Abstract
Objectives. We studied simulated interventions that leveraged social networks to increase physical activity in children.
Methods. We studied a real-world social network of 81 children (average age = 7.96 years) who lived in low socioeconomic status neighborhoods, and attended public schools and 1 of 2 structured afterschool programs. The sample was ethnically diverse, and 44% were overweight or obese. We used social network analysis and agent-based modeling simulations to test whether implementing a network intervention would increase children’s physical activity. We tested 3 intervention strategies.
Results. The intervention that targeted opinion leaders was effective in increasing the average level of physical activity across the entire network. However, the intervention that targeted the most sedentary children was the best at increasing their physical activity levels.
Conclusions. Which network intervention to implement depends on whether the goal is to shift the entire distribution of physical activity or to influence those most adversely affected by low physical activity. Agent-based modeling could be an important complement to traditional project planning tools, analogous to sample size and power analyses, to help researchers design more effective interventions for increasing children’s physical activity.
Although tremendous resources have been used to address the obesity epidemic, most interventions have been disappointing. Leading scientists and the National Institutes of Health have called for the application of system science methods for obesity prevention and treatment.1,2 The multiple, interdependent, nonlinear, and often time-delayed forces that sustain the obesity epidemic are too complex to reverse by focusing attention on an individual’s behavior change, without concurrently addressing change in the larger systems within which that individual is embedded.2–5
Social network analysis and agent-based modeling are 2 methods used to analyze and understand complex systems. Analysis of social networks can uncover how relationships constrain or enable our health behaviors, and how health behaviors shape which relationships we make or break. Agent-based models are social simulation models that can extend network models to predict future behavior from explicitly programmed, microlevel rules. In this article, we discussed the application of these models to obesity research, highlighted their utility in understanding social contagion (i.e., behavior spread), and identified scenarios that leveraged social contagion to accelerate behavior change.
A “network intervention” uses social network data to achieve behavior change.6 In a 2009 article, Bahr et al. used a cellular automata model to demonstrate that anti-obesity network interventions might require highly complex interventions, including locating the edges of network clusters and including “friends of friends” in the intervention.7 This novel study was limited by a focus on a highly regular grid lattice network that might not correspond to real-world networks. Recently, El-Sayed et al. used agent-based simulation models in which artificial individuals were nested in a preferential attachment8 social network to examine the potential for network interventions to reduce obesity.9 The results suggested no added benefit on reducing population obesity rates using such interventions. Shortly thereafter, de la Haye critiqued several of the assumptions underlying the models of El-Sayed et al. for failing to reflect robust networks effects (e.g., obesity is not distributed at random in real-world networks; obese individuals tend to be connected to each other and marginalized in larger social networks).10
Those studies evaluated network interventions in which an actor in the model was “treated” (lost weight) and examined how that influenced people in their social network to lose weight (or not become overweight). The mechanisms underlying behavior spread were generally unexamined. Social norms are thought to at least partially account for the network effects on obesity. Leahey et al. presented the first research to explicitly test this assumption. Their findings suggested that social norms specific to one’s social network (subjective norms) influenced weight more than broad societal-level social norms (injunctive norms).11 In addition to conformity to group norms, there were other mechanisms that that might explain the effect of networks on behaviors associated with obesity (e.g., physical activity), including social facilitation, social learning, social comparison, social support, coercion, or competition. There is strong experimental, network, and theoretical literature that has shown that social networks (peers, family) influence physical activity in adolescents.12–14
Multiple studies now suggest that network interventions to increase physical activity are warranted.7,15–22 This becomes important in light of a recent meta-analysis that provided strong evidence that physical activity interventions to date have had small effects (amounting to an increase of 4 minutes of activity per day).23 We recently demonstrated that children in afterschool programs adjusted their physical activity depending on the activity level of their friendship network.22 These activity adjustments were 10% or greater and greater than 6 times more likely to happen than not, which suggested that children’s activity levels could be improved by intervening on their friendship network.
We used computer simulations to test the expected outcome of implementing a network intervention to increase children’s physical activity by using a real-world social network that objectively measured physical activity, and we used agent-based modeling to test the comparative effectiveness of 3 intervention strategies. Accounting for network effects, we compared 3 intervention scenarios in an afterschool setting by (1) intervening on the most sedentary children within the network, (2) intervening on a random selection of children within the network, and (3) intervening on the most central, connected, or popular children within the network.
We chose these intervention scenarios for the following reasons. First, they are theoretically amenable to a network intervention. The most sedentary children were selected because there is evidence that they can bring down the physical activity levels22 of their immediate circle of friends in the afterschool setting. The most popular children were selected because some individuals (“opinion leaders”) play an especially important role in diffusion of disease and other contagion processes, including norms.24 Opinion leaders have more incoming ties relative to others in the network; thus, they have more social power and control over behavior spread.25 Network interventions that leverage opinion leaders as change agents have been implemented in contexts as diverse as preventing substance use,26 reducing HIV risk behavior,27 and implementing clinical practice guidelines,28 but these intervention have not yet been used for obesity-related behavior. Because of the success of this approach in other settings (albeit in adolescents and adults), we hypothesized that it would produce a greater effect than intervening on children at random or focusing efforts on those in greatest need of intervention. Second, we also chose these 3 intervention strategies for their simplicity of execution; program staff in an afterschool setting might easily identify the most well-connected and the most sedentary children without requiring the specialized knowledge necessary for collecting and analyzing complete social networks. Comparing simulated intervention scenarios allowed us to estimate the effectiveness of these network interventions before real-world implementation.
METHODS
The data used in this study were collected from February to May 2010. Parents provided written consent and children provided written assent. Our sample consisted of 81 children, who were a mean age of 7.96 years (SD = 1.74 years); 56% were at a healthy weight, 23% were overweight, 21% were obese, 40% were African American, 39% were White, 19% were Latino, and 65.4% were female. The children lived in low socioeconomic neighborhoods, and attended public schools and 1 of 2 afterschool programs.
Each afterschool program operated Monday through Friday (3:00–6:00 pm), and allotted time for play, homework, and snacks. One program was based in a community center, and the other was based in a school. Both programs enrolled children from the school in which the school-based program was located, as well as children from other schools in the area. Two waves of data, collected 6 weeks apart, were used. This data set was described in detail elsewhere.22
Measures
Anthropometrics.
We weighed each child while they wore light clothing without shoes, and after voiding, to the nearest 0.1 kg on a calibrated digital scale (model 758C; Detecto, Webb City, MO). We used the attached stadiometer to measure height (without shoes) to the nearest 0.1 cm. Children with a body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) 95th percentile or greater (using the Centers for Disease Control and Prevention calculator)29 were classified as obese.
Physical activity.
We captured physical activity levels through ActiGraphGT1M accelerometers (ActiGraph LLC, Pensacola, FL). The ActiGraph is an unobtrusive, lightweight activity monitor worn on a belt around the waist. It captures the intensity of physical activity from locomotion in continuous 10-second periods to capture the short activity bursts characteristic of children. For each wave of measurement, children wore monitors for 5 consecutive days from the time they entered the afterschool program to the time they left. We used empirically validated thresholds to code each child’s time spent at sedentary, light, moderate, and vigorous activity levels.30,31 We analyzed raw accelerometer data using a procedure analogous to that used with the National Health and Nutrition Examination Survey data.32 Details of the physical activity measurements were described previously.22
The total amount of time coded in sedentary behavior or physical activity was calculated by summing the total number of minutes each day the monitors were worn that met the predefined criterion count for each level of intensity. For each level of intensity, daily averages were calculated using data from all days of measurement. The hours of program-related playtime recorded in each afterschool program were used as cutoff points to accurately capture when children had free choice over their level of activity (playtime) versus structured sedentary periods (snack and homework times).
Each child spent varying amounts of total time in afterschool care, depending on family work schedules. Accordingly, the main outcome measure in our study was the overall proportion of free playtime recorded in moderate-to-vigorous physical activity (MVPA) as opposed to the raw number of minutes in MVPA. Although the outcome of interest was measured as a continuous variable, certain limitations of the analysis procedure used to derive initial model estimates (SIENA)33 required transformation to a categorical outcome variable. Accordingly, we recoded the continuous outcome measure into deciles of the percentage of each child’s playtime spent in MVPA: 0% to 9%, 10% to 19%, up to 100%.
Social network.
We mapped each child’s social network using an open-ended survey instrument, administered through private one-on-one interviews. We asked each student, “Please tell me the names of the friends you hang around with and talk to and do things with the most here in this after-school program.” No restrictions were placed on the number of friends each child could name. This name generator was consistent with those used in other youth social network studies and had predictive validity for obesity-related behaviors (diet, exercise).16 We referred to each student who provided activity data and completed the social network survey as the “ego,” and referred to their named friends as “alters.” We surveyed children at each wave of data collection to capture each child’s most salient friendships at each time point. The total number of friends in each child’s network included those friends that each ego nominated and nominations received from others. We did not find significant differences in parameter estimates between sites22 and concluded that the parameter estimates were homogenous. To maximize available statistical power, sociometric data from each afterschool setting (n = 46 and n = 35, respectively) were merged into a single network of 81 children. Ties among children who did not attend the same afterschool program were coded as “structural zeros.”33 This combination of sociometric data sets assumed that the dynamics of friend selection and influence on activity level operated similarly among children in each afterschool setting.
Each wave of network and physical activity data were analyzed using the stochastic actor-based methods in SIENA version 4.0.33 An important assumption of actor-based modeling is that changes observed in social ties and behaviors over time result from the actors’ attempts to optimize their network position at a given time point. The observed behavior and networks collected in panel data are assumed to be the outcomes of an underlying continuous-time Markov process. In other words, between each of the network and activity states observed at each measurement occasion, a number of incremental (unobserved) changes occur, which give rise to the observed states.34 The estimation algorithm of SIENA derives the most likely series of microchanges that occur between observed waves of data. Model parameters represent the various rules that govern such microchanges. This method is described in more detail elsewhere.34–36 Our SIENA models were described previously.22
Model Specifications
Agent-based modeling allowed us to model individual agents, give them certain characteristics, and then observe the resulting network change and behavior change of each individual. This allowed us to compare the network and behavior dynamics under different scenarios. Thus, we built an agent-based model to simulate the behavior change (physical activity) and network change (making and breaking of friendship ties) in 2 afterschool programs (2 networks) using parameters from our empirical SIENA model that were published elsewhere.22 We used NetLogo for all simulations37; a thorough description and example of how to incorporate SIENA parameters into NetLogo code is available elsewhere.38 We then examined the effects of interventions that focused on controlling the behavior of different groups of individuals (see the section on “Experiments”).
Agent-based models are computer simulations of synthetic agents (e.g., molecules, individuals, companies). Our models’ agents represented individual children in the empirical study. The elements of any agent-based model included Properties of agents, Actions, Rules for behavior, Time, and Environment (PARTE) specifications (R. Hammond, confirmed by personal communication, October 20, 2014).39 The agents in our models had the following properties: age, gender, race, and obesity status. The focal Action was the physical activity level. The agents followed a stochastic Rule of matching the average behavior (“average similarity” on activity level) of their friends: whether their friends were more, less, or at the same activity level, the agent would increase, decrease, or maintain their activity level. Time was specified according to the rate function from SIENA: on average, agents made 9.3 network choices (make, keep, or break a network tie) and 2.3 behavior choices (up, same, or down in the MVPA decile). The Environment was specified at 4 levels: (1) the agents’ social network, whereby other agents constituted the social environment of each agent; (2) the presence or absence of a sibling in the network; (3) attending the same school; and (4) the boundary of the network, which was the afterschool program.
All parameters from the empirical SIENA model were included in the agent-based model. The network parameters included out-degree (number of friends named), reciprocity, transitive triplets (friendship ties with an agent who was a friend of a friend), 3 cycles, same household, same school, same gender, same age, and same race. We assumed that agents made network decisions based both on whether they shared race and other characteristics and their structural positions within the network. The behavior parameters included linear shape (propensity for those who started with high levels of MVPA would continue at a high level), quadratic shape (increased probability for those with low MVPA or high MVPA would decrease or increase activity), obesity, age, program site, out-degree and in-degree ties (those who named the agent), and average similarity (compared with their average friends’ physical activity). The key behavioral parameter was average similarity or the tendency to assimilate to an alter’s behavior. The model simulated 6 weeks of behavior change.
Model Verification
We ran the simulation 100 times and compared the simulation results to target statistics in real-world data to validate and verify the model. Multiple model runs were required to rule out chance as an explanation for any particular run’s results, because the model was based on a stochastic process. These target statistics included the distribution of out-degree, number of tie changes and transitive triplets, and the final distribution of MVPA at the end of the model run.
We used box-and-whisker plots of the distribution to capture the median, 25th, and 75th percentiles of the target statistics across the model runs; whiskers represented 1.5 times the interquartile range above and below the box. In verified models, the observed distribution of target statistics should fall within these box-and-whisker plots (ideally within the boxes themselves). We called this model the “base-case” scenario.
Experiments
After verifying that the model matched observed patterns in the network and behavior, we defined 3 experimental scenarios and ran each simulation 100 times.
Scenario 1.
We increased the MVPA of children whose MVPA was less than 3 (below the third decile) to 3. This increase in physical activity was informed by our empirical data and the constraints of an afterschool program structure. We selected this parameter because the average MVPA in this real-world setting was 3.039. We wanted to examine reasonable behavior changes as opposed to ideal, yet unlikely, scenarios, in which, for example, we set children’s activity levels at extreme values, which have not documented in this type of afterschool setting. This parameter selection resulted in a new average MVPA of 3.607. This modeled a high-risk intervention, in which the most sedentary children became more active, but others were left unchanged.40 Such an intervention might be implemented through active involvement of adults with these high-risk children. We referred to this as the “sedentary target scenario.”
Scenario 2.
MVPA of randomly selected individuals was increased by 1 decile, to make the initial average MVPA equal to that in scenario 1 (3.607). We kept the increase in physical activity the same across the 3 scenarios so that comparisons were fair and meaningful; what changed among the scenarios was where in the network we initiated behavior change (among the most sedentary vs random vs most popular children). We then quantified the ripple effects that the initial change had on the other children in the network. Thus, in this scenario, a randomly chosen subset was shifted to a higher level of physical activity. Such an intervention could be implemented by having adults coach randomly selected children to become more active. We referred to this as the “random scenario.”
Scenario 3.
MVPA of 46 well-connected children (those with the highest in-degree) was increased by 1 decile to make the initial average MVPA equal in all 3 scenarios. Such an intervention could be implemented by having children identify the most popular children, and adults then coaching those children to become more active. We referred to this as the “opinion leader scenario.” Opinion leaders might be sedentary or active.
The core ingredient of all 3 interventions was to produce an increase in physical activity in particular children to achieve a ripple effect on the remainder of the network. How that behavior change was achieved in the children selected as “seeds” (incentivizing certain children, having energetic adults engage or coach particular children, offering activities favored by certain children, encouraging certain children, etc.) was immaterial in this computer simulation. Here, our focus was in seeding behavior change in different positions in the network and quantifying the effect that had on other children in the network.
Post Hoc Tests
In situations where data are a sample from a larger population, the central limit theorem states that the sample will converge to the true population mean (or true mean difference between populations) as the sample size increases. However, in our study, there was no limit to the number of simulations that could be run. We compared counterfactual scenarios based on the same real-world population. Therefore, we did not employ formal hypothesis testing; instead, we used qualitative comparisons between original estimates and the 3 experimental scenarios.
RESULTS
We verified that the model could capture the essential features of the network and behavior: out-degree and physical activity level (data available as a supplement to the online version of this article at http://www.ajph.org). Out-degree of the simulated network runs matched most of the empirical distribution (data available as a supplement to the online version of this article at http://www.ajph.org), with the observed distribution falling within the whiskers of the box plot. However, the model underestimated the number of children with low out-degree and overestimated those with high in-degree. Although the model did not fully capture the degree distribution of the empirical social network, the distribution of physical activity at the end of the model run was similar to the empirical distribution at the end of the study (data available as a supplement to the online version of this article at http://www.ajph.org), with nearly all levels of MVPAs falling within the boxes of the plots. This gave us confidence that results for both the network and behavior aspects of the model were accurate representations.
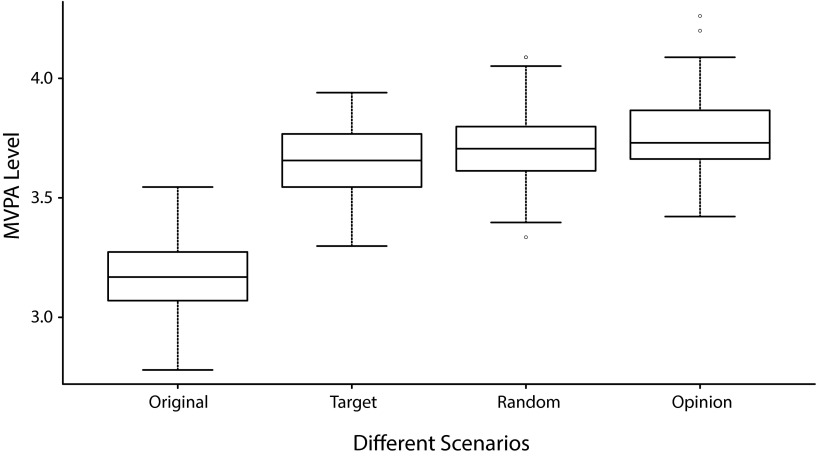
The amount of scheduled playtime children would be expected to spend in MVPA differed with each scenario (data available as a supplement to the online version of this article at http://www.ajph.org). The average amount of time spent in MVPA was higher in the opinion leader scenario (mean = 3.77; SD = 0.16) than that in the sedentary target scenario (mean = 3.65; SD = 0.15) or that in the random scenario (mean = 3.60; SD = 0.14).
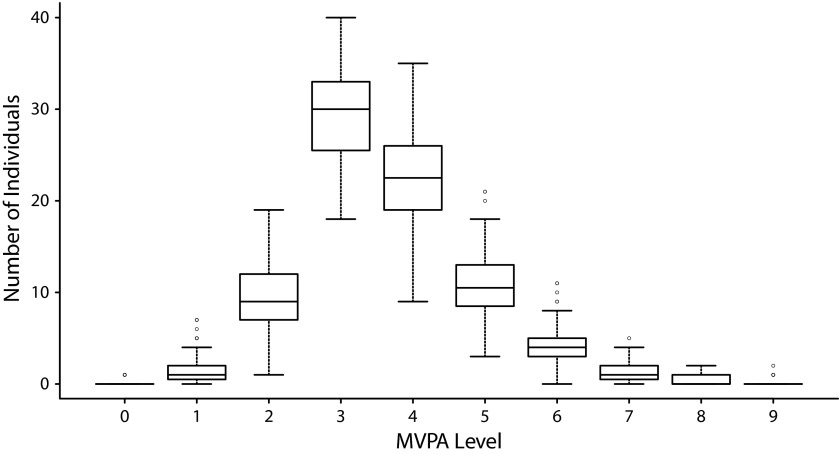
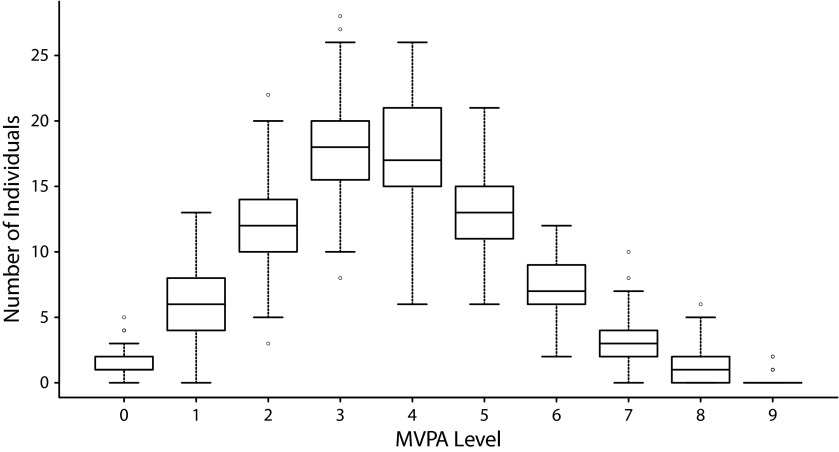
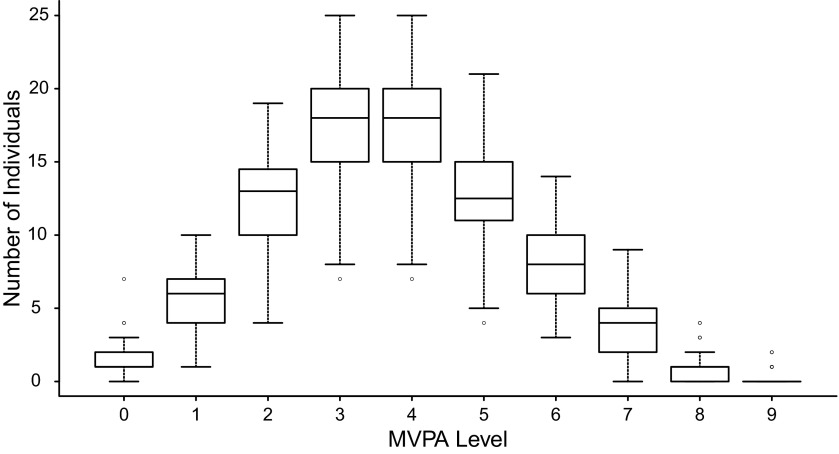
Although the intervention that targeted the opinion leaders was most effective in increasing the average level of physical activity across the entire network, it did not make the least active children more active. Figures 1 through 4 show the distribution of MVPA in each intervention scenario, both aggregated (Figure 1) and broken down into discrete deciles of MVPA for the sedentary targeted (Figure 2), random (Figure 3), and opinion leader (Figure 4) scenarios. The intervention that intentionally targeted the most sedentary children was the most effective in increasing the physical activity levels of these high-risk children, although it did not increase the average level of activity across the entire network as much as the opinion leader intervention.
FIGURE 1—
Comparison of mean moderate-to-vigorous physical activity (MVPA) under different scenarios (100 runs): February–May 2010.
FIGURE 2—
Mean moderate-to-vigorous physical activity (MVPA) distribution in sedentary target scenario: February–May 2010.
FIGURE 3—
Mean moderate-to-vigorous physical activity (MVPA) distribution in random scenario: February–May 2010.
FIGURE 4—
Mean moderate-to-vigorous physical activity (MVPA) distribution in opinion leader scenario: February–May 2010.
DISCUSSION
Our study was the first that we know of to use agent-based modeling based on an empirically observed network and objective measures of physical activity. Previous work examined self-reported physical activity and network change,15,20 but it did not examine simulated interventions based on the results. Work by El-Sayed et al.9 and Bahr et al.7 examined obesity interventions on stylized networks, including a grid lattice7 and a preferential attachment model.9 Although these were useful approaches for guiding theoretical development involving networks, they were not grounded in observed networks. Our study employed a real-world network and its dynamics to explore interventions that might actually be planned for the field.
Simulation could identify promising strategies and rule out less promising ones. Our work demonstrated that network interventions that leveraged friendship networks could be effective in increasing physical activity in the afterschool setting, but they might be most effective when the objective is to shift the mean of the whole distribution of behavior. According to our scenarios, an intervention that leveraged the natural influence of the most popular children within an afterschool program should increase physical activity across the program. However, the least active children might be unaffected by such a network intervention if they are socially marginalized.10,41 If the objective was to reach high-risk individuals, then targeting physical inactivity might be most appropriate.40
This was the first study to examine the role of popular children in shaping other children’s physical activity.17 The diffusion of innovations model by Rogers42 provided a framework to understand how ideas and behaviors could spread. According to Rogers, opinion leaders lead behavior change, but are not typically the first to advocate or adopt new behavior, because doing so might have social repercussions and jeopardize their leadership position. Rather, opinion leaders tend to monitor popular opinion and exert their influence to move others to change their behavior when the advantages of the behavior change are clear or when it is clear that social norms will be shifting.
Afterschool programs for children of working parents are an understudied yet promising venue for physical activity interventions, because of their reach into “a captured audience” and the potential for high dosage (5 days a week during the school year) without the common implementation challenges of attrition caused by transportation, waning interest, et- cetera. A systematic review of the effectiveness of afterschool programs in increasing physical activity demonstrated significant positive effects for critical obesity- and diabetes-related behaviors and clinical outcomes (specifically, physical activity, physical fitness, body composition, and blood lipids).43 Afterschool interventions that leverage existing network dynamics might increase these documented effects on health. Furthermore, agent-based modeling could be used to evaluate network interventions for older youths and adults before implementation in the field.
Strengths and Limitations
Our study demonstrated 1 application of agent-based modeling, namely, simulated network interventions. Comparisons between network interventions were not possible on single networks, primarily because of violations of treatment-unit independence. Although network interventions were compared across networks by Valente et al.,44 very little real-world work has been conducted in this area. Our work provided a bridge between real-world network interventions and pure simulations, such as those by Bahr et al.7 and El-Sayed et al.,9 and addressed the critique by de la Haye that such models might not be faithful representations of the ways that networks shape healthy and unhealthy behaviors.10
Our results had several limitations. First, the SIENA model did not appear to faithfully capture the degree distribution of the empirical network at the end of the study period. Compared with the observed data, the model underestimated the number of children with low out-degree and overestimated those with high in-degree. More terms could always be added to the model to improve fit, but the fundamental problem might be the architecture of SIENA itself, because of its basis on exponential-family utility functions.45 Nevertheless, SIENA is the best tool available to model both behavior and network change processes. Furthermore, we excluded other social influences (parents, built environment, teachers, policy environment) from the model to focus on peer influences. We hope to add such influences in future modeling efforts. Finally, the model faithfully captured the final MVPA distribution of the empirical data. Because we used simulation to test various scenarios, we do not know the effect size of the proposed interventions in a real-world setting.
Conclusions
We expected an afterschool intervention that targeted highly connected children to increase physical activity more effectively across program participants, compared with an intervention that targeted sedentary or randomly selected children. However, which intervention to implement depends on whether the goal is to shift the entire distribution or to influence those most adversely affected by low physical activity. Agent-based modeling could be an important complement to traditional project planning tools (sample size calculations and power analyses) to help researchers design more effective interventions to increase children’s physical activity.
Acknowledgments
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Development (award number K23HD064700), and the Modeling Obesity through Simulation (MOTS) grant, US National Institutes of Health-National Institute of Child Health and Development (NIH-NICHD; R01-HD-061978-0109). Furthermore, this work was done as part of the Envision Project, supported by the National Collaborative on Childhood Obesity Research, which coordinates childhood obesity research across the National Institutes of Health (NIH), Centers for Disease Control and Prevention (CDC), the Department of Agriculture, and the Robert Wood Johnson Foundation (RWJF). This work was supported in part by grants from RWJF (grant numbers 260639, 61468 and 66284), CDC (U48/DP00064-00S1 and 1U48DP001946), including the Nutrition and Obesity Policy, Research and Evaluation Network, and the Office of Behavioral and Social Sciences Research of NIH. The original data collection was supported by the Vanderbilt Institute for Obesity and Metabolism (award number UL1TRR24975, which is now UL1TR000445 at the National Center for Advancing Translational Sciences), and the American Heart Association Clinical Research Grant Program (09CRP2230246).
The authors would like to thank Karen Potvin Klein, MA, ELS (Translational Science Institute, Wake Forest University Health Sciences) for her editorial comments.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. The authors declare that they have no competing interests.
Human Participant Protection
The Wake Forest University Health Sciences institutional review board approved this study (IRB00022081).
References
- 1.Gortmaker SL, Swinburn BA, Levy D et al. Changing the future of obesity: science, policy, and action. Lancet. 2011;378(9793):838–847. doi: 10.1016/S0140-6736(11)60815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hammond RA. Complex systems modeling for obesity research. Prev Chronic Dis. 2009;6(3):A97. [PMC free article] [PubMed] [Google Scholar]
- 3.Levy DT, Mabry PL, Wang YC et al. Simulation models of obesity: a review of the literature and implications for research and policy. Obes Rev. 2011;12(5):378–394. doi: 10.1111/j.1467-789X.2010.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nader PR, Huang TT, Gahagan S, Kumanyika S, Hammond R, Christoffel KK. Next steps in obesity prevention: altering early life systems to support healthy parents, infants, and toddlers. Child Obes. 2012;8(3):195–204. doi: 10.1089/chi.2012.0004. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academics Press; 2012. [Google Scholar]
- 6.Valente TW. Network interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- 7.Bahr DB, Browning RC, Wyatt HR, Hill JO. Exploiting social networks to mitigate the obesity epidemic. Obesity (Silver Spring) 2009;17(4):723–728. doi: 10.1038/oby.2008.615. [DOI] [PubMed] [Google Scholar]
- 8.Barabasi AL, Albert R. Emergence of scaling in random networks. Science. 1999;286(5439):509–512. doi: 10.1126/science.286.5439.509. [DOI] [PubMed] [Google Scholar]
- 9.El-Sayed AM, Seemann L, Scarborough P, Galea S. Are network-based interventions a useful antiobesity strategy? An application of simulation models for causal inference in epidemiology. Am J Epidemiol. 2013;178(2):287–295. doi: 10.1093/aje/kws455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de la Haye K. Re: “Are network-based interventions a useful antiobesity strategy? Am J Epidemiol. 2013;178(5):837–838. doi: 10.1093/aje/kwt183. [DOI] [PubMed] [Google Scholar]
- 11.Leahey TM, Larose JG, Fava JL, Wing RR. Social influences are associated with BMI and weight loss intentions in young adults. Obesity (Silver Spring) 2011;19(6):1157–1162. doi: 10.1038/oby.2010.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harmon BE, Nigg CR, Long C et al. What matters when children play: influence of social cognitive theory and perceived environment on levels of physical activity among elementary-aged youth. Psychol Sport Exerc. 2014;15(3):272–279. doi: 10.1016/j.psychsport.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sawka KJ, McCormack GR, Nettel-Aguirre A, Hawe P, Doyle-Baker PK. Friendship networks and physical activity and sedentary behavior among youth: a systematized review. Int J Behav Nutr Phys Act. 2013;10:130. doi: 10.1186/1479-5868-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Macdonald-Wallis K, Jago R, Sterne JA. Social network analysis of childhood and youth physical activity: a systematic review. Am J Prev Med. 2012;43(6):636–642. doi: 10.1016/j.amepre.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 15.de la Haye K, Robins G, Mohr P, Wilson C. How physical activity shapes, and is shaped by, adolescent friendships. Soc Sci Med. 2011;73(5):719–728. doi: 10.1016/j.socscimed.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 16.de la Haye K, Robins G, Mohr P, Wilson C. Obesity-related behaviors in adolescent friendship networks. Soc Networks. 2010;32(3):161–167. [Google Scholar]
- 17.Maturo CC, Cunningham SA. Influence of friends on children’s physical activity: a review. Am J Public Health. 2013;103(7):e23–e38. doi: 10.2105/AJPH.2013.301366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shoham DA, Tong L, Lamberson PJ et al. An actor-based model of social network influence on adolescent body size, screen time, and playing sports. PLoS ONE. 2012;7(6):e39795. doi: 10.1371/journal.pone.0039795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de la Haye K, Robins G, Mohr P, Wilson C. Homophily and contagion as explanations for weight similarities among adolescent friends. J Adolesc Health. 2011;49(4):421–427. doi: 10.1016/j.jadohealth.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Valente TW, Fujimoto K, Chou CP, Spruijt-Metz D. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. J Adolesc Health. 2009;45(2):202–204. doi: 10.1016/j.jadohealth.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 22.Gesell SB, Tesdahl E, Ruchman E. The distribution of physical activity in an after-school friendship network. Pediatrics. 2012;129(6):1064–1071. doi: 10.1542/peds.2011-2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54) BMJ. 2012;345:e5888. doi: 10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- 24.Rothenberg RB, Woodhouse DE, Potterat JJ, Muth SQ, Darrow WW, Klovdahl AS. Social networks in disease transmission: The Colorado Springs Study. NIDA Res Monogr. 1995;151:3–19. [PubMed] [Google Scholar]
- 25.Valente TW. Social Networks and Health: Models, Methods, and Applications. New York, NY: Oxford University Press; 2010. [Google Scholar]
- 26.Valente TW, Ritt-Olson A, Stacy A, Unger JB, Okamoto J, Sussman S. Peer acceleration: effects of a social network tailored substance abuse prevention program among high-risk adolescents. Addiction. 2007;102(11):1804–1815. doi: 10.1111/j.1360-0443.2007.01992.x. [DOI] [PubMed] [Google Scholar]
- 27.Kelly JA, St Lawrence JS, Diaz YE et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81(2):168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flodgren G, Parmelli E, Doumit G et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2011;10(8):CD000125. doi: 10.1002/14651858.CD000125.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. BMI calculator for child and teens. Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_BMI/about_childrens_BMI.html. Accessed October 18, 2014.
- 30.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring) 2006;14(11):2000–2006. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 31.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res. 2002;10(3):150–157. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 32.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc. 2009;41(7):1384–1391. doi: 10.1249/MSS.0b013e318199885c. [DOI] [PubMed] [Google Scholar]
- 33.Ripley R, Snijders T. Manual for SIENA version 4.0. 2011. Available at: http://www.stats.ox.ac.uk/∼snijders/siena. Accessed October 18, 2014.
- 34.Snijders TAB, van de Bunt GG, Steglich CEG. Introduction to stochastic actor-based models for network dynamics. Soc Networks. 2010;32(1):44–60. [Google Scholar]
- 35.Snijders T, Steglich C, Schweinberger M. Modeling the co-evolution of networks and behavior. In: van Montfort K, Oud H, Satorra A, editors. Longitudinal Models in the Behavioral and Related Sciences. Mahwah, NJ: Lawrence Erlbaum; 2007. pp. 41–71. [Google Scholar]
- 36.Steglich S, Snijders TAB, Pearson M. Dynamic networks and behavior: separating selection from influence. Sociol Methodol. 2010;40(1):329–393. [Google Scholar]
- 37.Wilensky U. NetLogo. Center for Connected Learning and Computer-Based Modeling Web site. Available at: http://ccl.northwestern.edu/netlogo. Accessed October 18, 2014.
- 38.Zhang J, Tong L, Lamberson PJ, Durazo-Arvizu RA, Luke A, Shoham DA.Leveraging social influence to address overweight and obesity using agent-based models: the role of adolescent social networks Soc Sci Med 2015125:203–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hammond R. The Building Blocks of an ABM. Podium presentation at the Institute on Systems Science and Health (ISSH). Washington University, St. Louis, MO. June 2012. Available at: http://obssr.od.nih.gov/issh/2012/index.html. Accessed October 20, 2014.
- 40.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–432. doi: 10.1093/ije/30.3.427. discussion 433–434. [DOI] [PubMed] [Google Scholar]
- 41.Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003;157(8):746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 42.Rogers EM. Diffusions of Innovations. New York, NY: Free Press; 1995. [Google Scholar]
- 43.Beets MW, Beighle A, Erwin HE, Huberty JL. After-school program impact on physical activity and fitness: a meta-analysis. Am J Prev Med. 2009;36(6):527–537. doi: 10.1016/j.amepre.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 44.Valente TW, Hoffman BR, Ritt-Olson A, Lichtman K, Johnson CA. Effects of a social-network method for group assignment strategies on peer-led tobacco prevention programs in schools. Am J Public Health. 2003;93(11):1837–1843. doi: 10.2105/ajph.93.11.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shalizi CR, Thomas AC. Homophily and contagion are generically confounded in observational social network studies. Sociol Methods Res. 2011;40(2):211–239. doi: 10.1177/0049124111404820. [DOI] [PMC free article] [PubMed] [Google Scholar]