Abstract
Purpose
We compared the fixation stability measurements obtained with two microperimeters, the Micro Perimeter 1 (MP-1) and the Spectral OCT/SLO (OCT/SLO), in subjects with and without maculopathies.
Methods
A total of 41 eyes with no known ocular diseases and 45 eyes with maculopathies were enrolled in the study. Both eyes of each participant had a 20-second fixation test using the MP-1 and OCT/SLO. The bivariate contour ellipse area (BCEA) was used for fixation stability evaluation.
Results
In the normal group, BCEA was 2.93 ± 0.32 log minarc2 on OCT/SLO and 2.89 ± 0.30 log minarc2 on MP-1. In the maculopathy group, BCEA was 3.05 ± 0.41 log minarc2 on OCT/SLO and 3.15 ± 0.46 log minarc2 on MP-1. There was no statistically significant difference between the BCEA measured by OCT/SLO and by MP-1 in both groups. A moderate correlation was found between the two devices (r = 0.45, P < 0.001). The sample size during the fixation test was 535.5 ± 14.6 pairs of coordinates in the normal group and 530.7 ± 14.9 pairs in the maculopathy group with MP-1, while it was 72.3 ± 6.9 and 59.9 ± 10.1, respectively, with OCT/SLO. This was due to different tracking frequencies between the two microperimeters.
Conclusion
Fixation stability assessment yields similar results using the OCT/SLO and MP-1. A major difference in sampling rate between the two microperimeters does not significantly affect BCEA measurements.
Translational Relevance
Fixation stability assessments are comparable and interchangeable between the OCT/SLO and the MP-1.
Keywords: microperimetry, fixation stability, comparison
Introduction
Fixation stability, the precision of eye fixation when one fixates intently on a stimulus for a certain period of time, is a fundamental component of visual performance.1 It has been shown that fixation stability is impaired in patients with macular diseases2–4 and correlates with slow reading speed.5
The bivariate contour ellipse area (BCEA) values and the Fujii classification6 have been applied to measure fixation stability measurements using microperimeters. By plotting the position of each fixation point on a Cartesian axis and calculating the area of an ellipse that encompasses a given percentage of fixation points,7 BCEA provides a precise continuous value with a smaller value implying a more stable fixation.8 The Fujii classification is a semi-quantitative method.6 In this classification, fixation stability is classified as being: stable when 75% of fixation falls within a 2° circle, relatively unstable when 75% of fixation falls within a 4° circle, and unstable when less than 75% of fixation falls within a 4° circle.6 The arbitrariness of this classification recently has been criticized in the literature.3,8 The BCEA value has been shown to correlate strongly with the reading performance, whereas Fujii classification has not shown similar correlations.8
The Micro Perimeter 1 (MP-1; Nidek Technologies, Padova, Italy) has been the first microperimeter that uses a true eye-tracking system and allows a comprehensive fixation stability assessment.9 The fixation examination can be completed either as part of the routine light sensitivity examination or as an isolated test. The device built-in software automatically provides the BCEA values as well as the Fujii fixation grading.
Spectral OCT/SLO (OCT/SLO; Optos Plc., Dunfermline, UK) is a newer microperimeter that correlates retina sensitivity deficits not only with SLO infrared images (retinal en face images), but also with bidimensional cross-sectional OCT retinal images.10 It offers the same fixation test options as the MP-1 (either as part of the routine sensitivity examination or as a stand-alone test). In the routine sensitivity test of the OCT/SLO, the fixation stability is graded according to the Fujii classification. The isolated fixation test is designed for documenting the preferred retinal locus (PRL); hence, no BCEA or Fujii grading is provided. However, it is possible to export the raw data of the isolated fixation test (the Cartesian coordinates of fixation points during the test) and calculate the BCEA offline.
With different working parameters, the outputs of these two microperimeters are not the same. In our previous study,11 we explored the comparability and interchangeability of the sensitivity values provided by the two machines, which differ due to the inherent stimulus/background contrasts for sensitivity examinations. A dissimilarity of tracking frequency exists between their eye-tracking system settings: 25 Hz in MP-1 and 8 Hz in the OCT/SLO. An understanding of the comparability between fixation tests is vital as numerous studies are applying either MP-1 or OCT/SLO to analyze the fixation characteristics in various macular disorders.12–14
Comparing fixation stability results during routine sensitivity testing is not reliable due to variable test times, even when the same sensitivity pattern is used. For example, a subject who completes the Polar-3 sensitivity test in 3 minutes on MP-1 may complete the same pattern on OCT/SLO in 5 minutes. This, again, is due to the differences of sensitivity test algorithms or settings.
Hence, in this prospective study, we evaluated the fixation stability as an isolated fixation test in subjects with and without maculopathies using these two types of microperimetry devices. The fixation stability was evaluated quantitatively using BCEA.
Participants and Methods
Participants
In this prospective study, the inclusion criteria for normal subjects was best-corrected visual acuity ≥20/20, refractive errors within ± 6.00 diopters (D) sphere and ±1.00 D cylinder, and no known history of ocular diseases. Participants in the maculopathy group could have no more than one diagnosis of retinal disease involving the macula in the study eye. The type of macular disease was not specified as a criterion; maculopathy included diabetic macular edema, central serous retinopathy, idiopathic macular hole, age-related macular degeneration (AMD), and so forth.
The study followed the tenets of the Declaration of Helsinki and was approved by the Johns Hopkins Institutional Review Board/Ethics Committee. Informed consent was obtained from all subjects.
Methods
Fixation Examination
A single fixation test was performed in all participants using MP-1 and Spectral OCT/SLO. During the fixation test, subjects were asked to look toward the center of a 2° red cross target for 20 seconds with the fellow eye patched. Both eyes could be enrolled in the study if they met the study criteria.
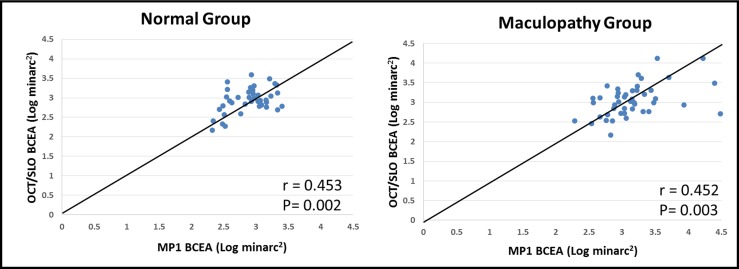
The working principle of the fixation tracking system in both microperimeters is the same. First, a reference image of the fundus is captured, and a reference area of high-contrast retinal landmark is selected. During the examination, built-in software (MP-1 SW 1.7 and OCT/SLO GUI 1.87) tracks the reference area, calculating any shift in its position between the reference image and the real-time fundus image at a certain frequency (25 Hz in MP-1 and 8 Hz in the OCT/SLO) and producing x and y coordinates of retinal position. If tracking of the real-time image fails, coordinates are not generated until tracking is resumed. At the end of testing, a scatter graph of fixation points is displayed (Fig. 1).
Figure 1. .
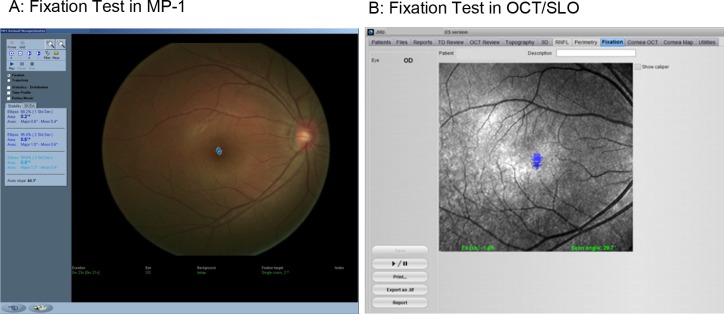
The fixation test in the MP-1 and the OCT/SLO microperimeters. Each of the blue dots represents the retinal area gazing the center of the target at a certain time; therefore, the cloud of dots identifies the retinal area involved in fixating a target stimulus.
BCEA Calculation
The BCEA value encompassing 68% of fixation was calculated using the formula:
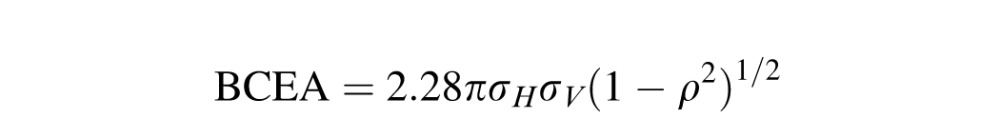 |
where σH and σV are the standard deviations of the fixation position in the horizontal and vertical meridians, respectively, and ρ is the product moment correlation of these two components.
The MP-1 built-in BCEA value was based on standardized fixation points, that is, eliminating the extreme outlier coordinates that were beyond ±3 standard deviations (SD). The fixation raw data of the OCT/SLO was exported (.csv data) and calculated in the same way as the MP-1.
Statistical Analysis
For statistical analysis, BCEA values (minutes of arc2) were normalized with a log transformation. In addition to the correlation between two devices, agreement between values from each instrument was assessed using the techniques described by Bland and Altman,15 whereby the difference between the two measurements is plotted against their mean.
Wilcoxon signed-ranks test was applied to compare the sample sizes between the two microperimeters due to the non-normal distribution of the data. The independent t-test and Mann Whitney test were used to compare the sample sizes between the groups according to normal or non-normal distribution of the data.
A P value less than 0.05 was considered statistically significant. All analyses were performed using SPSS statistical package (Version 19.0; SPSS, Inc., Chicago, Illinois).
Results
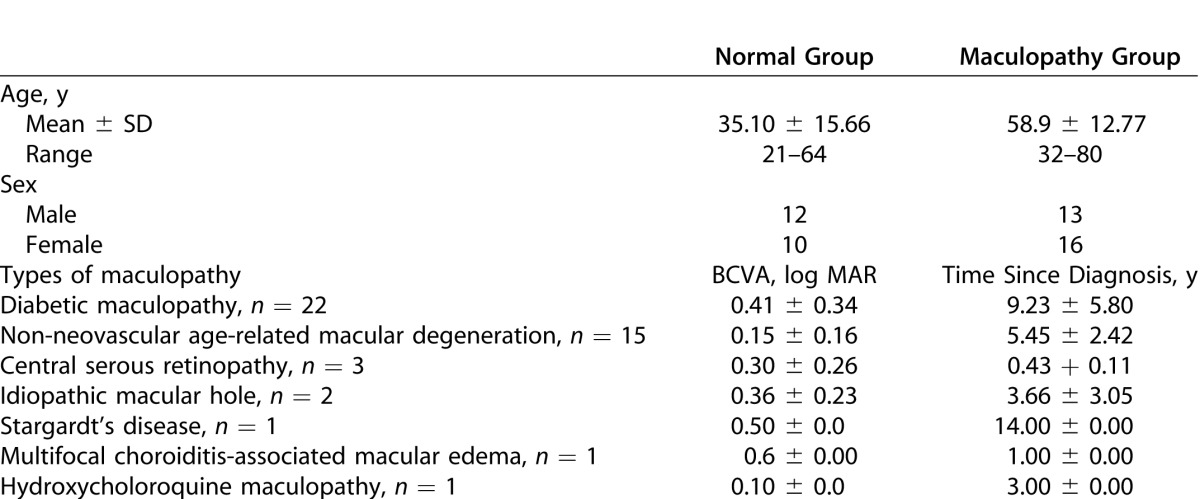
A total of 44 eyes of 22 healthy volunteers and 58 eyes of 29 patients with maculopathies were screened initially. Three eyes in the normal group and 13 eyes in the maculopathy group were excluded due to high refractive error (exceeding ± 6.00 D sphere and ±1.00 D cylinder) or not being able to detect the fixation target because of poor visual acuity. Therefore, 41 eyes from the 22 healthy volunteers (10 females, 12 males) with a mean age of 35.1 year (range, 21–64 years) and 45 eyes of the 29 patients with maculopathies (16 females, 13 males) with a mean age of 58.9 year (range, 32–80 years) were included prospectively in the study.
Maculopathies included diabetic maculopathy (22 eyes), age-related macular degeneration (15 eyes), central serous retinopathy (3 eyes), idiopathic macular hole (2 eyes), Stargardt's disease (1 eye), multifocal choroiditis with cystoid macular edema (1 eye), and hydroxychloroquine maculopathy (1 eye). Detailed demographic information of the study subjects are shown in Table 1.
Table 1. .
Demographics Information for Normal and Maculopathy Group
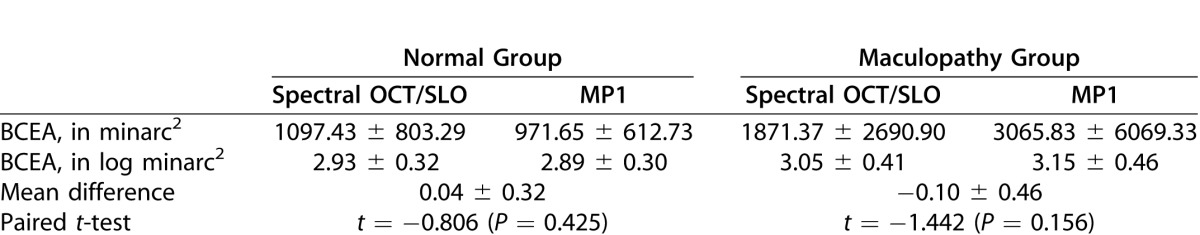
The BCEA values of the OCT/SLO and MP-1 are shown in Table 2. In the normal group, the BCEA was 2.93 ± 0.32 log minarc2 in the OCT/SLO and 2.89 ± 0.30 log minarc2 in the MP-1, with a mean difference of 0.04 ± 0.32 log minarc2 between the two microperimeters. In the maculopathy group, BCEA was 3.05 ± 0.41 log minarc2 in the OCT/SLO and 3.15 ± 0.46 log minarc2 in the MP-1, with a mean difference of −0.10 ± 0.46 log minarc2. There was no statistically significant difference between the two microperimeters in both groups.
Table 2. .
BCEA Values Measured with Two Microperimeters
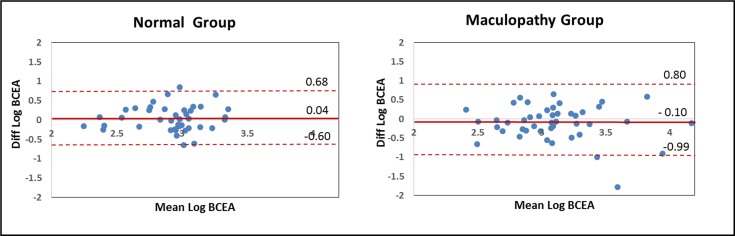
When the BCEA values of the two microperimeters were plotted against each other, the majority of data were distributed along the line of equality (Fig. 2). A moderate correlation between the two devices was found in both groups (r = 0.45, P < 0.05).
Figure 2. .
Plot of the BCEA values of two microperimeters.
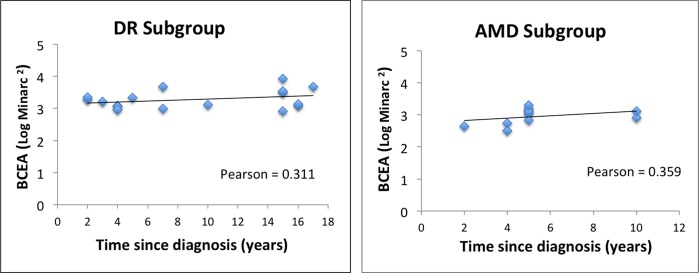
The Bland-Altman plots of BCEA values showed a good agreement in the two devices (Fig. 3), with 95% confidence limit of agreement of 0.68 to −0.60 log minarc2 in the normal group and 0.80 to −0.99 log minarc2 in the maculopathy group. As the main disease entities were diabetic maculopathies (diabetic retinopathy [DR], 22 eyes) and AMD (15 eyes), with the remaining 8 eyes scattered in six disease types, the relationship between BCEA and time since diagnosis was explored in the DR and AMD subgroups. The average BCEA from the MP-1 and OCT/SLO were applied, as the two types of microperimeters have no difference in the BCEA measurements.
Figure 3. .
The Bland-Altman plots of BCEA values in two microperimeters. Solid lines: Mean difference between the two values. Dashed lines: The 95% confidence limit of agreement. All values are in log minutes of arc squared.
Figure 4. .
The relationship between BCEA and time since diagnosis.
The mean time since diagnosis was 9.23 ± 5.80 years in the DR subgroup and 5.45 ± 2.42 years in the AMD subgroup. The BCEA correlated positively with time since diagnosis, but this correlation did not reach statistical significance (Pearson DR group = 0.311, Pearson AMD group = 0.359, both P > 0.05).
The sample sizes during the fixation test are shown in Table 3. More fixation points were generated by the MP-1 compared to the OCT/SLO for normal and maculopathy groups (P < 0.001). Within MP-1, the fewer sample size in the maculopathy group compared to the normal group did not achieve statistical significance (P = 0.95). However, for the OCT/SLO, the fewer sample size in the maculopathy group compared to the normal group reached the threshold of statistical significance (P = 0.007). The outliers accounted for 1% to 2% of the total sample size, regardless of the different devices or groups.
Table 3. .
Sample Size (Number of Fixation Points) Captured During the Fixation Test
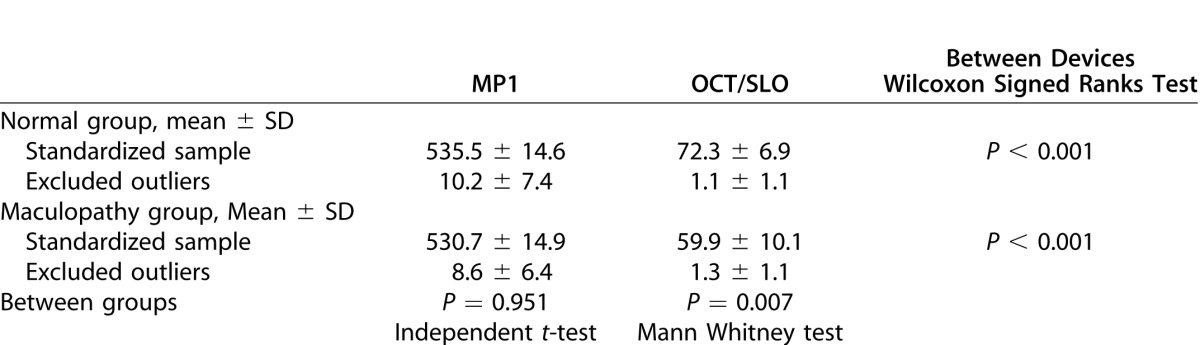
Table 4. .
BCEA of Full and Undersampled Data Set in MP1 (Unit, Minarc2)
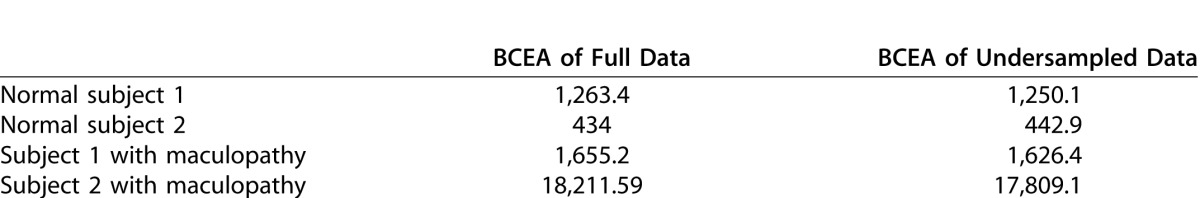
As the tracking frequency of OCT/SLO is approximately one-third of that in MP-1 (8 Hz in the OCT/SLO, compared to 25 Hz in MP-1), we also undersampled two representative MP-1 data files from each group by retaining every third line of the data, but discarding all others. In each subject, the BCEA of the undersampled data was comparable to that of the full data set (Table 3).
Discussion
Previous reports have shown that BCEA values with normal vision range from 80 to 1200 minarc2, while in macular diseases, the values range from near normal values to over 13,000 minarc2.1 Similar to visual acuity, BCEA usually is log-transformed due to non-normal distribution. In our study, BCEA values of the normal and maculopathy groups consistently fell within this data range.
The BCEA values are known to be influenced by different methods of fixation assessment. For example, BCEA obtained from SLO are up to 2.25 times smaller than those obtained from an infrared eye tracker system.16 This is due mainly to the participant's head being stabilized on a chin rest in the SLO, while the latter is a head-mounted eye tracker where the eye movements compensate for small head movements.16 The chin rest is applied in OCT/SLO and MP-1, which guaranteed a similar degree of head immobilization during the fixation test.
Extreme outlier coordinates beyond ±3 SD of fixation data also can influence BCEA measurements.3 These outliers often occur at blinks or spurious saccades during fixation test, which typically represent approximately 1% of all data.3 In our study, BCEA values can be 2 to 3 times smaller after eliminating the outlier. For example, BCEA of a normal subject was 2708.5 minarc2 when calculated using total fixation data, but dropped to 896.7 minarc2 when standardized data was used. The BCEA calculations in this study were based on standardized data of both devices; hence, there were no bias of outliers in the BCEA values.
With the tracking frequency of 25 Hz in MP-1 and 8 Hz in OCT/SLO, the sample size of MP1 was much more than that of OCT/SLO. However, it seems that sampling rate does not introduce BCEA differences at the given order of magnitude. No statistically significant difference of BCEA values was observed between the two devices in both groups. This also was observed in the study of Dunbar et al.,17 who reported no differences in BCEA evaluation when comparing 12.5 Hz of SLO and 25 Hz of MP-1.
In support of this finding, the undersampled BCEA was equivalent to the full data BCEA when the fixation data was reduced to one-third of its original size in our representative samples. This is in agreement with previous studies in which undersampling the fixation data of an infrared eye tracker to one-twentieth of its length16 or halving the MP1 fixation data17 did not result in different BCEA values.
Sample size in the maculopathies group was slightly less than that of the normal group when testing with MP-1, while this difference reached statistical significance in the OCT/SLO. Compared to normal subjects, subjects with maculopathies have impaired fixation stability and are more likely to lose the tracking of the microperimeter with no fixation coordinates generated in a fixed total fixation time. This difference may not be revealed when the tracking frequency is relatively high as in the MP-1, but may become obvious in the case of low tracking frequency as in the OCT/SLO. Increasing the tracking frequency in OCT/SLO may provide more complete fixation coordinates in diseased subjects and help to eliminate the difference of sampling between normal and diseased eyes.
Fixation location is another important aspect of fixation function. The distribution of the fixation points can be overlapped with the fundus images to indicate the fixation location as microperimetry allows simultaneous fundus observation and compensation of eye movements during the examination.18–20
Unfortunately, comparing the fixation location assessments currently is not available due to the methods of fixation location recording differing between the two microperimeters. In the MP-1, the Fujii grading of fixation locations (as central, pericentral, and eccentric) will be provided automatically after the reviewer manually annotated the fovea with the cursor by the built-in software. In OCT/SLO, the fixation test is designed originally for documenting the PRL, with a built-in caliper provided to measure the distance between the PRL and fovea (also must be annotated by the reviewer). Hence, there was no unified measurement parameter to access the fixation location in both devices. However, since the fixation tracking principles of both devices were very similar and they have shown the consistency in fixation stability measurement, it can be reasonably presumed that the fixation location will be in good agreement.
It has been reported that patients with macular disease may use two or more PRLs for fixation. Although PRL numbers will better describe the fixation location characteristics of retinal disease, accessing the numbers of PRL and calculating each “local” BCEA require special graphic processing techniques and complicated statistical computation, such as the kernel density estimator (KDE) and expectation maximization (EM) algorithm.21 For a device-comparison study that focus especially on fixation stability, we believe that “global” BCEA is sufficient to evaluate agreement between devices.
To compare fixation stability measurements of the two microperimeters, we examined various types of maculopathies with these two devices. The etiologies for the maculopathy were heterogeneous. No disease-specific conclusion could be drawn from the current study, due to the large variation in lesion characteristics, disease courses, and the small sample numbers in each subgroup. In our DR and AMD subgroups, BCEA increased with the time since diagnosis, which was consistent with the study by Luminita et al.3 The relationship did not reach statistical significance, probably due to the better BCEA and smaller sample size in our subdisease group compared to their study.
As for the user experience, the quality of SLO confocal fundus image in the OCT/SLO is superior to the infrared camera image in the MP-1, and does not need to be registered into the color fundus photography. Such image quality makes choosing the retina landmark much easier and fixation test operation smoother in the OCT/SLO compared to the MP-1.
On the other hand, we recommend that the OCT/SLO develops built-in BCEA values. The BCEA calculation has its considerable computational complexity. Exporting and standardizing the fixation raw data also is a very time-consuming task.
In summary, OCT/SLO and MP-1 were in high agreement with each other in obtaining the fixation stability, although the OCT/SLO device uses a smaller sample size than the MP-1. Both may be used in clinical care for patients with maculopathies.
Acknowledgments
We thank Michael D. Crossland, Institute of Ophthalmology, University College London, United Kingdom, for the validation of the BCEA calculation.
Meeting Presentation: Presented in part at the 2012 Association for Research of Vision and Ophthalmology Annual Meeting, May 6–10, 2012, Fort Lauderdale, Florida.
Footnotes
Financial Disclosure(s): The Johns Hopkins University and the University of Nebraska Medical Center have received research support from OPKO, Inc. and Optos, Inc. The sponsor had no role in the design or conduct of this research. The study was supported by the Hendrik Scholl Research Grant Award at the Wilmer Eye Institute, Johns Hopkins University (HL) and Research to Prevent Blindness (QDN). Dr. Nguyen serves on the Scientific Advisory Board for Optos, Inc. and Nidek, Inc.
Disclosure: H. Liu, None; M.G. Bittencourt, None; R. Sophie, None; Y.J. Sepah, None; M. Hanout, None; Z. Rentiya, None; R. Annam, None; H.P.N. Scholl, Fovea Pharmaceuticals, Trevena Inc., Guidepoint Global, LLC, Gerson Lehrman Group; Q.D. Nguyen, Optos, Inc., Nidek, Inc.
References
- 1.Gonzalez EG, Teichman J, Lillakas L, Markowitz SN, Steinbach MJ. Fixation stability using radial gratings in patients with age-related macular degeneration. Canad J Ophthalmol. 2006;41:333–339. doi: 10.1139/I06-019. [DOI] [PubMed] [Google Scholar]
- 2.Kube T, Schmidt S, Toonan F, Kirchof B, Wolf S. Fixation stability and macular light sensitivity in patients with diabetic maculopathy: a microperimetric study with a scanning laser ophthalmoscope. Ophthalmologica. 2005;219:16–20. doi: 10.1159/000081777. [DOI] [PubMed] [Google Scholar]
- 3.Tarita-Nistor L, Gonzalez EG, Markowitz SN, Steinbach MJ. Fixation characteristics of patients with macular degeneration recorded with the mp-1 microperimeter. Retina. 2008;28:125–133. doi: 10.1097/IAE.0b013e3180ed4571. [DOI] [PubMed] [Google Scholar]
- 4.Bellmann C, Feely M, Crossland MD, Kabanarou SA, Rubin GS. Fixation stability using central and pericentral fixation targets in patients with age-related macular degeneration. Ophthalmology. 2004;111:2265–2270. doi: 10.1016/j.ophtha.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Crossland MD, Culham LE, Rubin GS. Fixation stability and reading speed in patients with newly developed macular disease. Ophthalmic Physiol Opt. 2004;24:327–333. doi: 10.1111/j.1475-1313.2004.00213.x. [DOI] [PubMed] [Google Scholar]
- 6.Fujii GY, de Juan E, Jr, Sunness J, Humayun MS, Pieramici DJ, Chang TS. Patient selection for macular translocation surgery using the scanning laser ophthalmoscope. Ophthalmology. 2002;109:1737–1744. doi: 10.1016/s0161-6420(02)01120-x. [DOI] [PubMed] [Google Scholar]
- 7.Steinman RM. Effect of target size, luminance, and color on monocular fixation. J Opt Soc Am. 1965;55:1158–1165. [Google Scholar]
- 8.Crossland MD, Dunbar HM, Rubin GS. Fixation stability measurement using the MP1 microperimeter. Retina. 2009;29:651–656. doi: 10.1097/IAE.0b013e318196bd65. [DOI] [PubMed] [Google Scholar]
- 9.Midena E, Vujosevic S, Cavarzeran F. Normal values for fundus perimetry with the microperimeter MP1. Ophthalmology. 2010;117:1571–1576. doi: 10.1016/j.ophtha.2009.12.044. [DOI] [PubMed] [Google Scholar]
- 10.Anastasakis A, McAnany JJ, Fishman GA, Seiple WH. Clinical value, normative retinal sensitivity values, and intrasession repeatability using a combined spectral domain optical coherence tomography/scanning laser ophthalmoscope microperimeter. Eye (Lond) 2011;25:245–251. doi: 10.1038/eye.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu H, Bittencourt MG, Wang J, et al. Assessment of central retinal sensitivity employing two types of microperimetry devices. Transl Vis Sci Technol. 2014;3:3. doi: 10.1167/tvst.3.5.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carpineto P, Ciancaglini M, Di Antonio L, Gavalas C, Mastropasqua L. Fundus microperimetry patterns of fixation in type 2 diabetic patients with diffuse macular edema. Retina. 2007;27:21–29. doi: 10.1097/01.iae.0000256658.71864.ca. [DOI] [PubMed] [Google Scholar]
- 13.Midena E, Radin PP, Pilotto E, Ghirlando A, Convento E, Varano M. Fixation pattern and macular sensitivity in eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. A microperimetry study. Semin Ophthalmol. 2004;19:55–61. doi: 10.1080/08820530490882896. [DOI] [PubMed] [Google Scholar]
- 14.Vujosevic S, Pilotto E, Bottega E, Benetti E, Cavarzeran F, Midena E. Retinal fixation impairment in diabetic macular edema. Retina. 2008;28:1443–1450. doi: 10.1097/IAE.0b013e318183571e. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 16.Crossland MD, Rubin GS. The use of an infrared eyetracker to measure fixation stability. Optom Vis Sci. 2002;79:735–739. doi: 10.1097/00006324-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Dunbar HM, Crossland MD, Rubin GS. Fixation stability: a comparison between the Nidek MP-1 and the Rodenstock scanning laser ophthalmoscope in persons with and without diabetic maculopathy. Invest Ophthalmol Vis Sci. 2010;51:4346–4350. doi: 10.1167/iovs.09-4556. [DOI] [PubMed] [Google Scholar]
- 18.Andersen MV. Scanning laser ophthalmoscope microperimetry compared with Octopus perimetry in normal subjects. Acta Ophthalmol Scand. 1996;74:135–139. doi: 10.1111/j.1600-0420.1996.tb00057.x. [DOI] [PubMed] [Google Scholar]
- 19.Menke MN, Sato E, Van De Velde FJ, Feke GT. Combined use of SLO microperimetry and OCT for retinal functional and structural testing. Graefes Arch Clin Exp Ophthalmol. 2006;244:634–638. doi: 10.1007/s00417-005-0088-2. [DOI] [PubMed] [Google Scholar]
- 20.Rohrschneider K, Springer C, Bültmann S, Völcker HE. Microperimetry--comparison between the micro perimeter 1 and scanning laser ophthalmoscope--fundus perimetry. Am J Ophthalmol. 2005;139:125–134. doi: 10.1016/j.ajo.2004.08.060. [DOI] [PubMed] [Google Scholar]
- 21.Crossland MD, Simms M, Galbraith RF, Rubin GS. Evaluation of a new quantitative technique to assess the number and extent of preferred retinal loci in macular disease. Vision Res. 2004;44:1537–1546. doi: 10.1016/j.visres.2004.01.006. [DOI] [PubMed] [Google Scholar]