Abstract
The CRONICAS Centre of Excellence in Chronic Diseases, based at Universidad Peruana Cayetano Heredia, was created in 2009 with support from the United States National Heart, Lung, and Blood Institute (NHLBI). The vision of CRONICAS is to build a globally recognised Centre of Excellence conducting quality and innovative research and generating high-impact evidence for health. The Centre’s identity is embedded in its core values: generosity, innovation, integrity, and quality. This review has been structured to describe the development of the CRONICAS Centre, with a focus on highlighting the ongoing translational research projects and capacity building strategies. The CRONICAS Centre of Excellence is not a risk-averse organisation: it benefits from past experiences, including past mistakes, and improves upon them, and thus challenges traditional research approaches. This ethos and environment is key to fostering innovation in research.
A CENTRE OF EXCELLENCE IN PERU
Established in Peru, the CRONICAS Centre of Excellence in Chronic Diseases is based at Universidad Peruana Cayetano Heredia and was founded to close the research and capacity building gap in relation to non-communicable diseases (NCDs) in Peru. In Peru, the field of NCDs is still nascent in nearly all of its constituencies, from research to training to policy intervention. The CRONICAS Centre of Excellence serves as a collaborative research platform for NCDs and signals an example of a Peruvian-based, internationally funded, and horizontally led group conducting relevant research in various fronts, as described in this manuscript.
The CRONICAS Centre’s mission dictates our “commitment to train young researchers and collaborate with local and international institutions. Our motivation is to improve population health through high quality research.” Our vision is that “by 2024 CRONICAS will be a globally recognised Centre of Excellence, conducting quality and innovative research and generating high-impact evidence for health.”
The Centre was established in 2009 with support from the NHLBI, part of the U.S. National Institutes of Health. Within five years of its inception, the Centre has demonstrated that it is a recognised research-oriented and capacity-building group, both in the Peruvian and international context. It operates under its core values of generosity, innovation, integrity and quality, and brings together a multidisciplinary team from diverse backgrounds such as anthropology, communications, economy, medicine, nutrition, psychology, biostatistics, epidemiology, and public health.
The CRONICAS Centre of Excellence was built on the foundations of an established research-driven environment fostered within Universidad Peruana Cayetano Heredia. The consortium with Johns Hopkins University, one of many at Universidad Peruana Cayetano Heredia, provided a leveraging platform to conduct large-scale non-communicable disease-related population-based surveys. This collaboration enabled cross-fertilisation between public health, clinical medicine, and epidemiology and was able to nurture long-term visions for a highly productive research and training platform. Another initiative that created awareness about the importance of broadening the scope of research in low- and middle-income countries was the “Global Health Peru Program”[1, 2], funded by the Fogarty International Center. These initiatives, paired with solid international collaborations and partnerships, contributed to the creation of a critical mass aware of the major challenges facing global health. This capacity, based in Peru, was able to foster talent under a unique and exquisite academic environment within Universidad Peruana Cayetano Heredia.
Having an established Centre of Excellence within Peru that operates under a “locally-based yet globally competitive” approach, without sacrificing quality, signals a clear message to future researchers. Peru is developing and expanding its critical mass for conducting research, and in addition to decades of efforts in infectious diseases research and longstanding collaborative consortia, NCDs appear today as an attractive option for the development of younger generations of researchers and highly-qualified professionals.
INFORMING GLOBAL HEALTH AND IMPLEMENTATION SCIENCE
Currently, there is no non-communicable disease surveillance system in Peru, making accurate monitoring of the nine global non-communicable disease targets impossible[3, 4]. At the national level, hypertension prevalence is 21%[4], diabetes 4.5%[5], and NCDs are estimated to account for 66% of total deaths[4]. However, mortality profiles are heterogeneous throughout the country[6]. Peru’s diverse geography combined with varying levels of urbanisation and access to services accounts for the different stages of the epidemiological transition in different populations[7].
Most cardiovascular diseases and their risk factors have socioeconomic patterns. In this vein, Peru’s geographical scenario—with within-country variations in disease burden and disparity in healthcare delivery—adds complexities to the understanding of NCDs in low- and middle-income countries. These context-specific differences could help to explain how cardiovascular diseases appear, co-exist, and progress towards long-term complications and deaths. They also introduce additional considerations for non-communicable disease research programs in Peru.
This review has been structured to describe the development of the CRONICAS Centre. It highlights ongoing translational research projects that the center has undertaken in an effort to achieve its mission. This review is not intended to present project-specific findings, but to sensitize readers to eagerly anticipate the results of ongoing projects relevant to the country and the Latin American region. The reason for this is twofold. First, most research on NCDs has been conducted in high-income countries, but the need for research in low- and middle-income countries has been recognized[8]. Second, by understanding these research questions and its scope, we will be better positioned to address unanswered questions in the realms of post-clinical translational research and implementation science, much needed to advance global health and health inequities in general.
ONGOING TRANSLATIONAL RESEARCH PROJECTS
Late stage (T3 and T4) translational research is defined as “investigations that seek to establish in real world settings the effectiveness of proven efficacious interventions, including ensuring the appropriate adoption and implementation of such interventions with sustainable investment models.” T4 translational research ensures that evidence-based interventions are broadly applied and accessible to those who need them most, with a strong emphasis on dissemination and implementation in real world settings[9, 10].
In this section we describe different initiatives directly related to late stage translational research being conducted by our Centre, within Peru (Figure 1) and internationally (Figure 2). We initiate characterising the epidemiological burden that serve as the basis to propose research interventions. We then present multi-country studies working under the same or similar study protocols followed by specific examples of translational research in different spheres, i.e. interventions with expected impacts at the population-level, the community-level, and the individual clinical level. Studies focusing on healthcare organisation and delivering evidence-based healthcare are also reviewed, using them as examples for assessing what works in real world settings.
Figure 1. Study sites of ongoing projects in Peru.
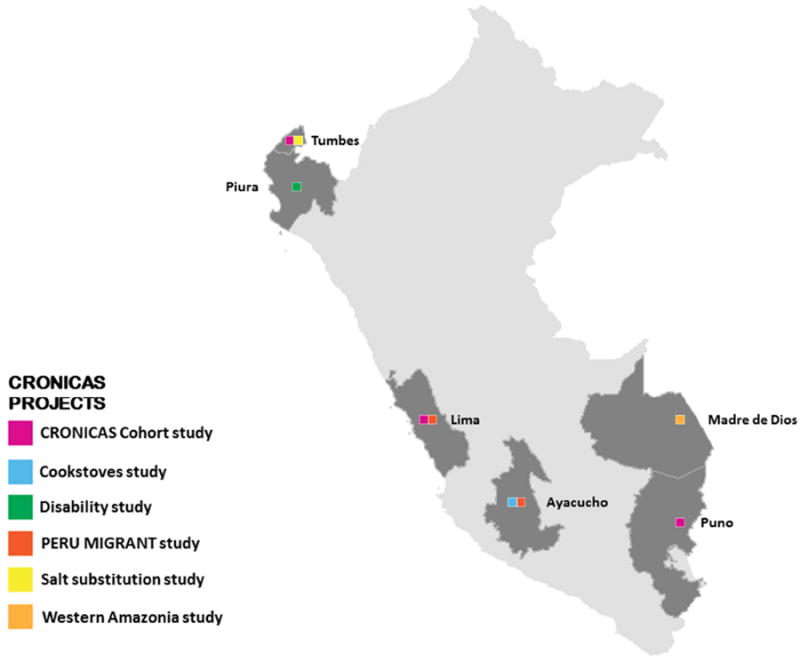
Figure 2. Global map of network collaborations.

Characterising the epidemiological context
Our Centre is extremely aware of the need to investigate what works in real world settings. Peru is a country that hosts desert coastal, Andean mountainous, and rainforest Amazonian ecological niches, hence adding complexity to the human-environment-disease interactions. In keeping with this, our Centre launched two population-based studies to characterise, in more detail, cardiovascular and pulmonary risk factor profiles in different geographical regions (Table 1). This was conducted initially in rural and urban populations with a particular emphasis on the effects of migration (PERU MIGRANT Study, Box 1), and then in low and high altitude settings to further advance our understanding of rates of progression to disease in different environments (CRONICAS Cohort Study, Box 2).
Table 1.
Research study sites, CRONICAS Cohort Study
| Setting | Degree of urbanisation | Use of biomass fuels | Outdoor air pollution | Altitude |
|---|---|---|---|---|
| Lima | Highly urbanised | Rare | High | Sea level |
| Tumbes | Semi-urban | Highly prevalent | Low | Sea level |
| Puno, urban | Urban | Rare | Low | 3825 meters above sea level |
| Puno, rural | Rural | Highly prevalent | Low | 3825 meters above sea level |
Source: CRONICAS cohort study protocol[35].
Box 1. PERU MIGRANT Study.
Urbanisation, in historical terms, is a fairly recent phenomenon: in 1975 only 27% of people in low- and middle-income countries lived in urban areas, but by 2000 the proportion was 40%. Projections suggest that by 2030 low- and middle-income countries will be 56% urban[36]. Rapid urbanisation, including rural-to-urban within-country migration, will certainly have significant impact on the profile of risk factors for non-communicable diseases (NCDs), patterns of risk exposures, and potential outcomes[37].
The cardiovascular, metabolic and inflammatory risk factor profiles of rural, urban, and rural-urban Andean immigrants were explored to demonstrate that uniform risk profiles are not the norm, and are influenced by the age at which migration occurs[38]. This study, funded by the Wellcome Trust, also demonstrated that using glycosylated haemoglobin for the diagnosis of diabetes, as per recent recommendations, would treble its prevalence compared to fasting glucose[39], possibly explained by discrepancies between haemoglobin-glucose in low versus high altitude settings. Data generated by this study has demonstrated important health burdens among immigrant population and socioeconomically deprived groups in terms of mental health and social capital[40], physical activity[41], acculturation[42], as well as awareness, treatment, and control gaps in hypertension and diabetes[43].
Among broader impacts of these findings, the PERU MIGRANT study is among the very few studies that have contributed Andean population data in the analyses of global trends[44, 45], avoiding the task of data imputation on the region. At the local level, it highlights challenging scenarios for local within-country health prioritization in terms of NCDs[46].
Box 2. CRONICAS Cohort Study.
Understanding the effects of rapid urbanisation is one of the grand challenges concerning chronic non-communicable diseases[47]. Peru offers a unique opportunity to assess the impact of geographical variation on non-communicable diseases, hence the rationale for the CRONICAS Cohort Study[35]. Importantly, the comprehensive data generated by this cohort across a diversity of scenarios will, in turn, provide important advances for public health and for the field of non-communicable diseases in low- and middle-income countries.
The CRONICAS Cohort Study has two main aims. Firstly, evaluation of the effects of variation in geographical settings on both cardiovascular and chronic pulmonary disease using a longitudinal design. Secondly, being aware of the reliance on biomass fuels, a feature that distinguishes low- from high-income countries, we are also looking into the longitudinal evaluation of lung function across different settings[48]. Exposure to by-products of biomass fuel combustion is considered to be the most important risk factor for COPD after cigarette smoking[49].
The CRONICAS Cohort Study, a joint effort between Universidad Peruana Cayetano Heredia and Johns Hopkins University; it is funded by the United States’ National, Heart, Lung and Blood Institute, and has been implemented in different population sites with varying degrees of urbanisation, air pollution and altitude features (Table 1). The choice of these populations provides the opportunity to study the potential effects of geographical location and other risk factors unique to low- and middle-income countries. For example, our group has characterised differences in household environmental exposures between urban and rural settings[48], and reported a link between chronic exposure to biomass fuel and increased carotid artery intima-media thickness[50].
Multi-country studies
Through the UnitedHealth Group/NHLBI Centres of Excellence Network[11, 12], our group has actively participated in designing and conducting pragmatic clinical trials with a direct focus on prevention and implementation. Together with teams from Argentina, Guatemala, and the U.S., we explored the use of mobile technology (mHealth) to prevent the progression of pre-hypertension in urban settings, capitalising on the commonalities of the Spanish language across countries and the potential of mHealth to deploy elements of preventative health (ClinicalTrials.gov NCT01295216). Similarly, together with teams from Kenya, Nepal, and the U.S., we worked on a feasibility intervention trial of two types of improved cookstoves (ClinicalTrials.gov NCT01686867) to ascertain practical approaches to increasing its uptake and usage[13].
Recognising the large burden of hypertension and stroke, the family oriented provision of care, and the low-resource and geographically isolated health system infrastructures[14], we are collaborating with China to address the impact of stroke on patient and their caregivers. This interest has expanded to taking advantage of Peru’s national disability survey to explore the epidemiological profiles of disability in Peru. We found that approximately 1.6 million Peruvians have at least one disability, 40% of them require assistance in daily living activities and informal caregiving is very common. In addition, together with colleagues from Tanzania and U.K., including disability advocacy groups, we are working closely to understand the extent to which persons with disabilities are included in social protection systems.
Finally, together with colleagues from Brazil, U.K. and the U.S., we are investigating the association between chronic diseases and mental health, with an emphasis on depression. This is being conducted as part of the Latin America Treatment & Innovation Network in Mental Health (LATIN-MH), which is part of a wider international network of collaborators that supports regional hubs for research, capacity building and knowledge sharing.
Population level
Our experience with co-ordinating and completing large population-based epidemiological studies enabled us to move rapidly into other research design ventures such as stepped-wedge trials. Our group leads one of the projects in the hypertension programme of the Global Alliance for Chronic Diseases[15]. This project focuses on using social marketing strategies to promote and implement a low-sodium high-potassium salt substitute campaign aimed at achieving population-wide reductions in blood pressure at the community level. (ClinicalTrials.gov NCT01960972)[16].
Community level
The Centre has engaged in several community-level undertakings. For instance, we created links with youth groups through a communication programme, the “multiplicadores jóvenes” (young multipliers)[17]. In this programme, young high-school students were given the opportunity to learn basic concepts of communication and access media resources including video, photography, and radio. They then developed their own messages for health campaigns. Interestingly, they created a much different approach to health promotion, in visual terms, than expected (pic.twitter.com/HCikSzmBwy), highlighting the importance of including this community in the development of interventions.
In another community level project, we introduced marketing techniques into poor urban settlements by capitalising on community kitchens to deliver healthy diets to low-income families in Peru[18]. In slum settings, where a meal is sold for PEN 1.5 soles (USD $0.52, GBP £0.32), we introduced sales of complementary salads and fresh fruit. By challenging assumptions that poor people are not willing or not interested in eating healthy foods, this project sought to address whether accessibility to fresh products in poor communities can be improved and under what circumstances. Price, food preparation time, amenability to storage, product availability, and quality control arose as important factors. After completion of the pilot phase of this work a total of eight community kitchens have continued to prepare and offer salads and fruit options as part of their menus.
Individual clinical level: shared-decision making
In collaboration with the Mayo Clinic’s Knowledge and Evaluation Unit and Conocimiento y Evidencia (CONEVID), a group of young investigators focused on the implementation of evidence-based practice at Universidad Peruana Cayetano Heredia, CRONICAS pioneered a study of patient-centred care for patients with chronic conditions in Peru.
This team first studied the context in which clinicians and patients interact and the likelihood that clinicians will invite patients to take part in decision making[19]. We also sought to understand the context of consultations in the public and private sector and the extent to which noise, lack of privacy, interruptions by healthcare personnel, and interruptions through the clinicians’ phone impaired the ability of patients and clinicians to engage[20].
More recently, this collaborative partnership has begun to explore the notion of minimally disruptive medicine in Peru[21], which refers to the attainment of patient goals while maintaining the smallest possible healthcare footprint. This notion has important implications for healthcare delivery, which includes determining the patient’s available capacity that can be mobilised to access, use, and enact care, as well as the workload necessary to achieve patient outcomes. The patient’s capacity results from the physical and mental health, financial health, social capital, literacy, and resilience, among other factors, and permits connections to be made between social determinants of health and clinical medicine. This concept of imposing the smallest possible healthcare footprint could revolutionise the patient-centred care of individuals with chronic conditions.
Healthcare organisation
Our group, together with collaborators based in Switzerland, was asked to conduct a pilot study of a tool developed by the World Health Organization to identify barriers in accessing non-communicable disease care and medicines[22]. This tool approaches the health system for the conditions of interest at three different levels: (1) the macro-level, which includes policies, funding allocation, and pricing and distribution of medicines, related to the conditions of interest; (2) the meso-level, which is the organisation of the healthcare system including referral paths; and (3) the micro-level, which is at the point-of-care, including patients and human resources[23, 24]. The work in Peru was focused on diabetes and hypertension, and builds on the rapid assessment protocol developed for insulin access[25].
Mental health has also been part of our explorations of what works in real world settings. Working within the health system and advocating for the incorporation of mental health services into the routine practice of primary healthcare is a big step towards integrated care[26]. This route addresses the existing gap in mental health treatment caused by insufficient specialised human resources[27] and the high prevalence of comorbid mental health conditions with both infectious and chronic NCDs[28, 29]. Allillanchu, a currently ongoing project at CRONICAS, aims to integrate mental health screening practices into primary healthcare services, specifically for people with an increased risk of depression, such as pregnant women, patients with tuberculosis, diabetes, HIV/AIDS, and hypertension. By combining the training of non-specialised health providers with the use of mHealth technology, specifically a screening app and a SMS delivery system to remind and motivate patients to seek mental healthcare, we expect to achieve early detection, opportune referral, and access to treatment for patients with depression[30].
Delivering evidence-based healthcare
Evidence based clinical practice and translation of findings from clinical trials into everyday practice[31] is a pending agenda in Peru. Hypertension and stroke are two important areas where therapeutic interventions have already demonstrated efficacy, but the major unresolved challenge rests on the adoption and implementation of those strategies. In the case of hypertension, only 50% of patients are aware of their condition, and of those who are aware, only 40% adhere to treatment[32]. Stroke is a common complication from hypertension, and its presence marks a significant patient burden[33]. This is compounded by ongoing human resource deficiencies and the absence of stroke care units to provide comprehensive care and rehabilitation services. Recognizing the need to implement practical solutions, our group is working towards a school for the caregivers of stroke patients focusing on rehabilitation therapy, control of cardiovascular risk factors, recognition of the signs of stroke, and adherence to medications. This initiative is complemented by our participation in a multi-country study in the Latin American region aimed at achieving adherence to evidence-based stroke management strategies[34] within the first 48 hours of the onset of stroke and at discharge from the hospital.
CAPACITY BUILDING AND AVOIDING A SILO MENTALITY
Capacity building is a key aspect of our Centre’s development. This is achieved through a number of initiatives including supported Fellowships, hands-on engagement of students through the different aspects of research, and the attraction of PhD graduates.
Also, our group believes in the advantages of linking diverse areas of expertise as means to move forward in conducting research. Hence, it is vital that every single team member from the CRONICAS Centre, from junior to senior levels, step out of their silos and work together to maximize the returns of innovative research. For example, some of these interdisciplinary interactions include linking infectious disease and child health with NCDs, hypoxia and human adaptation to high altitude and its effects on chronic diseases, individual-environment ecosystems and human vulnerability related to climate change.
FINAL REMARKS
All the initiatives and ongoing projects described are or have been possible thanks to the confluence of common interest from international funding agencies (see Financial Disclosure for a list of all funding sources), local institutions and international collaborators in high-income countries. This confluence, primarily concentrated around capacity building, has generated, supported, and promoted a unique environment where research can flourish. The research conducted at the CRONICAS Centre of Excellence is highly collaborative and interdisciplinary. This provides a foundation to address and engage in translational research —research with strong emphasis on dissemination and implementation in real world settings— by combining mixed methods, sound study designs, and both qualitative and quantitative research questions.
The core research group is entirely funded through research grants, thus grant writing consumes a sizeable portion of our efforts, and it is key to anticipate future periods of uncertainty. A part of our strategy for growth and sustainability relies on expanding the components of our research portfolio exemplified by the flagship projects described in this manuscript. However, this is particularly challenging because as new research foci and approaches arise, we are placed in a constant search for balance and equilibrium between the quest for growth, risk aversion, and the possibility of spreading ourselves too thin. Regardless, overall the Centre is not a risk-averse organisation: it benefits from past experiences, including past mistakes, improves upon them, and challenges traditional research approaches. This ethos and environment is key to fostering innovation in research. In so doing, it contributes to the advancement of global health and reduction of health disparities, by actively bringing the unique perspective of professionals based in low- and middle-income settings.
Acknowledgments
The authors are indebted to all current and previous CRONICAS staff, trainees and students that throughout the years have contributed to making CRONICAS what it is today. We are also thankful to all participants who kindly agreed to participate to many of the studies conducted by the Centre. Special thanks to all field teams for their commitment and hard work, including Lilia Cabrera, Rosa Salirrosas, Viterbo Aybar, Sergio Mimbela, and David Danz for their leadership at each of the study sites, Marco Varela for data coordination, and José Alfredo Zavala for preparing the maps. Our special gratitude to Silvia Rodríguez, her early departure is a great loss to our Peruvian research network.
Recognition is extended to our wider list of collaborators that have contributed, in several meaningful ways, with suggestions, ideas and shared thoughts for best possible research studies. These include, in a non-exhaustive list, David Beran, Peter Busse, Shah Ebrahim, Majid Ezzati, Harold I Feldman, Luis Huicho, Homero Martínez, Julio Medina, Paulo Menezes, Miguel Pinto, Cristina Rabadán-Diehl, Manuel Ramirez-Zea, Adolfo Rubinstein, Antonio Trujillo, Alberto Vásquez, Jonathan Wells and Lijing L Yan.
Disclaimer
The views expressed in this article are those of the authors only and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the U.S. Government.
Footnotes
AUTHOR CONTRIBUTION
JJM conceived the manuscript and wrote the first draft. All authors participated in writing of manuscript, contributed to specific sections, provided important intellectual input and content, and gave their final approval of the version submitted for publication.
FINANCIAL DISCLOSURE
The establishment of the CRONICAS Centre of Excellence in Chronic Diseases at Universidad Peruana Cayetano Heredia was funded in whole with Federal funds from the United States NHLBI, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN268200900033C.
The support of several institutions, listed in alphabetical order, is credited: Alliance for Health Policy and Systems Research (HQHSR1206660), Consejo Nacional de Ciencia y Tecnología (CONCYTEC), Grand Challenges Canada (0335-04), International Development Research Center Canada (106887-001), Inter-American Institute for Global Change Research (IAI CRN3036), Medtronics Philanthropy, NHLBI (5U01HL114180, HHSN268200900028C-3-0-1), National Institute of Mental Health (1U19MH098780), UnitedHealth Foundation, Universidad Peruana Cayetano Heredia, Wellcome Trust (GR074833MA, WT093541AIA), and World Bank.
Ricardo Araya declares receiving funding from the Wellcome Trust, National Mental Health Institute, Grand Challenges Canada, and United Kingdom’s Medical Research Council. William Checkley was supported by a Pathway to Independence Award (R00HL096955) from the NHLBI. The Global Health Peru Program – UPCH was funded by Fogarty International Center (R25TW00490). Participation of Andrés G Lescano and the UPCH/NAMRU-6 Epidemiology Masters were funded by the program “Peruvian Consortium of Training in Infectious Diseases” awarded by the Fogarty International Center (2D43 TW000393). Liam Smeeth is a Senior Clinical Fellow and Hector H García a Senior Fellow in Public Health and Tropical Medicine, both funded by Wellcome Trust. The funders had no role in decision to publish, or preparation of the manuscript.
COMPETING INTERESTS
The authors declare that they have no competing interests.
Copyright statement
One author of this manuscript is an employee of the U.S. Government. This work was prepared as part of his duties. Title 17 U.S.C. 1 105 provides that ‘Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. 1 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Garcia P, Armstrong R, Zaman MH. Models of education in medicine, public health, and engineering. Science. 2014;345:1281–3. doi: 10.1126/science.1258782. [DOI] [PubMed] [Google Scholar]
- 2.Villafuerte-Galvez J, Curioso WH. Teaching global health at the frontlines. A multidisciplinary course in Peru presents basic concepts to students. PLoS Med. 2007;4:e130. doi: 10.1371/journal.pmed.0040130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noncommunicable diseases country profile 2011 - WHO Global Report. WHO; Geneva, Switzerland: 2011. [Google Scholar]
- 4.World Health Organization. Noncommunicable diseases country profiles 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 5.International Diabetes Federation. IDF Diabetes atlas. 6. Brussels: International Diabetes Federation; 2013. [Google Scholar]
- 6.PAHO-Peru. Health in Americas - 2007 Edition. Washington D.C.: PAHO; 2007. [Google Scholar]
- 7.Goldstein J, Jacoby E, del Aguila R, et al. Poverty is a predictor of non-communicable disease among adults in Peruvian cities. Prev Med. 2005;41:800–6. doi: 10.1016/j.ypmed.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Ebrahim S, Pearce N, Smeeth L, et al. Tackling non-communicable diseases in low- and middle-income countries: is the evidence from high-income countries all we need? PLoS Med. 2013;10:e1001377. doi: 10.1371/journal.pmed.1001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institutes of Health. Bethesda, MD: National Institutes of Health, US Deparment of Health & Human Services; 2012; [2014 Aug 15]. Biennial Report of Director, National Institutes of Health, Fiscal Years 2010 & 2011. updated 2012; Available from: http://report.nih.gov/biennialreport/chapter2/NIH_Postclinical_Translational_Research.html. [Google Scholar]
- 10.Caravedo MA, Painschab MS, Davila-Roman VG, et al. Lack of association between chronic exposure to biomass fuel smoke and markers of right ventricular pressure overload at high altitude. American heart journal. 2014 doi: 10.1016/j.ahj.2014.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nabel EG, Stevens S, Smith R. Combating chronic disease in developing countries. Lancet. 2009;373:2004–6. doi: 10.1016/S0140-6736(09)61074-6. [DOI] [PubMed] [Google Scholar]
- 12.UnitedHealth Group/National Heart L, Blood Institute Centres of E. A global research network for non-communicable diseases. Lancet. 2014;383:1446–7. doi: 10.1016/S0140-6736(13)61808-5. [DOI] [PubMed] [Google Scholar]
- 13.Klasen E, Miranda J, Khatry S, et al. Feasibility intervention trial of two types of improved cookstoves in three resource-limited settings: study protocol for a randomized controlled trial. Trials. 2013;14:327. doi: 10.1186/1745-6215-14-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valle GA, Poterico JA, Quispe R. Informal caregivers of patients with cerebrovascular diseases. Revista peruana de medicina experimental y salud publica. 2014;31:169–80. [PubMed] [Google Scholar]
- 15.London: Global Alliance for Chronic Diseases; 2012. [2014 Aug 15]. Project 11: Launching a salt substitute to reduce blood pressure at the population level. updated 2012; Available from: http://www.gacd.org/projects/current-projects/hypertension/project-pages/project11. [Google Scholar]
- 16.Bernabe-Ortiz A, Diez-Canseco F, Gilman RH, et al. Launching a salt substitute to reduce blood pressure at the population level: a cluster randomized stepped wedge trial in Peru. Trials. 2014;15:93. doi: 10.1186/1745-6215-15-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farchi S, Molino N, Giorgi Rossi P, et al. Defining a common set of indicators to monitor road accidents in the European Union. BMC Public Health. 2006;6:183. doi: 10.1186/1471-2458-6-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Development Research Center. IDRC; 2014. [2014 31 Jul]. Delivering Healthy Diets to Low-Income Families through Community Kitchens in Peru. updated 2014; Available from: http://www.idrc.ca/EN/Themes/Science_Policy/Pages/ProjectDetails.aspx?ProjectNumber=106887. [Google Scholar]
- 19.Zevallos-Palacios C, Quispe R, Mongilardi N, et al. Patients’ participation in clinical decision making as a strategy to protect their rights. Revista peruana de medicina experimental y salud publica. 2013;30:363–4. [PubMed] [Google Scholar]
- 20.Mongilardi N, Montori V, Riveros A, et al. Clinicians’ involvement of patients in decision making. A video based comparison of their behavior in public vs. private practice. PLoS One. 2013;8:e58085. doi: 10.1371/journal.pone.0058085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeballos-Palacios C, Morey-Vargas OL, Brito JP, et al. Shared decision making and minimal disruptive medicine in the management of chronic diseases. Revista peruana de medicina experimental y salud publica. 2014;31:111–7. [PubMed] [Google Scholar]
- 22.Beran D, Higuchi M. How to investigate access to care for chronic noncommunicable diseases in low- and middle-income countries A survey manual based on a Rapid Assessment Protocol Draft for field testing, May 2012. London: International Insulin Foundation; 2012. [Google Scholar]
- 23.Beran D, Yudkin JS, de Courten M. Access to care for patients with insulin-requiring diabetes in developing countries: case studies of Mozambique and Zambia. Diabetes Care. 2005;28:2136–40. doi: 10.2337/diacare.28.9.2136. [DOI] [PubMed] [Google Scholar]
- 24.Beran D, Yudkin JS, de Courten M. Assessing health systems for type 1 diabetes in sub-Saharan Africa: developing a ‘Rapid Assessment Protocol for Insulin Access’. BMC health services research. 2006;6:17. doi: 10.1186/1472-6963-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beran D, Silva Matos C, Yudkin JS. The Diabetes UK Mozambique Twinning Programme. Results of improvements in diabetes care in Mozambique: a reassessment 6 years later using the Rapid Assessment Protocol for Insulin Access. Diabet Med. 2010;27:855–61. doi: 10.1111/j.1464-5491.2010.03053.x. [DOI] [PubMed] [Google Scholar]
- 26.Diez-Canseco F, Ipince A, Toyama M, et al. Integration of mental health and chronic non-communicable diseases in Peru: challenges and opportunities for primary care settings. Revista peruana de medicina experimental y salud publica. 2014;31:131–6. [PubMed] [Google Scholar]
- 27.World Health Organization. Integrating mental health into primary care A global perspective. Ginebra: World Health Organization; 2008. [Google Scholar]
- 28.Gilbody S, Whitty P, Grimshaw J, et al. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. Jama. 2003;289:3145–51. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- 29.Thota AB, Sipe TA, Byard GJ, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42:525–38. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 30.Diez-Canseco F, Araya R, Ipince A, et al. figshare; 2014. [2014 Aug 15]. Allillanchu: Integration of Mental Health into Quotidian Routine Practices of Primary Health Care Service. updated 2014 Aug 6; Available from: http://figshare.com/articles/Allillanchu_Integration_of_Mental_Health_into_Quotidian_Routine_Practices_of_Primary_Health_Care_Services/1128652. [Google Scholar]
- 31.Woolf SH. The meaning of translational research and why it matters. Jama. 2008;299:211–3. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- 32.Carhuallanqui R, Diestra-Cabrera G, Tang-Herrera J, et al. Adherencia al tratamiento farmacológico en pacientes hipertensos atendidos en un hospital general. Rev Med Hered. 2010;21:197–201. [Google Scholar]
- 33.Ferri CP, Schoenborn C, Kalra L, et al. Prevalence of stroke and related burden among older people living in Latin America, India and China. J Neurol Neurosurg Psychiatry. 2011;82:1074–82. doi: 10.1136/jnnp.2010.234153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fonarow GC, Reeves MJ, Smith EE, et al. Characteristics, performance measures, and in-hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines-stroke. Circulation Cardiovascular quality and outcomes. 2010;3:291–302. doi: 10.1161/CIRCOUTCOMES.109.921858. [DOI] [PubMed] [Google Scholar]
- 35.Miranda JJ, Bernabe-Ortiz A, Smeeth L, et al. Addressing geographical variation in the progression of non-communicable diseases in Peru: the CRONICAS cohort study protocol. BMJ Open. 2012;2:e000610. doi: 10.1136/bmjopen-2011-000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.United Nations Centre for Human Settlements. Cities in a globalizing world: Global report on human settlements 2001. London; Sterling, VA: Earthscan Publications; 2001. [Google Scholar]
- 37.Batty GD, Victora CG, Lawlor DA. Establishing family-based life course studies in low- and middle-income countries. In: Lawlor DA, Mishra GD, editors. Family matters: designing, analysing and understanding family based studies in life course epidemiology. Oxford: Oxford University Press; 2009. pp. 129–50. [Google Scholar]
- 38.Miranda JJ, Gilman RH, Smeeth L. Differences in cardiovascular risk factors in rural, urban and rural-to-urban migrants in Peru. Heart. 2011;97:787–96. doi: 10.1136/hrt.2010.218537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miranda JJ, Bernabe-Ortiz A, Stanojevic S, et al. A1C as a Diagnostic Criteria for Diabetes in Low- and Middle-Income Settings: Evidence from Peru. PLoS ONE. 2011;6:e18069. doi: 10.1371/journal.pone.0018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loret de Mola C, Stanojevic S, Ruiz P, et al. The effect of rural-to-urban migration on social capital and common mental disorders: PERU MIGRANT study. Soc Psychiatry Psychiatr Epidemiol. 2012;47:967–73. doi: 10.1007/s00127-011-0404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Masterson Creber RM, Smeeth L, Gilman RH, et al. Physical activity and cardiovascular risk factors among rural and urban groups and rural-to-urban migrants in Peru: a cross-sectional study. Rev Panam Salud Publica. 2010;28:1–8. doi: 10.1590/s1020-49892010000700001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bernabe-Ortiz A, Gilman RH, Smeeth L, et al. Migration Surrogates and Their Association With Obesity Among Within-Country Migrants. Obesity (Silver Spring) 2010;18:2199–203. doi: 10.1038/oby.2010.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lerner AG, Bernabe-Ortiz A, Gilman RH, et al. The “rule of halves” does not apply in Peru: awareness, treatment, and control of hypertension and diabetes in rural, urban, and rural-to-urban migrants. Critical pathways in cardiology. 2013;12:53–8. doi: 10.1097/HPC.0b013e318285ef60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Danaei G, Finucane MM, Lin JK, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet. 2011;377:568–77. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 45.Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 46.Miranda JJ, Wells JC, Smeeth L. Transitions in context: findings related to rural-to-urban migration and chronic non-communicable diseases in Peru. Revista peruana de medicina experimental y salud publica. 2012;29:366–72. doi: 10.1590/s1726-46342012000300012. [DOI] [PubMed] [Google Scholar]
- 47.Daar AS, Singer PA, Persad DL, et al. Grand challenges in chronic non-communicable diseases. Nature. 2007;450:494–6. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 48.Pollard SL, Williams DL, Breysse PN, et al. A cross-sectional study of determinants of indoor environmental exposures in households with and without chronic exposure to biomass fuel smoke. Environmental health : a global access science source. 2014;13:21. doi: 10.1186/1476-069X-13-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Torres-Duque C, Maldonado D, Perez-Padilla R, et al. Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc. 2008;5:577–90. doi: 10.1513/pats.200707-100RP. [DOI] [PubMed] [Google Scholar]
- 50.Painschab MS, Davila-Roman VG, Gilman RH, et al. Chronic exposure to biomass fuel is associated with increased carotid artery intima-media thickness and a higher prevalence of atherosclerotic plaque. Heart. 2013;99:984–91. doi: 10.1136/heartjnl-2012-303440. [DOI] [PMC free article] [PubMed] [Google Scholar]


