Abstract
Background
Cardiovascular disease (CVD) is on the rise in low- and middle-income countries (LMIC) and is proving difficult to combat due to the emphasis on improving outcomes in maternal and child health and infectious diseases, against a backdrop of severe human resource and infrastructure constraints.
Effective task-sharing from physicians or nurses to community health workers (CHWs) to conduct population-based screening for persons at risk, has the potential to mitigate the impact of CVD on vulnerable populations. CHWs in Bangladesh, Guatemala, Mexico, and South Africa were trained to conduct non-invasive population-based screening for persons at high risk for CVD.
Objective (s)
The objectives of this study were to quantitatively assess the performance of CHWs during training and to qualitatively capture their training and fieldwork experiences while conducting non-invasive screening for cardiovascular disease (CVD) risk in their communities.
Methods
Written tests were used to assess CHWs’ acquisition of content knowledge during training, and focus group discussions conducted to capture their training and fieldwork experiences.
Results
Training was effective at increasing the CHWs’ content knowledge of cardiovascular disease (CVD) and this knowledge was largely retained up to six months after the completion of field work. Common themes which need to be addressed when designing task sharing with CHWs in chronic diseases are identified, including language, respect, and compensation. The importance of having intimate knowledge of the community receiving services from design to implementation is underscored.
Conclusions
Effective training for screening for CVD in community settings should have a strong didactic core that is supplemented with culture-specific adaptations in the delivery of instruction. The incorporation of expert and intimate knowledge of the communities themselves is critical, from the design to implementation phases of training. Challenges such as role definition, defining career paths, and providing adequate remuneration, must be addressed.
Keywords: Community health workers, training, evaluation, mixed methods, intervention, cardiovascular disease
INTRODUCTION
BACKGROUND
Globally, non-communicable diseases (NCD) account for 60% of mortality and 80% of these deaths occur in low- and middle-income countries (LMIC). [1] Cardiovascular disease (CVD) is a major contributor to the increasing burden of NCDs in these settings and the high rates of mortality due to cardiovascular disease events amongst wage earners in their peak income years (ages 35 – 64) significantly impacts the economies of these countries.[2, 3] Some of the primary risk factors for CVD include hypertension (high blood pressure)1, overweight (body mass index ranges from 25.0 – 29.9kg/m2) 2 or obesity (body mass index ≥ 30 kg/m2), and tobacco consumption. These risk factors affect CVD-related morbidity and mortality, which can be improved by early detection of those who are at risk, or have undiagnosed disease.[4–7]
Like many LMIC, Bangladesh, Guatemala, Mexico, and South Africa are all experiencing increasing rates of CVD as part of the shift in disease burden due to the epidemiologic transition. [3] CVD mortality in these countries account for 18–24% of overall mortality (Guatemala, Mexico, South Africa) and rates of hypertension, a primary risk factor for CVD, are also very high. [5–9]
In addition to the burden of CVD in these four countries, there is also a severe shortage of formally trained health professionals, limiting effective screening and appropriate management of persons at high risk. [1, 10–12] Effective task-sharing has the potential to offset the burden of CVD by shifting screening functions from health professionals to health workers without traditional professional training, e.g. community health workers (CHWs).
A review of the impact of CHWs in primary health care concluded that there was insufficient evidence to assess the most effective training and intervention strategies in almost all areas of health care. [13] The review also noted that the evidence for the effectiveness of using CHWs for task-sharing in intervention trials is heterogeneous in part due to lack of qualitative inquiries as part of the study design. A second review of studies that did include qualitative assessments in intervention trials highlighted that the qualitative focus was largely confined to capturing trial participants’ input, but not that of CHWs. [14] There is very little assessment of the impact of CHWs’ training experiences, job functions, or interactions with health clinic staff and trained health professionals, on the effectiveness of interventions. [15] This is largely because the traditional quantitative measures used to assess the impact of CHWs in many programs and clinical trials, e.g. number of clients seen daily or changes in biomarker levels, do not systematically identify and articulate the issues that may impact the CHWs’ ability to effectively interact and function within the existing health care systems.
Currently there are no formal, standard assessments, or defined metrics for measuring qualitative outcomes related to CHW training and fieldwork performance. There is some evidence that CHWs’ personal beliefs about health, their working conditions, their interactions with health professionals, and perceptions about CHWs by both community members and policy makers, all directly impact the effectiveness of programs and policies that utilize CHWs for task-sharing. [16–19]
The evidence for the effectiveness of training provided to CHWs is sparse. There are some individual and regional training programs that are effective and plans are underway to develop training courses that will be accredited by the government. [20–23]
This study was conducted in communities in Bangladesh (rural), Guatemala (rural), Mexico (urban and rural), and South Africa (peri-urban) – all countries in the National, Heart, Lung and Blood Institute (NHLBI)/United Health Group Centers of Excellence (CoE) for chronic disease global network.
The objectives of this study was to use a mixed methods approach to assess the performance of CHWs during training (quantitative – all four sites), and their training and fieldwork experiences (qualitative – all sites except Bangladesh, which elected not to participate in this component of the study) while conducting non-invasive screening for CVD risk in their communities. The results enhance our understanding of the effectiveness of training and also provide further insight into how CHW interactions with both their communities and clinic staff impact the overall effectiveness of the population-based screening program.
METHODS
Both quantitative and qualitative methods were used to assess the objectives of the study. Content knowledge acquisition was assessed using pre-training, post-training, and post-field work testing. CHWs’ training and fieldwork experiences were captured in focus group discussions.
A NOTE ABOUT TERMINOLOGY
The use of terminology to describe health workers is an important source of debate in the published literature. For health workers that do not have traditional, formal training such as physicians or nurses, a variety of labels are in use, e.g. community health worker (CHW), lay health worker, health promoters, etc. In this paper we use the term CHW without seeking to assign any a priori value to the work they perform, or to their status in their respective communities and health systems. Rather, it is a choice made in the interest of simplicity and ease of access to the reader.
IMPLEMENTATION OF THE PROTOCOL FOR SCREENING
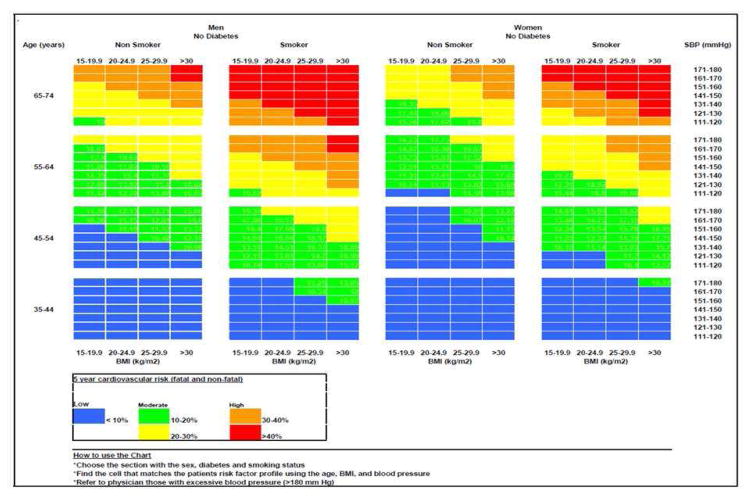
The study population for screening was drawn from the communities served by the local health centers, with residents aged 35 to 74 years considered eligible for screening and referral. Persons reporting a prior history of treatment for hypertension, diabetes, or known CVD (stroke, myocardial infarction, or angina) were ineligible for screening. Residents with a measured systolic blood pressure (SBP) > 180 mmHg were deemed clinically urgent cases and their clinical symptoms were evaluated using a simple questionnaire. They were provided with an urgent referral letter for immediate evaluation by a health professional at the closest health center and were ineligible for the CVD risk assessment arm but eligible for the referral arm. A CVD risk score was calculated for all remaining participants using the risk scoring tool (Figure 1). Persons whose risk score was greater than 20% were provided with non-urgent referral letters to see a health professional within two weeks of screening. Each CHW was expected to screen at least 100 people over a four to six week period at community screenings or in members’ homes.
Figure 1.
Risk Scoring Chart Used by CHWs to Obtain CVD Risk Scores
Assigned health professionals (registered nurse or physician) at each site calculated a second risk CVD risk score using de-identified data and were blinded to the CHWs’ risk scores and BMI calculations. Persons with discrepant CHW and health professional scores warranting a change in referral recommendations were contacted by the primary investigator about appropriate next steps. The primary endpoint was the level of direct agreement between the risk scores assigned by the CHW and those assigned by the health professional. The mean level of direct agreement across sites was found to be 96.8% and the statistical methods are described in detail in a separate publication currently under review for publication.
CHW TRAINEE SELECTION
Each site recruited at least eight to fifteen CHWs to participate in the training, based on usual site-specific norms for required levels of education and language competency, working with the local non-governmental organizations (NGOs) and the Ministry of Health (Mexico). CHWs had to reside in the community where the screenings were conducted and had to be fluent in that community’s dominant language, as well as the country’s official language for training, if the two differed. CHW profiles for each site are described in Table 1.
Table 1.
Summary of Characteristics of the Four Intervention Sites.
| Bangladesh (Matlab) | Guatemala (Santiago Atitlan) | Mexico (Hermosillo) | South Africa (Khayelitsha) | |
|---|---|---|---|---|
| Community Characteristics |
|
|
|
|
| Typical CHW Profile and Utilization | ||||
|
|
|
|
|
| CHW Employment, Supervision, and Career Paths | ||||
|
|
|
|
|
TRAINING
Individual site trainings were conducted during 1 to 2-week periods over four months in 2012. CHWs learned to measure and calculate mean blood pressure (systolic/SBP and diastolic/DBP) taken over three readings at five-minute intervals, using an automated Omron ® blood pressure. They learned to measure height using an adjustable height stick, weight using a digital scale, and to calculate body mass index (BMI) with the aid of a calculator. Finally, they learned to obtain a 5-year CVD risk score for experiencing an adverse cardiovascular event from the data they collected using the pre-printed risk chart (Figure 1).They used the variables necessary for determining a risk score (gender, age, smoking status, BMI, average SBP) to locate the individual cell where all of the variables intersect. They noted the color of the selected cell and selected the corresponding risk range using the legend on the bottom of the chart.
A training manual covering content knowledge about CVD and its risk factors was developed using two existing manuals for educating and training lay health workers which are already in use in the United States, Central America, and South Africa. Su Corazon, su Vida was developed in the United States (validation included focus group discussion with members of the community of Mixco, Guatemala in 2007 - unpublished data) and a manual developed at the University of the Western Cape School of Public Health, South Africa to train CHWs to provide health promotion activities for chronic disease lifestyles. [22, 24] All study materials were translated from English to Bangla (Bangladesh) and Spanish (Guatemala and Mexico). Content knowledge was supplemented with interactive components/activities designed and customized by trainers at individual sites. A workshop format that combined lectures and interactive lessons was used and instruction delivered in multiple languages, as necessary. Training teams were composed of health professionals (physicians, nurses, nutritionists, and other public health professionals).
Trainees learned to determine eligibility by administering a self-reported health risk factor questionnaire. Ethical conduct in all study activities was also taught, including maintaining confidentiality through the recruitment and screening processes, and assisting in the explanation and completion of informed consent forms.
At the conclusion of training, all qualified CHWs were deployed to conduct community screenings over 1–2 weeks. During this run-in period, site coordinators provided intensive, in-person supervision, via phone or using written assessments to address any challenges encountered during implementation. CHWs deemed unfit to perform effectively in the field during this run-in period were not allowed to continue with field work. For the rest of the trial, CHWs continued to be supervised by study coordinators who provided weekly assessments of performance and addressed any challenges that arose.
EVALUATION OF CHW TRAINEES
Quantitative Assessments of CVD Content Knowledge and Practical Skills
Immediately prior to, and after, training, a test covering content knowledge about CVD and its risk factors was administered. The post-training test included additional practical components testing skills for obtaining anthropomorphic measures and blood pressure, and the use of the risk tool to calculate a CVD risk score. Trainees who successfully passed the post-training assessment with a minimum score of 60% in content knowledge, full competency in measuring blood pressure, height, and weight, and scored 100% on the CVD risk score calculations were deemed fit to conduct field work. Trainees who failed to perform effectively during the run-in period were withdrawn from field work. Three to six months after the completion of field work, a second post-training test was re-administered, covering CVD content knowledge and use of the risk tool.
QUALITATIVE ASSESSMENT OF CHWs’ EXPERIENCES (CONDUCTED AT ALL SITES EXCEPT BANGLADESH)
Trainers’ and Supervisors’ Assessments of Training and Field Work
Trainers and supervisors kept detailed notes about training and field work, for later evaluation of CHWs’ performances.
Development of CHW Focus Group Guide
Prior to the commencement of training for the study, a focus group was held with CHWs employed in infectious disease management in Khayelitsha, by a NGO not involved in this study, to gain an understanding of attitudes in various domains reported in published evidence. Data from this focus group was used to develop an interview guide of seven questions for use in post-field work focus groups with CHWs at participating sites.
Data collection
After the completion of fieldwork, CHWs were invited to participate in focus groups to capture their training and the fieldwork experiences. Participants signed consent forms indicating their agreement to participate. All focus group discussions were recorded using digital audio recorders. Transcription of the recordings was completed and coded at individual sites. De-identified transcripts of all audio sessions were provided to investigators for pooled analysis. To further preserve confidentiality, all audio recordings were stored securely at individual sites in accordance with institutional policies.
ANALYSES
Descriptive summary statistics and analysis of variance (ANOVA) procedures for all quantitative analyses were conducted using statistical analysis software SAS ® 9.3 and Microsoft Excel® 2010. Qualitative analyses were conducted using a combination of Atlas Software ® or NVivo 9® software, and manual coding for content analysis. [25, 26] The software packages were used to efficiently identify themes in the transcript data using codes and keywords identified by researchers as pertinent to the research problem being studied. Additionally, manual coding of transcript data was undertaken by reading and reviewing transcripts in their entirety by investigators for at least two times in order to get a general sense of the data. Responses were then grouped into themes. Results from the software analyses and the manual analyses were combined for a comprehensive assessment of the data. Selected quotes from participants are included to illustrate themes without identifiers to preserve the anonymity of respondents. Field notes from supervisors and study coordinators were manually reviewed for thematic content.
In order to encourage candid feedback and promote trustworthiness of the study, the focus group facilitators were not part of the study. At the end of the discussions information was summarised for the participants to ensure that the summary was a true reflection of what was discussed.
ETHICS
All clinical and study staff completed ethics courses through the Collaborative Institutional Training Initiative (CITI). The study protocol was approved by the NHLBI as well as the respective institutional or ethics review boards in each of the four participating country sites.
RESULTS
COUNTRY AND COMMUNITY HEALTH WORKER CHARACTERISTICS
A summary describing the four intervention sites, along with typical profiles for the 64 CHW trainees is provided in Table 1. Eighty-four percent of the trainees were women. All of the 64 trainees were tested immediately prior to the start of training but only 49 were tested at the end of training as 15/23 of Guatemala’s trainees were withdrawn from the project prior to completion of training and re-assigned due to other commitments with the local health authority. Forty-two CHWs (83% women) were deemed fit to conduct field work after the run-in period: 15 in Bangladesh (3 men), 8 (1 man) in Guatemala, 9 (3 men) in Mexico and 10 (all women) in South Africa (Table 2).
Table 2.
Summary of Community Health Workers Available for Training and Field Work – All Sites
| Bangladesh | Guatemala | Mexico | South Africa | Trial-Wide | |
|---|---|---|---|---|---|
| Number of trainees starting training: | 15 | 23 | 11 | 15 | 64 |
| Number of trainees with pre-training scores: | 15 | 23 | 11 | 15 | 64 |
| Number of trainees with post-training scores: | 15 | 8 | 11 | 15 | 49 |
| Number of trainees with post-field work scores: | 15 | 8 | 9 | 10 | 42 |
CONTENT KNOWLEDGE TEST OUTCOMES
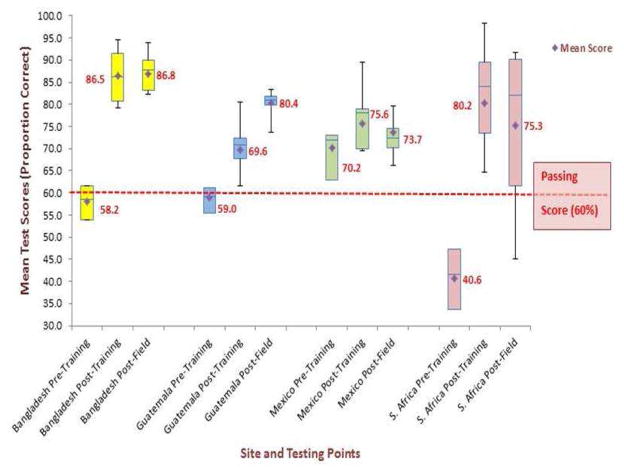
The mean scores across all sites increased from pre-training to post-training, with increases ranging from 7% in Mexico, to 39% in South Africa (Figure 2). Between the completion of training and field work, Bangladesh showed no difference in mean content knowledge levels, Guatemala experienced a mean increase of 11%, and both Mexico (−2%) and South Africa (−5%) saw decreases in mean scores. Across all sites, the mean changes in content knowledge between the end of training and the end of field work, remained above the minimum passing threshold of 60%.
Figure 2.
Summary of Mean Content Knowledge Test Outcomes - All Sites
CHWs TRAINING EXPERIENCES
A total of 3 focus groups were conducted. The main themes and the factors underlying the themes for both training and fieldwork are summarized in Figure 3. Please note that any differences in the color, shapes, and text sizes in this figure are for readability only and do not indicate any particular significance.
Figure 3. Main Themes from CHWs Field Work Experiences and Influencing Factors*.

*Please note that color, shape or text size do not assign any significance to individual components
SUMMARY OF MAIN THEMES EMERGING FROM TRAINING EXPERIENCES
Length of training and format
There was overall agreement by both trainees and trainers that training time should be extended from the one-week design to at least two weeks. This was borne out by the experience in South Africa where only 3/15 trainees scored above the passing threshold of 60% during the post-training assessment at the end of the week-long training. After discussions with the trainees, the trainers extended the training for an additional week, and in the second post-training assessment, 11/15 trainees scored above the required threshold. CHWs also expressed a desire for a less traditional format of instruction and that the site-specific innovations were valuable enhancements to training.
“It was a lot of information for four days and in such a traditional format.” – [CHW, Mexico]
Similarly, CHWs in Guatemala reported that the training was “a bit hard” at the beginning and felt that, while training covered a lot of topics they needed to learn about, it should probably have covered “nerve issues” (i.e. mood disorders). CHWs felt that the workshop format with interactive sessions beyond didactic instruction through lectures, enhanced learning.
“The trainers who participated included the materials we provided for them in the manual, but the ones who did the best job were those who provided additional material and data on the problems they were discussing.” – [Supervisor, Mexico]
This is consistent with the experience in South Africa where the workshop format was also adopted and the additional second week of training was heavily skewed toward interactive classroom exercises, role-playing, and opportunistic learning examples devised by the trainers.
Language Challenges
Trainers at all four sites noted that calculation of body mass index (BMI) was challenging, both for the trainers to teach, and also for the trainees to learn. This was largely because the manual was written in a language different from the teaching language (South Africa, Guatemala) and a lower level of numeracy. The use of a calculator mitigated these challenges to some extent. At some sites ongoing instruction and improvement in calculating BMI continued into the 1–2 week run-in period immediately following training.
“The thing that seemed to be most difficult, even though they had calculators, was to do the BMI calculation. They had to work on that multiple times and we had to be careful to supervise this well.” – [Supervisor, Mexico]
The language issue also extended to testing; trainers expressed disappointment in the mean change of content knowledge test scores from baseline to post-training, suggesting that poor studying skills might be to blame.
“Although they had the complete information, it was in their materials, some of them used nonspecific information to answer the questions. It seemed as if they had not even read the materials we had given them.” – [Supervisor, Mexico]
Adjustments such as assigning homework or increasing classroom exercises had to be made during training, in order to improve the trainees’ performance in this area.
Another perspective that was offered was that CHWs were not highly motivated to do well in their duties as a rule and that this impacted their performance during the tests.
“Some of them did not do that well on the pre- and post-tests, they did not seem to be used to that type of training and were too confident that they could do all right. I believe that it has to do with the demands, or lack of demands, that the Ministry of Health makes on them. For example, as long as they fulfill their goals, ‘their numbers’, then they are ok.” – [Supervisor, Mexico]
In contrast, CHWs at all sites expressed the belief that performance was impacted by their lack of ease with the language of the written tests (English, Spanish), as opposed to the combined languages of instruction (English and isiXhosa, Spanish and Tz’utujil). They suggested that verbal or practical assessments of their abilities by supervisors would offer a more accurate assessment of their acquisition of new knowledge.
“If you asked me [verbally] I know the answer, but if you ask me to write it down, I get it wrong.” - [CHW, Mexico]
Acquisition of knowledge and empowerment
Overall, CHWs expressed great excitement and appreciation for the new skills acquired during training, as they are not usually taught in depth about any given topic.
“It was a great experience, it was an opportunity provided to us by this institution [redacted] because no one else has taught us these things. Although we work with the nurses, they don’t teach us that.” - [CHW, South Africa]
“We learned a lot. People find us in the street and they ask us. Now we know how to explain, before we didn’t. Now I feel very satisfied that I can explain.” - [CHW, Guatemala]
Innovative aspects of the training, such as providing nutritious meals to trainees during the training, as a means to reinforce the impact of nutrition on NCD risk, led to the CHWs feeling empowered to change their own behaviors, as well as convincing community members to change their behaviors. The CHWs expressed positive feelings about this to their trainers.
“For most of the CHW, the material we used in the training was new; they did not have information on NCD and were not familiar with the tools we used.....Some of the CHW said they had not understood the implications of good nutrition, others had never eaten nutritious meals like we provided during the four days of training.” - [Supervisor, Mexico]
Gender Sensitivity and Recruitment
Across all sites, CHWs found that sensitivity to specific gender-related issues was critical to obtaining good anthropometric data and that community members’ discomfort in this area negatively impacted CHW efforts. In all the study sites, both men and women expressed levels of discomfort with removing outer clothing to facilitate blood pressure measurement. Here the CHWs’ expert knowledge of their communities’ norms and standards of behavior allowed them to navigate potentially difficult situations. The necessity of this community expertise was readily acknowledged by supervisors in South Africa.
“..the community health workers…are a great help because it’s difficult for us to go out and see what’s happening out there…I feel they play a vital role in helping us to make a decision with regard to treatment…a good community health…must know the community. People must be comfortable with them, they must be part of the community, they must be known within the area and…they must be observant….” – [Supervisor, South Africa]
In Guatemala, screenings that took place in convergence centers proved difficult because of the lack of private spaces to conduct screenings.
“We had difficulties with that place…for example if a woman…needed to remove her – güipil – (traditional clothing)…we didn’t have a private place....” – [CHW, Guatemala]
In Mexico CHWs noted that men were more resistant to participating than women.
Relationships with Communities
Overall, CHWs expressed recognition that their communities appreciated their work, relied on them and trusted them more compared to staff at the health clinics. This recognition provided a measure of satisfaction and motivation for CHWs.
“…when you … go out into the community, you communicate with the people in the community…When they see us, they see people who bring hope and people who smile at them. Then when they see us they know that even if a person is not well, s/he will get well because of the CHW’s presence. So, they (community) choose us rather…They easily confide in us with their issues.” - [CHW, South Africa]
“We went to Panaj to visit a person. We took her blood pressure, height, and weight. She was an obese person,….We talked to her and told her that if she normally eats eight tortillas to eat five tortillas or if she drank sodas, to quit that and to drink water…Two months later she went to the Convergence Center and told me that she had lost four pounds and was grateful that I visited (her home).” – [CHW, Guatemala]
At the same time, some CHWs were also frustrated by a lack of interest by community members in their own health.
“…hitting a brick wall…we do not have a culture of health promotion and prevention.” – [CHW, Mexico]
Safety concerns
Safety was a major concern in South Africa. Even though these CHWs work and live in the communities where they conducted screening and are respected by many, they are often working in areas with high rates of crime. They often wear uniforms that make them stand out and this makes them an easy target for theft. If they are known to be responsible for delivering medication to patients in their homes, or if they are provided with cell phones to communicate with supervisors, they are targeted.
“…Community health workers … they have that passion to go and help in spite of the negative actions… posed by the community members to them.” - [Supervisor, South Africa]
Work load, compensation and respect
These three features of the CHWs’ work experiences are intimately tied together. Overall, CHWs feel that their workload is disproportionate to the compensation that they receive.
Additionally, the range of tasks they are expected to perform in theory seriously underestimates the actual range of tasks that they have to perform in practice when delivering services. They also believe that the time allotted to them for these tasks by their supervisors severely underestimate the time it takes to achieve their goals.
“When we work in the community we must pay attention to many aspects, we do not work only on what we have been employed for, we look, perhaps look at a child’s condition if there is a sick child in the house, a bed-ridden person and other people use drugs in the same house, so we have to face all that in the same house and you discover that the work load is too much and you have too little… We need time and the money to be increased because we have too much work load and little time and sometimes there is an invalid who has to be bathed, dressed, prepared so that s/he is ‘right’...” - [CHW, South Africa]
Supervision of CHWs
Supervision of CHWs during field work proved to be challenging, both for the CHWs as well as their supervisors. Some CHWs felt unsupported by study staff and appeared to get caught in miscommunication between the official supporters of the study and supervisors who were not participating in the study.
DISCUSSION
There were two main findings in our study: first, training increases the CHWs’ content knowledge of CVD and this knowledge is largely retained up to six months after the completion of field work. Second, common themes across sites related to the CHW’s experiences of training and field work were identified using qualitative inquiry. The identified themes largely overlap with challenges noted in the experiences of task sharing with CHWs in the areas of communicable diseases. CHWs can be effectively trained to conduct non-invasive screening for CVD risk in their communities and their experiences of both training and field work can inform the design and integration of programs utilizing effective task sharing in chronic diseases.
The increase and retention of content knowledge provides evidence that the training as designed was effective. This means that training can be effectively implemented over a short period of time with CHWs who have low levels of education and little to no CVD knowledge. Further, the retention of knowledge beyond the conclusion of the field work indicates that retraining may not be necessary within 6 months of the original training. CHWs also reported unhappiness with the testing modality (written exams) and felt it did not accurately reflect their understanding. Using alternate methods of assessment such as the simulated client method might prove to be a useful alternative, as its effectiveness has already been demonstrated with other health care workers. [28, 29] The qualitative identification of common themes such as language issues, respect, compensation, trust, work load, supervision, etc. underscore that there is a core set of issues that need to be addressed when designing task sharing with CHWs in chronic diseases, across diverse settings.
The importance of having intimate knowledge of, as well as relationships with, the community receiving services is highlighted in the findings. [30, 31] For example, language – both as the mode of instruction and the predominant mode of communication for a given community – was a key element in the training experience of CHWs. Intimate levels of knowledge about the communities allows for customizing the effective delivery of training through site-specific adjustments by incorporating appropriate cultural norms, such as the supplementation of training with cooking lessons in Mexico. Similarly, in Guatemala and South Africa the languages of official instruction materials (Spanish, English) were consistently supplemented with parallel explanations in the community’s dominant languages (Tz’utujil, isiXhosa). The trainers’ intimate knowledge of the communities and fluency in the dominant spoken languages also allowed for effective role playing exercises to augment written scripts, consistent with the evidence available for training fidelity. [32] Inadequate remuneration and a lack of clear career paths are two of the stressors that are consistently noted as the most critical challenges by CHWs, especially as it impacts retention of trained CHWs. [33] Retention of trained and skilled CHWs are critical to scaling up efforts for successful interventions. It is critically important to establish clear career paths for CHWs as none currently exist and also to match remuneration levels with work load. [34] The lack of progressive career options and insufficient income directly affects the kind of persons who become CHWs.
As with most pilot projects, a limitation of this study was the limited ability to investigate the impact of potential confounders of performance during training and field work, e.g. individual educational levels, due to the relatively small number of CHWs trained. Even though our analysis of variance (ANOVA) for the changes in mean testing scores did indicate some statistically significant differences in the mean test scores between some sites at the post-field work testing point, it is not reported here due to this small numbers problem. The project-specific employment of the CHWs also precluded retesting of novel skills acquired during training, especially those related to obtaining anthropomorphic measurements, e.g. measuring blood pressure. Reassessment of these skills could potentially further inform the need for refresher training but CHWs were not allowed to continue to use these skills after the completion of field work so reassessment would not have yielded reliable comparisons. Finally, the lack of formal, universal tools available to effectively evaluate CHWs’ performance and experiences of training limits the extent to which our results can be generalized beyond these four settings. Despite these limitations, our results clearly demonstrate that training lay health workers to conduct non-invasive screening for CVD in their communities can be effectively achieved in a short period of time, with low levels of resources. Further, the results argue for the creation of a core curriculum that can potentially be extended to cover common risk factors for not only CVD but other chronic diseases, which can be customized to individual cultural contexts.
Further exploration is needed to determine how this specific training curriculum and testing format can be effectively incorporated into more comprehensive programs in primary care service delivery which target primary prevention of chronic diseases in community settings using task sharing with CHWs. The development and formalization of appropriate quantitative and qualitative metrics to assess CHWs’ performance and effectiveness in such screening and prevention efforts also bears further investigation on a larger scale.
Overall our results demonstrate that CHWs can be effectively trained to conduct non-invasive screening for CVD in the communities where they reside and that new knowledge acquired during training persists for up to six months after the completion of screening. The success of the training is dependent on the incorporation of expert and intimate knowledge of the communities themselves, both in the design and implementation phases of training.
HIGHLIGHTS.
We investigated the training and field work experiences of CHWs.
We identified key issues that are important to CHWs for training and field work.
We found that community knowledge and relationships are critical.
Training must cover core competencies and be customized to individual settings.
Acknowledgments
Funding: This project has been funded in part with Federal funds from the United States National Heart, Lung and Blood Institute, National Institutes of Health, Department of Health and Human Services under Contract Number HHSN268200900030C. The Center for Health Promotion in Northern Mexico also received funding from the UnitedHealth Chronic Disease Initiative. The funding sources played no role in the study design, data collection, data analysis and interpretation, or writing of the report. The funding source contractually required review and approval of the manuscript prior to submission for publication and no changes were requested.
The authors wish to thank Tracey Koehlmoos and Abdul Wazed (Bangladesh), Elsa Cornejo and Yanira Valle (Mexico) for their assistance with training and in supervising the field work and Lungiswa Tsolekile (South Africa) for assistance with the focus group discussions and training.
Footnotes
Definitions for hypertension vary based on regional guidelines but for this project we considered persons with a systolic blood pressure greater than 140 mmHg to have high blood pressure.
The definitions of the Centers for Disease Control and Prevention was used here (http://www.cdc.gov/obesity/adult/defining.html
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Shafika Abrahams-Gessel, Email: Shafika_Abrahams-Gessel@Harvard.Edu, Center for Health Decision Science, Harvard School of Public Health, 718 Huntington Avenue, Boston, MA 02115, USA.
Catalina A. Denman, Email: cdenman@colson.edu.mx, Centro de Estudios en Salud y Sociedad, El Colegio de Sonora, Avenida Obregón 54, Colonia Centro, Hermosillo, Sonora, México 83000.
Carlos Mendoza Montano, Email: cmendoza@incap.int, Institute of Nutrition of Central America and Panama (INCAP), Calzada Roosevelt 6-25 Zona 11, Apartado Postal 1188, Ciudad de Guatemala, Guatemala.
Thomas A. Gaziano, Email: TGaziano@Partners.Org, Division of Cardiovascular Medicine, Brigham & Women’s Hospital, 75 Francis Street, Boston MA, 02115, USA.
Naomi Levitt, Email: naomi.levitt@uct.ac.za, Chronic Diseases Initiative for Africa, J 47/86, Old Groote Schuur Building, Groote Schuur Hospital, Observatory, 7925. Division of Endocrinology and Diabetes, Department of Medicine, University of Cape Town, South Africa.
Alvaro Rivera-Andrade, Email: arivera@incap.int, Institute of Nutrition of Central America and Panama (INCAP), Calzada Roosevelt 6-25 Zona 11, Apartado Postal 1188, Ciudad de Guatemala, Guatemala.
Diana Munguía Carrasco, Email: dmunguia@colson.edu.mx, Centro de Estudios en Salud y Sociedad, El Colegio de Sonora, Avenida Obregón 54, Colonia Centro, Hermosillo, Sonora, México 83000.
Jabu Zulu, Email: jabuvictoria@gmail.com, School of Public Health, c/o Dr. Thandi Puoane, University of the Western Cape, Private Bag X17, Bellville 7535, Republic of South Africa.
Masuma Akter Khanam, Email: masuma@icddrb.org, Centre for Control of Chronic Diseases in Bangladesh, icddrb, Mohakali, Dhaka-1212, Bangladesh. Centre for Clinical Epidemiology and Biostatistics, School of Medicine and Public Health, Faculty of Health and Medicine, The University of Newcastle, Callaghan, NSW 2308, Australia.
Thandi Puoane, Email: tpuoane@uwc.ac.za, School of Public Health, University of the Western Cape, Private Bag X17, Bellville 7535, Republic of South Africa.
References
- 1.WHO. 2008–2013 Action plan for the prevention and control of non-communicable diseases. World Health Organization; Geneva, Switzerland: 2008. [Google Scholar]
- 2.Leeder S, Raymond S, Greenberg H, Liu H, Esson K. A race against time: the challenge of cardiovascular disease in developing countries. New York: Trustees of Columbia University; 2004. [Google Scholar]
- 3.Yusuf S, Reddy S, Ôunpuu S, Anand S. Global Burden of Cardiovascular Diseases: Part I: General Considerations, the Epidemiologic Transition, Risk Factors, and Impact of Urbanization. Circulation. 2001–2001 Nov 27;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 4.M. C. WHO; W. H. Organization, editor. Cardiovascular Diseases: Fact Sheet Number 317. Geneva, Switzerland: 2013. Update. [Google Scholar]
- 5.W. H. O. (WHO) Noncommunicable Diseases Country Profile [Online] Available: http://www.who.int/nmh/countries/en/#S.
- 6.Ikeda Nayu, Sapienza David, Guerrero Ramiro, Aekplakorn Wichai, Naghavi Mohsen, Mokdad Ali H, Lozano Rafael, Murray CJ, Lim SS. Control of hypertension with medication: a comparative analysis of national surveys in 20 countries. World Health Bulletin. 2014 Jan;92:10–19C. doi: 10.2471/BLT.13.121954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karar Z, Alam N, Streatfield P. Epidemiological transition in rural Bangladesh, 1986–2006. Glob Health Action. 2009;2:1–9. doi: 10.3402/gha.v2i0.1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.P. A. H. O. (PAHO) Central America Diabetes Initiative (CAMDI): survey of diabetes, hypertension, and chronic disease risk factors. Villa Nueva, Guatemala 2006. Washington, D.C: 2007. [Google Scholar]
- 9.H. S. Trust. Annual Health Report: Chapter 17. 2012/2013. [Google Scholar]
- 10.WHO. Preventing chronic diseases: a vital investment. World Health Organization; Geneva, Switzerland: 2005. [Google Scholar]
- 11.Anyangwe SCE, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Intl J Environ Res and Public Health. 2007;4:93. doi: 10.3390/ijerph2007040002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO; G. H. O. D. Repository, editor. Human Resources. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 13.Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, van Wyk B, Bosch-Capblanch X, Patrick M. Lay health workers in primary and community health care. Cochrane database of systematic reviews (Online) 2005:CD004015. doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Glenton C, Lewin S, Scheel IB. Still too little qualitative research to shed light on results from reviews of effectiveness trials: A case study of a Cochrane review on the use of lay health workers. Implementation science: IS. 2011;6:53. doi: 10.1186/1748-5908-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, van Wyk B, Bosch-Capblanch X, Patrick M. Lay health workers in primary and community health care. Cochrane database of systematic reviews (Online) 2005 doi: 10.1002/14651858.CD004015.pub2. 2009. [DOI] [PubMed] [Google Scholar]
- 16.Heunis JC, Wouters E, Norton WE, Engelbrecht MC, Kigozi NG, Sharma A, Ragin C. Patient- and delivery-level factors related to acceptance of HIV counseling and testing services among tuberculosis patients in South Africa: a qualitative study with community health workers and program managers. Implementation science: IS. 2011;6:27. doi: 10.1186/1748-5908-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hermann K, Van Damme W, Pariyo GW, Schouten E, Assefa Y, Cirera A, Massavon W. Community health workers for ART in sub-Saharan Africa: learning from experience–capitalizing on new opportunities. Hum Resour Health. 2009;7:31. doi: 10.1186/1478-4491-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mwai GW, Mburu G, Torpey K, Frost P, Ford N, Seeley J. Role and outcomes of community health workers in HIV care in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16:18586. doi: 10.7448/IAS.16.1.18586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nsibande D, Doherty T, Ijumba P, Tomlinson M, Jackson D, Sanders D, Lawn J. Assessment of the uptake of neonatal and young infant referrals by community health workers to public health facilities in an urban informal settlement, KwaZulu-Natal, South Africa. BMC Health Serv Res. 2013;13:47. doi: 10.1186/1472-6963-13-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Puoane TR, Zulu J, Tsolekile L, Bradly HA, Hughes GD. Community Health Workers’ Intervention Programme for Primary Prevention of Non-Communicable Diseases in Khayelitsha, an Urban Township in Cape Town. School of Public Health, University of the Western Cape; Bellville, South Africa: 2007. [Google Scholar]
- 21.Cruse D. Community Health Workers In South Africa: Information For Provincial Policy Makers. Health Systems Trust for the National Department of Health; Durban, South Africa: 1997. [Google Scholar]
- 22.Mendoza Montano C, Fort M, RM . Health Promotion International. Evaluation of a pilot hypertension and diabetes prevention programme for Guatemalan adults. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montano CM, Estrada K, Chávez A, Ramírez-Zea M. Perceptions, knowledge and beliefs about prevention of cardiovascular diseases in Villa Nueva, Guatemala. Prevention and Control. 2008;3:1–9. [Google Scholar]
- 24.Puoane T, Bradley H, Matsanda N, Alexander L. Training manual: Primary prevention of Non-Communicable Diseases (Lifestyle Modification) for Health Workers. Bellville, South Africa: School of Public Health, University of the Western Cape; 2005. [Google Scholar]
- 25.Welsh E. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2002. Dealing with data: Using NVivo in the qualitative data analysis process. [Google Scholar]
- 26.Basit T. Manual or electronic? The role of coding in qualitative data analysis. Educational Research. 2003;45:143–154. [Google Scholar]
- 27.C. o. C. T. Strategic Development Information and GIS Department, editor. 2011 Census – Cape Town: Profile for Suburb of Khayelitsha (July 2013) Cape Town, South Africa: Statistics South Africa; 2013. [Google Scholar]
- 28.Rowe AK, Onikpo F, Lama M, Deming MS. Evaluating health worker performance in Benin using the simulated client method with real children. Implementation Science. 2012;7:95. doi: 10.1186/1748-5908-7-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rowe AK, de Savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? The Lancet. 2005;366:1026–1035. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
- 30.Waiswa P, Kemigisa M, Kiguli J, Naikoba S, Pariyo GW, Peterson S. Acceptability of evidence-based neonatal care practices in rural Uganda - implications for programming. BMC Pregnancy Childbirth. 2008;8:21. doi: 10.1186/1471-2393-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wadler BM, Judge M, Prout JD, Allen AC, Geller AC. Improving Breast Cancer Control via the Use of Community Health Workers in South Africa: A Critical Review. LID - 10.1155/2011/150423 [doi] LID - 150423 [pii], 20101011 DCOM-20110714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beidas RS, Cross W, Dorsey S. Show me, don’t tell me: Behavioral rehearsal as a training and analogue fidelity tool. Cognitive and Behavioral Practice. 2014;21:1–11. doi: 10.1016/j.cbpra.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kahn RG. The Role of Community Health Workers in Northeast Brazil. [Google Scholar]
- 34.Martinez J, Ro M, Villa NW, Powell W, Knickman JR. Transforming the Delivery of Care in the Post–Health Reform Era: What Role Will Community Health Workers Play? American Journal of Public Health. 2011;101:e1. doi: 10.2105/AJPH.2011.300335. [DOI] [PMC free article] [PubMed] [Google Scholar]