Abstract
Introduction:
Considering the chronic nature of diabetes and its significant effect on quality of life of patients, the present study was conducted to evaluate predictors of quality of life in these patients in order to facilitate planning health promotion intervention programs.
Materials and Methods:
The present study was designed as a cross-sectional study on 140 type 2 diabetic patients of Om-ol-Banin Diabetes Center of Isfahan. Data collection tool was a multidimensional questionnaire including demographic and disease related data (12 items), the standard scale for diabetes distress (17 items), the standard scale for self-efficacy in diabetic patients (8 items), and standard scale for specific quality of life of diabetic patients (15 items). Collected data were evaluated by SPSS version 11.5 using the Chi-square test, Independent T-test, ANOVA, Pearson correlation and multivariate regression analysis.
Results:
Results showed that the quality of life of diabetic patients had a statistically significant correlation with diabetes distress variable (P < 0.001) and self-efficacy variable (P < 0.001). In this study R2 (predictive power) was 0.66. Multivariate regression model indicated diabetes distress (β = -0.277, P = 0.01) and self-efficacy (β = -0.161, P < 0.001) as variables influencing adjusted self-management for other variables.
Conclusion:
The result of the present study urges that in planning health promotion interventions in the field of diabetes, more attention be paid to self-efficacy and diabetes distress variables in order to improve the efficiency and effectiveness of the interventions carried out.
Keywords: Diabetes distress, predictive factors, quality of life, self-efficacy, type 2 diabetes
INTRODUCTION
Diabetes pandemic is accompanied with rapid cultural change, aging population, increasing urbanization, changes in eating habits, reduced physical activity, wrong lifestyle, and inappropriate behavior patterns.[1] The World Health Organization discuses that there is an apparent diabetes epidemic, which is strongly associated with the lifestyle changes and economic status of individuals.[2] Type 2 diabetes includes 90-95% of all diabetes diagnosed cases.[3] Today, more than three million people in Iran have diabetes, which according to World Health Organization estimation will reach to 7 million on 2030, if effective measures are not taken. Diabetes prevalence rate in adults is estimated between 2-10%.[4] Health Deputy of Ministry of Health and Medical Education reported this rate as 2.3%,[5] and Isfahan Endocrine Research Center have estimated this rate to be 2-3% in total population and 7.3% in people over 30 years old.[6] Chronic nature of diabetes affects the physical, mental, personal and social performance of the patient, so it is essential to check various aspects of health and quality of life in these patients. Diabetes is a serious public health problem that threatens the quality of life of patients and can lead to acute and chronic complications and is considered an important cause of morbidity and mortality in many countries.[7] Type 2 diabetes can be studied as a multifactorial disease that greatly affects the quality of life of patients.[8]
Chronic complications and problems of diabetes have a great impact on quality of life in diabetic patients and this can affect the economic conditions of patients, families and society.[9] Improvement of quality of life in patients with type 2 diabetes is greatly emphasized in clinical diabetes control manual; and one of the most basic goals of controlling diabetes is improving the quality of life.[10] Therefore quality of life is considered as an important outcome of health and an ultimate goal in all health-related interventions.[11] This fact indicates that the quality of life is considered as a long-term consequence of diabetes in monitoring and evaluation of diabetes load in societies, so that various studies reported a significant correlation between quality of life and age, sex, diabetes complications, diseases associated with diabetes, and disease severity.[12,13,14,15]
Diabetic patients compared to individuals without chronic disease, have the lowest quality of life but this outcome has a better condition compared to people with other chronic diseases with sever and serious complications.[16] Several studies have shown that the type of diabetes and its treatment, is not associated with quality of life in patients, rather they can experience a better quality of life with proper control and management of blood glucose.[17,18] Also, some studies reported the effect of demographic variables and psychological factors on quality of life in patients.[19] Quality of life of diabetic patients is studied in several studies;[17] however, the present study examined the predictive factors of quality of life in diabetic patients, which is considered a new approach in diabetes research. Identifying modifiable and associated predictive factors of quality of life, one can manage diabetes better and make a significantly more effective impact on improvement of long-term outcomes such as quality of life with applying cost-effective interventions. Considering the importance of quality of life as a long-term outcome of type 2 diabetes, this study examines some predicting factors of quality of life in type 2 diabetic patients. Results from this study can identify variables affecting the quality of life in type 2 diabetic patients in order to be considered more in interventions planned in the area of diabetes management.
MATERIALS AND METHODS
The present descriptive-analytic study was conducted during a simple sampling in the first 4 months of 1,390 on 140 outpatients with type 2 diabetes in Om-ol-Banin Diabetes Center of Isfahan that provides Prevention and Treatment Services to diabetes patients. Sampling was performed as follows: Two days a week (Monday and Tuesday), in a specified time, one of the researchers referred to the center and interviewed eligible patients. Observing ethical considerations, participation of patients in the interviews was free and optional and the research goals were completely explained to them before the interview. Each patient was interviewed only once. Inclusion criteria for this study were: (1) having type 2 diabetes, approved by the center's specialist, (2) having diabetes for at least one year, (3) not having a mental illness approved by the center's specialist, and (4) age over 30 years. People, who were not eligible for these criteria were excluded.
Data collection tool was a multidimensional questionnaire including four sections. The first section included demographic and disease-related data of subjects such as age, sex, marital status, family income, years spent with diabetes, patient's health status perspective, family history of diabetes (diabetes in the patient's family), and diseases associated with diabetes and diabetes complications (12 items). The second part was the scale of psychological distress in diabetic patients (17 items), which measured by a six options Likert scale. In this scale NEVER was scored with 1 point and ALWAYS had 6 points. The total score varies from 17 to 102.[20] The third section was the scale of self-efficacy in diabetic patients including 13 items measured by a 1-10 scale. Scoring range was from 1 “NOT SURE AT ALL” to 10 “ABSOLUTELY SURE”. Higher scores indicated higher self-efficacy.[21] The forth Section, was Audit of Diabetes Dependent Quality of Life (ADDQoL) including 15 items measured by a seven options scale. Last 2 items of this scale measures overall quality of life of diabetic patients and the remaining 13 items is related to specific quality of life of diabetic patients. This Audit of Diabetes Dependent Quality of Life reviews patients’ understanding of the impact of diabetes on quality of life. The original version of this tool has a good reliability (α = 0.85). The scoring is as follows: This tool measures the impact of diabetes on the lives of people with scoring each question in a range of -3 to +3 (extremely worse to extremely better), and in the next section it identifies the importance degree of each item with a scale of zero to 3 (not important at all to very important). The total scores of this tool measures the quality of life of diabetic patients according to the degree of effect, importance, and weight.[22] This tool was standard and was used after translation and retranslation by a fluent bilingual (Persian-English) team who were diabetes expert, and determination of its validity and reliability. Content validity was used to determine the scientific validity of the data collection tool. The translated items of the original questionnaire were given to 10 faculty members of Isfahan and Tehran University of Medical Sciences, who were experts in the field of diabetes and mental-social health issues. After applying recommended reforms, the questionnaire underwent a final evaluation and approval. To determine the reliability of the tool, the present multidimensional questionnaire was given to 30 patients of the center who were excluded later from the main study. Using the internal consistency method, alpha was measured for different parts of the questionnaire. The resulting alpha values for scales were 0.75 to 0.98 that is acceptable. Calculated alpha values for each of the study tools were: Diabetes distress (0.75), self-efficacy (0.98), quality of life associated with diabetes (0.91). It took 10-15 min to complete this tool. Finally, the data were collected and analyzed by SPSS software version 11.5 using the Chi-square, Independent T-test, and ANOVA tests for qualitative variables assessment, Pearson correlation for quantitative variables assessment, and multivariate regression to determine factors affecting quality of life. The significance level was 0.05 in this study.
RESULTS
The response rate was 100% in this study. The average age and years with diabetes of subjects were 53 ± 7.82 and 7.1 ± 5.63 years, respectively. The subjects were 54.3% female, 97.1% married, 57.11% with underlying diseases associated with diabetes, 73.6% with diabetes complications, and 71.4% had a history of diabetes. 53.6% of patients had an educational level under diploma, and 65.7% of patients had oral treatment. 51.4% of patients described their health status as moderate. The Clinical and Anthropometric indicators of subjects were HbA1c (7.81 ± 0.78), BMI (29.37 ± 4.20), and abdominal girth (97.55 ± 12.52). Diabetes distress and self-efficacy mean scores of subjects were (29.69 ± 0.83) and (32.171 ± 8.26), respectively. Results showed no statistically significant correlation of the demographic and associated with diabetes characteristics (P > 0.05).
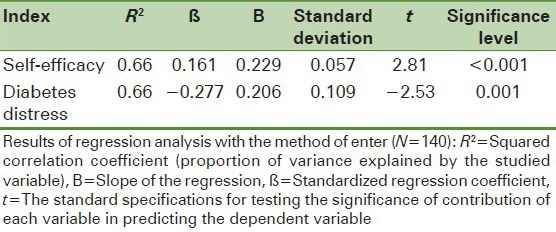
Pearson correlation coefficient test showed a linear and reverse relationship between diabetes distress variable and quality of life in diabetic patients (r= -0.341, P < 0.001), and a direct linear relationship between self-efficacy variable and quality of life in diabetic patients (r = 0.63, P < 0.001). Results showed that the quality of life of diabetic patients had a statistically significant correlation with diabetes distress variable (P < 0.001) and self-efficacy variable (P < 0.001). In this study, R2 (predictive power) was 0.66. Multivariate regression model indicated diabetes distress (β = -0.277, P-0.01) and self-efficacy (β = -0.161, P-0.001) as variables influencing adjusted self-management for other variables [Table 1]. Other variables used in this study, showed no significant relationship with quality of life in the first stage of tests to be used in the regression model.
Table 1.
Predictive factors of quality of life of subjects
CONCLUSION
The present study examined some factors associated with the quality of life in type 2 diabetic patients. Given various variables that affect the quality of life of diabetic patients, the present study tried to identify and analyze the relevant and affecting predictive variables of quality of life in diabetic patients and suggest the best regression model for them. Identification and focus on modifiable factors in the quality of life of patients with diabetes, is an important step in choosing the appropriate pattern and intervention methods to obtain the best results.[23]
This study found no significant correlation between demographic variables related to diabetic patients’ health and quality of life in order to enter regression model in the second stage, and only the two variables of diabetes distress and self-efficacy were significantly correlated with quality of life in the early stages, therefore they entered regression model in second stage of the study to suggest a model.
In the present study, regression model identified diabetes distress and self-efficacy as predictive factors of quality of life, which will be addressed in this section. In addition to physical effects of diabetes, people with diabetes also suffer from psychological distress. Factors such as diagnosis, symptoms and strict treatment and surveillance programs can be considered a resource for diabetes distress.[24] Emotional distress associated with the disease can be diverse from tragic problems to ongoing self-care needs caused by diabetes, such as continuous glucose monitoring, medication, insulin injections, control of food intake, and regular physical activities.[25] Researchers indicate that distress can dramatically affect the health consequences associated with diabetes including quality of life in diabetic patients.[26] An extensive study was conducted in 13 countries about diabetes distress, the results showed that psychological problems such as diabetes distress is very common in diabetic patients and dramatically affects the life with diabetes.[27]
Our results showed that distress has predictive effects on quality of life of diabetic patients which is consistent with findings of Wexler et al. (2006). The present study showed that depression has predictive effects on quality of life of patients,[28] while it has also been confirmed in other studies that depression is a factor reducing patients’ quality of life so that in this group of patients, quality of life becomes even less than other chronic diseases.[29,30]. Sundaram et al. findings somehow confirm our results, so that depression symptoms in patients who have had lower quality of life scores were more severe. This study justifies its findings in this way that the factors affecting adoption of self-management practices of diabetes also affect the quality of life in diabetic patients in some way and are considered predictive factors in the process, which he recommends to be measured along with the HbA1c measurement.[31] Liu et al. (2010) indicated that emotional distress is the most important factor in quality of life. This study suggests that health experts evaluate their patients’ emotional distress, consider a program for patients’ emotional support, and use empowerment strategies to improve the quality of life of patients.[32]
Another variable identified as predictive factor of quality of life in this study was self-efficacy. The results of this study about self-efficacy structure showed that self-efficacy is considered as a predictive factor of the quality of life. The importance and role of this structure is well proven to change the behavior and improve self-management process in chronic diseases. On the other hand it has been proved that adopting self-management behaviors affects the quality of life in diabetic patients. Studies on diabetes reported positive effects of perceived self-efficacy on self-management behaviors adoption,[33] diabetes control,[34] and thus long-term consequences of diabetes control which leads to improvement of quality of life of patients.
Cherrington et al. (2010) showed that self-efficacy reduces symptoms of depression and helps to improve patients’ quality of life[35] so that Mishalia et al. (2010) indicated the self-efficacy have a role in following treatment in diabetes control and it is essential that self-efficacy assessment be considered in the first phase of interventions design, as it would in turn improve the quality of life of patients.[36] The noteworthy point in this study is that focus on modifiable variables is very influential for effective interventions and determining strategies in improving the health of diabetics. Available studies suggest that attention should be paid to affecting variables for designation, implementation and evaluation of interventions; and psychological distress and self-efficacy assessment be performed on patients for planning interventions in chronic diseases such as diabetes, because with attention to these two important and influential variables, more effective results would be achieved in improving long term outcomes such as quality of life in diabetic patients.
This study had limitations, among which the following can be mentioned. This study was cross-sectional and the samples were almost similar and homogeneous, with a limited sample size and simple sampling method and self report instruments. Given the mentioned limitations of this study, the results provide evidences for importance and predictive effect of variables such as self-efficacy and diabetes distress on quality of life in diabetic patients.
ACKNOWLEDGEMENTS
The present study is a report of part of doctoral dissertation research with project number of 389410. Hereby the authors would like to thank the research deputy of Isfahan University of Medical Sciences for financial support, Om-ol-Banin Diabetes Center of Isfahan for permission to perform this study and dear patients for their participation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Butt J. Media backgrounder diabetes in the developing world. World Diabetes Foundation. 2010. [Last accessed on 2011 May 2]. Available from: http:// www.worlddiabetesfoundation.org .
- 2.Abolhassani F, Mohajeri Tehrani MR, Tabatabaei O, Larijani B. Burden of diabetes and its complications in Iran in year 2000. Journal of Diabetes and Metabolic Disorders. 2005;5:35–48. [Google Scholar]
- 3.Arian V. Tehran: Marzedanesh Publications; 2007. Approach on treatment and nutrition in diabetes. [Google Scholar]
- 4.Esteghamati A, Gouya MM, Abbasi M, Delavary A, Alikhani S, Alaedini F, et al. Prevalence of diabetes mellitus and impaired fasting glucose in the adult population of Iran: The national survey of risk factors for non-communicable disease of Iran. Diabetes Care. 2008;31:96–8. doi: 10.2337/dc07-0959. [DOI] [PubMed] [Google Scholar]
- 5.Tehran: Tabalwor publishing group; 2003. Deputy of Health Deputy for research and technology. National health situation states. [Google Scholar]
- 6.Mahdi Hazaveh A, Delavari A. Tehran: Deputy of Health; 2004. Diabetes of prevention and control. [Google Scholar]
- 7.Rakhshandehro S, Heidarnia AR, Rajab A. Determination of health education on quality of life in type 2 diabetic patients. Journal of Shahed University. 2006;63:15–20. [Google Scholar]
- 8.Bharati DR, Pal R, Rekha R, Yamuna TV. Evaluation of the burden of type 2 diabetes mellitus in population of Puducherry South India. Diabetes Metab Syndr. 2011;5:12–6. doi: 10.1016/j.dsx.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Massi-Benedetti M. The cost of diabetes type II in Europe. The CODE-2 study. Diabetologia. 2002;45:S1–4. doi: 10.1007/s00125-002-0860-3. [DOI] [PubMed] [Google Scholar]
- 10.Gries FA, Alberti KG. Management of non-insulin dependent diabetes mellitus in Europe: A consensus statement. IDF Bull. 1987;32:169–74. [Google Scholar]
- 11.Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. 16th ed. Columbus (OH): McGraw- Hill Publisher; 2005. Harrison's principles of internal medicine. [Google Scholar]
- 12.Saito I, Inami F, Ikebe T, Moriwaki C, Tsubakimoto A, Yonemasu K, et al. Impact of diabetes on health-related quality of life in a population study in Japan. Diabetes Res Clin Pract. 2006;73:51–7. doi: 10.1016/j.diabres.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L. Quality of life and associated characteristics in large national sample of adults with diabetes. Diabetes Care. 1997;20:562–7. doi: 10.2337/diacare.20.4.562. [DOI] [PubMed] [Google Scholar]
- 14.Wee HL, Cheung YB, Li SC, Fong KY, Thumboo J. The impact of diabetes mellitus and other chronic medical conditions on health-related quality of life: Is the whole greater than the sum of its parts? Health Qual Life Outcomes. 2005;3:2. doi: 10.1186/1477-7525-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maddigan SL, Majumdar SR, Toth EL, Feeny DH, Johnson JA. Health-related quality of life deficits associated with varying degrees of disease severity in type 2 diabetes. Health Qual Life Outcomes. 2003;1:78. doi: 10.1186/1477-7525-1-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Minet L, Møhler S, Vach W, Wagner L, Henriksen J. Mediating the effect of self-care management intervention in type 2 diabetes: A meta-analysis of 47 randomized controlled trials. Patient Educ Couns. 2010;80:29–41. doi: 10.1016/j.pec.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 17.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 18.Cezaretto A, Siqueira-Catania A, de Barros CR, Salvador EP, Cavalierf D, Ferreira SR. Benefits on quality of life concomitant to metabolic improvement in intervention program for prevention of diabetes mellitus. Qual Life Res. 2012;21:105–13. doi: 10.1007/s11136-011-9919-2. [DOI] [PubMed] [Google Scholar]
- 19.Santhanam P, Gabbay RA. Poor quality of life scores in persons with higher A1Cs in type 2 diabetes. Diabetes Res Clin Pract. 2011;92:e53–4. doi: 10.1016/j.diabres.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 20.Polonsky WH, Fisher L, Earles P, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care. 2005;28:626–31. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 21.Lorig K. Stanford self-efficacy for diabetes. Stanford Patient Education Research Center. [Last accessed on 2010 July 11]. Avilable from: http://patienteducation.stanford.edu/research/diabscales.htm .
- 22.Bradley C, Todd C, Gorton T, Symonds E, Martin A, Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: The ADDQoL. Qual Life Res. 1999;8:79–91. doi: 10.1023/a:1026485130100. [DOI] [PubMed] [Google Scholar]
- 23.Funnell MM, Brown T, Childs B, Hass L, Hoset G, Jensen B. National standards for diabetes self-management education. Diabetes Care. 2009;32(Suppl 1):S89–96. doi: 10.2337/dc10-S089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Macrodimitris SD, Endler NS. Coping, control and adjustment in type 2 diabetes. Health Psychol. 2001;20:208–16. [PubMed] [Google Scholar]
- 25.Spenser MS, Kieffer EC, Sinco BR, Palmisano G, Guzman JR, James SA, et al. Diabetes -specific emotional distress among African American and hispanics with type 2 diabetes. J Health Care Poor Underserved. 2006;17:88–105. doi: 10.1353/hpu.2006.0095. [DOI] [PubMed] [Google Scholar]
- 26.Whittermore R, Melkus G, Grey M. Metabolic control, self-management and psychosocial adjustment in women with type 2 diabetes. J Clin Nurs. 2005;14:195–203. doi: 10.1111/j.1365-2702.2004.00937.x. [DOI] [PubMed] [Google Scholar]
- 27.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: Result of the cross-national diabetes attitude, wishes and needs (DAWN) study. Diabet Med. 2005;22:1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 28.Wexler DJ, Grant RW, Wittenberg E, Bosch JL, Cagliero E, Delahanty L, et al. Correlates of health-related quality of life in type 2 diabetes. Diabetologia. 2006;49:1489–97. doi: 10.1007/s00125-006-0249-9. [DOI] [PubMed] [Google Scholar]
- 29.Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: A population study. Diabetes Care. 2004;27:1066–70. doi: 10.2337/diacare.27.5.1066. [DOI] [PubMed] [Google Scholar]
- 30.Brown GC, Brown MM, Sharma S, Brown H, Gozum M, Denton P. Quality of life associated with diabetes mellitus in an adult population. J Diabetes Complications. 2000;14:18–24. doi: 10.1016/s1056-8727(00)00061-1. [DOI] [PubMed] [Google Scholar]
- 31.Sundaram M, Kavookjian J, Patrick JH, Miller LA, Madhavan S, Scott V. Quality of life, health status and clinical outcomes in type 2 diabetes patients. Qual Life Res. 2007;16:165–77. doi: 10.1007/s11136-006-9105-0. [DOI] [PubMed] [Google Scholar]
- 32.Liu MY, Tai YK, Hung WW, Hsieh MC, Wang RH. Relationships between emotional distress, empowerment perception and self-care behavior and quality of life in patients with type 2 diabetes. Hu Li Za Zhi. 2010;57:49–60. [PubMed] [Google Scholar]
- 33.Skelly AH, Marshall JR, Haughey BP, Davis PJ, Dunford RG. Self-efficacy and confidence in outcomes as determinants of self-care practices in inner-city, African-American women with non-insulin-dependent diabetes. Diabetes Educ. 1995;21:38–46. doi: 10.1177/014572179502100107. [DOI] [PubMed] [Google Scholar]
- 34.Ludlow AP, Gein L. Relationships among self-care, self efficacy and Hb1c levels in individuals with non-insulin dependent diabetes mellitus. Can J Diabetes Care. 1995;19:10–5. [Google Scholar]
- 35.Cherrington A, Wallston KA, Rothman RL. Exploring the relationship between diabetes self-efficacy, depressive symptoms, and glycemic control among men and women with type 2 diabetes. J Behav Med. 2010;33:81–9. doi: 10.1007/s10865-009-9233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mishalia M, Omera H, Heymann AD. The importance of measuring self-efficacy in patients with diabetes. Fam Pract. 2011;28:82–7. doi: 10.1093/fampra/cmq086. [DOI] [PubMed] [Google Scholar]


