Abstract
Ehlers-Danlos syndrome, characterized by hyperextensible skin, hypermobile joints, and fragile vessels, is the most common heritable disorder of connective tissue and has an estimated prevalence of 1 in 5000. Pulmonary involvement with signs of lung destruction (bullous emphysema) as first presentation is unusual. We report a case of monozygotic twins 37 years old men with occasional evidence of bullous emphysema with previously undiagnosed Ehlers-Danlos syndrome type IV. We emphasize the importance of considering uncommon genetic causes of emphysema in young adults, discuss underlining pathophysiological mechanisms and propose a conservative management and follow-up.
Keywords: Ehlers-Danlos syndrome, Hemoptysis, Bullous emphysema, Monozygotic twins
Introduction
Ehlers-Danlos syndrome (EDS) type IV, also known as the vascular type of EDS, is an inherited disorder of connective tissue characterized by arterial and digestive complications which are rarely observed in other forms of EDS and affect 80% of patients by the age of 40 [1]. Pulmonary complications are rare including pneumothorax, hemoptysis, cavitary lung lesions and bullous emphysema [2]. Pulmonary signs is very uncommon as first presentation of type IV EDS [3]. We report a case of twins 37 years old men with occasional evidence of bullous emphysema with previously undiagnosed type IV EDS.
Case presentation
A 37 year man presented to the emergency department for a first episode of hemoptysis accompanied by stabbing right hemithoracic pain. He was a current heavy smoker (29 pack years) and he was working in a fiberglass boats factory. Medical history was negative for preceding pulmonary diseases and positive for capillary fragility with bruising and propensity to develop ecchymosis. Chest x-ray revealed a large distended cystic bullae in the upper right lobe with compression of remaining pulmonary parenchyma. Chest CT show multiple emphysematous bullae in the middle and upper lobe of right lung. In the upper and lingular lobe of left lung paraseptal and panlobular emphysema was also evident (Fig. 1). Patient was transferred to Pulmonary Unit in a stable clinical condition. Arterial gas-analysis was normal during spontaneous breathing and serum blood analysis revealed only mild elevation of CRP, VES and fibrinogen. No abnormality was present in the hemostasis screening test. Bronchoscopy showed blood coming from upper right lobe. Pulmonary function test demonstrated normal lung volumes with moderate reduction of carbon monoxide diffusing capacity (3, 25 ml/min/mmHg/L, 54% pred.) (Table 1). A significant difference between slow and forced vital capacity (6.24 L vs 4.84 L) was evident. Deeping into patient familiar medical history we discovered that patient had a twin homozygous brother current asymptomatic heavy smoker with bullous emphysema occasionally diagnosed by screening chest x-ray. Alpha-1 antitrypsin was in the normal range in both brothers. Skin was found to be thin and translucent with slightly hyperextensive of small joints of extremities (Fig. 2). An EDS was so suspected. Characteristic facial appearance was not so evident. Molecular gene testing was done to confirm the diagnosis in twins. Genomic DNA was extracted from peripheral blood leukocytes. Sequencing analysis of the patient's DNA revealed a novel missense mutation (c.2996G[A]; Gly999Asp) in exon 41 of the COL3A1 gene characteristic of EDS type IV. Echocardiography revealed no significant alterations in twins. Natural course of disease in the hospitalized twin was benign and hemoptysis with thoracic pain disappeared after two days after hospital admission. Twins were advised to stop smoking and has been followed for pulmonary and vascular emergencies. After three months twins are in a stable clinical condition.
Fig. 1.
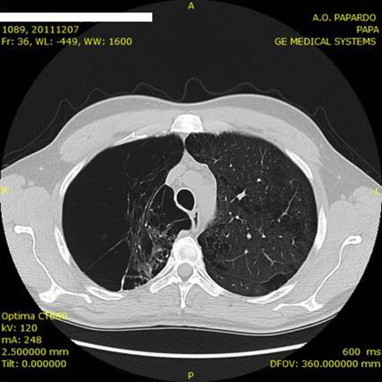
Chest computed tomography showing multiple emphysematous bullae in the middle and upper lobe of right lung. In the upper and lingular lobe of left lung paraseptal and panlobular emphysema was also evident.
Table 1.
Pulmonary function test.
| Reference | Actual | % Reference | |
|---|---|---|---|
| Spirometry | |||
| FVC (L) | 4.48 | 4.84 | 108 |
| FEV1 (L) | 3.73 | 4.14 | 111 |
| FEV1/FVC (%) | 86 | 80 | 107 |
| FEV1/SVC (%) | 66 | 83 | 80 |
| FEF 25–75% (L/sec) | 4.39 | 4.48 | 102 |
| Lung Volumes | |||
| SVC (L) | 4.48 | 6.24 | 139 |
| IC(L) | 3.27 | 4.17 | 127 |
| ERV(L) | 1.21 | 2.08 | 171 |
| TGV (L) | 3.23 | 3.85 | 119 |
| RV (Pleth) (L) | 1.82 | 1.77 | 97 |
| TLC (Pleth) (L) | 6.50 | 8.02 | 123 |
| RV/TLC (Pleth) % | 29 | 22 | 76 |
| Diffusing Capacity | |||
| DLCOcor (ml/min/mmHg) | 31 | 22.84 | 74 |
| DL/VA (ml/min/mmHg/L) | 6.02 | 3.25 | 54 |
Fig. 2.

Slightly hyperextensive of small joints of extremities.
Discussion
The EDS is an inherited defect (autosomal dominant) of connective tissue characterized by soft and hyperextensible thin skin, hypermobile joints, and a particular tendency to bruising and bleeding. Eight or more clinical types are currently recognized [4]. Specific biochemical abnormalities of collagen are known in EDS [4]. Literature review reveal no systematic association between EDS and pulmonary emphysema with only few cases report [5,6]. A more intrinsic correlation was found between Cutis Laxa and pulmonary emphysema [7]. In our case a differential diagnosis for congenital emphysematous diseases can be made (Table 2). EDS was more probable because of twin association. Obviously emphysema in both twins was aggravated by cigarette smoke exposure. Upper lobes predominance is attributable to the pressure gradient that augments stress to the upper lung zones. Moreover, the right-sided preponderance, as seen in this case, may be attributed to the larger septal surface area, reduced connective tissue support, and poorer blood supply of the lung. The ball-valve mechanism may accentuate dynamic hyperinflation in the emphysematous lung. Marked difference between SVC and FVC demonstrated collapsible airways due to decreased lung compliance during forced maneuver [8]. In our case FRC was measured by pletismography. It would have been interesting to perform a comparison with the determination of the FRC measured by He dilution test that only evaluates the ventilated volume. Significant reduction al DLCO/VA is attributable to significant reduction of lung surface and lung blood supply. In both twins surgical reduction of emphysema was not recommended for several reasons: traditionally, bullectomy is offered to patients in whom bulla fill half of the chest cavity with relatively preserved adjacent parenchyma [5]. In the case presented a diffuse bullous, paraseptal and panlobular emphysema was evident. Postoperative hemorrhagic complication of surgery in EDS patients is very high [5] and this procedure should be reserved to only emergency situations like massive pneumothorax or non resolving hemoptysis [9]. Bronchoscopic lung volume reduction with endobronchial valve is not indicated because patient wasn't hyperinflated and coil or thermal vapor ablation treatment has not been recommended for the risk of severe complications.
Table 2.
Genetic diseases associated with bullous emphysema.
| Inherited defect of connective: Cutis laxa, Ehlers-Danlos syndrome, Marfan syndrome |
| Idiopathic giant bullous emphysema (Vanishing lung syndrome) |
| Birt-Hogg-Dubè Syndrome |
| Neurofibromatosis |
| Placental transmogrification of the lung |
| Fabry disease |
| Salla disease |
Early resolving symptoms let us to consider a conservative approach with close monitoring and immediate smoking cessation program. The absence of chronic respiratory symptoms, such as exertional dyspnea, in presence of normal pulmonary function test not suggested inhaled treatment with bronchodilator agents.
A vascular follow-up is moreover important for known cardiovascular complications. A genetic counseling was extended to other family members.
Conclusion
Rare genetic causes can be considered in young adults presenting with not previous diagnosed bullous emphysema. EDS type IV can presented with predominantly pulmonary manifestation that can be early diagnosed and managed very carefully to avoid more serious complications.
Consent
Written informed consent was obtained from the twins patients for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Author's contribution
P.R. have made substantial contributions to conception, design and drafting of case report manuscript.
S.C. have made been involved in data acquisition.
G.G. have been involved to revisiting manuscript critically.
List of abbrevations
- CRP
C-reactive protein
- VES
erythrocyte sedimentation rate
- SVC
slow vital capacity
- FVC
forced vital capacity
- FRC
functional residual capacity
- DLCO/VA
diffusion capacity for carbon monoxide/alveolar volume
References
- 1.Pepin M., Schwarze U., Superti-Furga A., Byers Peter H. Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med. 2000;342(10):673–680. doi: 10.1056/NEJM200003093421001. [DOI] [PubMed] [Google Scholar]
- 2.Ayres J.G., Pope F.M., Reidy J.F., Clark T.J. Abnormalities of the lungs and thoracic cage in the Ehlers-Danlos syndrome. Thorax. 1985;40(4):300–305. doi: 10.1136/thx.40.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hatake K., Morimura Y., Kudo R., Kawashima W., Kasuda S., Kuniyasu H. Respiratory complications of Ehlers-Danlos syndrome type IV. Leg Med Tokyo. 2013;15(1):23–27. doi: 10.1016/j.legalmed.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 4.De Paepe A., Malfait F. The Ehlers-Danlos syndrome, a disorder with many faces. Clin Genet. 2012;82(1):1–11. doi: 10.1111/j.1399-0004.2012.01858.x. [DOI] [PubMed] [Google Scholar]
- 5.Safdar Z., O'Sullivan M., Shapiro J.M. Emergent bullectomy for acute respiratory failure in Ehlers-Danlos syndrome. J Intensive Care Med. 2004;19(6):349–351. doi: 10.1177/0885066604269645. [DOI] [PubMed] [Google Scholar]
- 6.Cavanaugh M.J., Cooper D.M. Chronic pulmonary disease in a child with the Ehlers-Danlos syndrome. Acta Paediatr Scand. 1976;65(6):679–684. doi: 10.1111/j.1651-2227.1976.tb18002.x. [DOI] [PubMed] [Google Scholar]
- 7.Champion P., Ryan F. A case of congenital cutis laxa (generalized elastolysis) Can Respir J. 2005;12(3):151–152. doi: 10.1155/2005/624875. [DOI] [PubMed] [Google Scholar]
- 8.Chan E.D., Irvin C.G. The detection of collapsible airways contributing to airflow limitation. Chest. 1995;107(3):856–859. doi: 10.1378/chest.107.3.856. [DOI] [PubMed] [Google Scholar]
- 9.Bergqvist D., Bjorck M., Wanhainen A. Treatment of vascular Ehlers-Danlos syndrome: a systematic review. Ann Surg. 2013;258(2):257–261. doi: 10.1097/SLA.0b013e31829c7a59. [DOI] [PubMed] [Google Scholar]


