Abstract
Introduction:
Diabetes is increasingly becoming prevalent worldwide. Pregnancy with diabetes is prone to maternal and fetal complications. Preconception care (PCC) is an important factor in alleviating gestational complications in those women who suffer from diabetes. This study seeks to gain insight into experiences of diabetic women and providers about PCC.
Subjects and Methods:
The present research was a qualitative research conducted on eight women with diabetes during the reproductive age and 15 health care providers of the public and private medical centers, which provide health care for women with diabetes in Isfahan (Iran), with a qualitative approach. Based on the aims of research, purposive sampling was done through semi-structuralized individual interview. Data were analyzed using conventional qualitative content analysis method.
Results:
Data analysis revealed three major categories: (1) Health centers weakness in providing PCC for diabetic women, (2) lack of a comprehensive PCC plan for diabetic women and (3) diabetic women's negligence about having planned pregnancy.
Conclusion:
In order to improve diabetic women's health, precise training of students, health care providers and patients themselves with respect to PCCs should be taken into account. Designing diabetic PCC system is an essential factor to succeed in this trend.
Keywords: Diabetic mellitus, health personnel, preconception care
INTRODUCTION
Prevalence of diabetes is increasing worldwide. 122 million women are suffering from this disease in the world, which is expected to reach 192 million by 2025.[1] Prevalence of diabetes among pregnant women was 1.2% in Canada in 2001.[2] In the United State, 10% of the pregnancies are accompanied with diabetes.[3]
In addition, according to one reports in 2005 distribution of positive history for diabetes (self reported) previously diagnosed by a doctor or other health professionals in those Iranian women who were between 15 and 24 years was 0.4%, in those who were between 25 and 34 years of old was 1.3% and in women who were between 35 and 44 years of old was 3.8%.[4]
The growth in the rate of pregnancies with diabetes has been resulted from the increase in the prevalence of diabetes in the world.[5]
Pregestational diabetes is accompanied with pregnancy complications including congenital malformations, macrosomia, stillbirth, urinary tract infection, hypertension, cesarean section, abortion, neonatal death, preterm labor, shoulder dystocia, Erb's palsy and low Apgar scores.[6] Duration and intensity of diabetes, chronic complications and blood sugar level would be affecting in the occurrence of pregnancy complications.[6,7,8,9,10,11] Now-a-days, the number of deaths pertaining to diabetes during pregnancy is 2.5–9 times as much as the number of deaths in the normal population.[12]
The relation between blood glucose control and pregnancy outcome is indicative of preconception cares (PCCs) significance.[13] Those women with diabetes who undergo PCC will experience less maternal and fetal complications, less need to insulin, better blood sugar control in 3 months prior to conception and during the first trimester, and increased consumption of folic acid compared with those who had a lack of any counseling.[14,15,16,17] PCC is one of the main solutions to improve the general health of the mother and fetus. The initial prenatal care (PNC) is normally provided at the end of the first trimester when any adverse effect on the fetus is irreversible. Risk factors can be identified in PCC before conception, and ultimately, pregnancy can be improved.[18]
Preconception care program goals in diabetic women include: Normal HbA1C, better blood sugar control, hyperglycemia reduction before and during initial pregnancy stages, proper nutrition, doing exercises, consuming folic acid supplement, having consultations with experts on congenital abnormalities and practicing contraception to control blood sugar properly, investigating diabetes complications, checking administration of all medicines, assessing immunity against rubella, counseling about pregnancy risks particularly congenital malformation, referring to relevant centers if necessary and undergoing other trainings.[15,19,20]
According to the results of the investigations, diabetic PCC has the following benefits: Better blood sugar control and higher consumption of folic acid 3 months before conception, more favorable metabolic condition during pregnancy, less need to insulin, lower risk of abortion and stillbirth and finally, reduction of poor pregnancy outcomes.[14,17]
Other studies have shown that PCC leads to frequent referrals for PNC and less HbA1C.[21]
Since PCC reduces maternal and fetal complications it should be considered as an essential item. Study and research about awareness of diabetic women of reproductive age in relation to PCC, reasons of lack of this practice in these women, design programs to prevent maternal and fetal complications of diabetes in pregnancy are necessary. PCC delivers strong strategy that should be designed to improve the health of women with diabetes before pregnancy.[22]
Evaluation of experiences is one of ways for design strategies. The searches conducted no studies related to health care and women's experiences in the field of PCC in diabetes in Iran. Because there is not any statistically data about the quality of diabetic PCC and its barriers in Iran and regarding the importance of evaluation of experiences of health care providers and also women with diabetes. This study was designed to investigate the experiences of these two groups about diabetic PCC. Health care providers in medical centers are the most important people who incessantly deal with pregnant women. Thus, their abilities in providing PCC and their views about this subject can be very helpful in improving health care system. On the other hand, diabetic women's experiences about PCC can provide us with the appropriate solutions. The objective of this study was applied to extract the strengths and weaknesses of this program and provide appropriate strategies to strengthen it with design systematic strategies plan to improve maternal health.
SUBJECTS AND METHODS
This research examines the experiences of health care providers and women with diabetes about PCC using a qualitative approach. The participants were eight diabetic pregnant women and 15 health care providers who provide women with diabetes with health care services in private and public centers in Isfahan, Iran.
The participants comprised health care providers working in above centers and women with diabetes referring to these centers. Purposive sampling was conducted. The viewpoints of various individuals, related to this issue were inquired increase the rigor of the study.
There are three general diabetes centers in which midwives, family health staffs, diabetes trained general physicians and endocrinologists work in Esfahan. In addition to this fact, numerous endocrinologists and midwives in private offices work on this issue. We added two obstetricians to them to obtain more data. The participants were selected from governmental and private centers and were from all aforementioned professions.
They were invited to take part in the study after being provided with a brief explanation on the research plan. Via a written letter of consent, the participants consented to take part in the study. Interview sessions were held according to the subjects’ will, mainly in the medical centers. Data were collected by using digital recording of individual semi-structured interviews (30–60 min). Notes were taken from the discussions, held with the participants and their reactions. Data collection and sampling continued until no new data were obtained, and the number of participants was determined accordingly. The data were analyzed by using conventional content analysis method, concurrent with the data collection. After recording the interviews, the researchers listened to them immediately after each session. In order to have a general outlook, the interviews were transcribed verbatim entirely. Through analysis, units and main ideas of the text were perused line by line; and important clauses were determined and underlined. The texts’ main contents were coded (encrypted). Similar codes were then merged and the initial categorization was performed. The declining trend in data reduction continued in all analysis units up to the emergence of categories. In this way, the general, conceptual, and abstract data were placed in the main category.
Data trustworthiness
Credibility was enhanced through member checking, validation of emerging codes and categories in subsequent discussions and debriefings with two supervisors. Using member checking, peer checking and maximum variation of sampling attested to the credibility. In order to establish inter transcripts reliability, three qualitative researchers carried out a second review. Approximately, 60% of the transcript, codes and categories were rechecked, and there was 90% agreement among them. The current research was approved by “Ethics Committee” of the University. The participants were also given the option to quit the study.
RESULTS
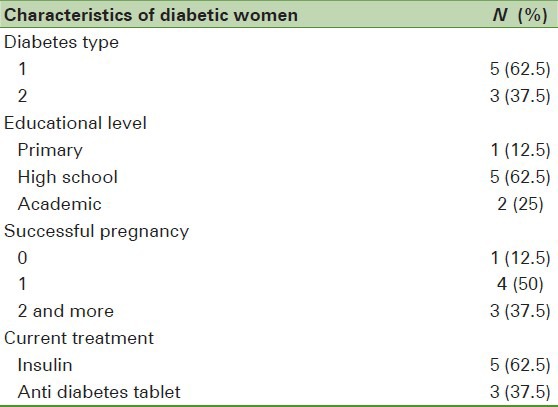
The participants were eight diabetic women, six diabetes trained general practitioners, three endocrinologists, three midwives, two obstetricians, and one family health expert. Mean age of the participants was 38 (standard deviation [SD] = 6.3) years with mean professional working experience of 6 years. Mean age of women with diabetes was 28 years (SD = 4.2). Participants’ other demographic characteristics have been presented in Table 1.
Table 1.
Characteristics of diabetic women participant in research
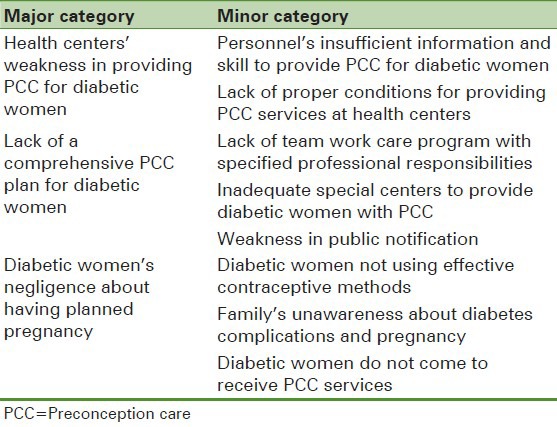
Analysis of participants’ descriptions about PCC experiences led to the emergence of three major and eight minor categories [Table 2]. Examples of the participants’ opinions are mentioned here.
Table 2.
Major and minor categories revealed from experiences of participants about diabetic women's preconception care
Health centers weakness in providing preconception care for diabetic women
Not only the personnel believed they were not qualified adequately for the provision of these services, but also they believed the health centers lack proper devices and conditions to provide PCC.
The extracted sub-categories are as below:
Personnel's insufficient information and skill to provide preconception care for diabetic women
Most of the participants expressed that they did not have enough information in this regard. Due to not receiving relevant training during education and job periods, health care providers do not know much about these services and are not able to provide them properly. An endocrinologist says: “Diabetes physicians realize the significance of the issue, but these physicians are not available. Patients mostly come to the medical/health centers for conception matters, but the patients do not have enough information there”. A midwife says: “Not much attention was paid to this issue during the training courses, and now that we have only received subtle training; our information is not sufficient”.
Lack of proper conditions at health care centers to provide preconception care services
The participants noted that there was no proper physical space and time for providing PCC to diabetic women. Women with diabetes are mainly treated by diabetes physicians; who do not have enough time and motivation to provide conception services. A midwife says: “Preconception consultation requires a great deal of time as well as skill. Responsible personnel for this practice do not have the needed motivation to spend their time on this issue.” According to the participants’ opinions, the personnel who are responsible for diabetic PCC have more problems in this area.
Diabetic lady states: “I do not know to whom I shall talk about pregnancy and contraception. My own physician does not even spend 1 min on the issue. Health centers do not care also”.
Lack of a comprehensive preconception care plan for diabetic women
Another main category explains the PCC planning in the health care system. Participants expected the health system to offer screening, PCC and proper training to women with diabetes and their families. There should be special centers with skilled staffs who have specified professional responsibilities to provide team game PCC services so that women with diabetes would be able to have a healthy gestational program.
The extracted sub-categories are as below:
Lack of team work care program with specified professional tasks
Most of the participants claimed that there was no teamwork planning for diabetic PCC with specified positioning of the individuals. People occasionally handle such activities individually. A family health assistant states “All members of the health team shift the blame onto each other and think that they have done their duties correctly.” Another says: “There shall be team work in diabetic PCC; none of the staff (that is family health officials), midwives, general practitioners, endocrinologists, etc., care about this fact. The duties should be specified”.
Inadequate special centers for providing preconception care to diabetic women
Some participants believed that perfect PCC requires special centers. For PCC to be properly performed there should be enough physical facilities, time and professional cases for screening and referral of patients. Another participant who was diabetes trained general physician says: “Examination of a diabetic patient needs 30 min; this is while we have only 30 s per each one. I do not know how many of the pregnancies of women with diabetes of reproductive age were intentional and how many were unintentional”. The whole system should be changed.” Another diabetes trained general physician states: “We need specialized centers and facilities. Many of our patients are not able to afford paying the costs, and do not have the patience to do the follow-ups.”
Weakness of public notification
Most of the participants believed that there was no proper notification about reproductive health in women with diabetes. There is confusion in awareness, attitude, and sensitivity in this regard in the society. An endocrinologist states: “If people are informed about the risks of diabetes and pregnancy, they will accept (not to get pregnant) because it is better for their health”.
Another participant who was diabetes trained general physician believed: “People are not notified well. Whenever we encounter women of reproductive age, we should instruct them and make them refer to the physician before conception.”
In general, according to the participants’ opinion, any country's health and medical system is responsible to provide instructional programs for diabetic PCC using the mass media, specialized services and capable planners so as to attain success in this regard. Direct supervision and complete coherency should be imposed in all stages of planning and implementation. Problems should be resolved with the cooperation of people and personnel. Another participant, a woman with diabetes says: “I do not know where to go for examinations. Nobody has ever told me to apply a contraceptive method or whether I can become pregnant or not. My physician has not asked me whether I use contraception or want a baby.”
Diabetic women's negligence about having a planned pregnancy
According to the participants’ opinions, women with diabetes are unaware of the significance and necessity of a planned pregnancy. This problem mainly originates from women's unawareness of those pregnancy complications, which result from diabetes, and in selecting contraceptive methods.
The extracted sub-categories are as below:
Diabetic women do not use effective contraceptive methods
According to the viewpoints of the participants, women with diabetes of reproductive age mostly fail to have a confident contraceptive method, so the likelihood of an unwanted pregnancy is high for them. They do not care about the serious riskiness of pregnancy. A diabetes trained general physician says: “Most of the patients apply unreliable contraceptive methods. We should instruct them”.
An endocrinologist states: “We do not care about women's contraceptive methods. I think they mostly use unreliable methods and do not know that conception is highly risky for them. We do not have time to provide them with training”.
A woman with diabetes states: “I have been applying natural method and using a condom for 6 years.”
Family's unawareness about diabetes complications and pregnancy
Family's unawareness of pregnancy's complications is among the most significant items mentioned by women with diabetes. Families are not aware of the combined effects of pregnancy and diabetes, which result in nonreferral for PCC and unplanned and repetitive conception. A diabetes trained general physician said says: “Husbands are usually unaware. When they find out about the complications, they accept and pursue the matter.”
A woman with diabetes states: “My husband does not care about my diabetes. He expects me to have three babies; I tell him, it's impossible, but he pays no attention.”
Diabetic women do not come to receiving receive preconception care
As expressed by most of the participants, another important problem was that women with diabetes do not refer to the centers on time to undergo PCC.
An endocrinologist says: “Patients scarcely refer to us before conception for pregnancy planning. They mainly come when they are pregnant”.
A midwifery expert asserts: “Women with diabetes usually refer to us when they are pregnant. They do not tell us that they are going to be conceived beforehand”.
A diabetic lady says: “I never went for consultation prior to any of my pregnancies. Nobody told me to go”.
Most of The PCC providers stated that few people intending to conceive referred to them for PCC. Endocrinologists offer no consultation regarding the pregnancy plan.
DISCUSSION
The first category of this research pertained to weakness in providing PCC for women with diabetes in health centers. The results indicated that PCC providers believed they did not have the required skill to provide the pregnant women with the PCC. They did not receive suitable training during their education and in their jobs. This lack of knowledge has led to unfavorable PCC quality. A study on midwives’ attitude about PCC showed that they were mainly familiar with PCC and were willing to have an active role in providing it, but the consultations were not mostly sufficient. Consultations were not offered before conception either because the women with diabetes referred at the end of the first 3-month.[23]
Results of the research conducted by Nekuei et al. on a number of midwifery students implied that most of them had an average level of knowledge and decision-making about PCC.[24] Findings of another research, which aimed at investigating the role of personnel's performance and training with regard to diabetic PCC, were indicative of the fact that most of the nurses were aware of the issue, but they had not been instructed precisely.[25] A study on family physicians with respect to providing PCC showed that the most received trainings were related to smoking and the least ones pertained to folic acid. Approximately all the participants believed that they had received meager instruction and should be instructed well.[26] In another study, midwives, while stressing that lack of awareness about the issue prevents providing proper PCC said that they required training in this regard.[23] Results of an instruction plan to diabetes instructors concerning PCC revealed the fact that they believed in the necessity of providing proper training before the instruction starts. Their awareness level was about 70% and their level of confidence was not high in this regard. Following the instruction, their awareness and confidence levels with respect to providing diabetic PCC increased significantly.[27]
Studies have shown that properly designed training program is effective in increasing the awareness of health care providers. Health care providers are very effective in controlling diabetes. Health systems need to design proper training and research programs in this area.[28] Lack of a comprehensive PCC plan for diabetic women, was the other major findings of the present study. Participants believed that managers’ negligence about fertility health of diabetic women was the major factor for the weakness in providing diabetic PCC, because gaining access to diabetic PCC requires a team; the key people to whom diabetic women refer shall refer them to PCC centers. Members of PCC team should be skilled, well-trained and ready for specified vocational responsibilities. Currently, diabetic women not only do not receive any sorts of fertility health services but also they themselves do not seriously care about referring to PCC centers. There is no comprehensive plan for screening diabetes in women of reproductive ages.
The results showed that social announcement about reproductive age diabetes and PCC is very weak while the diabetic women and their families should be very well informed about health maintenance in reproductive ages and receiving PCC through public notification. Based on the findings of Kapoor et al.'s study, providing team work PCC, is the key to have good pregnancy in diabetic women.[29] According to the participants’ opinions, all team members are responsible for providing services with specific duties. In fact, in order to achieve the best result from diabetic PCC, a team is required consisting of diabetes specialist or family physician, midwives, and nutritionists as well as trained instructors and social assistants. Several studies have implied that improvement of diabetic gestational maternal and fetal outcomes depends on having a proper understanding of the disease, providing training and using medical treatments using teamwork. Treatment of these patients consists of PCC, PNC procedures as well as providing cares during childbirth.[30] In a research on PCC experiences of health personnel, the personnel believed that consultation barriers included lack of clear scientific resources, having time restriction; restriction in consultation facilitating factors, the advancement made in terms of the methods of notifying the patients, applying electronic facilities, having a proper clinical care system and creating involvement in clinics and health systems. They were willing to access on-line resources during the consultation session.[31] Studies have demonstrated that lack of PCC for diabetic women is caused by systematic and individual agents.[32]
The first step in controlling diabetes and related complications is the use of basic methods to improve processes of care and services.[33] this should be done by the health system in several ways, such as electronic medical records, public education and others. Negligence of diabetic women's about having planned pregnancy was the last major finding of this research. With regard to the significance of family planning and conception adjustment under diabetes control conditions, diabetic women are expected to have the least number of children in appropriate intervals with proper planning and taking into account the disease circumstances. Awareness of the mutual complications of pregnancy and diabetes can have a significant impact on referring to the centers to receive PCC services. Results indicated that most of diabetic women in the current study avoided effective contraceptive methods due to their disease and preferred withdrawal method and condom. On the other hand, families are also unaware of the complications of unplanned and repetitive pregnancies. These factors cause most women to refer to health centers during their pregnancy when the chances of PCC are lost.
A study was carried out about the use of contraceptives in women with diabetes.
There was the difference in view of women with diabetes and diabetes specialists associated with contraception in this research. Many diabetes specialists felt that they have no sufficient power to provide adequate contraception to women with diabetes, and health care providers should do it. Most women with diabetes were using natural methods and they did not want to use hormone.[34]
A research was conducted by Rodrigues et al. on diabetic women with the aim of investigating the condition of blood sugar control before conception and using family control plan. The results showed that 42% had received recommendations about blood sugar control and 37% had used the family control plan. Final results suggested that the PCC's rate diabetic women are provided with is low and unfavorable.[35] A study on diabetic women by Murphy et al. showed that they had some information about diabetes and pregnancy: PCC benefits: 90%, necessity of blood sugar control: 80%, abnormality risk: 48% and macrosomia disorder: 35%. Most of them did not use planned contraceptive methods (70%). Some 45% had stopped using contraceptive methods personally and 14% had done that due to the side effects and contraindications. Awareness of pregnancy risks (90%), undergoing former PCC (38%) and having experience of poor pregnancy outcomes did not encourage them to attend PCC clinics.
Unpredicted pregnancy and having negative experiences about the personnel were among the causes for not attending PCC centers.[36] In a qualitative study, which was done by Mersereau, the health staff stated that a small number of diabetic patients plan their pregnancy; some of them have little information about the complications of diabetes and pregnancy. They believe that the obstacles on the way of blood sugar control in diabetic women were lack of knowledge, not having access to facilities and having disordered attitude. Their research result suggested that it is vital to instruct diabetic women with respect to pregnancy and diabetes and the significance of practicing contraception until succeeding in complete blood sugar control, which all together can lead to the reduction in the risk of pregnancy's side-effects and diabetes.[37] It was shown in another research that diabetic women had insufficient knowledge about the risks of diabetes and pregnancy.[38] A study was done about factors in relation to self-care diabetic women. The obtained results showed that the quality and quantity of expectations, performance and support of the family were the important barriers and facilitators of self-care.[39,40] Self-care is an important factor in prepregnancy diabetic care. According to the above study knowledge and positive reinforcement of the family can be effective in this area. The family that plays an important role in providing and receiving of PCC. Studies suggest that family education on diabetes that will help diabetic patient having a proper support system to receive properly care.[41] Family education especially husband can be a factor in improving PCC in women with diabetes. The studies accentuated that diabetic women's attendance in PCC clinics and having planned pregnancy are crucial factors in reduction of complications, in particular with regard to prenatal mortality, and thus, diabetic women and their care providers shall be aware of PCCs significance.[11] In a qualitative study aimed to assess the knowledge and attitudes of women with chronic diseases associated with health before pregnancy the following results were derived: Limited awareness of the risks associated with pregnancy related chronic illness, limited awareness of health before pregnancy and lack of proper operation to prevent unwanted pregnancy in relation to lack of awareness about the impact of chronic diseases on the choice of contraception. Chronic diseases did not encourage them to attend prepregnancy care.[42]
Increased awareness and attitudes through counseling before pregnancy can reduce the risk of unintended pregnancy.[43] By properly informing diabetic women when drawing up plans to improve diabetic women's fertility health, the possibility of conscious referring to the clinics can be increased. Health care centers are supposed to have skilled and well trained personnel to provide PCC services. Training the personnel and holding re-instructional courses are among the most fundamental measures, which need to be taken in this regard. Diabetes specialists should become sensitive to providing fertility consultations for diabetic women and refer them to the relevant centers. Launching special centers for fertility health consultation in diabetes and screening diabetes is vital, particularly in reproductive ages. There should be skilled personnel at PCC alongside such physicians in order to help diabetic women and their families to plan for their pregnancy; alternatively there should be a suitable reference system so that diabetes doctors can send their patients to skilled personnel at PCC centers.
Footnotes
Source of Support: Isfahan University of Medical Sciences (184031)
Conflict of Interest: None declared
REFERENCES
- 1.Wolfson EM, DeKalb A, Rojhani A. Women's health in the 21 st century. Int J Gynaecol Obstet. 2009;104:S2–3. doi: 10.1016/j.ijgo.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence JM. Women with diabetes in pregnancy: Different perceptions and expectations. Best Pract Res Clin Obstet Gynaecol. 2011;25:15–24. doi: 10.1016/j.bpobgyn.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Vargas R, Repke JT, Ural SH. Type 1 diabetes mellitus and pregnancy. Rev Obstet Gynecol. 2010;3:92–100. [PMC free article] [PubMed] [Google Scholar]
- 4.Alikhani S. Iran: [Date of access: 13 Jan 2015]. A national profile of NCD risk factors in the I.R. Iran. Selected results of the first survey of the Iranian NCD risk factor surveillance system 2005, Ministry of Health and Medical Education. Center for Disease Control. Available from: http://www.who.int/chp/steps/IR_IranSTEPSReport.pdf . [Google Scholar]
- 5.Temple R, Murphy H. Type 2 diabetes in pregnancy-An increasing problem. Best Pract Res Clin Endocrinol Metab. 2010;24:591–603. doi: 10.1016/j.beem.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 6.Roglic G. Diabetes in women: The global perspective. Int J Gynaecol Obstet. 2009;104(Suppl 1):S11–3. doi: 10.1016/j.ijgo.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 7.Sabaratnam A. Diabetes in pregnancy. Best Pract Res Clin Obstet. 2011;25:1. doi: 10.1016/j.bpobgyn.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Damti A, Riskin-Mashiah S. Preconception care and counseling for women with diabetes and those at risk for diabetes. Harefuah. 2009;148:447–51. 475. [PubMed] [Google Scholar]
- 9.Inkster ME, Fahey TP, Donnan PT, Leese GP, Mires GJ, Murphy DJ. The role of modifiable pre-pregnancy risk factors in preventing adverse fetal outcomes among women with type 1 and type 2 diabetes. Acta Obstet Gynecol Scand. 2009;88:1153–7. doi: 10.1080/00016340903176859. [DOI] [PubMed] [Google Scholar]
- 10.Melamed N, Chen R, Soiberman U, Ben-Haroush A, Hod M, Yogev Y. Spontaneous and indicated preterm delivery in pregestational diabetes mellitus: Etiology and risk factors. Arch Gynecol Obstet. 2008;278:129–34. doi: 10.1007/s00404-007-0541-z. [DOI] [PubMed] [Google Scholar]
- 11.Hawdon JM. Babies born after diabetes in pregnancy: What are the short- and long-term risks and how can we minimise them? Best Pract Res Clin Obstet Gynaecol. 2011;25:91–104. doi: 10.1016/j.bpobgyn.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Melamed N, Hod M. Perinatal mortality in pregestational diabetes. Int J Gynaecol Obstet. 2009;104(Suppl 1):S20–4. doi: 10.1016/j.ijgo.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 13.Tieu J, Middleton P, Crowther CA. Preconception care for diabetic women for improving maternal and infant health. Cochrane Database Syst Rev. 2010;8(12):CD007776. doi: 10.1002/14651858.CD007776.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Wender-Ozegowska E, Gutaj P, Szczepanek U, Ozegowska K, Zawiejska A, Brazert J. Influence of pregnancy planning on obstetrical results in women with pregestational diabetes mellitus. Ginekol Pol. 2010;81:762–7. [PubMed] [Google Scholar]
- 15.Temple R. Preconception care for women with diabetes: Is it effective and who should provide it? Best Pract Res Clin Obstet Gynaecol. 2011;25:3–14. doi: 10.1016/j.bpobgyn.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Wahabi HA, Alzeidan RA, Bawazeer GA, Alansari LA, Esmaeil SA. Preconception care for diabetic women for improving maternal and fetal outcomes: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2010;10:63. doi: 10.1186/1471-2393-10-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tripathi A, Rankin J, Aarvold J, Chandler C, Bell R. Preconception counseling in women with diabetes: A population-based study in the north of England. Diabetes Care. 2010;33:586–8. doi: 10.2337/dc09-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernasko J. Contemporary management of type 1 diabetes mellitus in pregnancy. Obstet Gynecol Surv. 2004;59:628–36. doi: 10.1097/00006254-200408000-00024. [DOI] [PubMed] [Google Scholar]
- 19.Kitzmiller JL, Wallerstein R, Correa A, Kwan S. Preconception care for women with diabetes and prevention of major congenital malformations. Birth Defects Res A Clin Mol Teratol. 2010;88:791–803. doi: 10.1002/bdra.20734. [DOI] [PubMed] [Google Scholar]
- 20.Mahmud M, Mazza D. Preconception care of women with diabetes: A review of current guideline recommendations. BMC Womens Health. 2010;10:5. doi: 10.1186/1472-6874-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy HR, Roland JM, Skinner TC. Effectiveness of a regional prepregnancy care program in women with type 1 and type 2 diabetes: Benefits beyond glycemic control. Obstet Gynecol Surv. 2011;66:189–91. doi: 10.2337/dc10-1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Negrato CA, Mattar R, Gomes MB. Adverse pregnancy outcomes in women with diabetes. Diabetol Metab Syndr. 2012;4:41. doi: 10.1186/1758-5996-4-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Heesch PN, de Weerd S, Kotey S, Steegers EA. Dutch community midwives’ views on preconception care. Midwifery. 2006;22:120–4. doi: 10.1016/j.midw.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Packguhar M, Nekui N, Khakbazan Z, Mahmud M. The midwifery students’ knowledge and clinical decision making skills about preconception care. Iran J Nurs Midwifery Res. 2008;13:65–71. [Google Scholar]
- 25.Michel B, Charron-Prochownik D. Diabetes nurse educators and preconception counseling. Diabetes Educ. 2006;32:108–16. doi: 10.1177/0145721705284371. [DOI] [PubMed] [Google Scholar]
- 26.Kitamura K, Fetters MD, Ban N. Preconception care by family physicians and general practitioners in Japan. BMC Fam Pract. 2005;6:31. doi: 10.1186/1471-2296-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cothran MM, Sereika SM, Fischl AR, Schmitt PL, Charron-Prochownik D. A self-instructional program for diabetes educators on preconception counseling for women with diabetes. Diabetes Educ. 2009;35:652–6. doi: 10.1177/0145721709334516. [DOI] [PubMed] [Google Scholar]
- 28.MakkiAwouda FO, Elmukashfi TA, Hag Al-Tom SA. Designing an educational and training program for diabetes health educators at Diabetic Health Centers, Khartoum State, Sudan; 2007-2010. Glob J Health Sci. 2013;5:207–11. doi: 10.5539/gjhs.v5n5p207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kapoor N, Sankaran S, Hyer S, Shehata H. Diabetes in pregnancy: A review of current evidence. Curr Opin Obstet Gynecol. 2007;19:586–90. doi: 10.1097/GCO.0b013e3282f20aad. [DOI] [PubMed] [Google Scholar]
- 30.Pridjian G. Pregestational diabetes. Obstet Gynecol Clin North Am. 2010;37:143–58. doi: 10.1016/j.ogc.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 31.Schwarz EB, Santucci A, Borrero S, Akers AY, Nikolajski C, Gold MA. Perspectives of primary care clinicians on teratogenic risk counseling. Birth Defects Res A Clin Mol Teratol. 2009;85:858–63. doi: 10.1002/bdra.20599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hone J, Jovanovic L. Approach to the patient with diabetes during pregnancy. J Clin Endocrinol Metab. 2010;95:3578–85. doi: 10.1210/jc.2010-0383. [DOI] [PubMed] [Google Scholar]
- 33.Pollard C, Bailey KA, Petitte T, Baus A, Swim M, Hendryx M. Electronic patient registries improve diabetes care and clinical outcomes in rural community health centers. J Rural Health. 2009;25:77–84. doi: 10.1111/j.1748-0361.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- 34.Shawe J, Smith P, Stephenson J. Use of contraception by women with type 1 or type 2 diabetes mellitus: ‘it's funny that nobody really spoke to me about it’. Eur J Contracept Reprod Health Care. 2011;16:350–8. doi: 10.3109/13625187.2011.597896. [DOI] [PubMed] [Google Scholar]
- 35.Rodríguez-Vigil E, Kianes-Pérez Z. Quality of care provided to patients with diabetes mellitus in Puerto Rico; managed care versus fee-for-service experience. Endocr Pract. 2005;11:376–81. doi: 10.4158/EP.11.6.376. [DOI] [PubMed] [Google Scholar]
- 36.Murphy HR, Temple RC, Ball VE, Roland JM, Steel S, Zill-E-Huma R, et al. Personal experiences of women with diabetes who do not attend pre-pregnancy care. Diabet Med. 2010;27:92–100. doi: 10.1111/j.1464-5491.2009.02890.x. [DOI] [PubMed] [Google Scholar]
- 37.Mersereau P, Williams J, Collier SA, Mulholland C, Turay K, Prue C. Barriers to managing diabetes during pregnancy: The perceptions of health care practitioners. Birth. 2011;38:142–9. doi: 10.1111/j.1523-536X.2010.00464.x. [DOI] [PubMed] [Google Scholar]
- 38.Diabetes and Pregnancy Group. Knowledge about preconception care in French women with type 1 diabetes. Diabetes Metab. 2005;31:443–7. doi: 10.1016/s1262-3636(07)70214-8. [DOI] [PubMed] [Google Scholar]
- 39.Shen H, Edwards H, Courtney M, McDowell J, Wei J. Barriers and facilitators to diabetes self-management: Perspectives of older community dwellers and health professionals in China. Int J Nurs Pract. 2013;19:627–35. doi: 10.1111/ijn.12114. [DOI] [PubMed] [Google Scholar]
- 40.Shiau SJ, Cheng LS, Gau BS, Tsai LM, Lin BJ. The effects of management difficulty and family functions on metabolic control of insulin-dependent diabetes mellitus. Gaoxiong Yi Xue Ke Xue Za Zhi. 1995;11:157–63. [PubMed] [Google Scholar]
- 41.Li J, Drury V, Taylor B. ‘Diabetes is nothing’: The experience of older Singaporean women living and coping with type 2 diabetes. Contemp Nurse. 2013;45:188–96. doi: 10.5172/conu.2013.45.2.188. [DOI] [PubMed] [Google Scholar]
- 42.Chuang CH, Velott DL, Weisman CS. Exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions. Matern Child Health J. 2010;14:713–9. doi: 10.1007/s10995-009-0518-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Charron-Prochownik D, Sereika SM, Falsetti D, Wang SL, Becker D, Jacober S, et al. Knowledge, attitudes and behaviors related to sexuality and family planning in adolescent women with and without diabetes. Pediatr Diabetes. 2006;7:267–73. doi: 10.1111/j.1399-5448.2006.00197.x. [DOI] [PubMed] [Google Scholar]


