Introduction
Following the Tokyo Electric Power Co., Inc. (TEPCO) Fukushima Daiichi Nuclear Power Station accident in the aftermath of the Great East Japan Earthquake in 2011, there was great pressure to overhaul Japan’s nuclear emergency preparedness measures. The nuclear emergency response guidelines were formulated by the Nuclear Regulation Authority (NRA) on October 31, 2012, and subsequently revised on June 5, 2013. Under the revised policy, local public authorities in Precautionary Action Zones (PAZ) are to construct a system enabling the distribution of iodine*1 to local residents in advance, and shall hold information meetings for local residents regarding the distribution of iodine at which physicians explain the prophylactic use and adverse reactions, etc. of iodine.
Thus, the Japan Medical Association (JMA) has formulated the guidelines for the administration of iodine, because it is anticipated that an emergency resulting from an accident at a nuclear power facility will affect not only the area immediately surrounding the nuclear facility but also a broader area including numerous prefectures; the guidelines are intended as reference materials for many physicians acting as local opinion leaders at information meetings on the distribution of iodine to enable them to smoothly explain the benefits and risks of iodine prophylaxis to block the uptake by the thyroid gland of radioactive iodine released to the environment, as well as to enable physicians and medical associations to swiftly distribute iodine at the time a nuclear emergency occurs.
These guidelines are distributed to local physicians in areas surrounding the Sendai Nuclear Power Plant (NPP) in Kagoshima Prefecture to provide a better understanding of predistribution of iodine to residents in the areas.
We hope that physicians and local medical associations will use their medical knowledge regarding the timing of distribution and administration of iodine to actively advise local residents and local public authorities, and thereby help reduce the risks of radiation exposure of the thyroid gland in local residents upon a nuclear emergency.
In future, the JMA intends to continue to promote various disaster prevention measures, including nuclear emergency preparedness, in order to protect the lives of the people of Japan as a healthcare professionals’ organization. We ask for your continuing support in these endeavors.
Necessity of Iodine Prophylaxis as a Protective Measure in the Event of an Accident at a Nuclear Facility
Radiation exposure and internal contamination
In the event that an accident occurs at a nuclear facility (a nuclear power station; nuclear reactor; or facility that separates radioactive isotopes, processes or reprocesses used nuclear fuels, or stores used nuclear fuel), the radioactive materials (substances that emit radiation) released to the environment from the facility through vents, etc., include iodine, cesium, strontium, plutonium, and others. The radiation emitted by these substances damage the DNA of cells. This is the main cause of health damage by radiation.
Exposure to radioactive materials is called “radiation exposure”; exposure from outside the body is called “external exposure,” while exposure from radioactive materials that are incorporated into the body is called “internal exposure or contamination”. These guidelines have been formulated in anticipation of cases of exposure—mainly “internal exposure”—to radioactive iodine (which has a tendency to accumulate in the thyroid gland).
The impact of internal exposure is determined by the effective dose coefficient (sievert/ Becquerel: Sv/Bq), which expresses the radiation dose when 1 becquerel of radioactive materials has been incorporated. This is determined by such factors as the type of the radioactive materials, their chemical forms, incorporation pathway, seize of particles and age.
In the case of internal exposure, the radioactive materials emit radiation within the body, and the effects of incorporated radioactive materials depends on the time required for the disintegration of one-half of the radioactive material (physical half-life) and also the time an organism takes to eliminate one half the amount of a radioactive material incorporated (biological half-life). The physical half-life of iodine-131 (131I) is approximately eight days.
Based on basic research and epidemiological studies conducted thus far, in Japan the annual dose limit for the public other than naturally occurring radiation or radiation used by medical facilities for testing and medical treatment has been deemed to be 1 mSv per year as an effective dose, and this level has been protected throughout the regulatory system.
The “effective dose” is the tissue-weighted sum of the equivalent doses in all specified tissues and organs of the body; this quantity takes into account each organ or tissue being irradiated. When radiation exposure to only the thyroid gland is being considered, the equivalent dose is used. The “2007 Recommendations of the International Commission on Radiological Protection” (ICRP Publication 103) defines 1:25 as the ratio of effective dose to equivalent dose in the case of internal exposure to iodine-131; when the equivalent dose for the thyroid gland is 25 mSv, the effective dose is 1 mSv. The dose limit for physicians, radiological technologists (the same as for nuclear power facility workers), and other workers in occupations involving radiation exposure is “100 mSv over 5 years, but the dose limit should not exceed 50 mSv in any single year.
Health damage caused by radioactive iodine
When radioactive iodine is incorporated into the body, it accumulates in the thyroid gland, and the radiation emitted can cause thyroid cancer within a few years to a few decades. While the Japan NRA has presented papers finding that “the results of epidemiological studies conducted on external radiation exposure in Hiroshima and Nagasaki indicate the possibility that increased risk of thyroid cancer persisted for people also in aged 40 years or older,” it must be noted that there is no current international consensus reached on this point.1
Furthermore, in the case of exposure to a high radiation dose, over a period of several months hypothyroidism may develop as a result of reduced excretion of thyroid hormone due to the death of thyroid gland cells.
Radiation can affect the thyroid gland both in the case of external radiation exposure and in the case of internal exposure where radioactive iodine accumulates in the thyroid gland. However, in the event that a serious accident occurs at a nuclear power facility, radioactive iodine is released into the atmosphere, and there is an increased risk of people inhaling the radioactive material or ingesting it by eating contaminated food.
Effects of iodine
If the radioactive iodine released by nuclear power facilities enters the human body through inhaling or ingestion it, approximately 10-30% of the amount incorporated will accumulate in the thyroid gland within 24 hours of contamination, and most of the remaining radioactive iodine will be eliminated from the body by the kidneys in urine.
As the result of exposure to radiation from this radioactive iodine, thyroid cancer or other diseases may develop in four years to a few decades.
The dose of this thyroid exposure can be averted by taking iodine (127I) within 24 hours before intake of radioactive iodine. This measure has been also reported to be effective for blocking radioactive iodine in the thyroid if iodine is administered within four hours after intake of radioactive iodine.2
When adequate quantities of iodine are administered, the iodine is incorporated into the circulation system and the concentration of iodine is increased in the blood, leading to high concentration of iodine in the thyroid gland. The synthesis of thyroid hormone requires iodine in the blood. Whereas detailed mechanisms for the blocking of thyroidal uptake of radioactive iodide are not established, several mechanisms have been postulated: saturation of the iodide transport mechanism, interference with intra-thyroidal organification of iodide, isotope dilution, and inhibition of hormone release.2 Thus, saturation of the iodide transport system by excess iodide leads to blockage of radioactive iodine uptake in the thyroid and the interference with intra-thyroidal organification of iodide results in inhibition of the thyroid hormone synthesis. Dilution of the radioactive iodine with one reduces probability for uptake of radioactive iodide.
When a healthy adult takes iodine, the concentration of iodine excreted in the urine peaks within 1-2 hours of taking the preparation, the amount of iodine in the urine gradually decreases, and the most of incorporated iodine will be eliminated from the body within 72 hours.
Iodine cannot prevent radioactive one from entering the body. Iodine is only effective for reducing the internal exposure of the thyroid gland to radioactive iodine and cannot reduce the dose of exposure to radioactive materials other than materials. Furthermore, administration of iodine will not treat injury of the thyroid gland or make the thyroid release radioactive iodine restore the thyroid gland after incorporation.
Administration of Iodine
Instructions for administration
Concerning administration of iodine to residents, the NRA has provided as below in the guidelines; information on pre-distribution of iodine to the local residents has to be provided based on the Authorities policies at meetings
Administration within Precautionary Action Zones (PAZ)
For commercial nuclear reactors to generate electricity, in Precautionary Action Zones (PAZ) within a radius of approximately 5 km of the reactor, when a “General Emergency” is called, the Nuclear Emergency Response Headquarters or the local public authorities will issue instructions for the administration of iodine in addition to instructions for evacuation, therefore iodine should be taken in accordance with these instructions in principle.
However, those who cannot take iodine such as infants (whose thyroid glands are more sensitive to radioactive iodine than those of adults), and the parents/guardians of infants are to evacuate on a priority basis at the “Site Area Emergency” stage where administration of iodine is not necessary.
Administration in areas outside Precautionary Action Zones (PAZ)
In areas outside PAZ, when a “General Emergency” is called, based on the instructions of the National Government or local public authorities, people should immediately shelter indoors, thereafter the NRA will determine whether it is necessary to distribute/administer iodine in addition to evacuating or sheltering indoors, depending on the status of the nuclear power facility and amounts of airborne radiation. If the Nuclear Emergency Response Headquarters or the local public authorities then issue instructions for the administration of iodine, it should in principle be taken in accordance with these instructions.
Dose and frequency
As a general rule, iodine should be taken once only; continuously repeated administration should be avoided. However, in the case that the possibility of internal exposure from radioactive iodine continues for 24 hours or more and a second administration is unavoidable, subsequent iodine should be administered at an interval of 24 hours or more.
As a general rule, repeated dosing should only be carried out when the NRA has determined that another administration is necessary.
Dose (Table 1)
Table 1.
Recommended single dose of Iodine prophylaxis
| Age groups |
Iodine amount (mg) Amount equivalent to potassium iodide |
Potassium iodide amount (mg) | Potassium iodide pills |
| (Source: Nuclear Regulatory Agency.3) | |||
| Neonates (Birth to 1 month) |
12.5 | 16.3 | — |
| Infants (1 month to 35 months) |
25 | 32.5 | — |
| Children (3 years to 12 years) |
38 | 50 | 1 tablet |
| Adults and Adolescents (13 years or over) |
76 | 100 | 2 tablets |
(1) Adults and adolescents aged 13 years or over: 2 tablets (1 tablet contains 50 mg of potassium iodide; 2 tablets contain 100 mg)
(2) Children aged between 3 and 12 years: 1 tablet (50 mg of potassium iodide)
(3) Infants aged between one month and 35 months: 32.5 mg of potassium iodide
(4) Neonates: 16.3 mg of potassium iodide
Note that for infants aged under three years (36 months), neonates, and others for whom taking tablets is difficult, liquid iodine prepared from powder by a pharmacist should be administered.
Furthermore, people of all ages should be administered with iodine, but in principal priority is to be given to small children and youth.
Precautions Regarding Administration of Iodine
Adverse reactions
At the time of the Chernobyl nuclear power plant accident in 1986, iodine was distributed to 10 million children and 7 million adults in Poland, and follow-up studies were conducted on 34,491 of these people. The results of these studies showed a 0.37% of neonates with hypothyroidism, and 4.6% of children experienced symptoms such as vomiting, skin rashes, stomach pain, diarrhea, and headache. It is not clear whether these symptoms were adverse reactions of iodine, and since then it has been reported that these adverse effects were transient.4
Contraindications and precautions
Those with a medical history of hypersensitivity to iodine substance are deemed to be inappropriate for the administration of iodine. When it has been revealed that a resident may develop such symptoms after predistribution of iodine, he/she has to be informed to no take iodine.
In addition, iodine should be administered with caution in the case that the person exhibits any of the following symptoms.
(1) Hypersensitivity to iodinated contrast medium
(2) Thyroid dysfunction
(3) Renal dysfunction, myotonia congenital, hyperkalemia
(4) Hypocomplementemic urticarial vasculitis, Duhring dermatitis herpetiformis
(5) Pulmonary tuberculosis
Medicines possibly interacting with iodine
For people currently under medical treatment, in the case that they take iodine in addition to their medicines currently being taken, there is the possibility of health effects due to interaction between the medicines and iodine. As a general rule, iodine is administered once only following a nuclear power facility accident, and so the risk of serious health effects due to the interaction of the drugs seems less concerned; however, citizens taking the medicines shown in Table 2 should be encouraged to consult a physician before taking iodine. The same applies when people who have received iodine in advance newly start any of these medicines.
Table 2.
Examples of medicines with which the iodine could interact
| Note: It is possible to search for detailed names of pharmaceuticals using the RAD-AR Council, Japan “Kusurino-Shiori [Drug information Sheet].” (http://www.rad-ar.or.jp/siori/english/index.html) |
Since the medicines that people are currently taking should be checked, it is recommended to distribute iodine based on advise of pharmacists at information meetings to local residents for iodine predistribution.
Administration to children
An iodine product currently available for predistribution is potassium iodide (50 mg), “Potassium Iodide Tablet 50 mg (Nichi-Iko Pharmaceutical Co., Ltd.),” which has a shelf-life of approximately 3 years.
For this reason, dose is 1 tablet for children aged between 3 and 12 years and 2 tablets for adolescents aged 13 years or over.
However, for infants aged under three years (36 months), neonates, and others who cannot take tablets, liquid iodine prepared from powder by a pharmacist should be administered. For this reason, in addition to constructing a system for preparing and distributing liquid iodine at times of emergency, the development of syrup-type iodine products that can be stored for a certain period of time is required.
In addition, in case of pediatric use, beware that there is the possibility that administration may cause rashes or suppress thyroid function.
Pregnant, nursing and lactating women
Women who are or could possibly be pregnant should be administered with a single dose of iodine in a case where the effectiveness of reducing internal exposure of thyroid gland outweighs the risk of taking iodine. However, multiple doses must be avoided.
Furthermore, in the case that iodine is administered during the third trimester of pregnancy, there is a risk that hypothyroidism may affect mental development to neonates.
Iodine can cross the placental barrier and cause thyroid adenoma or thyroid dysfunction in the fetus.
Nursing mothers must avoid breastfeeding when they take iodine and for a certain period of time afterwards.
Iodine can transfer into breast milk so breast-fed infants may develop skin rashes and/or its thyroid functioning may be suppressed. In addition, it is reported that 65-80% of the potassium iodide in iodine tablets is eliminated from the body in urine within 24 hours.
The elderly
The NRA has announced that “based on recent research, it has been reported that the risk for developing thyroid cancer for people aged 40 years or above decreases with age, but this risk remains amongst the elderly. It has also been reported that the possibility of adverse reactions [from taking iodine] such as temporary suppression of thyroid function increases with age.”
However, it must be noted that international evaluations have not been established regarding the risk of developing cancer amongst elderly people.
As age increases, organ function may be reduced in addition to decrease in vision and hearing. For example, if gastric acid secretion and/or gastrointestinal movement is reduced, absorption of drugs may be suppressed.
Furthermore, because it becomes easier for the ingredients of administered drugs to remain in the body due to decrease in liver detoxification and renal excretion, elderly people should be encouraged to consult a physician before taking iodine.
Effects of overdose
Taking more than the recommended dose of iodine will not increase the protective effects; it rather increases the possibility of adverse events such as thyroid dysfunction. Therefore, no more than the recommended dose can be administered. Even if a dose higher than the prescribed dose is accidentally administered, it is not necessary to take such measures as to get the person vomited, it is recommended that the person be checked to determine whether there has been any abnormal change in their physical condition and a physician consulted.
Predistribution of Iodine at Residents’ Information Meetings
At residents’ information meetings regarding the predistribution of iodine, residents should check the items explained by the physician on the check sheet themselves and have these items cross-checked by a pharmacist or local government employee before being issued with a iodine in exchange for a receipt. Of the items residents fill out on their check sheets, if the person checks items under “Inappropriate for administration” (does the person have a health history of hypersensitivity to the ingredients of iodine or iodine?) or items under “Administer with caution,” the following measures should be taken.
Items under “Inappropriate for Administration”
-
Residents who reply “item does not apply to me”
Distribute the iodine in exchange for a receipt.
-
Residents who reply “do not know”
It is important to take the necessary preparations and for all staff involved to work together; for example, if it is possible for a physician to determine whether iodine can be administered through interviews at the meeting venue with the residents regarding their health history, it can be decided that iodine can be distributed.
-
Residents who reply “item does apply to me”
Do not distribute iodine to such residents.
Items under “Administer with Caution”
-
Residents who reply “item does not apply to me/do not take medication”
Distribute the iodine in exchange for a receipt.
-
Residents who reply “do not know” or “item does apply to me/do take medication”
It is important to take the necessary preparations and for all staff involved to work together; for example, if it is possible for a physician to determine whether iodine can be administered through interviews at the meeting venue with the residents regarding their health history, it can be decided that iodine can be distributed.
Residents should be instructed to consult their family physician if there are any aspects of the items explained by the physician at the information meeting that they do not understand, including items other than the two mentioned above. They should also be instructed to take their completed check sheet with them when consulting with their family physician.
Evacuation in the Event of a Nuclear Power Facility Accident and Administration of Iodine
Evacuation or relocation in the event of a nuclear power facility accident
Evacuation and relocation in the event of a nuclear power facility accident are both safeguards to be implemented in the case that there is the possibility that local residents may be exposed to radiation levels higher than a prescribed level. Residents can reduce their exposure doses by distancing themselves from the radioactive materials and/or the radiation source.
Evacuation
Evacuation is carried out urgently when the levels of radiation being released into the atmosphere are higher than an approved level or there is a risk that they will become high, or in order to quickly separate residents from the site from which the radioactive materials are being released.
Relocation
Relocation is carried out in order to reduce needless exposure to radiation that would occur if residents continuously lived in the affected area, as well as to separate residents from the affected area for a certain period of time.
Sheltering in place
Sheltering in place is a countermeasure carried out to reduce radiation exposure by the inhalation of radioactive substances and from neutrons and gamma radiation.
Sheltering in place is carried out under the instructions of the National Government or local public authorities in the case that residents are required to wait in order to reduce the risk of radiation exposure following a nuclear power facility until the National Government or local public authorities order evacuations, etc., or in the case that carrying out evacuations is difficult.
For hospitals and nursing care facilities in particular, in certain cases priority needs to be given to sheltering in place rather than evacuation. In such cases, sheltering in place in concrete buildings—which generally have a shielding effect and are relatively airtight—is effective.
Responses by medical facilities in consideration of vulnerable people
In consideration of vulnerable people requiring nursing care, etc., in the case that a nuclear emergency occurs and a recommendation or order to evacuate is issued, administrators of hospitals and other medical facilities shall swiftly and safely evacuate or transfer to another medical institution all inpatients, outpatients, and patients’ visitors, etc. in accordance with an evacuation plan formulated in advance by each medical facilities and under the direction and guidance of physicians, nurses, and other staff.
Physicians’ advice regarding distribution and administration of iodine
Regarding the timing of administration and efficacy of iodine, “administration of iodine 24 hours prior to exposure to radioactive iodine” has “an inhibitory efficacy of 90% or higher,” but “administration of iodine 8 hours after exposure to radioactive iodine” has “an inhibitory efficacy of 40%.” Moreover, “administration of iodine 24 hours after exposure to radioactive iodine” has “an inhibitory efficacy of only 7%”5 (Table 3).
Table 3.
Timing of administration and effect of iodine
| (Source: Preston LD, et al.1) | |
| Administration 24 hours prior to exposure to radioactive iodine | Protective effect of 90% or higher |
| Administration 8 hours after exposure to radioactive iodine | Protective effect of 40% |
| Administration 24 hours after exposure to radioactive iodine | Protective effect of 7% |
Accordingly, it is important that, based on their understanding of the nuclear accident status and evaluation of risks for a broad area, not only the nuclear power facilities and the surrounding area, physicians and medical associations provide advice to local public authorities based on their medical knowledge regarding the timing of distribution and administration of iodine in order to reduce the risks to local residents.
In addition, one lesson learned from the Tokyo Electric Power Co., Inc. (TEPCO) Fukushima Daiichi Nuclear Power Station accident was that, in the case that local residents are unable to obtain information regarding instructions for evacuation and taking iodine due to interruption of telecommunications, as well as in the case that discussions are held with local public authorities regarding the necessity and timing of iodine administration—including when iodine are to be taken and their efficacy—the following items need to be checked.
(1) Collection of information to enable a decision to be made as to whether or not there is a possibility of local residents being exposed to a certain level of radiation within 24 hours
(2) Situation regarding iodine stockpiles
(3) Situation regarding the preparation of explanatory pamphlets, etc., describing the health damage caused by radioactive iodine and the benefits/efficacy as well as adverse reactions of iodine, etc.
(4) Situation regarding the preparation of medical questionnaires
Instructions for administering iodine in the accident/emergency zone
Under Japan’s nuclear emergency policy, criteria have been established for prompt implementation of evacuation and other measures following the occurrence of a nuclear power facility accident.
Depending on the accident status, emergency situations are classified into three categories: “Alert,” “Site Area Emergency,” and “General Emergency.” In cases such as when the level of radiation near the perimeter of a nuclear power facility site is 5 μSv/h or higher, if facility workers have received a warning from the National or a Prefectural Government, the situation is deemed a “Site Area Emergency,” and at this stage safeguards for local residents, etc.—that is, making preparations for the distribution of iodine while at the same time evacuating and/or administering iodine to vulnerable people—are to be implemented.
Furthermore, in the case that the above-mentioned radiation level rises to 500 μSv/h or higher, the situation is deemed to be at the “General Emergency” stage—the level at which the general public is affected (or there is a high possibility the general public will be affected) by radiation—and the distribution/administration of iodine and evacuations are carried out (Table 4).
Table 4.
Overview of Japan’s emergency situation classifications
| Classification | “Alert” | “Site Area Emergency” | “General Emergency” |
| (Source: Japan Atomic Energy Agency (JAEA).) | |||
| * Persons requiring evacuation: persons requiring support at times of disaster (people who are sick or injured, hospitalized, elderly, or disabled; foreign nationals, infants, pregnant woman, and others who require assistance in disasters) for whom evacuation would take more time than normal and who amongst those whose health risks would not increase due to evacuation, to whom iodine cannot be distributed in advance, or for whom administration of a stable iodine preparation is inappropriate but needs safeguards such as early evacuation at the “Facility Emergency” stage. | |||
| Accident status | |||
| Radiation effects to the general public (Statement of the Nuclear disaster response policy) |
No (Not an emergency) |
Rare (Possible) |
Yes (Highly possible) |
| Main countermeasures | |||
| Monitoring in emergency situations | Preparation | Implementation | (Implementation) |
| Preventative evacuation of people requiring evacuation* | Preparation | Implementation | (Implementation) |
| Safeguards for residents | Preparation | Implementation | |
| Laws and regulations | |||
| Act on Special Measures Concerning Nuclear Emergency Preparedness | — | Article 10 (Obligation to Notify of a Nuclear Emergency Preparedness Manager) |
Article 15 (Declaration of Nuclear Emergency Situation) |
Accordingly, it is important that local medical associations discuss with local governments concrete measures such as methods for administering iodine following evacuation procedures.
Administration of iodine in radiation emergency medical
When a nuclear emergency occurs, medical treatment for injured and sick people who could have been contaminated with a radioactive material or exposed to radiation is to be carried out smoothly at the first response stage in accordance with a medical care system that has been prepared in advance.
Under this system, as a general rule the person responsible for nuclear emergency preparedness for the affected area overall is to communicate instructions to medical institutions, etc., to promptly administer iodine in accordance with National Government instructions in the case that the release of radioactive iodine is anticipated or radioactive iodine has been released.
Methods for obtaining necessary information regarding evacuation and iodine administration instructions
In order to ensure the safety and security of local residents as well as support appropriate decision-making and action-taking by local residents themselves, the National Government and local public authorities are to endeavor to promptly convey and disclose accurate and easy-to-understand information to the general public. In the case of a nuclear emergency in particular, the following information is to be conveyed.
(1) The situation concerning the nuclear power facility accident
(2) Monitoring results
(3) Weather forecasts
(4) Forecasts for the diffusion of radioactive materials in the atmosphere, etc.
Furthermore, government information at the time the accident occurs can be conveyed via various methods, and so people should try to obtain information through the following methods.
(1) TV, radio, one-segment (digital terrestrial) broadcasting
(2) Local community broadcasting
(3) The Internet, electronic bulletin boards for government announcements
(4) Mobile terminals and other emergency flash news e-mail
(5) Police information
(6) Information from fire departments or volunteer fire companies, etc.
Moreover, it is important that local medical associations and other organizations obtain information from the local disaster response headquarters using telecommunications methods such as community wireless disaster information systems, satellite telephones, and disaster priority telephones, to relay appropriate information to doctors and medical institutions.
Actions of Local Medical Associations in a Nuclear Emergency and Advance Preparations
It’s important that local medical associations take the following 3 actions—(1) Collecting Nuclear Emergency-related Information, (2) Evaluating Risks of Radiation Exposure, (3) Sharing their Information with Medical and Health Professions—in a nuclear emergency and make each preparation for doing so in advance.
Collecting nuclear emergency-related information
First, local medical associations should turn on the following two “switches” in order to collect nuclear emergency-related information.
(1) Turn on the TV and/or radio
(2) Turn on their “risk management switch”
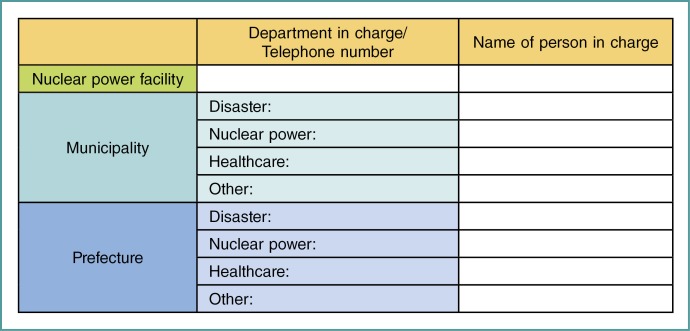
The “risk management switch” refers to beginning to gather information from the nuclear power facility, the prefecture/municipality headquarters for disaster control, the Off-site center, and health and medical care departments, and promptly beginning to provide the collected information to physicians and medical institutions. In preparation for this, a table of names of the organizations from which information can be obtained is to be drawn up in advance (Fig. 1).
Fig. 1.
Example of a table of relevant organizations
Evaluating risks of radiation exposure
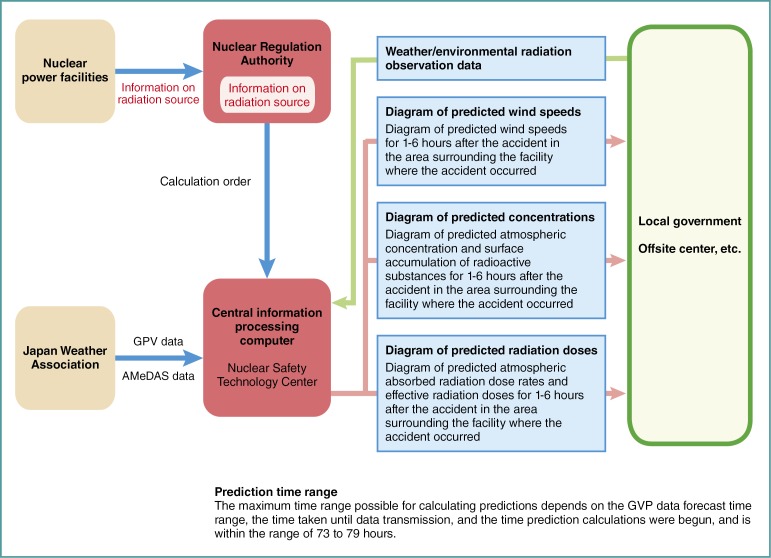
Next, it is necessary to evaluate risks of radiation exposure based on highly reliable information. For example, there is the System for Prediction of Environmental Emergency Dose Information (SPEEDI) data as useful information in Japan.
SPEEDI is a system to predict the atmospheric concentration of radioactive particles in the surrounding environment, radiation exposure amounts, and other environmental impacts, based on information of radiation source, weather conditions, and topographical data. This system can forecast the critical information such as the concentration of radioactive materials in the atmosphere, effective radiation doses from external exposure, and equivalent dose for the thyroid gland through inhalation (Fig. 2).
Fig. 2.
Flow of SPEEDI information
However, since some uncertainty is inherent in the forecasted information, decisions should be made based on the actually observed or detected values as much as possible.
Sharing information with medical professions on the affected areas
Medical professions such as physicians, nurses, and pharmacists will be involved in administering iodine tablets on the affected areas. The local medical associations should establish the system for providing nuclear emergency-related information and risk evaluations of radiation exposure for them promptly in a nuclear emergency.
Disaster Preparedness in Local Medical Associations
Collecting nuclear emergency-related information
Hospitals or medical association in local governments with nuclear facilities should share information required for evacuation and iodine with local governments in advance.
Information regarding the disaster prevention plans of the company of nuclear power plant,
-
Information about the social infrastructure environment
(1) Information regarding designated evacuation centers and concrete buildings suitable for sheltering in place
(2) Local government evacuation plans
(3) Documents regarding the location of public facilities, etc.
a. Daycare centers, kindergartens, schools, clinics, hospitals, nursing care facilities, facilities for disabled persons, etc.
b. Maps showing distance between these facilities and the nuclear power facility and localization of the nuclear power facility
(4) Information regarding radiation emergency medicine facilities
(5) Information regarding the content and locations of stockpiles of iodine and equipment for medical care
(6) Documents and lists of names, etc. for people requiring assistance to evacuate, etc.
Training and education against a nuclear disaster
At the time of the accident at the Fukushima Daiichi Nuclear Power Station, physicians were asked for explanations on health effects of radiation and advice about iodine administration by residents, when they provided medical care at first aid stations. However, they could not make satisfactory responses to the residents because of lack of information and knowledge on radiation and its effects.
Since physicians use radiation for their clinical works and are experts of health care, they have to have basics on radiation. They also play important roles in radiation emergency. Therefore, it is necessary to conduct training and educational programs against a nuclear disaster for physicians.
JMA held a symposium of “Disaster Medicine and Medical Associations” (http://www.med.or.jp/english/journal/toc/v55no05.html) and “the JMAT Training Course on Disaster Medicine” in 2012. The reports of these conferences have been posted on the JMA website and are available to anyone for reference.
Acknowledgments
We acknowledge with gratitude the lots of advice of Mr. Yuji Noto, Division chief, International division, Japan Medical Association and Mr. Paul Talcott, Researcher, Japan Medical Association Research Institute in developing the guidelines; and the cooperation of Ms. Yukako Maniwa in translating the guidelines into English.
Footnotes
*1 Iodine: Potassium Iodide (KI) for thyroid blocking in a radiation emergency.
References
- 1.Preston DL, Ron E, Tokuoka S, et al. Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat Res. 2007;168:1-64. [DOI] [PubMed] [Google Scholar]
- 2.Sternthal E, Lipworth L, Stanley B, Abreau C, Fang SL, Braverman LE. Suppression of thyroid radioiodine uptake by various doses of stable iodide. N Engl J Med. 1980;303:1083-1088. [DOI] [PubMed] [Google Scholar]
- 3.Nuclear Regulatory Agency. Distribution and Administration of Stable Iodine Preparations (for Medical Professionals).
- 4.Nauman J, Wolff J. Iodide prophylaxis in Poland after the Chernobyl reactor accident: benefits and risks. Am J Med. 1993;94:524-532. [DOI] [PubMed] [Google Scholar]
- 5.Zanzonico PB, Becker DV. Effects of time of administration and dietary iodine levels on potassium iodide (KI) blockade of thyroid irradiation by 131I from radioactive fallout. Health Phys. 2000;78:660-667. [DOI] [PubMed] [Google Scholar]