Abstract
Objectives. I explored the structural and operational practices of the chronic disease prevention and control unit of a state health department and proposed a conceptual model of structure, function, and effectiveness for future study.
Methods. My exploratory case study examined 7 elements of organizational structure and practice. My interviews with staff and external stakeholders of a single chronic disease unit yielded quantitative and qualitative data that I coded by perspective, process, relationship, and activity. I analyzed these for patterns and emerging themes.
Results. Chi-square analysis revealed significant correlations among collaboration with goal ambiguity, political support, and responsiveness, and evidence-based decisions with goal ambiguity and responsiveness.
Conclusions. Although my study design did not permit conclusions about causality, my findings suggested that some elements of the model might facilitate effectiveness for chronic disease units and should be studied further. My findings might have important implications for identifying levers around which capacity can be built that may strengthen effectiveness.
Public health agencies struggle to identify optimal administrative and programmatic structures. Although public health effectiveness literature documents how a state health department should function to achieve the intended impact on population health, little is known about how organizational structure changes affect function, and ultimately, health.1,2 Proposed guidelines for professional and organizational competencies exist,3–5 but the role public health agency structure plays in effective functioning has not been definitively examined.1,6–9 My case study examined the attributes (how an organization is structured) and practices (how an organization operates) of the chronic disease prevention and control unit of a state health department. My findings could inform a conceptual model for future empirical study and might assist state health departments in identifying levers of effectiveness.
State-level public health agencies and funders, which are faced with difficult economic realities, seek administrative and programmatic efficiencies that maximize public health impact with the available resources. Three recent initiatives focused on state health department operations: state health department accreditation,3 the National Prevention Strategy,10 and Coordinated Chronic Disease funding from the Centers for Disease Control and Prevention (CDC).11
The pressures of accreditation and coordinated chronic disease funding have resulted in small- and large-scale organizational changes, ranging from alterations in leadership to structural reorganization.12,13 Despite a mandate to use evidence-based decision-making in public health practice,10,14–16 and the broad uptake of evidence-based interventions for risk factor reduction, the evidence linking organizational structure and public health outcomes remains undeveloped.1,9 State health departments have had very little evidence to apply in creating highly efficient organizational structures that maximize population health outcomes.2,9 The assumption remains that an effectively run state health department with adequate resources and competent professional staff employing evidence-based decision-making will improve population health.14,17,18
METHODS
Data collection and analysis took place between November 2012 and March 2013. Because of the wide variability among state health departments and the exploratory nature of this study, I used a single case to perform a descriptive examination of the conceptual model and the study questions.19 The overarching question driving the case study asked: how is the organizational structure of state health departments related to chronic disease unit performance? My specific study questions included:
How is the state health department’s chronic disease prevention and control unit structured?
What are the perceptions of managers, internal stakeholders, and external stakeholders regarding the effectiveness of the chronic disease unit?
What do managers, internal stakeholders, and external stakeholders believe are the structural factors that influence the unit’s effectiveness?
How are these beliefs consistent with the elements included in the conceptual model?
Case Identification
The chronic disease unit examined in this study was selected via a convenience sample. To protect the sample from possible study fatigue, I considered states that were current or recent participants in case study or similar projects. To bound data collection appropriately, I considered chronic disease units with fewer than 100 staff members. I chose 5 states with varying geography, population density, and demographic characteristics make-up, and I solicited for their interest. Three states indicated interest. I based my final decision on timing and availability of potential participants. The case I selected had a chronic disease unit that included 53 staff positions and was in a state with a population of approximately 1 million people.
Literature Review and Model Development
I began an iterative literature review using an electronic database search for peer-reviewed articles that addressed organizational structure and function in state health departments. I followed this with an Internet search for reports and recommendations from organizations that were working to build state health department capacity. I expanded the search to include nonprofit and private sector literature, as well as other types of government agencies. I assessed all findings for relevance to the research questions, and I scanned the bibliographies of those studies that met the inclusion criteria for potential sources. I queried experts in the field of state public health practice for recommendations for additional sources. I included a final collection of 122 sources, only 9 of which were related to the empirical study results, in the formal review for this study.
Although the review of the literature revealed measures of organizational effectiveness and related functional domains, I did not find any investigations of the relationship between state-level public health organizational structure and the effectiveness of chronic disease prevention activities. However, structural attributes, including staffing levels, stability, resource levels, and organizational change, influenced effectiveness.1,6,8,20–22 Workforce competency including leadership, experience level, technical skills, and professionalism were linked to effectiveness.7,8,20,23 Evidence-based decision-making, performing essential services, goal clarity, and managing uncertainty were also linked to effectiveness.1,17,20,21,23
I was particularly interested in a proposed and tested organizational performance model by Stazyk and Gordel.1 Drawing on resource dependence and contingency theories, the authors proposed and then showed that hierarchical authority in health and human services bureaucracies could moderate the negative effects of goal ambiguity and low political support on organizational performance.1 They concluded the following:
Hierarchical authority describes centralization in decision-making,
Goal ambiguity describes the extent to which organizational goals are understood by the staff, and
Political support describes the level of endorsement a program receives from decision-makers inside the organization as well as policymakers external to the organization.
Four additional elements were especially prominent in the literature and relevant to current performance improvement activities nationwide. These included collaboration, evidence-based decision-making, workforce competency, and responsiveness. They are defined as follows:
Collaboration is working internally and externally for the purpose of leveraging resources to maximize effectiveness and efficiency,2,24,25
Evidence-based decision-making is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of populations,15
Responsiveness is the ability of the organization to react dynamically to changes in the political environment and to address emerging public health needs,23–29 and
Workforce competency is the level of skill, professionalism, and knowledge present among the staff.21,23,24,29
Although it was apparent that these performance improvement elements contributed to effectiveness, the relationship among these elements and the organizational structure was not clear. For the purpose of my study, I considered these in 2 groups and defined them as follows: (1) attributes are elements that describe how the unit is structured, and (2) practices are elements that describe how the unit operates.
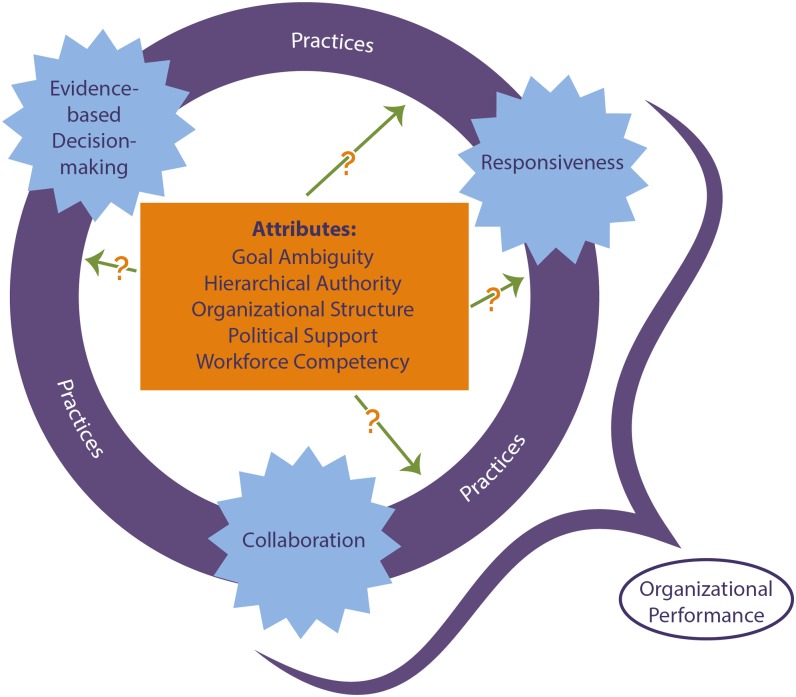
The resulting model included the attributes of hierarchical authority, goal ambiguity, and political support as taken from the model of organizational performance by Stazyk and Goerdel1 and also incorporated evidence-based decision-making, responsiveness, and collaboration (Figure 1). The organizational attributes of goal ambiguity, hierarchical authority, organizational structure, political support, and workforce competency form the center of Figure 1. Organizational practices, including evidence-based decision-making, responsiveness, and collaboration encircle the attributes.
FIGURE 1—
Conceptual model of organizational attributes and practices in state health department chronic disease units.
Data Collection
I collected data through document review and key informant interviews. Documents included the chronic disease unit organizational chart, the state chronic disease plan, and a report of the Public Health Framework Assessment Tool capacity assessment conducted by the state before I began this case study. These documents were provided to me by the director of the chronic disease unit. Key informants included managers of programs within the chronic disease prevention and control unit, the chronic disease director, other senior staff of the chronic disease unit, program and administrative staff of the chronic disease unit, the state health official, 2 senior staff members from the state health official’s office, and representatives of 2 key partner organizations identified by the chronic disease director. Table 1 details the question topics I included in the interviews. I collected and summarized the detailed field notes. Participants were given the opportunity to clarify, edit, or amend draft notes. Of 42 participants, 12 (or 28.5%) submitted edits.
TABLE 1—
Interview Question Topics: US State Health Departments, November 2012–March 2013
| Model Element | Question Topic |
| Goal ambiguity | Perception of goal clarity within the leadership |
| Perception of goal clarity within the staff | |
| Hierarchical authority | Perception of level of authority in current position |
| Perception of where decision authority rests within the structure | |
| Political support | Perception of external political support |
| Perception of internal political support | |
| Workforce competency | Opinion of staff professional competency |
| Use of competency standards | |
| Access to ongoing training | |
| Evidence-based decision-making | Perception of criteria for decision-making |
| Inputs used in decision-making | |
| Perception of robustness of decision-making | |
| Collaboration | Perception of extent of collaboration |
| Perception of collaboration competency | |
| Responsiveness | Confidence that emerging needs can be adequately addressed |
| Confidence that core work will continue if resources are interrupted | |
| Confidence that the unit can respond strategically to new opportunities | |
| Perception of changes in responsiveness over last 5 years | |
| Performance | Perception of program effectiveness |
| Perception of unit effectiveness | |
| Perception of state health department effectiveness | |
| Perception of structural elements that facilitate effectiveness | |
| Perception of structural elements that impede effectiveness | |
| Perception of impact of changes to structure or operating practices | |
| Perception of ideal unit structure |
All potential key informants were invited to participate and to engage in the proscribed informed consent process. Confidentiality procedures included blinding of interview response data in the analysis.
I organized the data by model element, coded it by perspective, process, relationship, and activity, and reviewed it for patterns and emerging themes. I explored the identified patterns for all respondents and for each factor in the conceptual model. I interviewed participants to determine their assessment of the unit’s performance and capacity in each element of the conceptual model, as well as the relevance of each element to effectiveness. I paired open-ended interview questions with Likert-scale response categories. This focused the discussion and allowed for quantitative analysis of each of the model elements.
Data Analysis
I performed quantitative, qualitative, and mixed methods analyses using the Dedoose platform (Dedoose, Los Angeles, CA), which is a web-based analysis package designed to maintain rigorous security for datasets, to link quantitative and qualitative data, and to perform χ2 testing of relationships between quantitative variables and weighted mixed methods analysis.30
I uploaded the cleaned and de-identified qualitative interview data to Dedoose, and I linked the quantitative and qualitative records. Interview data were initially coded by conceptual model element and then by theme. Themes emerged through an iterative process of key word identification and memoing. As concepts emerged during this process, codes were reassessed and revised. This necessitated removing all coding tags and memos and starting the process anew. This cycle was completed multiple times until no new codes emerged, which resulted in the final set of codes (see the box on page e5).31–33
Code Development: US State Health Department Chronic Disease Units, November 2012–March 2013
| Original Codes | Key Words | Emerging Themes | Final Codes |
| Collaboration | Communications | Culture | Culture |
| Evidence-based decision-making | Partners | Entrepreneurial behavior | - Communications |
| Political support | Environment | Environment | - Entrepreneurial behavior |
| Responsiveness | Funder | Technology | - Evaluation |
| Performance | Administrative rules | Specialization | - Innovation |
| Structure | Leadership | Oversight | - Partnership |
| Staffing | Proximity | Environment | |
| Innovation | - Physical environment | ||
| Visibility | - Proximity | ||
| Politics | - Technology | ||
| Management | Outputs | ||
| Interventions | - Intervention | ||
| Problem-solving | - Media presence | ||
| - Visibility | |||
| Oversight | |||
| - Administrative processes | |||
| - Funder influence | |||
| Structure | |||
| - Leadership | |||
| - Roles or responsibilities | |||
| - Staffing | |||
| Elements | |||
| - Collaboration | |||
| - Evidence-based decision-making | |||
| - Goal ambiguity | |||
| - Political support | |||
| - Workforce competency | |||
| - Performance |
RESULTS
Interview participants were solicited from among the employees of the chronic disease unit, the leadership of the same state health department, and representatives of external partner organizations. Of the 53 positions indicated on the organizational chart, 2 shared 1 position, 5 were vacant, 1 was a contractor, 1 was on maternity leave, and 8 either declined, failed to respond, or were unable to keep their interview appointments. This left a total of 37 chronic disease unit respondents. In addition, the state health official, the state medical officer for public health, and the public health systems improvement coordinator or accreditation manager participated. Two representatives of external partner organizations, a local health department and chronic disease–focused advocacy organization, also participated. A third external partner representative was unable to participate at the last moment. The total number of interviews completed was 42, with a response rate of 82.4%. I classified the participants according to organizational level and position per the unit’s organizational chart.
Quantitative Analysis
I performed frequency calculations and χ2 analysis on the scaled response data obtained through the key informant interviews. Complete data are available by request. I examined the association of the quantitative variables by χ2 analysis (Table 2).
TABLE 2—
Chi-Square Analysis of Conceptual Model Elements: US State Health Department Chronic Disease Units, November 2012–March 2013
| Variable | Evidence-Based Decision-Making, χ2 (df) | Goal Ambiguity, χ2 (df) | Political Support, χ2 (df) | Responsiveness, χ2 (df) | Workforce Competency, χ2 (df) | Effectiveness, χ2 (df) |
| Collaboration | 22.49 (16) | 22.97* (12) | 28.97* (16) | 33.82* (16) | 8.77 (8) | 1.60 (4) |
| Evidence-based decision-making | 36.10* (12) | 16.44 (16) | 32.38* (16) | 9.91 (8) | 6.86 (8) | |
| Goal ambiguity | 13.64 (12) | 15.97 (12) | 7.48 (6) | 9.29 (6) | ||
| Political support | 8.48 (16) | 7.17 (8) | 5.41 (8) | |||
| Responsiveness | 5.84 (8) | 6.22 (8) | ||||
| Workforce competency | 2.54 (4) |
Note. df = degree of freedom.
*P ≤ .05.
Workforce competency and effectiveness did not show a statistically significant association with any of the model elements. Associations between collaboration and goal ambiguity, collaboration and political support, collaboration and responsiveness, evidence-based decision-making and goal ambiguity, and evidence-based decision-making and responsiveness each were statistically significant with at least 95% confidence levels. The nature of these relationships was unknown.
Qualitative Analysis
Aspects of the unit that were reported to facilitate collaboration included culture and a willingness to pitch in to help each other, open and regular communication, physical proximity to each other, and leadership at the section, unit, and department levels. External respondents noted specifically that the unit’s practice of approaching collaboration purposefully and strategically helped these partners understand how they could contribute, and trust that their time would not be wasted. The department’s new integrated performance management system was also identified as supporting collaboration. This system was organized around the work being done and not around the organizational structure.
Collaboration was influenced both negatively and positively by funder involvement, especially in the case of the CDC. The CDC National Center for Chronic Disease Prevention and Health Promotion is currently working to encourage coordinated chronic disease prevention and health promotion within state health departments. The state health department in this study is currently leveraging CDC’s grant for coordinated chronic disease prevention into support for collaborative approaches within the chronic disease unit. However, guidance from CDC’s categorical programs is sometimes at odds with broader collaboration, and rather than encourage a coordinated approach, it reinforces existing position bias related to categorical silos.
Collaboration was valued as a method to improve effectiveness. The collaborative culture of the chronic disease unit was credited with encouraging individuals to seek out advisers and peer-to-peer learning opportunities. This was true for learning new skills or quick information sharing, as well as longer term mentoring for new managers. This resulted in efficiency in data and information sharing that minimized the need for collaborators to “reinvent the wheel.”
Identifying an appropriate balance between specialization and shared tasks and expertise emerged as an important component of successful collaboration. Some specialist groups met across program areas. This allowed each individual to develop specialized knowledge in a program area and share skill-based knowledge across programs. Program-based finance analysts met regularly as a chronic disease unit-wide group. Epidemiologists met regularly in the chronic disease unit and regularly, but less often, across the state health department.
Evidence-Based Decision-Making
Nearly all respondents reported a clear expectation of evidence-based decision-making. Per unit culture and practice, the typical decision-making framework included documenting needs and pairing them with programs, processes, and interventions that had the strongest likelihood of success. Sources of evidence included peer-reviewed literature, Cochrane Reviews, the Guide to Community Preventive Services, the US Preventive Services Task Force recommendations, and guidance or direction from federal agencies, coalition and stakeholder recommendations, surveillance data, evaluation data, and performance forecasting. Logic models were identified as a tool to assist in evidence-based decision-making.
Translation was identified as a sometimes-difficult component of evidence-based public health practice. This seemed to be true when interventions existed, but were created for demographic characteristics that varied substantially from this state’s characteristics. Although traditional public health literature was frequently employed, literature and expertise from fields such as sociology and communications were not often used.
Positive influences on evidence-based decision-making included a culture of accountability, clear expectations, open and empowered leadership, weighing alternatives against program and unit goals, and frequent communication.
Goal Ambiguity
Most respondents rated proximal goals as having more clarity than distal goals. Although they stated that their immediate program goals were very clear, the objectives became less obvious at the unit level, and even less apparent at the state health department level.
Characteristics contributing to goal clarity included funder instructions defining goals, training offered by the CDC, the Public Health Accreditation Board accreditation preparation process, program maturity, coordination, and communication.
Political Support
Perceptions of political support were less concrete than those of other elements. Respondents expressed curiosity about the potential support from a newly elected administration. Communication, collaboration, and the new performance management system were identified as elements that had or could help strengthen political support.
Foundation, stakeholder, and advocate support were described as disorganized by both internal and external respondents. Support in this context did not reference funding for external partners, but rather referenced access to information, a shared agenda, and consistent messaging.
Responsiveness
Respondents attributed the responsiveness of the unit in part to strong leadership and a culture of collaboration and communication. Workforce capacity was built specifically to facilitate grant writing and procurement. The unit maintained a priority list of proposal topics ready to be matched with opportunities.
Challenges to responsiveness included a lengthy hiring process that impeded the ability to build staff capacity in a timely manner and created a lag time to start new activities. The data collection and reporting process could also be slow, which resulted in data that were not as current as decision-makers and funders would have liked it to be. Occasionally, the strategies used to ensure responsiveness were met by resistance from funders (e.g., securing contractors) to begin work on a grant-funded project during a hiring freeze.
Workforce Competency
Of the 37 unit employees, 6 had a master’s in public health. An additional 4 unit employees had public health education other than a master’s in public health. Other public health education experience reported included health education, health promotion, community health management, and public health certificates.
There was clear support from leadership for training, but it was largely left up to individuals to identify their own needs and find appropriate opportunities to fulfill their needs. Out-of-state travel was prohibited, but leadership was willing to approve vacation requests so that staff could use their own time and resources to access out-of-state opportunities. This policy was not feasible for everyone. The travel restriction isolated this state’s chronic disease staff, prevented them from attending national training sessions and networking with peers from other states, and decreased their access to cutting edge public health practices.
Currently, the unit has begun to look at workforce competency systematically, and has developed training opportunities accordingly, including a communications training and an epidemiology journal club. In addition, the state health department is planning a comprehensive workforce competency assessment in spring 2015 as part of the accreditation preparation process.
Performance
Respondents were asked to identify evidence of effectiveness, recommendations to improve effectiveness, and recommendations for an ideal structure to facilitate effectiveness. Indicators of effectiveness cited by respondents included visibility in the media, implementation of evidence-based programs, progress toward grant objectives, and documentation of meeting quantifiable outcomes. Effectiveness ratings were high overall and highest at the program level, and once again increased with proximity.
DISCUSSION
My study served both to document a point in time for a particular chronic disease unit and to explore the elements of the conceptual model that might facilitate effectiveness for chronic disease units in other states, other units within state health departments, and public health agencies at other levels. The results of the qualitative and quantitative analysis suggested interrelationships between the elements of the model rather than a simple linear cause and effect pathway. These findings suggested levers around which capacity could be built that might strengthen effectiveness. The limitations of this study precluded conclusions regarding causality among the conceptual model elements and the potential magnitude of effects. Translations of these results to another chronic disease unit might be complicated by contextual factors that were outside of the scope of this study, such as geography, economics, and demographic characteristics. More research is needed.
Characteristics that respondents associated with effectiveness included elements of the conceptual model: collaboration, evidence-based decision-making, goal ambiguity, hierarchical authority, and workforce competency. By contrast with the correlation analysis, the qualitative data supported the model proposed by Stazyk and Goerdel16 and suggested that goal ambiguity and low political support could undermine effectiveness.
Although the quantitative analysis did not show a significant association between effectiveness and any of the elements in the conceptual model, qualitative response indicated a belief that evidence-based decision-making, goal ambiguity, political support, responsiveness, and workforce competency all facilitated effectiveness, and that collaboration facilitated each of these elements. Structure was identified as an influence on collaboration, responsiveness, goal ambiguity, and hierarchical authority. However, culture, leadership, and physical proximity also emerged as elements that might play a role that might mitigate the effects of structure, enhance the effects of structure, or be amplified by structure.
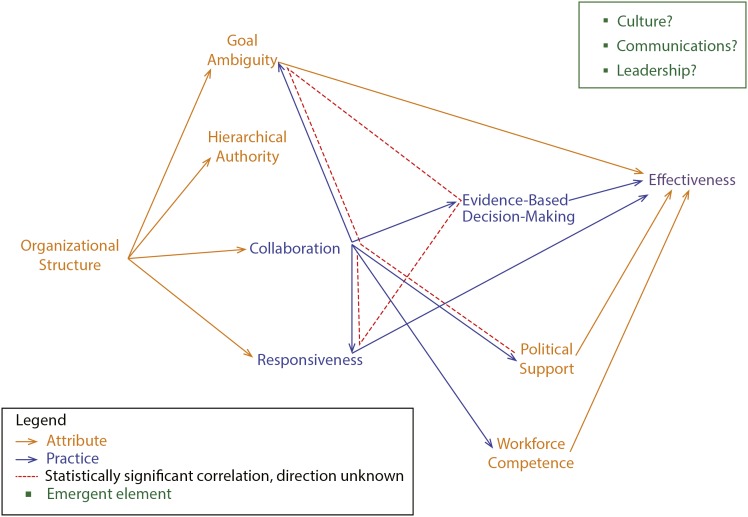
The results of my case study examination suggested that the conceptual model elements were related to each other. The qualitative analysis suggested additional relationships among the attribute and practice elements examined in my study; however, causality could not be determined. In concordance with Stazyk and Goerdel, my results suggested that political support and goal ambiguity influenced effectiveness, but there were no findings regarding a relationship between hieratical authority and political support or goal ambiguity or between hierarchical authority and effectiveness. I did not prove that the model proposed by Stazyk and Goerdel could not be appropriately applied to state health department chronic disease units; this is an area that requires further study. The practice element collaboration influenced the other 2 practice elements (evidence-based decision-making and responsiveness) and 2 of the attribute elements (political support and workforce competency). The attribute element organizational structure influenced 2 practice elements (collaboration and responsiveness) and 1 attribute element (hierarchical authority). Two practice elements (evidence-based decision-making and responsiveness) and 3 attribute elements (goal ambiguity, political support, and workforce competency) influenced effectiveness.
However, the pathway of effect was more complicated than proposed in the original conceptual model. The simplified original conceptual model proposed that attribute elements might influence practice elements, and together, these might influence organizational performance, and therefore, public health effectiveness. It seemed rather that there might be a direct interrelationship between some of the practice elements and that some attribute elements might contribute directly to effectiveness (Figure 2). Three additional factors (culture, communications, and leadership) emerged as influencing effectiveness, but their position and role in the conceptual model was unclear.
FIGURE 2—
Organizational attributes and practices relationships in state health department chronic disease units.
A synthesis of the analysis yielded answers to the 4 research questions.
Structure of the Chronic Disease Prevention and Control Unit
The formal reporting structure of the Bureau of Chronic Disease Prevention and Health Promotion, as documented previously, included more leadership and specialized skill capacity at the individual program level than other bureaus in the Division of Public Health and Safety. This structure was believed to be supportive of program specific specialization that complements collaborative approaches.
Perceptions of the Unit’s Effectiveness
Managers, internal stakeholders, and external stakeholders were in agreement that the Bureau of Chronic Disease Prevention and Health Promotion performance was somewhat to very effective. In general, respondents rated program effectiveness above bureau effectiveness and bureau effectiveness above division effectiveness. This might be related to a similar finding regarding goal ambiguity. Goal ambiguity increased from program to bureau to division. As goal ambiguity increased, understanding of performance goals might decrease, which, in turn, might decrease a respondent’s confidence that the goals were being met effectively.
Structural Factors That Influence the Unit’s Effectiveness
Structure supported collaboration when potential collaborators were proximal to each other in terms of where they sat in the building, where they resided in the organizational chart, and how closely aligned their task and content expertise were.
Respondents appreciated the program specialization inherent in the formal structure and cited this as complementary to collaborative activities. Three formal collaboration initiatives were cited as facilitating effectiveness: epidemiology networking, finance and logistics networking, and the Coordinated Chronic Disease Program.
Epidemiology networking.
The presence of epidemiology staff embedded in programs was identified as a strength of the bureau, by enabling the rapid and systematic use of data for decision-making. This was coupled with regular meetings that allowed epidemiologists to learn from and support each other. This was structured in part around a journal club that allowed participants to apply knowledge in ways that might be different from their day-to-day work, and therefore, could help them build skills.
Finance and logistics networking.
The finance and logistics specialists met regularly, as the epidemiologists did. This meeting was designed to assist in problem solving and identify systems-level changes to support systems improvement bureau-wide.
Coordinated Chronic Disease Program.
The Coordinated Chronic Disease Program took leadership for identifying opportunities for collaboration that might enhance bureau effectiveness. Using communication strategies, this program facilitated connections that leveraged the specialization and general skill areas that each program might benefit from.
Consistency With the Conceptual Model
Although the correlation analysis did not show a significant association between effectiveness and any of the elements in the conceptual model, qualitative response indicated a belief that evidence-based decision-making, goal ambiguity, political support, responsiveness, and workforce competency all facilitated effectiveness and that collaboration facilitated each of those elements. Structure was identified as an influence on collaboration, responsiveness, goal ambiguity, and hierarchical authority. However, culture, leadership, and physical proximity also played a role that might mitigate the effects of structure, enhance the effects of structure, or be amplified by structure.
Conclusions
State and local health departments, schools of public health, and other practice leaders each have an important role to play in furthering this work. Within state health department chronic disease units, creating a culture that values evidence-based innovation, communicating a clear vision, and employing collaborative leadership practices will be instrumental for chronic disease directors who seek to strengthen the effectiveness of their units. Schools of public health and other academic institutions are in a unique position to influence the evolution of practice-based research and literature, and to prepare future public sector public health leaders for success. Practice leaders in national organizations and federal agencies and their partners can support technical assistance, strategic leadership, and organizational capacity development that align with the emerging evidence base. The voluntary accreditation process in progress under the direction of the Public Health Accreditation Board offers further opportunity to build the science informing our understanding of the levers of organizational effectiveness in public health. New wisdom emerging from each of these efforts, the practice-based literature growing out of new applications of quality improvement methods, and longitudinal observation of accreditation measures will allow us to continue studying the organizational attributes and practice elements of the conceptual model investigated in this case study on a larger scale.
Acknowledgments
I wish to thank all those working in state health departments and especially the volunteers who graciously agreed to participate in this study. Thanks also to Todd Harwell and Ginny Furshong who assisted with volunteer recruitment and provided feedback on preliminary results; Wendy Sarratt and Maggie Moore who provided critical editorial support; and Leslie Best, Leah McCall Devlin, Sandra Greene, Suzanne Havala Hobbs, and Rebecca Wells, who advised this work as members of my doctoral dissertation committee.
Human Participant Protection
Expedited institutional review board approval was obtained for this study from the University of North Carolina, Chapel Hill.
References
- 1.Stazyk EC, Goerdel HT. The benefits of bureaucracy: public managers’ perceptions of political support, goal ambiguity, and organizational effectiveness. J Public Adm Res Theory. 2011;21(4):645–672. [Google Scholar]
- 2.Slonim AB, Callaghan C, Daily L et al. Recommendations for integration of chronic disease programs: are your programs linked? Prev Chronic Dis. 2007;4(2):A34. [PMC free article] [PubMed] [Google Scholar]
- 3.Bender K, Benjamin G, Carden J et al. Final recommendations for a voluntary accreditation program for state and local health departments: steering committee report. J Public Health Manag Pract. 2007;13(4):342–348. doi: 10.1097/01.PHH.0000278026.49196.40. [DOI] [PubMed] [Google Scholar]
- 4.Slonim A, Wheeler FC, Quinlan KM, Smith SM. Designing competencies for public chronic disease practice. Prev Chronic Dis. 2010;7(2):A44. [PMC free article] [PubMed] [Google Scholar]
- 5. The Council on Linkages. Core competencies for public health professionals. 2014. Available at: http://www.phf.org/resourcestools/Pages/Core_Public_Health_Competencies.aspx. Accessed February 8, 2015.
- 6.Bhandari MW, Scutchfield FD, Charnigo R et al. New data, same story? Revisiting studies on the relationship of local public health systems characteristics to public health performance. J Public Health Manag Pract. 2010;16(2):110–117. doi: 10.1097/PHH.0b013e3181c6b525. [DOI] [PubMed] [Google Scholar]
- 7.Erwin PC, Greene SB, Mays GP et al. The association of changes in local health department resources with changes in state-level health outcomes. Am J Public Health. 2011;101(4):609–615. doi: 10.2105/AJPH.2009.177451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hajat A, Cilenti D, Harrison LM et al. What predicts local public health agency performance improvement? A pilot study in North Carolina. J Public Health Manag Pract. 2009;15(2):E22–E33. doi: 10.1097/01.PHH.0000346022.14426.84. [DOI] [PubMed] [Google Scholar]
- 9.Scutchfield FD, Mays GP, Lurie N. Applying health services research to public health practice: an emerging priority. Health Serv Res. 2009;44(5 pt 2):1775–1787. doi: 10.1111/j.1475-6773.2009.01007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Prevention Council. National prevention strategy. June 2011. Available at: http://www.surgeongeneral.gov/initiatives/prevention/strategy. Accessed October 28, 2014.
- 11. Department of Health and Human Services, Centers for Disease Control and Prevention. Prevention and Public Health Fund Coordinated Chronic Disease Prevention and Health Promotion. 2011. Available at: http://www.grants.gov/web/grants/view-opportunity.html?oppId=98533. Accessed October 28, 2014.
- 12.Beitsch LM, Brooks RG, Grigg M, Menachemi N. Structure and functions of state public health agencies. Am J Public Health. 2006;96(1):167–172. doi: 10.2105/AJPH.2004.053439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Association of Chronic Disease Directors. Workshop Summary Report. Presented at: Workshop on Chronic Disease Program Integration; March 29–30, 2006; Atlanta, GA.
- 14.Anderson LM, Brownson RC, Fullilove MT et al. Evidence-based public health policy and practice: promises and limits. Am J Prev Med. 2005;28(5 suppl):226–230. doi: 10.1016/j.amepre.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175–201. doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- 16.Dodson EA, Baker EA, Brownson RC. Use of evidence-based interventions in state health departments: a qualitative assessment of barriers and solutions. J Public Health Manag Pract. 2010;16(6):E9–E15. doi: 10.1097/PHH.0b013e3181d1f1e2. [DOI] [PubMed] [Google Scholar]
- 17.Mays GP, McHugh MC, Shim K et al. Institutional and economic determinants of public health system performance. Am J Public Health. 2006;96(3):523–531. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mullahy J. Understanding the production of population health and the role of paying for population health. Prev Chronic Dis. 2010;7(5):A95. [PMC free article] [PubMed] [Google Scholar]
- 19.Yin RK. Case Study Research Design and Methods. 4th ed. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 20.Ballew P, Brownson RC, Haire-Joshu D . Dissemination of Effective Physical Activity Interventions: Are We Applying the Evidence? Health Education Research. Oxford, UK: Oxford University Press; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gist ME, Locke EA, Taylor MS. Organizational behavior: group structure, process, and effectiveness. J Manage. 1987;13(2):237–257. [Google Scholar]
- 22.Greenhalgh L. Maintaining organizational effectiveness during organizational retrenchment. J Appl Behav Sci. 1982;18(2):155–170. doi: 10.1177/002188638201800204. [DOI] [PubMed] [Google Scholar]
- 23.Kimberly JR, Rottman DB. Environment, organization, and effectiveness: a biographical approach. J Manage Stud. 1987;24(6):595–622. [Google Scholar]
- 24.Centers for Disease Control and Prevention. Promising Practices in Chronic Disease Prevention and Control: A Public Health Framework for Action. Atlanta, GA: Department of Health and Human Services; 2003. [Google Scholar]
- 25.Barnett DJ, Balicer RD, Blodgett D et al. The application of the Haddon Matrix to public health readiness and response planning. Environ Health Perspect. 2005;113(5):561–566. doi: 10.1289/ehp.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bender K, Halverson PK. Quality improvement and accreditation: what might it look like? J Public Health Manag Pract. 2010;16(1):79–82. doi: 10.1097/PHH.0b013e3181c2c7b8. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine–Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press; 2003. [Google Scholar]
- 28.Institute of Medicine–Committee for the Study of the Future of Public Health. The Future of Public Health. Washington, DC: The National Academy Press; 1988. [Google Scholar]
- 29. US Department of Health and Human Services, Public Health Service. Healthy People 2020: Public health infrastructure. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/public-health-infrastructure. Accessed October 28, 2014.
- 30.Liber E. Mixing qualitative and quantitative methods: insights into design and analysis issues. J Ethnogr Qual Res. 2009;3:218–227. [Google Scholar]
- 31.Boyatzis R. Transforming Qualitative Information. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 32.Creswell JW. Research Design–Qualitative, Quantitative, and Mixed Methods Approaches. 2nd ed. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- 33.Miles & Huberman. Qualitative Data Analysis–An Expanded Sourcebook. 2nd ed. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]