Abstract
Techniques for digital pathology are envisioned to provide great benefits in clinical practice, but experiences also show that solutions must be carefully crafted. The Nordic countries are far along the path toward the use of whole-slide imaging in clinical routine. The Nordic Symposium on Digital Pathology (NDP) was created to promote knowledge exchange in this area, between stakeholders in health care, industry, and academia. This article is a summary of the NDP 2014 symposium, including conclusions from a workshop on clinical adoption of digital pathology among the 144 attendees.
Keywords: Clinical adoption, digital pathology, image analysis, informatics, whole-slide imaging
INTRODUCTION
The introduction of digital technologies in clinical pathology practice could produce great benefits in the form of improved patient care, better efficiency of health services, and novel diagnostic tools.[1,2] At the same time, it is clear that these benefits can only be achieved if digital pathology solutions are carefully crafted for the clinical prerequisites. Whereas low-volume and nonurgent situations such as research, teaching, and to some extent, consultations, are currently feasible with existing digital pathology systems, if digital pathology is to reach prime time status then more work is needed to enhance the suitability of the systems for clinical routine. Clinical deployment also requires solving issues such as validation mechanisms, cost-efficient digital storage, and medico-legal demands, as well as redesigning work practices for the digital era.
Efforts to advance the field are taking place around the world. In the Nordic countries (Sweden, Denmark, Norway, Finland, and Iceland), there is a particular concentration of development work towards clinical use of whole slide imaging (WSI). For example, all routine histology slides are today scanned in the hospitals of Linköping and Kalmar and extensive digital primary review is performed,[3] and >60 WSI scanners have been installed in Sweden to date.
Against this backdrop, the Nordic Symposium on Digital Pathology (NDP) was created to promote knowledge exchange regarding the state-of-the-art in digital pathology. The specific focus of NDP is advances toward the clinical adoption of WSI and other digital technologies in pathology. As these advances require a concerted effort from health care, industry, and academia, NDP is intended as a forum where professionals from all domains can meet. The first NDP event was organized in November 2013 and attracted 125 attendees, whose feedback lead to an expanded NDP event in November 2014 as will be detailed below.
Judging from the history of digitization of radiology imaging, there is reason to believe that the Nordics will continue to be a forerunner in clinical use of digital pathology. While perhaps not reflected by its regional name, NDP aims to be a venue of broad international interest where state-of-the-art in digital pathology is discussed and advanced. This article is a summary of the NDP 2014 symposium.
MEETING OVERVIEW
Nordic Symposium on Digital Pathology Symposium 2014 took place November 5–6 in Linköping, Sweden. A total of 144 attendees gathered, of which 47% listed health care as the primary affiliation, 33% industry, and 19% academia. The health care representatives were dominated by pathologists, but also laboratory technologists and IT staff were in significant numbers. The participants represented 14 different countries from Europe, North America, and Australia, with the Nordic attendees being in a large majority (87%).
Central to the program was a series of invited talks and a collaborative workshop on clinical deployment issues. The contents of these sessions will be outlined in the sections below. In the science and innovation session, 15 posters were presented, and top contributions were invited to submit full papers. A double-blind review process was carried out by the symposium's International Program Committee with 15 senior researchers in the field and this resulted in three JPI papers published alongside this editorial: “A comparative study of input devices for digital slide navigation” (Jesper Molin et al.), “RandomSpot: a web-based tool for systematic random sampling of virtual slides” (Alexander Wright et al.), and “Histopathology in three-dimensional: From three-dimensional reconstruction to multi-stain and multi-modal Analysis” (Derek Magee).
In addition, the NDP included an industrial exhibition consisting 13 vendors, ranging from large multinationals to recent startups, showing everything from WSI scanners through enterprise image management to desktop electron microscopy. Figure 1 shows a session snapshot and the program details are available at the NPD website http://www.liu.se/ndp?l=en.
Figure 1.

Nordic Symposium on Digital Pathology attendees assembled for the keynote of Dr. Evans
WORKSHOP ON CLINICAL DEPLOYMENT OF DIGITAL PATHOLOGY
A key part of the NDP program was the workshop discussing clinical adoption of digital pathology. The workshop was organized as an open floor discussion where broad participation was encouraged and also achieved. As an input to the discussion, a survey was distributed among the health care attendees in advance of the symposium. Some results from this survey will be presented next as it paints an interesting picture of the attitude toward digital pathology in Nordic health care.
It must be noted that the respondents of the survey represents an extremely biased selection among the pathology community. Since only NDP participants were asked, this means that respondents are likely to be among the most positive to digital pathology and also among the most experienced. There is also strong geographical dominance from the Nordics and in particular Sweden. Of 74 receiving the survey, 44 responses were gathered. The distribution of roles is given in Figure 2. It is likely that the pathologist dominance were even higher for some questions that require deep knowledge of clinical practice.
Figure 2.
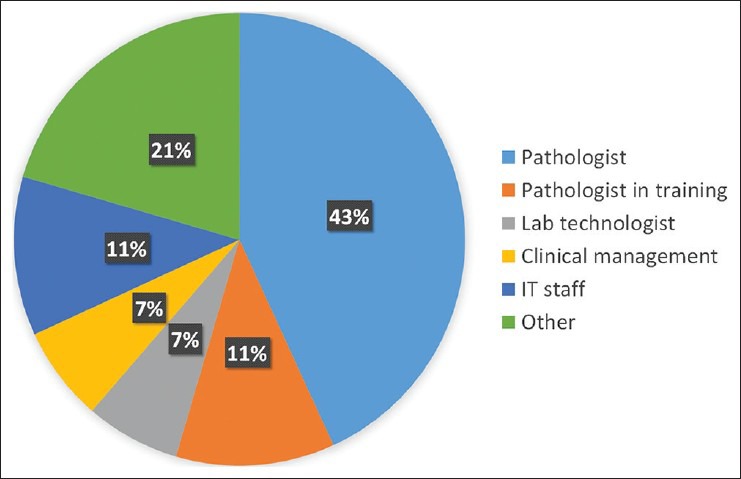
Role distribution of survey respondents
The survey first asked: “Today, to what degree do you use digital images of histology slides in your practice? (In % of all histology cases.)” The results are shown in Figure 3, showing moderate levels of adoption but no use in about 50% of respondents. Another bias to note for these questions is that several people from the same institution may have responded. Since the most digitized sites Kalmar and Linköping had several attendees, these numbers are likely to represent higher usage than numbers on a per site basis.
Figure 3.
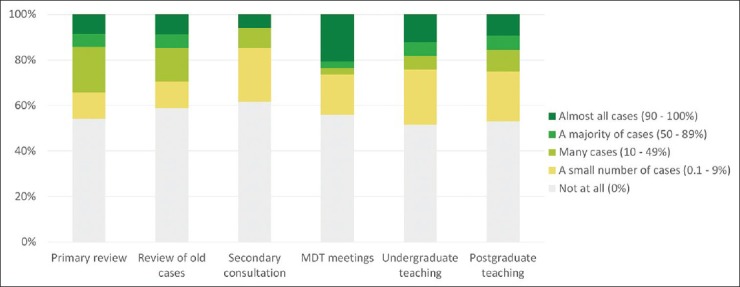
Current use of digital pathology among survey respondents
The same question was asked for the predicted situation at the end of 2016, shown in Figure 4, showing significant optimism for near-future use of digital pathology.
Figure 4.
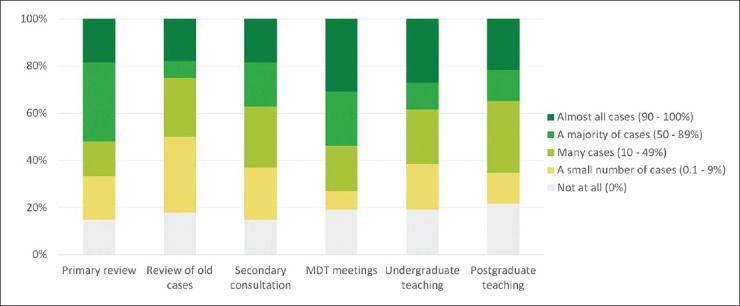
Predicted use of digital pathology at the end of 2016
The respondents were also asked to judge the impact of digitization: “What effect do you foresee that digital pathology will have compared to traditional microscope practice, with regards to the following areas?” The impact grading was given in a five-point scale, “Major negative”–“Minor negative” – “Status quo” – “Minor positive” – “Major positive.” The assessments with regards to pathologist work are in Figure 5 whereas other laboratory aspects are in Figure 6 and overall impact in Figure 7.
Figure 5.
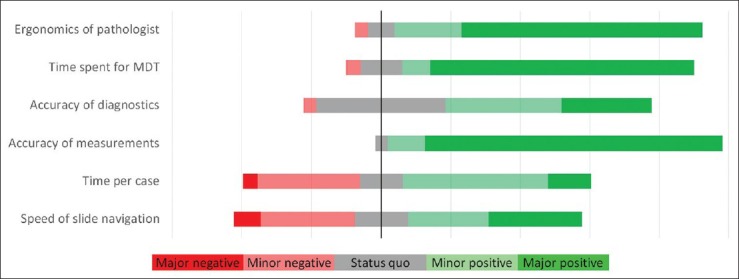
Foreseen impact of digitization with regards to pathologist's work
Figure 6.
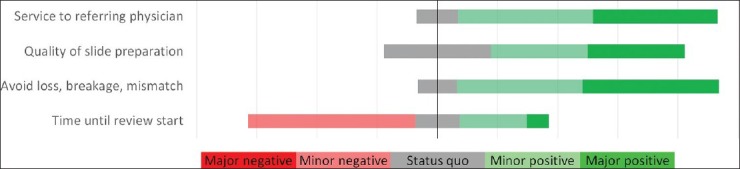
Foreseen impact of digitization with regards to laboratory aspects
Figure 7.

Foreseen impact of digitization with regards to overall effects
Broadly, these responses indicate a very positive attitude toward digital pathology in terms of its effects on pathologist and laboratory working. However, more negative responses were received in the effect on pathologists’ efficiency (time per case and speed of slide navigation) as well as perceived delays in slide arrival from the laboratory until starting review. Overall effects of digitization were seen as very positive, especially for the quality of care. Some concerns about the cost for the pathology department are reflected in Figure 7.
Finally, the respondents also were asked to state the three main barriers for adoption of digital pathology in their clinical practice. It was clear that the cost of implementation is a major issue; 79% of the responses mentioned lack of sufficient funds as a barrier. Technology limitations were listed in 71% of the responses, some referring to insufficient performance of commercial solutions and some referring to lacking IT infrastructure in their organization. A conservative attitude among colleagues was brought up as a barrier by 46%. Other responses concerned lack of organizational engagement at local, national and international levels to develop protocols, work practices, and standards.
After the survey results had been presented, a guided discussion between all participants took place. A summary of the overall themes discussed follows.
Advanced digital pathology implementation efforts were reported by many contributors, either established (e.g. Skåne, Linköping) or in planning (e.g., Gothenburg, Karolinska/Stockholm, Oslo, Copenhagen). The planned use cases covered similar areas such as retrieving archived cases, presenting at multi-disciplinary meetings, obtaining second opinions (either for individual cases or to share work between institutions). Digital pathology was seen by many contributors as a key enabler of higher quality pathology services, by increasing specialist reporting of cases or supporting and supporting colleagues across distances. Those who had implemented digital pathology on a large scale were positive about the effects it had on workflow and reported no untoward delay in slide arrival caused by the extra step of scanning (in fact, one pointed out that the cases arrived in a more continuous flow, rather than the batches of glass slides normally received).
Pathologists working with digital images all day long were discussed. Several contributors (Linköping, Skåne, Toronto) had experience of working with moderate or large volumes of the digital work. Fatigue using DP systems was mentioned by a few, possibly a combination of older less effective slide viewing software and the known effect of computer displays on eye fatigue. Several experienced commenters pointed out that fatigue was often an issue with the microscope and that digital pathology offered ergonomic benefits which could be beneficial in the long term for the pathologist's experience.
Data storage was a very commonly raised issue. Laboratories produce a lot of glass slides, and WSIs produce large amounts of storage space. It was felt that data storage was very often raised as a concern by IT departments involved in discussions about digital pathology implementations. Some contributors pointed out that projections of hundreds of terabytes of image data per year, while realistic for 100% digital practice, may serve to inhibit pathologists and IT departments from trying the technology, and that in fact to start going digital-only a modest storage capacity of a few terabytes is needed. IT contributors pointed out that mature information lifecycle management systems for digital pathology had yet to appear (some contributors reported being charged excessive monthly costs for even small amounts of data), but it was likely that tiered storage systems would ameliorate the daunting costs associated with large amounts of live online storage, as would the constant reduction in price per terabyte of storage media. Some discussion around how long digital images should be kept for and what latency before image retrieval might be tolerated revealed that several contributors had envisaged such tiered data arrangements would be needed.
IT support was a common issue in the group. Experience and knowledge of IT departments with digital pathology ranged from none to extensive. Centers with mature or second-generation digital pathology systems often had IT staff who understood well the complexities of WSI data, and well-integrated systems. Others reported poor experiences with IT departments not fully engaging with digitization efforts. Experienced users re-emphasized the need for digital pathology to be supported by knowledgeable and (preferably) designated IT staff.
Standards were mentioned by only a few contributors - the IT staff, who expressed surprise at the lack of standardization of digital pathology image formats and interoperability, and those pathologists on their second generation of scanners who had experienced incompatibility between two different vendors products (e.g. in viewers or in image analysis algorithms).
Some audience members had experience of the last digital revolution in medical imaging (in radiology) and saw many parallels in the IT needs, questions about validation/safety and clinical acceptance of the technology.
The room was understandably full of those keen to adopt digital pathology, many of whom reported colleagues with more conservative attitudes. Some of the objections were seen, however, as entirely justifiable (e.g. concerns over speed of diagnosis and diagnostic accuracy with digital systems) and many in the room agreed that these were issues that needed to be addressed.
For successful implementations, the need for champions in each department was mentioned, as well as the value in immersing trainees in a digital working pattern from an early stage. Wiser (and older) heads pointed out the benefits of actively seeking out sceptics and involving them in digitization projects.
SPEAKER CONTRIBUTIONS
Dr. Andrew Evans from the University Health Network, Toronto described a long-standing program of digitization including telepathology and WSI in a university hospital network. He provided a very detailed description of the assiduous planning involved in digital pathology adoption and his experiences of involving the entire department in projects.
Dr. Metin Gurcan of Ohio State University spoke about his work in image analysis and computer aided diagnosis, introducing many parallels from radiological imaging and emphasizing the importance of pathologist-computer scientist partnerships and validation in such work.
Prof. Jan Baak from Stavanger University Hospital gave an expansive talk on his long career in pathology imaging, especially speaking about his role in the prognostication of breast cancer with morphology and image analysis, emphasizing the ongoing value of good pathological assessment even in a genomic era.
Dr. Sten Thorstenson from Linköping University Hospital explained his long experience of digital pathology at Kalmar and Linköping, starting at a time when a terabyte really was a large amount of data. After 9 years he reports being entirely comfortable working digitally and has been reporting 100% from home for almost a year now without access to a microscope or physical slides.
Dr. Derek Magee from the University of Leeds gave an overview of his work in image analysis research. A focus area has been digital three-dimensional pathology, and in particular tackling the inherent challenges of the slide registration, color normalization, and histology-radiology correlation.
Thomas Miliander from Värmland County Council, Sweden, presented this health-care provider's strategy for imaging IT infrastructure. The approach taken is an enterprise image management backbone for all medical images, relying on standards for tight integrations with other information systems, a context into which now also WSI is entering.
Dr. Johan Lundin from the Institute for Molecular Medicine Finland, Helsinki, provided an overview of his group's work in digital pathology. The portfolio presented spanned from web and touch-enabled WSI viewing applications to low-cost handheld microscopes utilizing smartphone camera components.
In a special session, Dr. Elin Kindberg of Sectra presented preliminary results from a national Swedish effort to investigate key medico-legal issues arising when deploying digital pathology. Regarding access to Swedish patient data outside of Sweden the legal situation is clear that this is possible provided those appropriate security measures are taken. Legal directions regarding whether all WSI data must be stored does not, however, exist; the Swedish law only mandates “good and safe health care.” The conclusion is that the pathology profession needs to define what the legal mandate means in this case. The Swedish pathologist society is now finalizing an official guideline document describing different possible paths, all legal, and all with different advantages and drawbacks.
CONCLUSIONS
The 2nd NDP spanned across many areas of interest with regards to the emerging use of WSI and related IT tools in clinical routine. Feedback from attendees indicates that this sharing of knowledge and experiences across organizations, disciplines, and sectors is an important catalyst for development of best practices and overall progress. Organizing NDP 2014 has been a very rewarding experience, and we welcome attendees from all over the globe to future gatherings of this group.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2015/6/1/5/151889
REFERENCES
- 1.Cooper LA, Carter AB, Farris AB, Wang F, Kong J, Gutman DA, et al. Digital Pathology: Data-Intensive Frontier in Medical Imaging: Health-information sharing, specifically of digital pathology, is the subject of this paper which discusses how sharing the rich images in pathology can stretch the capabilities of all otherwise well-practiced disciplines. Proc IEEE Inst Electr Electron Eng. 2012;100:991–1003. doi: 10.1109/JPROC.2011.2182074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ho J, Ahlers SM, Stratman C, Aridor O, Pantanowitz L, Fine JL, et al. Can digital pathology result in cost savings? A financial projection for digital pathology implementation at a large integrated health care organization. J Pathol Inform. 2014;5:33. doi: 10.4103/2153-3539.139714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thorstenson S, Molin J, Lundström C. Implementation of large-scale routine diagnostics using whole slide imaging in Sweden: Digital pathology experiences 2006-2013. J Pathol Inform. 2014;5:14. doi: 10.4103/2153-3539.129452. [DOI] [PMC free article] [PubMed] [Google Scholar]


