Abstract
Eravacycline is a fluorocycline antibiotic in phase 3 clinical development for complicated intra-abdominal and urinary tract infections. To support its clinical development, a study was conducted to evaluate the effects of various susceptibility test parameters on the MIC values for aerobic bacteria. The results showed that eravacycline appears to be largely unaffected by medium age, medium additives, and other nonstandard assay conditions.
TEXT
This study investigated whether the age of the cation-adjusted Mueller-Hinton broth (CA-MHB) and other testing parameters affected the activity of eravacycline, a new broad-spectrum fluorocycline antibiotic (1) (Fig. 1) and whether any special accommodations need to be made for routine susceptibility testing with eravacycline. The in vitro activities of other tetracyclines, tigecycline and omadacycline, are known to be affected by the age of the test medium (2, 3, 4), and as a result, the Clinical and Laboratory Standards Institute (CLSI) guidelines specify the use of freshly prepared medium or medium that has been frozen within less than 12 h after preparation for susceptibility testing with these antibiotics. In addition to medium age, the effects of nonstandard conditions (addition of serum or blood, Haemophilus test medium [HTM], altered pH, high/low inoculum, various cation concentrations, polysorbate addition, or incubation in 5% CO2) on the eravacycline activity profile were evaluated.
FIG 1.
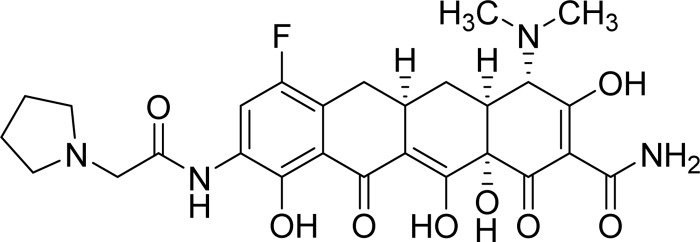
Chemical structure of eravacycline.
Testing was done using standardized CLSI methodology (1, 5) with CLSI quality control (QC) organisms (Staphylococcus aureus ATCC 29213, Enterococcus faecalis ATCC 29212, Streptococcus pneumoniae ATCC 49619, Escherichia coli ATCC 25922, and Haemophilus influenzae ATCC 49247) alongside 10 clinical isolates of each species from the Eurofins Medinet repository (Chantilly, VA). Concurrent inocula of test organisms were used during testing for the comparison of different test conditions. Assays with quality control organisms were run in triplicate. Any change in the MIC value beyond one doubling dilution of that observed under standard CLSI conditions was noted, and essential agreement was defined as MIC values at or within one doubling dilution of standard. For E. faecalis, hazy growth at concentrations below the MIC was observed for all tetracyclines, and MIC values were defined at the lowest concentration producing a clear well.
Eravacycline was synthesized at Tetraphase Pharmaceuticals (1). Tigecycline (Thermo Fisher, Cambridge, MA) and tetracycline (Sigma-Aldrich, St. Louis, MO) were used as comparators. Antibiotic panels contained either cation-adjusted Mueller-Hinton broth (CA-MHB) (Difco; BD, Franklin Lakes, NJ) reconstituted from powder on the day of testing (fresh CA-MHB) or CA-MHB aged on the benchtop at room temperature for 2 weeks. Also, a set of fresh CA-MHB panels were frozen at −70°C for 2 weeks prior to use. Testing by broth microdilution was compared to that by agar dilution in Mueller-Hinton agar (BBL and Difco; BD). Nonstandard assay parameters evaluated for broth microdilution testing included the following: Haemophilus test medium (Thermo Fisher, Cambridge, MA, or prepared in-house), added human serum (5% or 10%; Bioreclamation, Westbury, NY) or lysed horse blood (Innovative Research, Novi, MI), altered pH (6.0 and 8.0), additional calcium (25 mg/liter Ca2+), added polysorbate (0.002%), carbon dioxide (5%), and altered inoculum size (5 × 104 CFU/ml and 5 × 106 CFU/ml).
The overall results showed that eravacycline MIC values in aged medium were unchanged or within one doubling dilution of the MIC values in fresh medium for 92.3% of all tested clinical E. coli, S. aureus, and E. faecalis isolates and the QC strains (Table 1). By organism, essential agreement of the eravacycline MIC values between fresh versus aged medium was seen for 100%, 92.3%, and 84.6% of E. coli, S. aureus, and E. faecalis isolates, respectively. Significantly less agreement was observed for tigecycline at 76.9% and 30.8% for E. coli and E. faecalis, respectively; however, 100% agreement was observed for S. aureus. The tetracycline MIC values were in 100% agreement for all organisms. Two E. faecalis isolates showing uncharacteristically poor agreement for eravacycline (≥+3 log2 difference between fresh versus aged medium) were retested in new batches of aged and fresh MHB in duplicate. The retesting results showed that the original eravacycline values were likely aberrant, and the essential agreement for E. faecalis was changed to 100%, while the agreements for tetracycline (100%) and tigecycline (30.8%) remained unchanged (see Table 1, footnote b).
TABLE 1.
Comparison of MIC values for isolates of E. coli, S. aureus, and E. faecalis using fresh versus aged CA-MHB
| Organism and drug | No.a | Result for aged vs fresh medium: |
Essential agreementb | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Log2 difference |
% log2 difference |
|||||||||||||||
| ≥−3 | −2 | −1 | 0 | +1 | +2 | ≥+3 | ≥−3 | −2 | −1 | 0 | +1 | +2 | ≥+3 | |||
| Overall | ||||||||||||||||
| Eravacycline | 39 | 3 | 22 | 11 | 1 | 2 | 7.7 | 56.4 | 28.2 | 2.6 | 5.1 | 92.3 | ||||
| Tetracycline | 29 | 5 | 23 | 1 | 17.2 | 79.3 | 3.4 | 100.0 | ||||||||
| Tigecycline | 39 | 2 | 25 | 10 | 2 | 5.1 | 64.1 | 25.6 | 5.1 | 69.2 | ||||||
| E. coli | ||||||||||||||||
| Eravacycline | 13 | 1 | 8 | 4 | 7.7 | 61.5 | 30.8 | 100.0 | ||||||||
| Tetracycline | 7c | 1 | 5 | 1 | 14.3 | 71.4 | 14.3 | 100.0 | ||||||||
| Tigecycline | 13 | 1 | 9 | 3 | 7.7 | 69.2 | 23.1 | 76.9 | ||||||||
| S. aureus | ||||||||||||||||
| Eravacycline | 13 | 1 | 9 | 2 | 1 | 7.7 | 69.2 | 15.4 | 7.7 | 92.3 | ||||||
| Tetracycline | 13 | 3 | 10 | 23.1 | 76.9 | 100.0 | ||||||||||
| Tigecycline | 13 | 1 | 12 | 7.7 | 92.3 | 100.0 | ||||||||||
| E. faecalis | ||||||||||||||||
| Eravacycline | 13 | 1 | 5 | 5 | 2d | 7.7 | 38.5 | 38.5 | 15.4 | 84.6 | ||||||
| Tetracycline | 9e | 1 | 8 | 11.1 | 88.9 | 100.0 | ||||||||||
| Tigecycline | 13 | 4 | 7 | 2 | 30.8 | 53.8 | 15.4 | 30.8 | ||||||||
Number of isolates with defined MIC values available for analysis.
Essential agreement is defined as MIC values at or within one doubling dilution of standard (fresh).
Six isolates were highly tetracycline resistant (MIC of >32 μg/ml) and excluded from the analysis as a log2 fold difference in MIC could not be determined.
Results for two E. faecalis isolates with ≥+3 log2 difference for eravacycline were found to be aberrant. Retesting of these isolates in fresh and aged MHB, respectively, showed fresh/aged MIC values (in μg/ml) of 0.008/0.008 and 0.008/0.016 for eravacycline, 0.03/0.25 and 0.06/0.25 for tigecycline, and 1/1 and >32/>32 for tetracycline. Taking the retest data for all three antibiotics into consideration, essential agreements for eravacycline, tetracycline, and tigecycline were 100%, 100%, and 30.8%, respectively.
Four isolates were highly tetracycline resistant (MIC of >32 μg/ml) and excluded from the analysis as a log2 fold difference in MIC could not be determined.
For all tested clinical E. coli, S. aureus, and E. faecalis isolates and the QC strains, no effects on eravacycline microdilution MIC values were seen for fresh versus frozen medium. No effects on eravacycline MIC values were seen for the microdilution assays conducted with fresh broth versus those for agar dilution assays.
When the eravacycline MIC values were evaluated against the QC strains, 2- to 4-fold decreases were observed for S. pneumoniae at pH 6.0 and E. faecalis at pH 8.0. A 4-fold increase in the eravacycline and tigecycline MIC values was observed only for E. faecalis in 0.002% polysorbate and 5% and 10% human serum (eravacycline only). The variations in inoculum size, incubation in 5% CO2, and supplemental Ca2+ in test medium had no effect on the eravacycline MIC values. The tigecycline MIC values for S. aureus, E. faecalis, and S. pneumoniae were elevated in HTM by 8-, 32- and 8-fold, respectively, while the eravacycline MIC values were unchanged. Further, the tigecycline MIC values against H. influenzae ATCC 49247 were outside the CLSI QC range. These results were likely due to the use of HTM that was not freshly prepared for testing.
In conclusion, the in vitro antibacterial activity of eravacycline appears to be largely unaffected by medium age, medium additives, and other nonstandard assay conditions. In agreement with literature reports, the activity of tigecycline in this study was significantly affected by aged medium (3, 4).
REFERENCES
- 1.Xiao X-Y, Hunt DK, Zhou J, Clark RB, Dunwoody N, Fyfe C, Grossman TH, O'Brien WJ, Plamondon L, Ronn M, Sun C, Zhang W-Y, Sutcliffe JA. 2012. Fluorocyclines. 1. 7-Fluoro-9-pyrrolidinoacetamido-6-demethyl-6-deoxytetracycline: a potent, broad spectrum antibacterial agent. J Med Chem 55:597–605. doi: 10.1021/jm201465w. [DOI] [PubMed] [Google Scholar]
- 2.Clinical Laboratory Standards Institute. 2012. Methods for dilution antimicrobial susceptibility for bacteria that grow aerobically; approved standard, 9th ed CLSI document M07-A9E, vol 32, no. 2 Clinical Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 3.Petersen PJ, Bradford PA. 2005. Effect of medium age and supplementation with biocatalytic oxygen-reducing reagent oxyrase on in vitro activities of tigecycline against recent clinical isolates. Antimicrob Agents Chemother 49:3910–3918. doi: 10.1128/AAC.49.9.3910-3918.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradford PA, Petersen PJ, Young M, Jones CH, Tischler M, O'Connell J. 2005. Tigecycline MIC testing by broth dilution requires use of fresh medium or addition of biocatalytic oxygen-reducing reagent oxyrase to standardize the test method. Antimicrob Agents Chemother 49:3903–3909. doi: 10.1128/AAC.49.9.3903-3909.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clinical Laboratory Standards Institute. 2014. Performance standards for antimicrobial susceptibility testing; 24th informational supplement. CLSI document M100-S24, vol. 34, no. 1 Clinical Laboratory Standards Institute, Wayne, PA. [Google Scholar]


