Abstract
Deterioration in premorbid functioning is a common feature of schizophrenia, but sensitivity to psychosis conversion among clinical high-risk samples has not been examined. This study evaluates premorbid functioning as a predictor of psychosis conversion among a clinical high-risk sample, controlling for effects of prior developmental periods. Participants were 270 clinical high-risk individuals in the North American Prodrome Longitudinal Study—I, 78 of whom converted to psychosis over the next 2.5 years. Social, academic, and total maladjustment in childhood, early adolescence, and late adolescence were rated using the Cannon–Spoor Premorbid Adjustment Scale. Early adolescent social dysfunction significantly predicted conversion to psychosis (hazard ratio = 1.30, p = .014), independently of childhood social maladjustment and independently of severity of most baseline positive and negative prodromal symptoms. Baseline prodromal symptoms of disorganized communication, social anhedonia, suspiciousness, and diminished ideational richness mediated this association. Early adolescent social maladjustment and baseline suspiciousness together demonstrated moderate positive predictive power (59%) and high specificity (92.1%) in predicting conversion. Deterioration of academic and total functioning, although observed, did not predict conversion to psychosis. Results indicate early adolescent social dysfunction to be an important early predictor of conversion. As such, it may be a good candidate for inclusion in prediction algorithms and could represent an advantageous target for early intervention.
Poor premorbid functioning is a central feature of schizophrenia (Kraepelin, 1919) and of other psychotic disorders (Tarbox, Brown, & Haas, 2011). Premorbid dysfunction is strongly associated with postonset illness characteristics including severity of negative symptoms, cognitive deficits, motor slowing, and treatment refraction (e.g., Addington, van Mastrigt, & Addington, 2003; Haim, Rabinowitz, & Bromet, 2006; Larsen, McGlashan, Johannessen, & Vibe-Hansen, 1996; Levitt, O'Donnell, McCarley, Nestor, & Shenton, 1996; Silverstein, Mavrolefteros, & Turnbull, 2003). Furthermore, a history of poor functioning in childhood and adolescence in nonpsychotic adult relatives of schizophrenia patients (Shapiro et al., 2009; Walshe et al., 2007), including monozygotic twins (Picchioni et al., 2010), suggests a genetic component to this association.
Studies of first- and multiple-episode psychotic disorders emphasize the prognostic importance of functioning prior to psychosis onset (Haas, & Sweeney, 1992; MacBeth, & Gumley, 2008). “Stable-poor” and “deteriorating” patterns of functioning are associated with earlier age of onset, greater severity and poorer treatment responsiveness of negative symptoms, worse social functioning, greater poverty of movement, greater deficits in verbal fluency and verbal memory, and poorer quality of life (e.g., Addington & Addington, 2005; Haas & Sweeney, 1992; Strous et al., 2004). In addition, premorbid social dysfunction is particularly associated with longer duration of untreated psychosis, greater severity of negative symptoms at baseline and at 5-year follow-up, and decreased likelihood of remission of negative symptoms after 5 years (Larsen et al., 2004; Piskulic, Addington, Auther, & Cornblatt, 2011; Strous et al., 2004), whereas poor premorbid academic functioning is associated with earlier onset of prodromal symptoms and greater neurocognitive deficits (e.g., working memory and verbal learning; Larsen et al., 2004; Norman, Malla, Manchanda, & Townsend, 2005; Rund et al., 2007).
Functioning in Clinical High-Risk (CHR) Individuals
Poor functioning is an important feature of the premorbid period (Tarbox & Pogue-Geile, 2008) and may also predict conversion to psychosis among individuals identified clinically as high risk for psychosis (Miller et al., 2002; Yung et al., 1996). Such individuals are at high risk for becoming psychotic (Ruhrmann et al., 2010; Woods et al., 2009), yet many do not convert (Addington et al., 2011). Improving prediction of which “high-risk” individuals are truly at risk has become an important area of investigation.
At baseline, CHR individuals demonstrate significant deficits in global social and role functioning 1 compared to normal controls (Addington, Penn, Woods, Addington, & Perkins, 2008; Corcoran et al., 2011; Cornblatt et al., 2007; Pinkham, Penn, Perkins, Graham, & Siegel, 2007; Woods et al., 2009). Furthermore, the CHR individuals who convert to psychosis have significantly worse social and/or role functioning compared to nonconverters (Cornblatt et al., 2011; Dragt et al., 2011; Mason et al., 2004; Yung et al., 2003; Yung, Phillips, Yuen, & McGorry, 2004). Functioning at baseline is consistently found to be one of the few predictor variables making a significant contribution to prediction of psychosis independent of prodromal symptoms (Cannon et al., 2008; Ruhrmann et al., 2010; Thompson, Nelson, & Yung, 2011; Velthorst et al., 2009).
Developmental change in premorbid functioning has received less attention, but it may also be an important correlate of conversion to psychosis. The PAS (Cannon-Spoor, Potkin, & Wyatt, 1982) provides separate social and academic maladjustment ratings for childhood, early and late adolescence, and adulthood. Reports from the North American Prodrome Longitudinal Study (NAPLS-I) consortium that use the PAS suggest a pattern of premorbid functional deterioration through late adolescence in CHR individuals (Addington et al., 2008; Woods et al., 2009). Furthermore, studies from the Dutch Prediction of Psychosis Study and the Psychological Assistance Service (Carr et al., 2000) suggest a possible correlation between deterioration of functioning from childhood to early adolescence and transition to psychosis (Dragt et al., 2011; Mason et al., 2004).
At this time, the association between premorbid functional development and conversion to psychosis has not been examined directly in CHR youths, and there are no data on development of premorbid functioning in relation to baseline prodromal symptoms. As such, it appears timely to assess prospectively whether premorbid functioning is informative regarding risk of psychosis conversion (MacBeth & Gumley, 2008). To our knowledge, this is the first prospective study of premorbid functional development and prediction of psychosis in CHR individuals.
Method
The data here are from the NAPLS-I consortium, a collaboration of eight NIMH-funded projects prospectively examining psychosis-risk factors. The database has been described previously (Addington et al., 2007). The Structured Interview for Psychosis-Risk Syndromes (SIPS) was used to evaluate and monitor psychosis-risk symptoms. Diagnostic agreement with gold standard SIPS diagnoses was in the excellent range (κ > 0.80) at each center (Addington et al., 2007). Detailed descriptions of SIPS symptom severity scales and psychometric properties are available (Hawkins et al., 2004; Lencz, Smith, Auther, Correll, & Cornblatt, 2004; McGlashan, Walsh, & Woods, 2010; Miller et al., 2002, 2003). The database was closed to inclusion of follow-up information after September 30, 2006.
Participants
The NAPLS-I study includes data for 860 nonpsychotic individuals enrolled across the eight sites between 1998 and 2005. After clinical referral, 377 individuals across sites met criteria for psychosis-risk syndromes outlined in the SIPS interview (McGlashan et al., 2010; Woods et al., 2009). Specifically, one or more of three risk-syndrome criteria had to be met: (a) new onset or recent worsening of subsyndromal (“attenuated”) positive psychotic symptoms, (b) very brief periods of fully psychotic positive symptoms, or (c) deterioration in functioning within the last year and having either schizotypal personality disorder or a first-degree relative with psychosis. Detailed research definitions of the three psychosis-risk syndromes have been published previously (McGlashan et al., 2010; Miller et al., 2002, 2003). In the literature, this psychosis-risk syndrome population is often referred to as CHR, and that is the convention we follow.
Current study
Participants meeting criteria for a psychosis-risk syndrome (i.e., CHR) were eligible for the current study if SIPS follow-up data were available for a minimum of 6 months and if PAS (Cannon-Spoor et al., 1982) data were available.
Assessments
Baseline assessments were conducted at each site. Positive, negative, disorganized, and general psychosis-risk symptoms were rated using the Scale of Psychosis-risk Symptoms contained within the SIPS (Hawkins et al., 2004; Lemos et al., 2006; Lencz et al., 2004; McGlashan et al., 2010; Miller et al., 2002, 2003) for nearly all participants. Comorbid Axis I and II diagnoses were established by structured interview, for example, the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1995) and the Structured Interview for DSM-IV Personality Disorders (Zimmerman & Coryell, 1989), conducted by trained interviewers who met local reliability standards.
Conversion to psychosis
The primary course variable was time from baseline to conversion to psychosis. After baseline assessment, the SIPS was readministered at 6-month intervals for up to 30 months. Conversion to psychosis was defined, according to criteria operationalized in the SIPS, as the presence of positive symptoms of sufficient intensity that are either seriously disorganizing or dangerous, or have been present for at least half the days in a month for at least an hour per day (McGlashan et al., 2010; Miller et al., 2002, 2003). Cases that were possibly converting were interviewed with the SIPS and a structured diagnostic interview to determine DSM-IV-TR psychotic disorder diagnosis. When potentially converting participants could not be interviewed in person, sites established best estimates of conversion diagnosis based on review of hospital and other medical records and telephone interviews with participants, family members, and members of the treatment team.
Premorbid functioning
The PAS (Brill, Reichenberg, Weiser, & Rabinowicz, 2008; Cannon-Spoor et al., 1982) was administered to the participant at the baseline assessment. The PAS is an interview-based rating schedule designed to assess functioning retrospectively, particularly social and academic maladjustment. The PAS has established predictive and concurrent validity (Brill et al., 2008) and is one of the most widely used measures of premorbid functioning in schizophrenia. Items are interviewer rated on a 7-point scale based on an interview with the patient, with 0 representing freedom from maladjustment and higher ratings representing greater maladjustment. The interview focuses on four periods of development: childhood (age 5–11), early adolescence (age 12–15), late adolescence (age 16–18), and adulthood (age 19 and above). Social functioning items (e.g., withdrawal and peer relationships) are rated for all four age periods. Academic functioning items (scholastic performance, adaptation to school) are rated for childhood through late adolescence. General information, including years of education, occupational history, and independence in living, also is assessed. Total maladjustment ratings are calculated for each developmental period and for overall functioning.
Premorbid adjustment ratings
For the current study, mean PAS ratings were derived for social, academic, and total maladjustment (social and academic ratings combined) for three developmental periods: childhood, early adolescence, and late adolescence. Adult maladjustment was not included in analyses because ratings for that period were only available for 35.2% of the sample, and adult ratings that were available were excluded to minimize overlap with the putative prodromal phase of the disorder. The primary reason for missing adult items was baseline age under 18 years, in which case adult maladjustment ratings were not applicable. The general information PAS ratings also were not utilized in keeping with the developmental emphasis of the hypotheses and concerns of bias against younger participants (Van Mastrigt & Addington, 2002).
Analyses
Group demographic comparisons were accomplished using either t tests or chi-square analyses. Identification of demographic characteristics that could potentially confound associations between premorbid functioning and conversion to psychosis was accomplished by first identifying demographic factors that differentiated the conversion and nonconversion groups and then examining these identified demographic variables for correlation with PAS ratings in the full CHR sample. The threshold for significance was adjusted for multiple comparisons. This process was repeated to identify potential confounds to the associations between premorbid maladjustment and baseline prodromal symptoms and between baseline prodromal symptoms and conversion to psychosis.
Cox proportional hazards regression was the primary technique used to examine the associations between premorbid maladjustment ratings and conversion status at follow-up for the social, academic, and total functioning domains. In this method, predictors are modeled in relation to time from baseline to conversion, and noncompleters contribute all available observations to the model up to time of censorship. This approach maximizes sample size and power under conditions in which complete data are not available for all participants. In these analyses, applicable covariates were entered into the model first, followed by predictors of interest.
First, individual contributions of maladjustment at each developmental period to conversion outcome, without accounting for maladjustment at other ages, were examined in separate Cox regression models. Second, standardized maladjustment ratings for childhood, early adolescence, and late adolescence were entered sequentially into a Cox regression model to examine developmental effects on conversion at each age while controlling for maladjustment at prior developmental periods. Accounting for earlier developmental periods in this manner tests the extent to which maladjustment arising in successive developmental periods contributes to prediction of psychosis over and above any existing differences in maladjustment. Models were tested that included one predictor (childhood), two predictors (childhood and early adolescence), and three predictors (childhood, early adolescence, and late adolescence). Omnibus tests were conducted at each step to examine if the addition of a predictor (“step change”) resulted in a model with a better fit to the data than before the predictor was added. Omnibus tests were also performed to examine “overall” fit of each model.
It was expected that some of the younger participants would not have late adolescent data, requiring the three predictor models to be tested in a smaller sample restricted to participants with data for all three developmental periods. Thus, for comparison, child and early adolescent two-predictor models were estimated in both the full and the restricted sample. Given the conservative nature of these analyses, the relative contributions of childhood, early adolescence, and late adolescence to prediction of psychosis were also examined without the imposed developmental sequence using backward stepwise elimination (likelihood-ratio test).
Third, for each significant relation between premorbid maladjustment and conversion, mediation effects of baseline severity of positive and negative prodromal symptoms as assessed on the SIPS (unusual thought content, suspiciousness, grandiose ideas, perceptual abnormalities, disorganized communication, social anhedonia, avolition, [diminished] expression of emotion, experience of emotion and self, [diminished] ideational richness, and occupational functioning) were tested using the approach suggested by Baron and Kenny (1986). Evidence of mediation requires loss of significant association between premorbid maladjustment and conversion when accounting for the prodromal symptom, in conjunction with significant association between premorbid maladjustment and the prodromal symptom and between the prodromal symptom and conversion. As such, associations between individual premorbid maladjustment ratings and conversion status were retested for loss of significance when prodromal symptoms were included in the Cox regression model. Next, the effects of premorbid maladjustment ratings on prodromal symptom severity scores were tested using linear regression modeling, and the effects of prodromal symptom scores on conversion status, controlling for premorbid maladjustment, were tested using Cox regression modeling.
Fourth, combined effects of premorbid maladjustment and baseline severity of positive and negative prodromal symptoms on prediction of conversion status were examined for each maladjustment rating and prodromal symptom rating identified as uniquely associated with conversion. Each of these predictors was dichotomized, such that sensitivity and specificity to conversion were maximized as determined by receiver operating characteristic analysis. Each maladjustment rating was paired with each symptom rating to form dichotomized variables indicating individuals who were rated positive on both characteristics versus those with one or zero positive ratings. Individuals who were missing either characteristic were excluded from these analyses. Cox regression analysis was performed to examine the effect of each unique and combined dichotomized predictor on conversion status. Receiver operating characteristic and life table survival analyses were used to calculate positive and negative likelihood ratios and positive and negative predictive values for each predictor.
Results
Sample characteristics
There were 270 CHR individuals who had at least partial PAS data and who were followed in the study for a minimum of 6 months. Seventy-eight of these CHR participants converted to psychosis during the 2.5-year follow-along period.
Demographic and clinical comparisons
Demographic characteristics of the full CHR sample and the conversion and nonconversion groups are presented in Table 1. At a conservative threshold of p < .007 to correct for multiple comparisons, the conversion sample entered the study earlier (mean baseline year: 2001.3 vs. 2002.4; p < .001) than those who did not convert. Reported age of first positive prodromal symptom was available for a subsample of 149 participants. Converters in this subsample (n = 39) reported a later age of positive prodromal symptom onset compared to nonconverters (n = 110; M age = 18.4, SD = 3.7 vs. M age = 16.0, SD = 4.3, respectively;p = .003). In the complete sample, converters and nonconverters did not differ on baseline age, sex, race, baseline education, mother education, or father education.
Table 1. Demographic characteristics of full, conversion, and nonconversion groups.
| Conversion Status (n) | Demographic Characteristics | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age (years) Mean (SD) |
% Male | % EuAm/ % AfAm |
Education (years) Mean (SD) |
Mother HS% |
Father HS% |
Baseline Year Mean (SD) |
|
| Full CHR sample (270) | 18.0 (4.5) | 59.3 | 79.6/9.3 | 10.3 (3.1) | 90.8 | 91.3 | 2002.0 (1.9) |
| Psychosis conversion (78) | 18.4 (3.8) | 55.1 | 76.9/12.8 | 10.6 (2.7) | 87.2 | 86.0 | 2001.3*** (1.9) |
| Nonconversion (192) | 17.9 (4.8) | 60.9 | 80.7/7.8 | 10.1 (3.2) | 93.5 | 95.1 | 2002.4 (1.9) |
Note: HS%, percentage with at least a high school level of education; CHR, clinical high risk.
p < .001. Psychosis conversion > nonconversion.
Baseline mean severity ratings of positive and negative prodromal symptoms for the full CHR sample and the conversion and nonconversion groups are presented in Table 2. At a conservative threshold of p ≤ .005 (given multiple comparisons), the conversion group reported greater severity of suspiciousness (p < .001), disorganized communication (p < .001), social anhedonia (p < .001), and ideational richness (p < .001) compared to nonconverters.
Table 2. Severity of positive and negative prodromal symptoms at baseline in the full, conversion, and nonconversion groups.
| Conversion Status (n) |
Positive Prodromal Symptom SIPS Score | Negative Prodromal Symptom SIPS Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Unusual Thought Content |
Suspic. | Grandi. Ideas |
Percept. Abnorm. |
Disorg. Comm. |
Social Anhed. |
Avolit. | Express. Emot. |
Exper. Emot/Self |
Ideation. Rich. |
Occup. Funct. |
|
| Full CHR sample (270) | 3.10 (1.5) | 2.83 (1.5) | 1.14 (1.3) | 3.02 (1.7) | 2.51 (1.9) | 2.51 (1.9) | 2.44 (1.7) | 1.48 (1.6) | 1.44 (1.7) | 1.28 (1.5) | 3.17 (1.8) |
| Psychosis conversion (78) | 3.38 (1.6)* | 3.46 (1.4)*** | 1.14 (1.5) | 3.15 (1.7) | 2.42 (1.6)*** | 3.27 (1.8)*** | 2.70 (1.7) | 1.84 (1.6)* | 1.62 (1.7) | 1.86 (1.6)*** | 3.53 (1.7)* |
| Nonconversion (192) | 2.98 (1.4) | 2.57 (1.4) | 1.14 (1.3) | 2.96 (1.7) | 1.63 (1.4) | 2.20 (1.9) | 2.33 (1.7) | 1.33 (1.5) | 1.37 (1.6) | 1.05 (1.4) | 3.02 (1.9) |
Note: All values are means (standard deviations). SIPS, Structured Interview for Psychosis-Risk Syndromes; CHR, clinical high risk.
p ≤ .05.
p ≤ .001.
Psychosis conversion > nonconversion.
Premorbid maladjustment
The unadjusted social, academic, and total maladjustment mean PAS ratings for the psychosis conversion and nonconversion groups are presented in Table 3, and social and academic maladjustment across developmental periods is represented in Figure 1. PAS ratings across developmental periods were significantly, positively correlated with each other, and the strength of these associations was similar regardless of domain or conversion status. The correlations in the complete CHR sample ranged across domains as follows: r childhood = .44 versus r early adolescence = .47, r early adolescence = .69 versus r late adolescence = .78, and r childhood = .32 versus r late adolescence = .40. However, diagnostics indicated no significant collinearity among developmental periods for social, academic, or total functioning.
Table 3. Premorbid maladjustment ratings and univariate prediction of conversion to psychosis versus nonconversion.
| Conversion Status | Developmental Period | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Childhood | Early Adolescence | Late Adolescence | ||||
|
|
|
|
||||
| Mean (SE, n) | HR (95% CI) | Mean (SE, n) | HR (95% CI) | Mean (SE, n) | HR (95% CI) | |
| Social maladjustment | ||||||
| Psychosis conversion | 1.70 (0.2, 72) | 1.16 (0.92–1.44) | 2.20 (0.2, 74) | 1.30* (1.06–1.61) | 2.30 (0.2, 57) | 1.23† (0.96–1.58) |
| Nonconversion | 1.46 (0.1, 173) | 1.72 (0.1, 177) | 1.82 (0.1, 99) | |||
| Academic maladjustment | ||||||
| Psychosis conversion | 1.48 (0.1, 72) | 0.97 (0.77–1.21) | 2.34 (0.2, 73) | 0.91 (0.72–1.13) | 2.58 (0.2, 56) | 1.06 (0.83–1.36) |
| Nonconversion | 1.42 (0.1, 171) | 2.41 (0.1, 177) | 2.21 (0.2, 99) | |||
| Total maladjustment | ||||||
| Psychosis conversion | 1.59 (1.2, 72) | 1.06 (0.85–1.34) | 2.25 (1.1, 74) | 1.12 (0.90–1.40) | 2.39 (1.3, 57) | 1.14 (0.88–1.49) |
| Nonconversion | 1.44 (1.0, 175) | 1.99 (1.6, 180) | 1.97 (1.2, 102) | |||
Note: Mean values reflect unadjusted Premorbid Adjustment Scale ratings, with higher scores representing greater pathology. Cox regression analyses were performed using standardized Premorbid Adjustment Scale ratings. The covariate for academic and total maladjustment is baseline year. HR, hazard ratio; CI, confidence interval.
p ≤ .10.
p ≤ .05.
Psychosis conversion > nonconversion.
Figure 1.
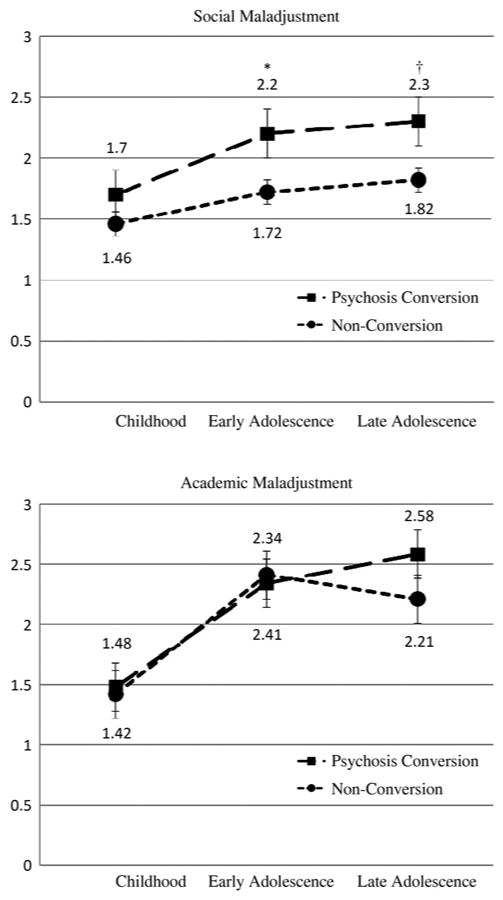
Social and academic maladjustment across development in clinical high-risk (CHR) individuals who converted to psychosis versus nonconverters. Data labels for psychosis conversion are positioned above the data points; labels for nonconversion are below. Values are unadjusted mean Premorbid Adjustment Scale ratings, with higher scores representing greater pathology. Error bars indicate standard error of the mean scores. Cox regression analyses were performed using standardized Premorbid Adjustment Scale ratings. The covariate for academic maladjustment is baseline year. Psychosis conversion > nonconversion: †p < .10, *p < .05.
Demographic characteristics and premorbid maladjustment
Full sample
In the full CHR sample, at a significance threshold of p ≤ .007 (given multiple comparisons), male participants had worse social functioning in early (p = .007) and late adolescence (p = .001). Less education at baseline was associated with worse academic adjustment in childhood (p < .001), early adolescence (p < .001), and late adolescence (p = .002), and worse total adjustment in early (p < .001) and late adolescence (p < .001). Younger age at baseline was associated with worse academic and total adjustment in early adolescence (academic, p < .001; total, p = .002). Earlier year of study entry was associated with worse academic and total adjustment in early (academic, p = .004; total, p = .005) and late adolescence (academic, p = .006; total, p = .001). In the subsample of participants with data on age of first positive prodromal symptom, earlier age of symptom onset was associated with worse academic adjustment in childhood (p = .006) and early adolescence (p < .001), and worse total adjustment in early adolescence (p < .001). Race, mother education, and father education were not associated with social, academic, or total adjustment in the full sample.
Conversion sample
Among converters, at a conservative threshold of p ≤ .006, less education at baseline was associated with worse academic adjustment in early (p < .001) and late adolescence (p = .001). Baseline age, age at conversion, age of first positive prodromal symptom, year of study entry, sex, race, mother education, and father education were not associated with social, academic, or total adjustment among converters.
Nonconversion sample
Among nonconverters, at a significance threshold of p ≤ .007, male participants had worse academic functioning in late adolescence (p = .003). Less education at baseline was associated with worse academic adjustment in childhood (p < .001), early adolescence (p < .001), and late adolescence (p = .002), and younger age at baseline was associated with worse academic adjustment in early adolescence (p < .001). Earlier year of study entry was associated with worse academic adjustment in childhood (p = .003) and late adolescence (p = .005). Among participants with data on reported age of first positive prodromal symptom, earlier age of symptom onset was associated with worse academic adjustment in childhood (p = .001) and early adolescence (p < .001), and worse total adjustment in early adolescence (p < .001). Race, mother education, and father education were not associated with social, academic, or total adjustment among nonconverters.
Covariates for premorbid maladjustment and conversion analyses
In the full CHR sample, year of baseline assessment correlated both with conversion status and with academic and total adjustment in early and late adolescence, but it was not correlated with social adjustment at any age. Thus, year of baseline assessment was included as a covariate in all regression analyses testing the association between conversion status and academic or total adjustment unless noted otherwise. Reported age of first positive prodromal symptom correlated both with conversion status and with academic adjustment in childhood and early adolescence and total adjustment in early adolescence, but it was not associated with social adjustment. Given that these data were only available for 55% of the sample, reported age of first positive prodromal symptom was not automatically included as a covariate. In the case of significant associations between academic or total maladjustment and conversion, potential effects of age of positive prodromal symptom onset were examined. No covariates were included in analyses of social maladjustment.
Demographic characteristics and baseline prodromal symptoms
Full sample
In the full CHR sample, at a significance threshold of p ≤ .006, male participants had greater severity of disorganized communication (p < .001). Less education at baseline was associated with worse occupational functioning (p = .003), and earlier year of study entry was associated with greater severity of perceptual abnormalities (p = .005). In the subsample of participants with data on age of first positive prodromal symptom, older age at positive prodromal symptom onset was associated with greater severity of unusual thought content (p = .003). Age at baseline, race, mother education, and father education were not associated with severity of baseline prodromal symptoms in the full sample.
Conversion sample
In the conversion sample, at a conservative threshold of p ≤ .006, male participants had greater severity of disorganized communication (p < .001). Age at baseline, age at conversion, age of first positive prodromal symptom, year of study entry, race, mother education, and father education were not associated with severity of baseline prodromal symptoms among converters.
Nonconversion sample
Among nonconverters, at a significance threshold of p ≤ .006, female participants had greater severity of unusual thought content (p = .005) and perceptual abnormalities (p = .004). Earlier year of study entry was also associated with greater severity of perceptual abnormalities (p = .001). Less education at baseline was associated with worse occupational functioning (p = .004). Lower educational achievement in either parent was associated with greater severity of ideational richness (mother p = .005; father p = .006). Age at baseline, age of first positive prodromal symptom, and race were not associated with severity of baseline prodromal symptoms in the nonconversion sample.
Covariates for prodromal symptom and conversion analyses
In the full CHR sample, year of study entry correlated both with conversion status and with baseline severity of perceptual abnormalities and thus was included as a covariate in regression analyses testing the association between perceptual abnormalities and conversion status. Reported age of first positive prodromal symptom correlated both with conversion status and with severity of unusual thought content, but it was not automatically included as a covariate in regression analyses given that prodrome symptom onset data were only available for 55% of the sample. In the case of significant association between unusual thought content and conversion, potential effects of age of positive prodromal symptom onset were examined.
Covariates for premorbid maladjustment and prodromal symptom analyses
In the full CHR sample, sex was associated with baseline severity of disorganized communication and social maladjustment in early and late adolescence. Number of years of education at baseline was associated with occupational functioning at baseline and with academic adjustment in childhood, early adolescence, and late adolescence, and total adjustment in early and late adolescence. Likewise, year of study entry was associated with baseline severity of perceptual abnormalities and with academic and total adjustment in early and late adolescence. Sex, years of education, and year of study entry were thus included as covariates in relevant analyses.
Among converters, there were no demographic characteristics associated with both prodromal symptom severity and premorbid maladjustment. Among nonconverters, sex was associated with baseline severity of unusual thought content and perceptual abnormalities, and with academic maladjustment in late adolescence. Year of study entry was associated with severity of perceptual abnormalities and with academic maladjustment in childhood and late adolescence. Number of years of education at baseline was associated with occupational functioning and with academic maladjustment in childhood, early adolescence, and late adolescence. Sex, year of study entry, and years of education were thus included as covariates in relevant analyses in the nonconversion sample.
Premorbid maladjustment and prediction of conversion to psychosis
Premorbid maladjustment in independent developmental periods
Table 3 presents the independent effects of social, academic, and total maladjustment at each developmental period on conversion status. Cox regression analyses of social maladjustment at each developmental period indicated that compared to nonconverters, individuals who converted to psychosis were rated significantly higher (greater pathology) on social maladjustment for early adolescence (hazard ratio [HR]=1.30, p = .014). In contrast, converters and nonconverters did not differ on academic or total maladjustment at any developmental period. The results for academic and total maladjustment did not change if baseline year was excluded from the model.
Progression of premorbid maladjustment across development
Social maladjustment
The effects of early and late adolescent functioning on conversion status were examined further by controlling for the effect of maladjustment at previous developmental periods. Accounting for previous developmental periods tests the extent to which additional maladjustment arising in successive developmental periods contributes to prediction of psychosis over and above existing maladjustment. Consistent with univariate analyses, results of multivariate analysis indicated that when accounting for childhood maladjustment, social maladjustment in early adolescence continued to be associated with significantly greater risk of conversion to psychosis relative to “risk” of nonconversion in the full sample (HR = 1.28, Wald χ2 = 4.00, p = .046; Table 4, Model 1). In the restricted sample of participants for whom late adolescent ratings were available (n = 139), social maladjustment in early adolescence was associated at a trend level with risk of conversion to psychosis when controlling for childhood maladjustment (Table 4, Model 2). In this restricted sample, late adolescent social maladjustment did not predict psychosis when controlling for the effects of both childhood and early adolescent maladjustment (Table 4, Model 3). Omnibus testing indicated that the addition of late adolescence (Model 3) did not provide a better fit to the data than the model in which childhood and early adolescence are the only predictors (Model 2). When the relative contributions of childhood, early adolescent, and late adolescent social maladjustment were examined simultaneously in the restricted sample without specifying developmental sequence through stepwise backward elimination (Table 4, Model 4), early adolescent social maladjustment was retained in the model as the only unique predictor of psychosis (HR = 1.33, Wald χ2 = 4.70, p = .030).
Table 4. Social maladjustment and prediction of conversion to psychosis versus nonconversion.
| Predictors | Parameter Estimates | Omnibus Tests | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Overall | Step Changea | |||||||||
|
|
|
|
||||||||
| β | SE β | Wald | p | HR (eβ) | 95% CI (eβ) | χ2 | p | χ2 | p | |
| Model 1 (n = 240) | ||||||||||
| Childhood social adj. | 0.02 | 0.13 | 0.02 | .900 | 1.02 | 0.79–1.31 | ||||
| Early adoles. social adj. | 0.25 | 0.12 | 4.00 | .046 | 1.28 | 1.01–1.63 | 5.52 | .063 | 3.87 | .049 |
| Model 2 (n = 139) | ||||||||||
| Childhood social adj. | 0.04 | 0.14 | 0.10 | .755 | 1.05 | 0.79–1.38 | ||||
| Early adoles. social adj. | 0.27 | 0.14 | 3.49 | .062 | 1.31 | 0.99–1.74 | 4.82 | .090 | 3.29 | .070 |
| Model 3 (n = 139) | ||||||||||
| Childhood social adj. | 0.04 | 0.14 | 0.08 | .780 | 1.04 | 0.79–1.38 | ||||
| Early adoles. social adj. | 0.22 | 0.19 | 1.32 | .250 | 1.25 | 0.86–1.82 | ||||
| Late adoles. social adj. | 0.07 | 0.18 | 0.15 | .695 | 1.07 | 0.76–1.52 | 4.98 | .173 | 0.15 | .695 |
| Model 4 (n = 139) | ||||||||||
| Early adoles. social adj. | 0.29 | 0.13 | 4.70 | .030 | 1.33 | 1.03–1.73 | 4.75 | .029 | ||
Note: A Cox regression analysis was performed using standardized Premorbid Adjustment Scale ratings. The reference group is nonconversion. Models 1–3, the method is forced entry; Model 4, the method is stepwise backward elimination. HR, hazard ratio; CI, confidence interval.
The change from the previous step. For Model 1, this indicates the change from a univariate model with childhood as the only predictor (see Table 3). For Model 3, this indicates the change from Model 2.
Academic maladjustment
The association between developmental course of academic maladjustment and risk of conversion to psychosis versus nonconversion was examined next. Results of multivariate Cox regression analyses paralleled those of univariate tests and indicated that when accounting for effects of earlier developmental periods, academic functioning in early and late adolescence was not significantly associated with risk of conversion to psychosis relative to nonconversion in the complete sample (Table 5, Model 1) and in the restricted sample of participants for whom late adolescent ratings were available (Table 5, Models 2 and 3). When the relative contributions of childhood, early adolescent, and late adolescent academic maladjustment were examined simultaneously in the restricted sample through stepwise backward elimination, none of the developmental periods were retained in the model. Results for academic maladjustment did not change if baseline year was excluded from these models. Given that none of the models for academic maladjustment were significant, omnibus tests of model fit are not presented in Table 5.
Table 5. Academic maladjustment and prediction of conversion to psychosis versus nonconversion.
| Predictors | Parameter Estimates | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| β | SE β | Wald | p | HR (eβ) | 95% CI (eβ) | |
| Model 1 (n = 238) | ||||||
| Baseline year | −0.21 | 0.06 | 11.65 | .001 | 0.81 | 0.72–0.92 |
| Childhood acad. adj. | 0.02 | 0.13 | 0.02 | .887 | 1.02 | 0.79–1.32 |
| Early adoles. acad. adj. | −0.09 | 0.13 | 0.49 | .486 | 0.91 | 0.70–1.18 |
| Model 2 (n = 135) | ||||||
| Baseline year | −0.16 | 0.07 | 5.23 | .022 | 0.85 | 0.74–0.98 |
| Childhood acad. adj. | 0.03 | 0.15 | 0.05 | .823 | 1.04 | 0.77–1.39 |
| Early adoles. acad. adj. | 0.10 | 0.16 | 0.36 | .547 | 1.10 | 0.80–1.52 |
| Model 3 (n = 135) | ||||||
| Baseline year | −0.16 | 0.07 | 5.09 | .024 | 0.85 | 0.74–0.98 |
| Childhood acad. adj. | 0.03 | 0.15 | 0.05 | .833 | 1.03 | 0.77–1.39 |
| Early adoles. acad. adj. | 0.05 | 0.24 | 0.04 | .834 | 1.05 | 0.66–1.68 |
| Late adoles. acad. adj. | 0.06 | 0.21 | 0.08 | .783 | 1.06 | 0.70–1.61 |
Note: The reference group is nonconversion, and the method is forced entry. A Cox regression analysis was performed using standardized Premorbid Adjustment Scale ratings. HR, hazard ratio; CI, confidence interval.
Total maladjustment
Results for total maladjustment were similar to those for academic maladjustment. Consistent with univariate analyses, results of multivariate Cox regression analyses indicated that total maladjustment in early and late adolescence was not associated with risk of conversion when controlling for effects of earlier developmental periods in the complete sample (Table 6, Model 1) and in the restricted sample of participants for whom late adolescent ratings were available (Table 6, Models 2 and 3). When the relative contributions of childhood, early adolescent, and late adolescent total maladjustment were examined through stepwise backward elimination in the restricted sample, none of the developmental periods were retained in the model. Results for total maladjustment did not change if baseline year was excluded from these models. Because none of the models for total maladjustment were significant, omnibus tests of model fit are not presented in Table 6.
Table 6. Total maladjustment and prediction of conversion to psychosis versus nonconversion.
| Predictors | Parameter Estimates | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| β | SE β | Wald | p | HR (eβ) | 95% CI (eβ) | |
| Model 1 (n = 247) | ||||||
| Baseline year | −0.20 | 0.06 | 10.66 | .001 | 0.82 | 0.73–0.92 |
| Childhood total adj. | 0.01 | 0.13 | 0.00 | .953 | 1.01 | 0.78–1.31 |
| Early adoles. total adj. | 0.11 | 0.13 | 0.71 | .398 | 1.12 | 0.87–1.44 |
| Model 2 (n = 141) | ||||||
| Baseline year | −0.16 | 0.07 | 5.09 | .024 | 0.85 | 0.74–0.98 |
| Childhood total adj. | 0.06 | 0.14 | 0.21 | .651 | 1.06 | 0.81–1.39 |
| Early adoles. total adj. | 0.16 | 0.15 | 1.27 | .260 | 1.18 | 0.89–1.57 |
| Model 3 (n = 141) | ||||||
| Baseline year | −0.16 | 0.07 | 4.92 | .027 | 0.85 | 0.74–0.98 |
| Childhood total adj. | 0.06 | 0.14 | 0.18 | .671 | 1.06 | 0.81–1.39 |
| Early adoles. total adj. | 0.10 | 0.20 | 0.24 | .622 | 1.11 | 0.74–1.65 |
| Late adoles. total adj. | 0.09 | 0.21 | 0.20 | .656 | 1.10 | 0.73–1.64 |
Note: The reference group is nonconversion, and the method is forced entry. A Cox regression analysis was performed using standardized Premorbid Adjustment Scale ratings. HR, hazard ratio; CI, confidence interval.
Effect of baseline prodromal symptoms
The predictive association between early adolescent social maladjustment and conversion to psychosis was examined further to test the mediation and combined effects of baseline severity of positive prodromal symptoms (unusual thought content, suspiciousness, grandiose ideas, perceptual abnormalities, and disorganized communication) and negative prodromal symptoms (social anhedonia, avolition, [diminished] expression of emotion, experience of emotion and self, [diminished] ideational richness, and occupational functioning) on this association. Correlations between premorbid maladjustment and baseline prodromal symptoms in the conversion and nonconversion samples are provided in Table 7 and Table 8, respectively.
Table 7. Conversion sample: Premorbid social and academic maladjustment and severity of prodromal symptoms at baseline.
| Domain and Developmental Period |
Correlations With Premorbid Maladjustment (r) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Unusual Thought Content |
Suspic. | Grandi. Ideas |
Percept. Abnor. |
Disorg. Comm. |
Social Anhed. |
Avolit. | Express. Emot. |
Exper. Emot./ Self |
Ideation. Rich. |
Occup. Funct. |
|
| Social maladjustment | |||||||||||
| Childhood | .15 | <.01 | .12 | .20† | .37*** | .38*** | .21† | −.05 | .23† | .08 | .09 |
| Early adolescence | .08 | .20† | .07 | .17 | .45*** | .40*** | .24* | .16 | .11 | .03 | −.03 |
| Late adolescence | .20 | <−.01 | −.09 | .19 | .37** | .33* | .28* | .28* | .07 | .12 | .14 |
| Academic maladjustment | |||||||||||
| Childhood | .10 | .15 | −.11 | .29* | .17 | .39*** | .10 | .05 | .06 | .27* | .13 |
| Early adolescence | .07 | .13 | −.18 | .20† | −.06 | .30** | .10 | −.05 | −.11 | .19 | .24* |
| Late adolescence | .13 | .03 | −.15 | .09 | −.19 | .19 | −.03 | −.05 | −.15 | .04 | .23† |
Note: The values are Pearson rs. No covariates were used in the analyses.
p ≤ .10.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Table 8. Nonconversion sample: Premorbid social and academic maladjustment and severity of prodromal symptoms at baseline.
| Domain and Developmental Period |
Correlations With Premorbid Maladjustment (r) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Unusual Thought Content |
Suspic. | Grandi. Ideas |
Percept. Abnor. |
Disorg. Comm. |
Social Anhed. |
Avolit. | Express. Emot. |
Exper. Emot./ Self |
Ideation. Rich. |
Occup. Funct. |
|
| Social maladjustment | |||||||||||
| Childhood | .13† | .03 | .09 | .11 | .08 | .20** | .14† | .06 | .10 | .20** | .13† |
| Early adolescence | .01 | .11 | .06 | −.04 | .22** | .49*** | .24** | .24*** | .08 | .19* | .10 |
| Late adolescence | −.07 | .19† | .08 | −.05 | .31** | .56*** | .29** | .31** | .11 | .18† | .20* |
| Academic maladjustment | |||||||||||
| Childhood | .03 | −.11 | .12 | .08 (BLyr) | .12 | .04 | .15† | .06 | −.07 | .07 | .10 (BLeduc) |
| Early adolescence | .09 | .01 | .05 | .10 | .14† | .13† | .24*** | .13† | .08 | .02 | .32*** (BLeduc) |
| Late adolescence | <.01 (sex) | .11 | .11 | .03 (sex, BLyr) | .38*** | .30** | .17† | .17† | .16 | <.01 | .21* (BLeduc) |
Note: The values are Pearson rs, and covariates are in parentheses. BLyr, year of baseline assessment; BLeduc, the number of years of education at baseline; sex, 1 = female, 2 = male.
p ≤ .10.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Mediation effect
To assess mediation effects of each positive and negative prodromal symptom on the association between early adolescent social maladjustment and conversion status, individual Cox regression models were tested in which the prodromal symptom score was entered first followed by the early adolescent social maladjustment rating. Controlling for prodromal symptom severity in this manner, early adolescent social maladjustment continued to predict conversion status over and above the following symptoms (Table 9): unusual thought content (HR = 1.29, p = .021), grandiose ideas (HR = 1.31, p = .013), perceptual abnormalities (HR = 1.31, p = .013), avolition (HR = 1.27, p = .033), experience of emotion and self (HR = 1.27, p = .028), and occupational functioning (HR = 1.27, p = .027). Conversely, early adolescent social maladjustment no longer predicted conversion when accounting for disorganized communication (p = .159), social anhedonia (p = .424), suspiciousness (p = .081), diminished expression of emotion (p = .058), or diminished ideational richness (p = .083). No significant interaction effects between prodromal symptoms and early adolescent social maladjustment were identified.
Table 9. Early adolescent social maladjustment and prediction of conversion to psychosis versus nonconversion, controlling for baseline prodromal symptoms.
| Covariate | Main Effect of Early Adolescent Social Maladjustment | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Parameter Estimates | Overall Fit | |||||||||
|
|
|
|||||||||
| β | SE β | Wald | p | HR (eβ) | 95% CI (eβ) | χ2 | p | |||
| Unusual thought content | 0.25 | 0.11 | 5.34 | .021 | 1.29 | 1.04–1.59 | 9.67 | .008 | ||
| Suspiciousness | 0.20 | 0.11 | 3.05 | .081 | 1.22 | 0.98–1.52 | 17.05 | <.001 | ||
| Grandiose ideas | 0.27 | 0.11 | 6.18 | .013 | 1.31 | 1.06–1.62 | 6.29 | .043 | ||
| Perceptual abnormalities | 0.27 | 0.11 | 6.14 | .013 | 1.31 | 1.06–1.62 | 6.44 | .040 | ||
| Disorganized communication | 0.62 | 0.12 | 1.98 | .159 | 1.18 | 0.94–1.47 | 14.65 | .001 | ||
| Social anhedonia | 0.10 | 0.12 | 0.64 | .424 | 1.10 | 0.87–1.41 | 12.89 | .002 | ||
| Avolition | 0.24 | 0.11 | 4.54 | .033 | 1.27 | 1.02–1.58 | 6.33 | .042 | ||
| Expression of emotion | 0.21 | 0.11 | 3.60 | .058 | 1.24 | 0.99–1.55 | 7.93 | .019 | ||
| Experience of emotion and self | 0.24 | 0.11 | 4.81 | .028 | 1.27 | 1.03–1.58 | 5.68 | .058 | ||
| Ideational richness | 0.20 | 0.11 | 3.01 | .083 | 1.22 | 0.98–1.52 | 16.39 | <.001 | ||
| Occupational functioning | 0.24 | 0.11 | 4.89 | .027 | 1.27 | 1.03–1.58 | 8.04 | .018 | ||
Note: The reference group is nonconversion. A Cox regression analysis was performed using standardized Premorbid Adjustment Scale ratings. The method is forced entry. HR, hazard ratio; CI, confidence interval.
In conjunction with loss of significant association between early adolescent social maladjustment and conversion, evidence of mediation requires significant association between early social maladjustment and the prodromal symptom, and between the prodromal symptom and conversion. As shown in Table 10, linear regression analysis indicated that in the full CHR sample, early adolescent social maladjustment significantly predicted greater baseline severity of disorganized communication (p < .001), social anhedonia (p < .001), suspiciousness (p = .005), diminished expression of emotion (p < .001), and diminished ideational richness (p = .008). Early social maladjustment also was associated with greater severity of avolition at baseline (p < .001). Results for disorganized communication were not altered by excluding sex from the model. Cox regression analyses accounting for early adolescent social maladjustment indicated that disorganized communication (HR = 1.27, p = .004), social anhedonia (HR = 1.20, p = .008), suspiciousness (HR = 1.33, p < .001), and diminished ideational richness (HR = 1.26, p = .002) at baseline each showed a significant effect on conversion status. Diminished expression of emotion did not predict conversion, however (Table 11). Results thus support a significant mediation effect of disorganized communication, social anhedonia, suspiciousness, and diminished ideational richness on the association between early adolescent social maladjustment and conversion to psychosis.
Table 10. Early adolescent social maladjustment and prediction of baseline prodromal symptoms in the full sample.
| Predicted Prodromal Symptom | Main Effect of Early Adolescent Social Maladjustment | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Parameter Estimates | ||||||
|
| ||||||
| β | SE β | t | p | 95% CI (β) | R2 | |
| Unusual thought content | 0.08 | 0.09 | 0.87 | .388 | −0.10–0.27 | <.01 |
| Suspiciousness | 0.26 | 0.09 | 2.82 | .005 | 0.08–0.45 | .03 |
| Grandiose ideas | 0.08 | 0.09 | 0.93 | .353 | −0.09–0.25 | <.01 |
| Perceptual abnormalities | 0.05 | 0.11 | 0.50 | .621 | −0.16–0.26 | <.01 |
| Disorganized communication | 0.43 | 0.09 | 4.84 | <.001 | 0.26–0.61 | .13 |
| Social anhedonia | 0.94 | 0.11 | 8.66 | <.001 | 0.72–1.15 | .23 |
| Avolition | 0.43 | 0.11 | 4.02 | <.001 | 0.22–0.64 | .06 |
| Expression of emotion | 0.37 | 0.10 | 3.78 | <.001 | 0.18–0.56 | .06 |
| Experience of emotion and self | 0.15 | 0.11 | 1.44 | .152 | −0.06–0.36 | .01 |
| Ideational richness | 0.25 | 0.09 | 2.68 | .008 | 0.07–0.44 | .03 |
| Occupational functioning | 0.15 | 0.12 | 1.30 | .194 | −0.08–0.38 | .01 |
Note: Linear regression was performed using standardized Premorbid Adjustment Scale ratings. The method is forced entry. The covariate for disorganized communication was sex; otherwise no covariates were used. CI, confidence interval.
Table 11. Baseline prodromal symptoms and prediction of conversion to psychosis versus nonconversion.
| Predictor | Parameter Estimates | Overall Fit | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| β | SE β | Wald | p | HR (eβ) | 95% CI (eβ) | χ2 | p | |
| Unusual thought content | 0.16 | 0.08 | 3.64 | .056 | 1.17 | 1.00–1.38 | 9.67 | .008 |
| Suspiciousness | 0.29 | 0.09 | 10.96 | .001 | 1.33 | 1.12–1.58 | 17.05 | <.001 |
| Grandiose ideas | −0.04 | 0.09 | 0.19 | .666 | 0.96 | 0.81–1.15 | 6.29 | .043 |
| Perceptual abnormalitiesa | <0.01 | 0.07 | <0.01 | .975 | 1.00 | 0.87–1.15 | 16.43 | .001 |
| Disorganized communication | 0.24 | 0.08 | 8.42 | .004 | 1.27 | 1.08–1.50 | 14.65 | .001 |
| Social anhedonia | 0.19 | 0.07 | 7.07 | .008 | 1.20 | 1.05–1.38 | 12.89 | .002 |
| Avolition | 0.06 | 0.07 | 0.70 | .404 | 1.06 | 0.93–1.22 | 6.33 | .042 |
| Expression of emotion | 0.11 | 0.07 | 2.32 | .128 | 1.12 | 0.97–1.29 | 7.93 | .019 |
| Experience of emotion and self | 0.05 | 0.07 | 0.49 | .483 | 1.05 | 0.92–1.20 | 5.68 | .058 |
| Ideational richness | 0.23 | 0.07 | 9.90 | .002 | 1.26 | 1.09–1.45 | 16.39 | <.001 |
| Occupational functioning | 0.10 | 0.07 | 2.31 | .128 | 1.10 | 0.97–1.26 | 8.04 | .018 |
Note: The reference group is nonconversion. A Cox regression analysis was performed using standardized Premorbid Adjustment Scale ratings. The method is forced entry. The covariate for all analyses was early adolescent social maladjustment, and the year at baseline was an additional covariate for perceptual abnormalities. HR, hazard ratio; CI, confidence interval.
The results for perceptual abnormalities remained nonsignificant when the year at baseline was not included as a covariate.
Combined effect
Finally, we examined positive predictive power and specificity of early adolescent social maladjustment as a unique predictor of conversion status and in conjunction with the prodromal symptoms that independently predicted conversion: suspiciousness, disorganized communication, social anhedonia, and diminished ideational richness. As unique predictors, early adolescent social maladjustment and the four prodromal symptoms all demonstrated modest positive predictive power (range = 40%–51%). Among unique predictors, specificity was good for early adolescent social maladjustment and suspiciousness (71.2% and 75.5%, respectively) and modest for the other three. The combination of premorbid early adolescent social maladjustment and baseline suspiciousness predicted conversion with the highest positive predictive power (59%) and specificity (92.1%) of all unique and combined predictors. The association and prediction statistics for early adolescent social maladjustment, suspiciousness, disorganized communication, social anhedonia, and diminished ideational richness as unique predictors, and for early adolescent social maladjustment in combination with each of the four prodromal symptoms, are presented in Table 12.
Table 12. Association and predictive statistics for unique predictors and combined effects.
| Convrt/ Total (n) |
HR (95% CI) | p | LR+ | LR− | PPP (%) |
NPP (%) |
Sensit (%) |
Specif (%) |
|
|---|---|---|---|---|---|---|---|---|---|
| Early adolescent social maladjustment (>2) | 74/251 | 2.02 (1.28–3.18) | .003 | 1.74 | 0.70 | 46 | 72 | 50.0 | 71.2 |
| Suspiciousness (>3) | 78/270 | 2.51 (1.61–3.91) | <.001 | 2.15 | 0.63 | 51 | 75 | 52.6 | 75.5 |
| Disorganized communication (>1) | 78/270 | 1.89 (1.15–3.09) | .012 | 1.32 | 0.62 | 40 | 76 | 71.8 | 45.8 |
| Social anhedonia (>2) | 77/268 | 2.42 (1.49–3.92) | <.001 | 1.64 | 0.54 | 46 | 80 | 68.8 | 58.1 |
| Ideational richness (>0) | 77/266 | 2.36 (1.45–3.82) | .001 | 1.57 | 0.56 | 45 | 78 | 68.8 | 56.1 |
| Early social maladjustment + suspiciousness | 74/251 | 2.81 (1.69–4.66) | <.001 | 3.59 | 0.77 | 59 | 70 | 28.4 | 92.1 |
| Early social maladjustment + disorganized communication | 74/251 | 2.42 (1.52–3.85) | <.001 | 2.31 | 0.71 | 51 | 72 | 41.9 | 81.9 |
| Early social maladjustment + social anhedonia | 73/249 | 2.11 (1.32–3.35) | .002 | 1.97 | 0.73 | 49 | 72 | 42.5 | 78.4 |
| Early social maladjustment + ideational richness | 73/247 | 2.07 (1.26–3.40) | .004 | 2.03 | 0.81 | 50 | 70 | 31.5 | 84.5 |
Note: The reference group is nonconversion. The values in parentheses indicate the lowest threshold for positive test (positive test = 1, negative test = 0). Convrt, conversion sample size; Total, total sample size; HR, hazard ratio from Cox regression analysis; LR+, positive likelihood ratio (sensitivity/1-specificity); LR−, negative likelihood ratio (1-sensitivity/specificity); PPP, positive predictive power; NPP, negative predictive power; Sensit, sensitivity; Specif, specificity.
Discussion
This is the first study to examine the association between developmental course of social, academic, and total maladjustment and conversion to psychosis in a CHR sample. Specific findings are as follows:
Early adolescent social dysfunction is a significant predictor of conversion to psychosis over and above childhood social maladjustment and independent of the baseline severity of most positive and negative prodromal symptoms.
Disorganized communication, social anhedonia, suspiciousness, and diminished ideational richness provide the strongest evidence of a mediation effect on the association between early adolescent social functioning and conversion status.
Early adolescent social maladjustment in conjunction with baseline suspiciousness demonstrates high positive predictive power and high specificity in predicting conversion to psychosis.
Deterioration of academic and total functioning is observed in this CHR sample, but neither domain predicts conversion to psychosis at any developmental period.
Prediction of conversion to psychosis
Social maladjustment
The current results argue that timing and type (domain) of premorbid functional decline have important prognostic implications for conversion to psychosis in CHR samples, especially social maladjustment in early adolescence. As illustrated in Figure 1, conversion and nonconversion groups reported equivalent social adjustment in childhood. However, individuals who converted to psychosis reported a marked increase in social dysfunction during early adolescence compared to nonconverters. As such, early adolescent social maladjustment was a significant, albeit modest, predictor of conversion status independent of childhood maladjustment (HR range = 1.25–1.33). This is consistent with Dragt et al's (2011) recent examination of individual childhood and early adolescent items on the PAS indicating that “sociability and withdrawal” and “social–sexual aspects” in early adolescence, but not in childhood, significantly predicted conversion in a high-risk sample.
In contrast, nonconverters showed a gradual worsening of social dysfunction across developmental periods, which approached that of converters only by late adolescence. Consequently, social dysfunction associated with entering late adolescence was not a significant predictor of conversion status. The reduced effect of early adolescence with the addition of late adolescence into the developmental model likely reflects the strong positive correlation between early and late adolescent social functioning and perhaps loss of power associated with the smaller size of the restricted sample and the increased complexity of the model.
Role of prodromal symptoms
As described above, poor functioning at baseline (Cornblatt et al., 2007) was previously shown to be a sensitive predictor of conversion to psychosis independent of baseline clinical state in NAPLS-I (Cannon, 2008; Cornblatt et al., 2011) and other CHR samples (Dragt et al., 2011; Mason et al., 2004; Ruhrmann et al., 2010; Thompson et al., 2011; Velthorst et al., 2009; Yung et al., 2003, 2004). Consistent with these reports, examination of social dysfunction prior to baseline indicated that early adolescent social maladjustment predicted conversion to psychosis independent of the majority of positive and negative prodromal symptoms assessed on the SIPS (HR range = 1.10–1.31). Furthermore, early adolescent social maladjustment predicted greater severity of several baseline prodromal symptoms, four of which in turn predicted conversion to psychosis: suspiciousness, disorganized communication, social anhedonia, and diminished ideational richness. These results fit well with the substantial evidence that poor premorbid social adjustment predicts greater symptom severity at first psychotic episode, particularly negative symptoms, and predicts worse illness course and functional outcome among schizophrenia patients (Larsen et al., 2004; Piskulic et al., 2011; Strous et al., 2004). This apparent association over time among premorbid social maladjustment, prodromal symptoms, conversion to psychosis, and illness severity and outcome supports a durable effect of social functioning and is congruent with a developmental conceptualization of schizophrenia and other psychotic disorders.
Identification of developmentally informative markers of psychosis risk is an important step in improving power and specificity of multivariate prediction models. Although not entirely independent of premorbid adjustment, variation in magnitude of mediation contributed by prodromal symptoms of suspiciousness, disorganized communication, social anhedonia, and diminished ideational richness suggests unique sensitivity to developmental pathology of psychotic disorders that, in conjunction with early adolescent social maladjustment, may enhance prediction of psychosis. In the current study, the combination of early adolescent social dysfunction and baseline suspiciousness provided the strongest predictive effect on conversion status (HR = 2.81) and produced the greatest elevation in positive predictive power (59%) and specificity (92.1%) to psychosis conversion compared to social maladjustment alone. Of note, suspiciousness is also observed in relatives of schizophrenia patients, which is consistent with an association between suspiciousness and liability to schizophrenia (although contribution of genes versus shared environment is unclear; Ingraham, 1995; Katsanis, Iacono, & Beiser, 1990; Tarbox, Almasy, Gur, Nimgaonkar, & Pogue-Geile, 2012).
Social dysfunction in early adolescence thus appears to be a critical prognostic indicator of conversion to psychosis among CHR individuals. Furthermore, results are consistent with the idea that premorbid social maladjustment may be an early manifestation of pathological developmental process(es), later signs of which would include prodromal symptoms (e.g., suspiciousness) and eventual psychosis. If so, early adolescence may be a time of heightened neurodevelopmental vulnerability and, correspondingly, a time during which the brain could be particularly responsive to psychosocial and/or pharmacological intervention. Even without a clear neurodevelopmental connection, evidence suggests a strong need for treatments that target functional deficits, and given current findings, interventions targeting social dysfunction would be particularly important. Psychosocial treatments that target social cognitive deficits and poor interpersonal skills have already shown positive results in both recent-onset and chronic schizophrenia patients (e.g., Bellack, Mueser, Gingerich, & Agresta, 2004; Eack, Pogue-Geile, Greenwald, Hogarty, & Keshavan, 2010; Hogarty et al., 2004; Marder et al., 1996; Roberts & Penn, 2009).
Academic and total maladjustment
Similar to social functioning, academic adjustment showed a pattern of deterioration from childhood to early adolescence in this CHR sample, and in adolescence, ratings for academic maladjustment were generally higher (more pathological) than those for social maladjustment, a finding also reported in patient samples (Allen, Frantom, Strauss, & van Kammen, 2005; Monte, Goulding, & Compton, 2008). However, the conversion and nonconversion groups did not differ in severity of academic maladjustment at any developmental period. This is consistent with a prior report that PAS academic items were not associated with psychosis in the Dutch Prediction of Psychosis Study (Dragt et al., 2011). These results suggest that deterioration in academic functioning does not predict conversion to psychosis among CHR individuals. 2
Likewise, deterioration in total adjustment was present in both the conversion and the nonconversion groups, but it did not predict psychosis. Given the notable differences between premorbid social and academic maladjustment, it is possible that sensitivity of “total” maladjustment to conversion outcome may be limited by heterogeneity across these two domains of functioning. Overall, current results indicate that social maladjustment would be a better choice for inclusion in prediction algorithms than would either total or academic maladjustment.
Limitations
The decision to examine conversion to psychosis, rather than conversion to a specific psychotic disorder (e.g., schizophrenia), is common in this area of research. However, potential limitations of using a broader and perhaps more heterogeneous conversion group should be acknowledged. To the extent that psychotic disorders differ in premorbid maladjustment, conversion and nonconversion group differences would tend to be underestimated, making it more difficult to predict conversion to psychosis. If such heterogeneity is a factor, our results may underestimate the sensitivity of premorbid maladjustment to predict conversion. In addition, combining multiple psychotic disorders makes it impossible to compare specific disorders on severity and developmental trajectory of premorbid maladjustment. For example, current evidence is mixed regarding the extent of premorbid dysfunction in psychotic mood disorders and whether poor premorbid functioning is inherent in all “schizophrenia-spectrum” diagnoses or only in schizophrenia. If this were the case here, then results could principally reflect functioning in the subsample of participants who converted to schizophrenia.
Regarding the assessment of premorbid functioning, a frequently cited limitation of the PAS (Cannon-Spoor et al., 1982) is its retrospective design, although predictive and concurrent validity have been established (Brill et al., 2008). Use in CHR samples has the advantage of assessing individuals who are close in age to the developmental periods of interest and who are not psychotic, two principal sources of recall bias on the PAS. A related limitation is that, by design, PAS ratings for each age period are made during the same interview. This could influence participant recall, possibly inflating similarities across age periods. If so, the magnitude of change in functioning across developmental periods could be underestimated in this study. Finally, administration instructions for the PAS indicate that maladjustment ratings are to be obtained for the developmental periods up to and excluding onset of psychosis. However, use in CHR samples raises the issue of potential overlap between “premorbid” maladjustment and concurrent “prodromal” symptoms, a distinction not clearly established when the PAS was published. Such an overlap could potentially inflate maladjustment ratings for that developmental period. In the current subsample for which age of prodromal symptom onset was available, 70% of converters reported symptom onset after age 16 versus 39% of nonconverters. In the context of current results, inflation of nonconverters' maladjustment ratings during early adolescence is not a strong concern.
Conclusion
The results of this study argue that severity of premorbid social dysfunction in early adolescence is a significant predictor of conversion to psychosis among CHR youths, independent of childhood social maladjustment and most baseline prodromal symptoms. Results are consistent with the idea that premorbid social maladjustment is an important early manifestation of developmental pathophysiology of psychotic disorders. Based on the current findings, early adolescent social maladjustment may be a particularly good candidate for inclusion in prediction algorithms and could be an important target for early intervention.
Acknowledgments
This work was supported by National Institute of Mental Health (U01 MH066134 to J.A., R01 MH060720 and K24 MH76191 to K.S.C., R01 MH065079 to T.D.C., R01 MH061523 to B.A.C., U01 MH066069 and P50 MH064065 to D.O.P, R01 MH065562 and P50 MH080272 to L.J.S., R21 MH075027 to M.T.T, R01 MH062066 to E.F.W., K05 MH01654 to T.H.M., and U01 MH066160 to S.W.W.), the Donaghue Foundation (to S.W.W.), and Eli Lilly and Co. (study HGGF to T.H.M., J.A., D.O.P.).
Footnotes
Role functioning includes occupational, educational, and homemaker roles. Academic functioning refers only to the education setting.
Note that academic maladjustment as assessed on the PAS is not a measure of cognitive ability per se, but rather a gauge of adaptation to the school environment. There is evidence that neuropsychological deficits are sensitive to conversion among CHR individuals (Mason et al., 2004; Pukrop et al., 2007; Seidman et al., 2010).
References
- Addington J, van Mastrigt S. Patterns of premorbid functioning in first episode psychosis: Relationship to 2-year outcome. Acta Psychiatrica Scandinavica. 2005;112:40–46. doi: 10.1111/j.1600-0447.2005.00511.x. [DOI] [PubMed] [Google Scholar]
- Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, et al. North American Prodrome Longitudinal Study: A collaborative multisite approach to prodromal schizophrenia research. Schizophrenia Bulletin. 2007;33:665–672. doi: 10.1093/schbul/sbl075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Cornblatt B, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, et al. At clinical high risk for psychosis: Outcome for nonconverters. American Journal of Psychiatry. 2011;168:800–805. doi: 10.1176/appi.ajp.2011.10081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophrenia Research. 2008;99:119–124. doi: 10.1016/j.schres.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, van Mastrigt S, Addington D. Patterns of premorbid functioning in first-episode psychosis: Initial presentation. Schizophrenia Research. 2003;62:23–30. doi: 10.1016/s0920-9964(02)00408-5. [DOI] [PubMed] [Google Scholar]
- Allen DN, Frantom LV, Strauss GP, van Kammen DP. Differential patterns of premorbid academic and social deterioration in patients with schizophrenia. Schizophrenia Research. 2005;75:389–397. doi: 10.1016/j.schres.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Mueser KT, Gingerich S, Agresta J. Social skills training for schizophrenia: A step-by-step guide. New York: Guilford Press; 2004. [Google Scholar]
- Brill N, Reichenberg A, Weiser M, Rabinowicz J. Validity of the Premorbid Adjustment Scale. Schizophrenia Bulletin. 2008;34:981–983. doi: 10.1093/schbul/sbm128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: A multisite longitudinal study in North America. Archives of General Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon-Spoor H, Potkin S, Wyatt R. Measurement of premorbid adjustment in chronic schizophrenia. Schizophrenia Bulletin. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- Carr V, Halpin S, Lau N, O'Brien S, Beckmann J, Lewin T. A risk factor screening and assessment protocol for schizophrenia and related psychosis. Australian and New Zealand Journal of Psychiatry. 2000;34:170–180. doi: 10.1080/000486700240. [DOI] [PubMed] [Google Scholar]
- Corcoran CM, Kimhy D, Parrilla-Escobar MA, Cressman VL, Stanford AD, Thompson J, et al. The relationship of social function to depressive and negative symptoms in individuals at clinical high risk for psychosis. Psychological Medicine. 2011;41:251–261. doi: 10.1017/S0033291710000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Auther AM, Neidham T, Smith CW, Zinberg J, Bearden CE, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophrenia Bulletin. 2007;33:688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Carrion RE, Addington J, Seidman L, Walker EF, Cannon TD, et al. Risk factors for psychosis: Impaired social and role functioning. Schizophrenia Bulletin. 2011 doi: 10.1093/schbul/sbr136. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragt S, Nieman DH, Veltman D, Becker HE, van de Fliert R, de Haan L, et al. Environmental factors and social adjustment as predictors of a first psychosis in subjects at ultra high risk. Schizophrenia Research. 2011;125:69–76. doi: 10.1016/j.schres.2010.09.007. [DOI] [PubMed] [Google Scholar]
- Eack SM, Pogue-Geile MF, Greenwald DP, Hogarty SS, Keshavan MS. Mechanisms of functional improvement in a 2-year trial of cognitive enhancement therapy for early schizophrenia. Psychological Medicine. 2010:1–9. doi: 10.1017/S0033291710001765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I disorders, patient edition (SCID-I/P Version 2.0) New York: New York State Psychiatric Institute, Biometrics Research Department; 1995. [Google Scholar]
- Haas GL, Sweeney JA. Premorbid and onset features of firstepisode schizophrenia. Schizophrenia Bulletin. 1992;16:373–386. doi: 10.1093/schbul/18.3.373. [DOI] [PubMed] [Google Scholar]
- Haim R, Rabinowitz J, Bromet E. The relationship of premorbid functioning to illness course in schizophrenia and psychotic mood disorders during two years following first hospitalization. Journal of Nervous and Mental Disease. 2006;194:791–795. doi: 10.1097/01.nmd.0000240158.39929.e3. [DOI] [PubMed] [Google Scholar]
- Hawkins KA, McGlashan TH, Quinlan D, Miller TJ, Perkins DO, Zipursky RB, et al. Factorial structure of the Scale of Prodromal Symptoms. Schizophreia Research. 2004;68:339–347. doi: 10.1016/S0920-9964(03)00053-7. [DOI] [PubMed] [Google Scholar]
- Hogarty GE, Flesher S, Ulrich R, Carter M, Greenwald D, Pogue-Geile MF, et al. Cognitive enhancement therapy for schizophrenia: Effects of a 2-year randomized trial on cognition and behavior. Archives of General Psychiatry. 2004;61:866–876. doi: 10.1001/archpsyc.61.9.866. [DOI] [PubMed] [Google Scholar]
- Ingraham LJ. Family-genetic research and schizotypal personality. In: Raine A, Lencz T, Mednick SA, editors. Schizotypal personality. Cambridge: Cambridge University Press; 1995. pp. 19–42. [Google Scholar]
- Katsanis J, Iacono W, Beiser M. Anhedonia and perceptual aberration in first-episode psychotic patients and their relatives. Journal of Abnormal Psychology. 1990;99:202–206. doi: 10.1037//0021-843x.99.2.202. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Dementia praecox and paraphrenia. Huntington, NY: Krieger; 1919. [Google Scholar]
- Larsen JK, Friis S, Haahr U, Johannessen JO, Melle I, Opjordsmoen SR, et al. Premorbid adjustment in first-episode non-affective psychosis: Distinct patterns of pre-onset course. British Journal of Psychiatry. 2004;185:108–115. doi: 10.1192/bjp.185.2.108. [DOI] [PubMed] [Google Scholar]
- Larsen TK, McGlashan TH, Johannessen JO, Vibe-Hansen L. First-episode schizophrenia: II. Premorbid patterns by gender. Schizophrenia Bulletin. 1996;22:257–269. doi: 10.1093/schbul/22.2.257. [DOI] [PubMed] [Google Scholar]
- Lemos S, Vallina O, Fernandez P, Ortega JA, Garcia P, Gutierrez A, et al. Predictive validity of the Scale of Prodromal Symptoms (SOPS) Actas Espanolas De Psiquiatria. 2006;34:216–223. [PubMed] [Google Scholar]
- Lencz T, Smith CW, Auther A, Correll CU, Cornblatt B. Nonspecific and attenuated negative symptoms in patients at clinical high-risk for schizophrenia. Schizophrenia Research. 2004;68:37–48. doi: 10.1016/S0920-9964(03)00214-7. [DOI] [PubMed] [Google Scholar]
- Levitt JJ, O'Donnell BF, McCarley RW, Nestor PG, Shenton ME. Correlations of premorbid adjustment in schizophrenia with auditory event-related potential and neuropsychological abnormalities. American Journal of Psychiatry. 1996;153:1347–1349. doi: 10.1176/ajp.153.10.1347. [DOI] [PubMed] [Google Scholar]
- MacBeth A, Gumley A. Premorbid adjustment, symptom development and quality of life in first episode psychosis: A systematic review and critical reappraisal. Acta Psychiatrica Scandinavica. 2008;117:85–99. doi: 10.1111/j.1600-0447.2007.01134.x. [DOI] [PubMed] [Google Scholar]
- Marder SR, Wirshing WC, Mintz J, McKenzie J, Johnston K, Eckman TA, et al. Two-year outcome of social skills training and group psychotherapy for outpatients with schizophrenia. American Journal of Psychiatry. 1996;153:1585–1592. doi: 10.1176/ajp.153.12.1585. [DOI] [PubMed] [Google Scholar]
- Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with “at-risk mental states. Schizophrenia Research. 2004;71:227–237. doi: 10.1016/j.schres.2004.04.006. [DOI] [PubMed] [Google Scholar]
- McGlashan T, Walsh B, Woods SW. The psychosis-risk syndrome: Handbook for diagnosis and follow-up. New York: Oxford University Press; 2010. [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the Scale of Prodromal Symptoms: Predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: Preliminary evidence of interrater reliability and predictive validity. American Journal of Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- Monte RC, Goulding SM, Compton MT. Premorbid functioning of patients with first-episode nonaffective psychosis: A comparison of deterioration in academic and social performance, and clinical correlates of Premorbid Adjustment Scale scores. Schizophrenia Research. 2008;104:206–213. doi: 10.1016/j.schres.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RMG, Malla AK, Manchanda R, Townsend L. Premorbid adjustment in first episode schizophrenia and schizoaffective disorders: A comparison of social and academic domains. Acta Psychiatrica Scandinavica. 2005;112:30–39. doi: 10.1111/j.1600-0447.2005.00555.x. [DOI] [PubMed] [Google Scholar]
- Picchioni MM, Walshe M, Toulopoulou T, McDonald C, Taylor M, Waters-Metenier S, et al. Genetic modeling of childhood social development and personality in twins and siblings with schizophrenia. Psychological Medicine. 2010;40:1305–1316. doi: 10.1017/S0033291709991425. [DOI] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, Perkins DO, Graham KA, Siegel M. Emotion perception and social skill over the course of psychosis: A comparison of individuals “at-risk” for psychosis and individuals with early and chronic schizophrenia spectrum illness. Cognitive Neuropsychiatry. 2007;12:198–212. doi: 10.1080/13546800600985557. [DOI] [PubMed] [Google Scholar]
- Piskulic D, Addington J, Auther A, Cornblatt BA. Using the global functioning social and role scales in a first-episode sample. Early Intervention Psychiatry. 2011;5:219–223. doi: 10.1111/j.1751-7893.2011.00263.x. [DOI] [PubMed] [Google Scholar]
- Pukrop R, Ruhrmann S, Schultze-Lutter F, Bechdolf A, Brockhaus-Dumke A, Klosterkotter J. Neurocognitive indicators for a conversion to psychosis: Comparison of patients in a potentially initial prodromal state who did or did not convert to a psychosis. Schizophrenia Research. 2007;92:116–125. doi: 10.1016/j.schres.2007.01.020. [DOI] [PubMed] [Google Scholar]
- Roberts DL, Penn DL. Social cognition and interaction training (SCIT) for outpatients with schizophrenia: A preliminary study. Psychiatry Research. 2009;166:141–147. doi: 10.1016/j.psychres.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Ruhrmann S, Schultze-Lutter F, Salokangas RKR, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: Results from the Prospective European Prediction of Psychosis Study. Archives of General Psychiatry. 2010;67:241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- Rund BR, Melle I, Friis S, Johannessen JO, Larsen TK, Midboe LJ, et al. The course of neurocognitive functioning in first-episode psychosis and its relation to premorbid adjustment, duration of untreated psychosis, and relapse. Schizophrenia Research. 2007;91:132–140. doi: 10.1016/j.schres.2006.11.030. [DOI] [PubMed] [Google Scholar]
- Seidman LJ, Giuliano AJ, Meyer EC, Addington J, Cadenhead KC, Cannon TD, et al. Neuropsychology of the prodrome to psychosis in the NAPLS consortium. Archives of General Psychiatry. 2010;67:578–588. doi: 10.1001/archgenpsychiatry.2010.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro DI, Marenco S, Spoor EH, Egan MF, Weinberger DR, Gold JM. The Premorbid Adjustment Scale as a measure of developmental compromise in patients with schizophrenia and their healthy siblings. Schizophrenia Research. 2009;112:136–142. doi: 10.1016/j.schres.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein ML, Mavrolefteros G, Turnbull A. Premorbid factors in relation to motor, memory, and executive functions deficits in adult schizophrenia. Schizophrenia Research. 2003;61:271–280. doi: 10.1016/s0920-9964(02)00312-2. [DOI] [PubMed] [Google Scholar]
- Strous RD, Alvir JMJ, Robinson D, Gal G, Sheitman B, Chakos M, et al. Premorbid functioning in schizophrenia: Relation to baseline symptoms, treatment response, and medication side effects. Schizophrenia Bulletin. 2004;30:265–278. doi: 10.1093/oxfordjournals.schbul.a007077. [DOI] [PubMed] [Google Scholar]
- Tarbox SI, Almasy L, Gur RE, Nimgaonkar VL, Pogue-Geile MF. The nature of schizotypy among multigenerational multiplex schizophrenia families. Journal of Abnormal Psychology. 2012 doi: 10.1037/a0026787. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarbox SI, Brown LH, Haas GL. Premorbid adjustment in affective and non-affective psychosis: A first episode study. Schizophrenia Bulletin. 2011;37(suppl):21–22. [Google Scholar]
- Tarbox SI, Pogue-Geile MF. Social functioning in pre-schizophrenia children and adolescents: A systematic review. Psychological Bulletin. 2008;34:561–583. doi: 10.1037/0033-2909.34.4.561. [DOI] [PubMed] [Google Scholar]
- Thompson A, Nelson B, Yung A. Predictive validity of clinical variables in the “at risk” for psychosis population: International comparison with results from the North American Prodrome Longitudinal Study. Schizophrenia Research. 2011;126:51–57. doi: 10.1016/j.schres.2010.09.024. [DOI] [PubMed] [Google Scholar]
- Van Mastrigt S, Addington J. Assessment of premorbid function in first-episode schizophrenia: Modifications to the Premorbid Adjustment Scale. Journal of Psychiatry and Neuroscience. 2002;27:92–101. [PMC free article] [PubMed] [Google Scholar]
- Velthorst E, Nieman DH, Becker HE, van de Fliert R, Dingemans PM, Klaassen R, et al. Baseline differences in clinical symptomatology between ultra high risk subjects with and without a transition to psychosis. Schizophrenia Research. 2009;109:60–65. doi: 10.1016/j.schres.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Walshe M, Taylor M, Schulze K, Bramon E, Frangou S, Stahl D, et al. Familial liability to schizophrenia and premorbid adjustment. British Journal of Psychiatry. 2007;191:260–261. doi: 10.1192/bjp.bp.106.033688. [DOI] [PubMed] [Google Scholar]
- Woods SW, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Validity of the prodromal risk syndrome for first psychosis: Findings from the North American Prodrome Longitudinal Study. Schizophrenia Bulletin. 2009;35:894–908. doi: 10.1093/schbul/sbp027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A. Monitoring and care of young people at incipient risk of psychosis. Schizophrenia Bulletin. 1996;22:283–303. doi: 10.1093/schbul/22.2.283. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophrenia Research. 2003;60:21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: Psychopathology and clinical features. Schizophrenia Research. 2004;67:131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Coryell W. The reliability of personality disorder diagnoses in a non-patient sample. Journal of Personality Disorders. 1989;3:53–57. [Google Scholar]


