Abstract
While Internet interventions can improve health behaviors, their impact is limited by program adherence. Supporting program adherence through telephone counseling may be useful, but there have been few direct tests of the impact of support. We describe a Telephone Motivational Interviewing (MI) intervention targeting adherence to an Internet intervention for drivers with Type 1 Diabetes, DD.com, and compare completion of intervention benchmarks by those randomized to DD.com plus MI vs. DD.com only. The goal of the pre-intervention MI session was to increase the participant's motivation to complete the Internet intervention and all its assignments, while the goal of the post-treatment MI session was to plan for maintaining changes made during the intervention. Sessions were semi-structured and partially scripted to maximize consistency. MI Fidelity was coded using a standard coding system, the MITI. We examined the effects of MI support vs. no support on number of days from enrollment to program benchmarks. Results show that MI sessions were provided with good fidelity. Users who received MI support completed some program benchmarks such as Core 4 (t176 df= -2.25; p<.03) and 11 of 12 monthly driving diaries significantly sooner, but support did not significantly affect time to intervention completion (t177 df= -1.69; p<. 10) or rates of completion. These data suggest that there is little benefit to therapist guidance for Internet interventions including automated email prompts and other automated minimal supports, but that a booster MI session may enhance collection of follow-up data.
1. Introduction
Internet interventions are increasingly used to improve health behaviors to manage chronic illness, but their efficacy is limited by patient adherence to the program. Many participants never complete a health-behavior focused Internet intervention, limiting the potential impact (Blankers, Koeter, & Schippers, 2009; Christensen et al., 2009; Christensen, Griffiths, & Farrer, 2009; Ritterband et al., 2008). Characteristics of Internet interventions that seem to foster more program adherence include highly relevant content, tailored interactivity, and personalization of feedback and user assignments (Ritterband, Thorndike, Cox, Kovatchev, & Gonder-Frederick, 2009). A systematic review of the technology features of web-based programs in health revealed that the presence of specific technology strategies, including primary task support, dialogue support, more frequent intended usage, and more frequent contact with a counselor and more frequent reminders explain more than half of the variance in adherence to the program (Kelders, Kok, Ossebaard, & Van Gemert-Pijnen, 2012). However, even with such features, users may require additional strategies to increase their motivation to engage in, and fully utilize, Internet interventions.
Some developers of Internet interventions assert that therapist support such as weekly email or telephone calls providing guidance might be required to improve patient outcomes via better usage and completion of the Internet intervention, while unguided self-help interventions are appropriate as population-level preventive interventions (Andersson & Carlbring, 2011). In contrast to this view, meta-analyses have found that some unguided Internet interventions are efficacious, even in the areas of mental health (Christensen et al., 2009) and alcohol problems (Riper et al., 2014). However, there have been just a few direct tests of the impact of therapist Support or guidance on program use, completion, or provision of follow-up data. In an Internet intervention for social anxiety, researchers found that the impact of therapist guided vs. unguided interventions varied by a set of patient characteristics and that some patients benefitted from Internet interventions without therapist support (Nordgreen et al., 2012). Currently, investigators are comparing a therapist guided vs. unguided mobile and Internet combination Cognitive Behavioral Therapy (CBT) intervention for social anxiety and panic disorder; this trial is ongoing and results are not yet available (Lindner, Ivanova, Ly, Andersson, & Carlbring, 2013). Unfortunately, we could not find any tests of therapist support to enhance program adherence in the area of diabetes. Therefore, it is unknown whether the emerging information about unguided mental health interventions applies to diabetes interventions.
When therapist support is provided, it is often based on CBT, but in general, focuses on the behavioral target, such as depression. When targeting program completion however, there is a need to increase motivation to use programs and persist until completion. In these cases, it may be appropriate to use the counseling style of Motivational Interviewing (MI). MI facilitates behavior change for many health behaviors beyond its foundation in treating drinking problems, including alcohol and drug use, medication adherence, uptake of exercise, and others when delivered as 1-4 sessions of 15 minutes or more (Hettema, Steele, & Miller, 2005; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010; Rubak, Sandbaek, Lauritzen, & Christensen, 2005). MI sessions include processes of Engaging, Focusing, Evoking, and Planning, culminating in behavior change that is freely chosen by the patient (Miller & Rollnick, 2012). MI has a large evidence base, and several meta-analyses have shown that it has a small to moderate effect size, similar to other psychotherapies (Burke, Arkowitz, & Menchola, 2003; Heckman, Egleston, & Hofmann, 2010; Hettema et al., 2005; Hettema & Hendricks, 2010; Lundahl et al., 2010; Rubak et al., 2005; Smedslund et al., 2011; Vasilaki, Hosier, & Cox, 2006). MI has been tested in a number of studies as a prelude to enhance adherence to a primary intervention, and has been found to improve session attendance and outcomes (Carroll et al., 2006; Coyne & Correnti, 2014; Martino, 2011; Miller & Rollnick, 2012).
MI is promising when delivered over the telephone for 1-2 sessions (Aharonovich et al., 2012; Bennett, Young, Nail, Winters-Stone, & Hanson, 2008; Cook, McCabe, Emiliozzi, & Pointer, 2009; Farrell-Carnahan et al., 2013; Walker, Roffman, Picciano, & Stephens, 2007). Telephone delivery is important in Internet-delivered interventions, because participants from wide geographic areas may enroll, making face to face sessions impractical if not impossible. We hypothesized that MI might improve usage of an Internet program, and could lead to improved completion of the program, or of follow-up assessments.
The purposes of this paper are 1) to describe a Telephone Motivational Interviewing (MI) therapist support intervention targeting completion of an Internet intervention for drivers with Type 1 Diabetes, DD.com, and 2) to compare program utilization by those randomized to Internet intervention plus MI vs. those randomized to the Internet intervention alone.
2. Methods
2.1. Internet intervention
DiabetesDriving.com (DD.com) is an interactive Internet intervention program for high risk drivers with Type 1 Diabetes Mellitus (T1DM) targeting behaviors related to the risk of future collisions. Specifically, DD.com guides users to improve the prevention, detection, and treatment of hypoglycemia while driving. DD.com can be completed in 5 weeks, and has automated prompting to complete various tasks sent by email to users. The initial two Cores explain how to use the program (Core 0) and how to use a driver's toolkit that was mailed to participants (Core 1). The subsequent Cores (Cores 2-5) are content-based and are metered out at a rate of one per week. All cores took approximately 30 minutes to complete, and were organized in a similar manner: Participants reviewed the previous week's homework; then interacted with new Core content, including reviewing videos and case reports and completing checklists and questionnaires. Participants then completed a “self-test” on new content, which was a multiple choice quiz that provided feedback on the correct answer following answering each item. Each Core concluded with users identifying activities they wanted to complete. Beginning after Core 2, users completed daily progress notes to monitor new behaviors introduced in the Cores. The program tracked when users started and completed each Core, along with their utilization and completion of interactive elements. Specific contents of each Core, and required tasks associated with each Core are shown in Table 1. A U.S. randomized clinical trial tested DD.com alone compared to DD.com plus 2 MI sessions, and to treatment as usual, and found that the intervention reduced driving mishaps significantly (Cox et al., 2014). In this report, we focus only on the two conditions receiving DD.com.
Table 1. DD.com Core Contents.
| Core 0 Introduction |
| How to Use the Internet Intervention |
| Core 1 Tool Kit |
| Orientation to study tool kit for car |
Tool kit included:
|
| Self-test and closing |
| Core 2 Driving Risks |
| Review of general and diabetes-specific driving risk factors |
| Develop a plan to reduce risk of future driving mishaps |
| Learn what to expect in upcoming Cores |
| Preliminary Driving Contract |
| Core 3 Preventing Hypoglycemia |
| Anticipating and preventing extreme BG while driving |
| Review of Tool Kit |
| Daily Progress Notes |
| Learn to anticipate low BG |
| Learn to prevent hypoglycemia during a drive |
| Revised Driving Contract |
| Daily automated e-mails asking them to record findings from their diary |
| Core 4 Detecting and Treating Hypoglycemia while Driving |
| Improving detection and management of extreme BG while driving |
| Using Tool Kit |
| Using Driving Diaries |
| Review Core 3 Driving Contract |
| Learn to detect hypoglycemia |
| Learn to manage hypoglycemia for immediate and long term benefits |
| Revise Contract to detect and manage hypoglycemia while driving |
| Completion of personally relevant diaries after each drive |
| Daily e-mail reminders to upload driving data |
| Core 5 Review, Reflect, and Relapse Prevention |
| Review and summarize progress |
| Maintaining safe long-term driving habits. |
| Anticipating barriers and designing solutions for barriers |
2.2. Procedures
The study was approved by the University of Virginia Institutional Review Board for Health Sciences Research. Individuals came to the DiabetesDriving.com website and read about the study, described as a trial of an Internet intervention designed to reduce driving mishaps among those with T1DM, versus usual care, or versus the Internet intervention plus 2 telephone counseling sessions. Interested individuals signed an online consent form agreeing to provide screening information over the Internet, and completed a screening questionnaire between March 2012 and June, 2013. We contacted those who met the inclusion criteria and scheduled a telephone appointment, during which we reviewed their inclusion/exclusion criteria and provided further details about the study. After this telephone interview, interested eligible participants signed a second consent form to participate in the randomized trial. Participants were randomized to one of three conditions, Routine Care (RC), DiabetesDriving.com (DD.com only) or DD.com plus Motivational Interview (DD.com plus MI). Routine Care participants served as the control group and did not receive any intervention content. All study participants continued with their routine diabetes care throughout the study.
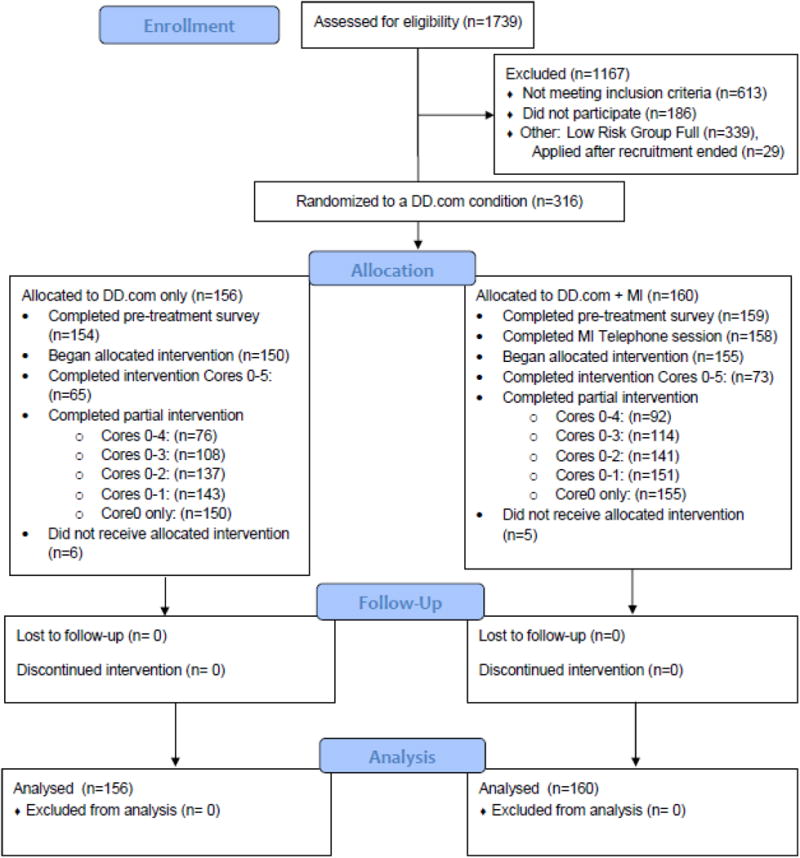
Those assigned to the DD.com plus MI group were scheduled for an MI session on the telephone during the enrollment call, and MI appointments were scheduled to occur within a week of enrollment. Consenting individuals were sent a URL by email that gave them access to a baseline questionnaire. After completing this questionnaire, DD.com only participants received access to the program immediately, while DD.com+MI participants received access after completing the questionnaire and the telephone MI session. Participants were told that they had 10 weeks (70 days) to complete DD.com. After 70 days, whether or not they had completed DD.com, those assigned to DD.com plus MI completed a second MI telephone session. At 70 days, all participants completed an online post-treatment questionnaire, and subsequently completed monthly driving diaries prompted by automated emails for the following year. Monthly driving diaries provided the information on driving mishaps that will serve as primary outcomes in the RCT. Figure 1 depicts the flow of the study, reported in accordance with Consort guidelines (The Consort Group, 2015).
Figure 1. Study Consort Flow Chart.
2.3. Sample
The program screened 1739 drivers with T1DM from across the country, with potential participants coming from all 50 states. We recruited potential participants through several diabetes websites (MyGlu.com, dLife.com, Dex4.com) and through professional organizations (American Diabetes Association, American Association of Diabetes Educators), and through referral from clinicians specializing in diabetes care. Inclusion criteria for randomization to either DD.com condition were: 1) between ages 18 and 70, 2) had T1D, 3) had diabetes for at least 12 months, 4) had a valid driver's license, and 5) met criteria for T1D drivers at risk for future driving mishaps based on the Risk Assessment for Diabetic Drivers (RADD), which accurately discriminated drivers at high vs. low risk of future driving mishaps within 12 months (Cox et al., 2014). After excluding 613 participants (who may have had more than one reason for exclusion), the final sample size classified in the High Risk group was 449 adults. 444 participated.
2.4. Telephone Motivational Interviewing
The goal of the initial MI session was to increase the participant's motivation to complete the Internet intervention and all its assignments. Therefore the impact of the first MI session should be measured in terms of completion of program benchmarks. The goal of the second MI session was to solidify commitment to maintain changes users had made and lessons learned during DD.com. Therefore, the impact of the second MI session should be measured in terms of subsequent maintenance of changed behaviors related to driving safety. Sessions were semi-structured and partially scripted to enhance fidelity to MI and maximize consistency across counselors. Each 20-30 minute MI session progresses through 4 processes (Engaging, Focusing, Evoking, and Planning, which is optional and depends on the participant's interest). Table 2 presents the contents of the MI sessions. The first MI session focused on eliciting participants' own reasons for planning to complete the Internet program and its assignments. In brief, Motivational Interviewers introduced themselves, reviewed a session agenda, and asked a short series of open questions that elicited the participant's experiences of driving with diabetes and their interests in participating in the study. Interviewers summarized key points several times across the session. They evoked and reflected participant's concerns about diabetes and driving and potential interests in changing. They asked key questions and summarized participants' statements about change.
Table 2. Telephone Motivational Interviewing Session 1 Outline.
| Engaging |
| Introductions, reminder about recording the call, and confidentiality |
| Agenda setting |
| Reflect and summarize agenda |
Open questions followed by reflections of answers, selected from samples below:
|
| Summary of diabetes factors that have a link to driving. |
| Guiding |
Open questions followed by reflections
|
| Summary of main ideas |
| Evoking |
Key questions followed by reflection of answers:
|
| Listen and reflect. |
| Provide information about DD.com. |
| Ask scaling questions about importance and confidence to complete DD.com. |
| Summary of change talk |
| Planning (Skip if not part of logical flow of conversation) |
Key questions followed by reflection of answers:
|
| Summarize |
| Ending session |
| Orient participant and ask final open question |
| What else would you like to talk about today, before we stop? Reflect. |
| Briefly summarize entire conversation, focusing on change talk. |
| Ask: What did I miss? Reflect. |
| Thank participant and end conversation with plan for future. |
2.5. MI Therapist Selection and Training
Interviewers were psychology students and postdoctoral clinical and research fellows. Interviewers in the training phase were 2 postdoctoral fellows, 1 graduate student, and 2 undergraduate research assistants experienced in working with patients and research participants with Type 1 diabetes. Training included 4 2-hour sessions on MI skills, and 2-hour sessions to practice the full MI session. One undergraduate student was not utilized after the training period due to failing to master MI skills in practice sessions.
2.6. MI Fidelity Assessment
Interviews were digitally recorded using a telephone pickup device in the ear of the interviewer. MI practice was supervised weekly for the group of interviewers by an experienced MINT trainer who also coded 10% of the sessions using the widely-used, reliable Motivational Interviewing Treatment Integrity code (MITI 3.1.1; (Moyers, Martin, Manuel, Miller, & Ernst, 2009). Coding of MI was used to provide feedback for counselors, to detect and correct drift from the MI protocol, and to determine MI fidelity for the study.
2.7. Data Analyses
The primary analysis of the RCT found that the DD.com intervention significantly reduced subsequent driving mishaps as reported in monthly driving diaries (Cox et al., 2014). In the current analyses, we examined the impact of the first MI session on completion of program benchmarks. Specifically, we examined whether the DD. com plus MI condition providing therapist support differed from the DD.com only condition that provided no therapist support in usage and completion of the Internet intervention. The outcome variable indicating engagement was number of days from enrollment to completion of tasks such as Cores, daily progress notes, and monthly driving diaries following the active intervention period. Adherence to the program was indicated by completing at least 4 Cores in the 70 day period, because by Core 4, participants would have learned the most important aspects of preventing hypoglycemia while driving. Finally, the outcome variable indicating program completion was the number of Cores completed within the allotted 70 days. We used Chi Square-tests or t-tests to determine whether there were differences in means or proportions in outcome variables between the DD.com only vs. DD.com plus MI conditions.
3.Results
3.1. Participants
As shown in Figure 1, a group of 449 adults with T1DM at high risk for future driving mishaps enrolled in the study. Of those rated as high risk for future driving mishaps, 156 were randomized to DD.com only and 160 were randomized to the DD.com + MI condition. Those drivers assigned to routine care are not included in the present analysis. In brief, participants' mean age was 40.50 (SD=12.50), with 64 between the age of 18-25 and 6 being older than age 65. Mean duration of diabetes was 25.0 years (SD=13.62). 71% of the sample was female and 95% were White, 2.2% were Black, and 3.8% were Hispanic. Table 3 shows the participants' characteristics.
Table 3. Participant Characteristics.
|
DD.com sub-sample n=316 (313 provided data) |
DD.com only n=156 (154 provided data) |
DD.com plus MI (n=160) (159 provided data) |
||
|---|---|---|---|---|
|
| ||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||
|
| ||||
| Age | 40.60 (12.84) | 40.23 (12.19) | 40.96 (13.47) | |
|
| ||||
| Miles driven annually | ||||
| 1,001 to 5,000 | N=6 | N=2 | N=4 | |
| 5,001 to 10,000 | N=86 | N=44 | N=42 | |
| 10,001 to 14,000 | N=86 | N=43 | N=43 | |
| 14,001 to 16,000 | N=135 | N=65 | N=70 | |
|
| ||||
| Years with T1DM | 24.67 (13.81) | 23.86 (14.01) | 25.46 (13.62) | |
|
| ||||
| Risk score* | .451 (.172) | .460 (.176) | .443 (.167) | |
|
| ||||
| n (%) | n (%) | n (%) | ||
|
| ||||
| Sex | ||||
| Male | N=222 | N=103 | N=119 | |
| Female | N=91 | N=51 | N=40 | |
|
| ||||
| Race | ||||
| White | N=297 | N=144 | N=153 | |
| Black | N=6 | N=4 | N=2 | |
| Asian | N=4 | N=3 | N=1 | |
| Native | N=2 | N=0 | N=2 | |
| Multiracial | N=4 | N=3 | N=l | |
|
| ||||
| Ethnicity | ||||
| Hispanic | N=11 | N=7 | N=4 | |
| Non-Hispanic | ||||
|
| ||||
| Education | ||||
| High school graduate | N=43 | N=26 | N=17 | |
| Associate degree | N=48 | N=20 | N=28 | |
| Bachelor's degree | N=142 | N=66 | N=76 | |
| Master's degree | N=63 | N=33 | N=30 | |
| Doctoral degree | N=17 | N=9 | N=8 | |
|
| ||||
| Income Group | ||||
| Less than $10,000 | 12 | 6 | 6 | |
| $10,000 - $24,999 | 18 | 12 | 6 | |
| $25,000 - $49,999 | 56 | 31 | 25 | |
| $50,000 - $74,999 | 69 | 35 | 34 | |
| $75,000 - $99,999 | 53 | 25 | 28 | |
| $100,000 - $149,999 | 69 | 31 | 38 | |
| $150,000 - $199,999 | 20 | 7 | 13 | |
| $200,000 or more | 16 | 7 | 9 | |
255 of the 316 people randomized to DD.com or to MI plus DD.com had risk scores on the RADD that placed them in the category of high risk for future driving mishaps, while 61 were not in the high risk category.
3.2. MI Quality
MI fidelity measured with the MITI 3.1.1 on a sample of 10% of sessions conducted was good to excellent, as shown in Table 4. Interviewers achieved competency in both Global MI characteristics and Ratios based on behavior counts, although the ratio of Reflections to Questions was lower than desired. There was little variability in global ratings or in calculated ratios. This indicates that while sessions were not perfect MI, interviewers achieved a consistent and acceptable level of MI practice.
Table 4. Motivational Interviewing Treatment Integrity (MITI 3.1.1) Scores.
| MITI Globals | Mean (SD) | Range | Benchmark |
|---|---|---|---|
| MI Spirit | 4.64 (.37) | 4.33-5 | 4 |
| Direction | 4.85 (.38) | 4-5 | 4 |
| Empathy | 4.62 (.51) | 4.33-5 | 4 |
| MI Behavior Counts | |||
| Giving information | 2.46 (1.66) | 1-6 | n/a |
| MI-adherent | 3.46 (1.45) | 1-6 | 100% |
| MI-nonadherent | 0 | 0 | 0% |
| Closed Question | 3.23 (2.77) | 1-10 | n/a |
| Open Question | 6.69 (2.78) | 2-11 | n/a |
| Simple Reflection | 5.77 (2.13) | 3-9 | n/a |
| Complex Reflection | 5.15 (2.51) | 2-10 | n/a |
| MI Ratios | |||
| Open to closed questions | 3.76 (3.18) | .43-10.0 | Open > Closed |
| Reflections to questions | 1.21 (.44) | .63-2.33 | 2:1 |
| % MI Adherent | 100 | 100 | 100% |
(n=14 tapes from DD.com + MI condition)
3.3. Outcomes
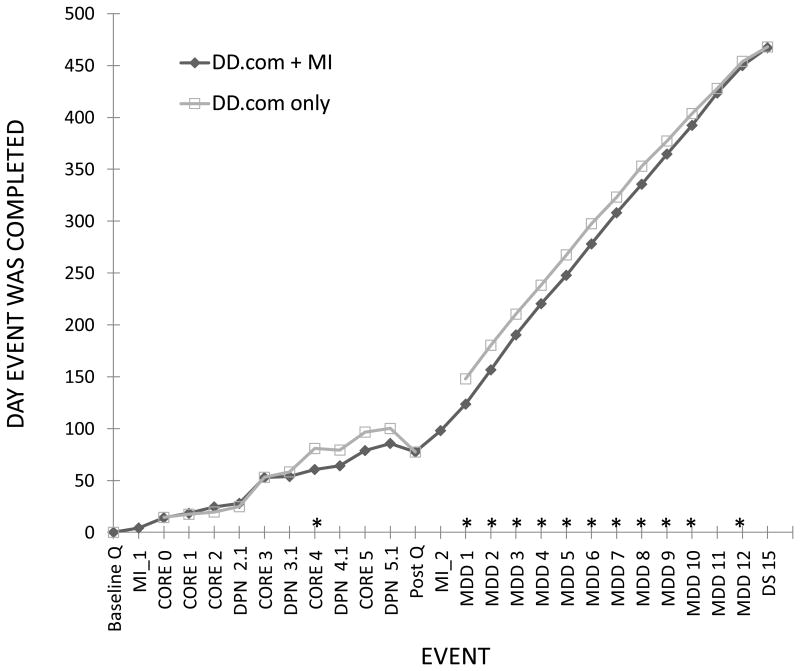
Table 5 shows the outcomes by condition. Program usage did not vary by condition, based on the rate of completed Cores or the submission of daily progress notes. However, those in the DD.com plus MI condition completed Core 4 significantly sooner, on day 61, than did those in the DD.com only condition, who completed it on day 81(t176 df= -2.25; p<.03). Program completion did not vary by condition, but there were indications of better adherence among those in DD.com plus MI. There was a trend for a higher proportion of those randomized to the DD.com plus MI condition to complete Cores 0-4 than those in DD.com only. Those in the DD.com plus MI condition submitted the same number of monthly driving diaries as those in the DD.com only condition, but submitted them significantly sooner for 11 of 12 monthly driving diaries. They remained approximately 20 days ahead of their peers in submitting these diaries through the 12 month post-treatment follow-up. Figure 2 shows the timing of event completion by condition.
Table 5. Program Benchmarks completed and dates completed by condition.
|
DD.com only n=156 |
DD.com + MI n=156* |
||
|---|---|---|---|
| n (%) | n (%) | Chi Squared Test | |
| Completed Cores 0-5 | 108 (69.2%) | 119 (76.3%) | X2=.50, ns |
| Completed Cores 0-4 | 116 (74.4%) | 124 (79.5%) | X2=2.45(p=.12) |
| Completed Cores 0-3 | 128 (82.1%) | 136 (87.2%) | X2=.15, ns |
| Completed Cores 0-2 | 142 (91.0%) | 147 (94.2%) | X2=.01, ns |
| Completed Cores 0-1 | 148 (94.9%) | 154 (98.7%) | X2=.89, ns |
| Completed Core 0 | 152 (97.4%) | 154 (98.7%) | X2=.12, ns |
| Completed no Cores | 4 (2.6%) | 2 (1.3%) | X2=.12, ns |
| Mean (SD) | Mean (SD) | t-test+ | |
|---|---|---|---|
| # Cores completed | 5.1 (1.6) | 5.3 (1.3) | ns |
| Core 4 completion day | 80.9 (85.8) | 60.6 (47.3) | t=-2.29, p = 0.03 |
| Daily Progress Notes (DPNs) Completed Core 2 | 4.7 (2.7) | 4.7 (3.0) | ns |
| DPNs Core 3 | 4.6 (3.2) | 4.3 (2.5) | ns |
| DPNs Core 4 | 4.0 (3.0) | 4.0 (2.7) | ns |
| DPNs Core 5 | 2.3 (1.7) | 2.6 (1.7) | ns |
| MDD 1 completion day | 148 (93) | 124 (41) | t=-2.74,p = 0.01 |
| MDD 2 completion day | 180 (89) | 157 (54) | t =-2.58, p = 0.02 |
| MDD 3 completion day | 210 (87) | 190 (59) | t =-2.12, p = 0.04 |
| MDD 4 completion day | 238 (82) | 220 (53) | t =-2.02, p = 0.05 |
| MDD 5 completion day | 268 (79) | 248 (46) | t =-2.40,p = 0.02 |
| MDD 6 completion day | 298 (75) | 278 (43) | t =-2.48, p = 0.02 |
| MDD 7 completion day | 323 (66) | 308 (42) | t=-2.14,p = 0.04 |
| MDD 8 completion day | 353 (58) | 336 (34) | t =-2.86, p = 0.005 |
| MDD 9 completion day | 377 (47) | 365 (28) | t =-2.55, p = 0.02 |
| MDD 10 completion day | 404 (37) | 392 (22) | t =-2.94, p = 0.004 |
| MDD 11 completion day | 428 (27) | 424 (20) | t=-1.41,p = 0.16 |
| MDD 12 completion day | 454 (18) | 450 (14) | t=-1.99,p = 0.05 |
| MDD 15 completion day | 468 (7) | 467 (5) | t =-0.97, p = 0.33 |
For these analyses, only the 156 DD.com plus MI participants who had an MI session were included.
Due to inequality of variances, these t-tests required Satterthwaite corrections (Moser, Stevens, & Watts, 1989).
Figure 2. Timing of Event Completion by Condition.
4. Discussion
4.1. Telephone MI support feasibility and fidelity
This report shows that a flexible, semi-scripted Motivational Interviewing session guided by the 4 processes of MI can be delivered consistently in telephone support sessions prior to and immediately following an Internet intervention. Semi-scripted telephone MI can achieve good MI fidelity when delivered by moderately trained interviewers experienced with the patient population.
4.2. Impact of MI Telephone Support
The primary effect of the initial session of MI support focusing on program adherence appears to be achieving program benchmarks sooner. Specifically, those who received MI support completed Core 4 sooner, and submitted their first 9 follow-up monthly driving diaries sooner, than those who received DD.com without MI. While not achieving differences that reached statistical significance, those who received the MI session also reached other benchmarks (such as completion of Cores) sooner. Completion rates favored the DD.com plus MI condition. At each point during the intervention period, the proportion of users completing each Core by the DD.com plus MI group exceeded that of the DD.com only group, although these differences did not attain statistical significance.
4.3. Limitations
In this study, we conducted an initial MI session targeting program adherence, and a second MI session targeting maintenance of changes made during the program. It is possible that a single 20-minute MI session, even skillfully conducted, was not enough to have an impact on achieving program benchmarks, even though the literature on MI outcomes shows an impact of similarly brief interventions. One potential reason is that the target behavior was pre-determined (program adherence) by investigators, rather than selected by participants themselves. It is also possible that some people discontinued once they got what they needed from the program, and our analysis cannot determine this. In this report, we did not address the relationship of MI support to intervention outcomes. It is possible that the second MI session, which was designed to focus participants on maintaining changes, and which evoked target behaviors and goals from participants, could have had an impact on subsequent driving mishaps, or related issues such as specific blood glucose management strategies. We plan to investigate this further once all follow-up data are collected. The design did not provide an opportunity to compare MI support with general telephone support, and so we cannot disentangle the MI from telephone support in this analysis. Another challenge to interpreting these findings is that DD.com included automated support such as emails that prompt users to complete the next step, affirming messages when Cores are complete, and reminders about assessments. Users get daily and weekly emails prompting them to complete next steps throughout the program, and during the follow-up periods. Therefore, we were unable to test the potential utility of therapist support in an Internet intervention lacking automated prompts.
4.4. Conclusions
These findings suggest that therapist support using a single session of telephone-delivered Motivational Interviewing prior to an Internet intervention had a non-significant effect on adherence to or completion of the intervention, but that it may significantly speed completion of follow-up assessments. Those who received MI support completed some intervention period benchmarks sooner as well. We found no effects on intervention program components completed or study components completed. These findings contribute to a small but growing literature suggesting that therapist support targeting adherence does not improve adherence to an Internet intervention, at least when programs already include automated support such as reminders. However, it also highlights a potential benefit in promoting completion of assessments.
Highlights.
There is an active debate about whether therapist support is needed to enhance engagement with, adherence to, and completion of, Internet interventions
This paper describes a novel semi-scripted therapist support intervention using Motivational Interviewing to target usage of an Internet intervention for drivers with diabetes
Findings indicate no benefit of therapist support on program completion or other benchmarks, but that those receiving MI sessions completed many benchmarks sooner
Acknowledgments
This project was funded by NIH 2R01DK028288. We thank Dr. Lee Ritterband for consultation on the concept for this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aharonovich E, Greenstein E, O'Leary A, Johnston B, Seol SG, Hasin DS. HealthCall: Technology-based extension of motivational interviewing to reduce non-injection drug use in HIV primary care patients - a pilot study. AIDS Care. 2012;24(12):1461–1469. doi: 10.1080/09540121.2012.663882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G, Carlbring P. Social phobia (social anxiety disorder) In: O'Donohue WT, Draper CR, editors. Stepped care and E-health: Practical applications to behavioral disorders. Springer; 2011. pp. 99–114. [Google Scholar]
- Bennett JA, Young HM, Nail LM, Winters-Stone K, Hanson G. A telephone-only motivational intervention to increase physical activity in rural adults: A randomized controlled trial. Nursing Research. 2008;57(1):24–32. doi: 10.1097/01.NNR.0000280661.34502.c1. [DOI] [PubMed] [Google Scholar]
- Blankers M, Koeter M, Schippers GM. Evaluating real-time internet therapy and online self-help for problematic alcohol consumers: A three-arm RCT protocol. BMC Public Health. 2009;9:16. doi: 10.1186/1471-2458-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankfurter TL, Farentinos C, et al. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug and Alcohol Dependence. 2006;81(3):301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. Journal of Medical Internet Research. 2009;11(2):e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook PF, McCabe MM, Emiliozzi S, Pointer L. Telephone nurse counseling improves HIV medication adherence: An effectiveness study. The Journal of the Association of Nurses in AIDS Care: JANAC. 2009;20(4):316–325. doi: 10.1016/j.jana.2009.02.008. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Gonder-Frederick L, Ritterband L, Clarke WL, Kovatchev BP, Schmidt K, et al. Internet intervention designed to identify and reduce risk of diabetic driving mishaps, oral abstract 260-OR. Diabetes. 2014;(Supplement 1)(63):a68. [Google Scholar]
- Coyne N, Correnti D. Effectiveness of motivational interviewing to improve chronic condition self-management: What does the research show us? Home Healthcare Nurse. 2014;32(1):56–63. doi: 10.1097/NHH.0000000000000001. [DOI] [PubMed] [Google Scholar]
- Farrell-Carnahan L, Hettema J, Jackson J, Kamalanathan S, Ritterband LM, Ingersoll KS. Feasibility and promise of a remote-delivered preconception motivational interviewing intervention to reduce risk for alcohol-exposed pregnancy. Telemedicine Journal and e-Health : The Official Journal of the American Telemedicine Association. 2013;19(8):597–604. doi: 10.1089/tmj.2012.0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman CJ, Egleston BL, Hofmann MT. Efficacy of motivational interviewing for smoking cessation: A systematic review and meta-analysis. Tobacco Control. 2010;19(5):410–416. doi: 10.1136/tc.2009.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hettema JE, Hendricks PS. Motivational interviewing for smoking cessation: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(6):868–884. doi: 10.1037/a0021498. [DOI] [PubMed] [Google Scholar]
- Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE. Persuasive system design does matter: A systematic review of adherence to web-based interventions. Journal of Medical Internet Research. 2012;14(6):e152. doi: 10.2196/jmir.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindner P, Ivanova E, Ly KH, Andersson G, Carlbring P. Guided and unguided CBT for social anxiety disorder and/or panic disorder via the internet and a smartphone application: Study protocol for a randomised controlled trial. Trials. 2013;14 doi: 10.1186/1745-6215-14-437. 437-6215-14-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke B. A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20:137–160. [Google Scholar]
- Martino S. Motivational interviewing to engage patients in chronic kidney disease management. Blood Purification. 2011;31(1-3):77–81. doi: 10.1159/000321835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing. New York: Guilford Press; 2012. [Google Scholar]
- Moser BK, Stevens GR, Watts CL. the two-sample t-test versus Satterthwaite's approximate F test. Communications in Statistics: Theory and Methods. 1989;18:3963–3975. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised global scales: motivational interviewing treatment integrity 3.1.1. 2009 Unpublished manuscript. Retrieved May 3, 2011, from http://casaa.unm.edu/download/MITI3_1.pdf.
- Nordgreen T, Havik OE, Ost LG, Furmark T, Carlbring P, Andersson G. Outcome predictors in guided and unguided self-help for social anxiety disorder. Behaviour Research and Therapy. 2012;50(1):13–21. doi: 10.1016/j.brat.2011.10.009. [DOI] [PubMed] [Google Scholar]
- Riper H, Blankers M, Hadiwijaya H, Cunningham J, Clarke S, Wiers R, et al. Effectiveness of guided and unguided low-intensity internet interventions for adult alcohol misuse: A meta-analysis. PloS One. 2014;9(6):e99912. doi: 10.1371/journal.pone.0099912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Ardalan K, Thorndike FP, Magee JC, Saylor DK, Cox DJ, et al. Real world use of an internet intervention for pediatric encopresis. Journal of Medical Internet Research. 2008;10(2):e16. doi: 10.2196/jmir.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for internet interventions. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2009;38(1):18–27. doi: 10.1007/s12160-009-9133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. The British Journal of General Practice : The Journal of the Royal College of General Practitioners. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- Smedslund G, Berg RC, Hammerstrom KT, Steiro A, Leiknes KA, Dahl HM, et al. Motivational interviewing for substance abuse. Cochrane Database of Systematic Reviews (Online) 2011;5(5):CD008063. doi: 10.1002/14651858.CD008063.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Consort Group. CONSORT: Transparent reporting of trials. 2015 Retrieved 01/28, 2015 from http://www.consort-statement.org/
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism (Oxford, Oxfordshire) 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Walker DD, Roffman RA, Picciano JF, Stephens RS. The check-up: In-person, computerized, and telephone adaptations of motivational enhancement treatment to elicit voluntary participation by the contemplator. Substance Abuse Treatment, Prevention, and Policy. 2007;2:2. doi: 10.1186/1747-597X-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]