine H, Lin MS, Caliguiri LA. Profile of Children Requiring Emergency Treatment for Asthma. Ann Allergy Asthma Immunol. 1997;78(2):221–224. doi: 10.1016/S1081-1206(10)63391-1. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001–2009. MMWR. 2011;60(17):547. [PubMed] [Google Scholar]
- 14.Moorman J, Akinbami L, Bailey C, et al. National Surveillance of Asthma: United States, 2001–2010. Vital & Health Statistics. 2012;3(35):1–67. [PubMed] [Google Scholar]
- 15.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110(2):315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 16.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of Childhood Asthma in the United States, 1980–2007. Pediatrics. 2009;123(3):S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Breathing Easier. Chamblee, GA: 2009. [Google Scholar]
- 18.Centers for Disease Control and Prevention. CDC’s National Asthma Control Program: An Investment in America’s Health. Chamblee, GA: U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 19.Centers for Disease Control and Prevention. [Accessed April 18, 2014];CDC’s National Asthma Control Program. 2013 http://www.cdc.gov/asthma/nacp.htm.
- 20.Kit BK, Simon AE, Ogden CL, Akinbami LJ. Trends in Preventive Asthma Medication Use Among Children and Adolescents, 1988–2008. Pediatrics. 2012;129(1):62–69. doi: 10.1542/peds.2011-1513. [DOI] [PubMed] [Google Scholar]
- 21.McCaig LF, Burt CW. Understanding and interpreting the National Hospital Ambulatory Medical Care Survey: key questions and answers. Ann Emerg Med. 2012;60(6):716–721. doi: 10.1016/j.annemergmed.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. [Accessed April 17, 2014.];NHAMCS Scope and Sample Design. 2010 http://www.cdc.gov/nchs/ahcd/ahcd_scope.htm-nhamcs_scope.
- 23.Agency for Healthcare Research and Quality. [Accessed April 15, 2014.];Pediatric Quality Indicators Technical Specifications Version 4.5: PDI 14. 2013 [Google Scholar]
- 24.Johnson PJ, Ghildayal N, Ward AC, Westgard BC, Boland LL, Hokanson JS. Disparities in Potentially Avoidable Emergency Department (ED) Care: ED Visits for Ambulatory Care Sensitive Conditions. Med Care. 2012;50(12):1020–1028. doi: 10.1097/MLR.0b013e318270bad4. [DOI] [PubMed] [Google Scholar]
- 25.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and Characteristics of U.S. Emergency Department Visits, 1997–2007. JAMA. 2010;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001–2009. MMWR. 2011;60(17):547. [PubMed] [Google Scholar]
- 27.Rust G, Zhang S, Reynolds J. Inhaled corticosteroid adherence and emergency department utilization among Medicaid-enrolled children with asthma. J Asthma. 2013;50(7):769–775. doi: 10.3109/02770903.2013.799687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parker JD, Schoendorf KC. Variation in hospital discharges for ambulatory care-sensitive conditions among children. Pediatrics. 2000;106(4 Suppl):942–948. [PubMed] [Google Scholar]
- 29.Friedman B, Berdahl T, Simpson LA, et al. Annual report on health care for children and youth in the United States: focus on trends in hospital use and quality. Acad Pediatr. 2011;11(4):263–279. doi: 10.1016/j.acap.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Dickinson ET, Lozada KN. Trend Alert: the trending & interpretation of vital signs. JEMS. 2010;35(3):62–64. 66, 68, 71. doi: 10.1016/S0197-2510(10)70066-8. [DOI] [PubMed] [Google Scholar]
- 31.Browner B, Pollack AN, Gupton C American Academy of Orthopaedic Surgeons. Energency Care and Transportation for the Sick & Injured. 8. Burlington, MA: Jones & Bartlett Publishing; 2002. [Google Scholar]
- 32.National Center for Health Statistics. 2010 NHAMCS Micro-Data File Documentation. Hyattsville, MD: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 33.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: Evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006;117(5):e868–e877. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 34.Oraka E, Iqbal S, Flanders WD, Brinker K, Garbe P. Racial and ethnic disparities in current asthma and emergency department visits: findings from the National Health Interview Survey, 2001–2010. J Asthma. 2013;50(5):488–496. doi: 10.3109/02770903.2013.790417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valet RS, Perry TT, Hartert TV. Rural health disparities in asthma care and outcomes. J Allergy Clin Immunol. 2009;123(6):1220–1225. doi: 10.1016/j.jaci.2008.12.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lowe RA, Localio AR, Schwarz DF, et al. Association Between Primary Care Practice Characteristics and Emergency Department Use in a Medicaid Managed Care Organization. Med Care. 2005;43(8):792–800. doi: 10.1097/01.mlr.0000170413.60054.54. [DOI] [PubMed] [Google Scholar]
- 37.Zickafoose JS, DeCamp LR, Prosser LA. Association between enhanced access services in pediatric primary care and utilization of emergency departments: a national parent survey. J Pediatr. 2013;163(5):1389–1395. doi: 10.1016/j.jpeds.2013.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Malley AS. After-hours access to primary care practices linked with lower emergency department use and less unmet medical need. Health Aff (Millwood) 2013;32(1):175–183. doi: 10.1377/hlthaff.2012.0494. [DOI] [PubMed] [Google Scholar]
- 39.National Center for Health Statistics. [Accessed August 12, 2013.];Table 4-1: Current Asthma Prevalence Percents by Age, United States: National Health Interview Survey Data, 2001. 2004 http://www.cdc.gov/asthma/nhis/01/table4-1.htm.
- 40.National Center for Health Statistics. [Accessed August 12, 2013.];Table 4-1: Current Asthma Prevalence Percents by Age, United States: National Health Interview Survey Data, 2010. 2012 http://www.cdc.gov/asthma/nhis/2010/table4-1.htm.
- 41.Centers for Disease Control and Prevention. [Accessed May 1, 2014.];Breathing Easier: Success Stories from CDC’s National Asthma Control Program. 2013 http://www.cdc.gov/asthma/state_success_stories.htm.
- 42.U.S. Environmental Protection Agency. [Accessed April 18, 2014.];Air Quality Trends: Percent Change in Air Qualiy. 2013 http://www.epa.gov/airtrends/aqtrends.html-airquality.
- 43.Garrett BE, Dube SR, Trosclair A, Caraballo RS, Pechacek TF. Cigarette Smoking -- United States, 1965–2008. MMWR Surveill Summ. 2011;60(1):109–113. [PubMed] [Google Scholar]
- 44.US Census Bureau. Health Insurance Historical Tables - HIB Series. 2011. Table HIB-2. Health Insurance Coverage Status and Type of Coveragem, All Persons by Age and Sex -- 1999 to 2011. [Google Scholar]
- 45.Bisgaier J, Rhodes KV. Auditing Access to Specialty Care for Children with Public Insurance. N Engl J Med. 2011;364(24):2324–2333. doi: 10.1056/NEJMsa1013285. [DOI] [PubMed] [Google Scholar]
- 46.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat. 2011;10(250):1–80. [PubMed] [Google Scholar]
- 47.Shi L, Lu N. Individual sociodemographic characteristics associated with hospitalization for pediatric ambulatory care sensitive conditions. J Health Care Poor Underserved. 2000;11(4):373–384. doi: 10.1353/hpu.2010.0732. [DOI] [PubMed] [Google Scholar]
- 48.Green SM. Congruence of Disposition After Emergency Department Intubation in the National Hospital Ambulatory Medical Care Survey. Ann Emerg Med. 2013;61(4):423–426. e428. doi: 10.1016/j.annemergmed.2012.09.010. [DOI] [PubMed] [Google Scholar]