Abstract
Background
Coagulase-negative Staphylococcus (CoNS) is the most common cause of bloodstream infections (BSI) in hospitalized infants. CoNS BSI is most reliably treated with vancomycin; however, concerns about side effects and promoting resistance often delay empirical vancomycin therapy until culture results become available.
Methods
All infants with CoNS BSI discharged from 348 neonatal intensive care units managed by the Pediatrix Medical Group from 1997–2012 were identified. Empirical vancomycin therapy was defined as vancomycin exposure on the day of the first positive blood culture. Delayed vancomycin therapy was defined as vancomycin exposure 1–3 days after the first positive blood culture. We used multivariable logistic regression with random effects for site to evaluate the association between the use of empirical vancomycin therapy vs. delayed vancomycin therapy and 30-day mortality, controlling for gestational age, small-for-gestational age status, postnatal age on the day of the first positive culture, oxygen requirement, ventilator support, and inotropic support on the day the first positive culture was obtained.
Results
Of the 4364 infants with CoNS BSI, 2848 (65%) were treated with empirical vancomycin. The median postnatal age at first positive culture was 14 days (interquartile range: 9, 21). Unadjusted 30-day mortality was similar for infants treated with empirical vancomycin and infants treated with delayed vancomycin therapy (166/2848 [6%] vs. 69/1516 [4%]; p=0.08). There was no significant difference in 30-day mortality on multivariable analysis (odds ratio: 1.14 [0.84, 1.56]). The median duration of bacteremia was 1 day longer for infants with delayed vancomycin therapy (4 days [interquartile range 2, 6] vs. 3 days [2, 5]; p<0.0001).
Conclusions
The median duration of bacteremia was 1 day longer in infants with CoNS BSI who received delayed vancomycin therapy. Despite this finding, empirical vancomycin therapy for CoNS BSI was not associated with improved mortality.
Keywords: late-onset sepsis, NICU
Coagulase-negative staphylococci (CoNS) are the most common cause of late-onset bloodstream infections (BSI) in hospitalized infants, accounting for 48% of infections.1–3 CoNS BSI has been shown to increase the incidence of intraventricular hemorrhage, retinopathy of prematurity, bronchopulmonary dysplasia, cerebral palsy, and neurodevelopmental impairment.4–6 These long-term complications are associated with increased hospital length of stay and increased costs.7,8
To avoid these complications, infants with suspected infection often receive empirical antibiotic therapy while awaiting culture results. Agents used for empirical antibiotic therapy vary by institution, postnatal age, and clinical symptoms but frequently include vancomycin due to the high risk of CoNS infection.9–11
Vancomycin is used for treatment of infections caused by CoNS and other gram-positive organisms, which are frequently resistant to beta-lactam antibiotics.10 However, use of empirical vancomycin is associated with increased incidence of infections caused by resistant organisms such as vancomycin-resistant Enterococcus and highly resistant enteric gram-negative bacteria.12,13 Moreover, the impact of empirical vancomycin therapy on the outcome of infants with CoNS infections is unknown.
In the current study, we used a large, nationally representative database to evaluate whether empirical vancomycin therapy improves outcomes for infants with CoNS BSI.
METHODS
We identified all infants diagnosed with CoNS BSI in the first 120 days of life discharged from 348 neonatal intensive care units (NICUs) managed by the Pediatrix Medical Group between 1997 and 2012. Data were obtained from an administrative database that prospectively captures information from notes generated by clinicians on all infants cared for by the Pediatrix Medical Group. Data are extracted, de-identified, and stored in the Pediatrix Clinical Data Warehouse.14 Information stored for infants on a daily basis includes maternal history, demographics, medications, laboratory results, microbiology results, diagnoses, and procedures. We excluded infants with major congenital anomalies.
Definitions
We included the first episode of CoNS bacteremia in each infant who met the following criteria: 2 positive blood cultures within 4 days, 3 positive cultures within 7 days, or 4 within 10 days.15 All positive CoNS cultures obtained within 21 days of each other were considered as single infectious episodes. Duration of bacteremia was defined as the time from the first to the last positive CoNS culture within a single episode. Inotropic support was defined as exposure to dopamine, dobutamine, epinephrine, norepinephrine, or milrinone on the day the first positive culture was obtained. Mechanical ventilation was defined as exposure to any invasive mechanical ventilation on the day the first positive culture was obtained. Oxygen supplementation was defined as the administration of any fraction of inspired oxygen >21% on the day the first positive culture was obtained. Small-for-gestational-age status was defined as previously described.16 Vancomycin exposure on the day the first positive CoNS culture was obtained was considered empirical therapy. Delayed vancomycin therapy was defined as vancomycin exposure 1–3 days after the first positive blood culture. Infants who were never given vancomycin or who were started on vancomycin >4 days after the positive culture were excluded. However, we did include these infants in a sensitivity analysis.
To describe empirical vancomycin use by NICU size, we divided NICUs into tertiles based on mean number of discharges per year over the entire study period. The mean number of annual discharges was <122 for small NICUs, 122–291 for medium-sized NICUs, and >291 for large NICUs. The proportion of infants treated with empirical vancomycin annually was determined.
Statistical Analysis
The primary outcome of our study was mortality within 30 days of the first positive CoNS culture. Secondary outcomes were mortality within 7 days from the first positive CoNS culture, mortality prior to hospital discharge, length of hospital stay, and duration of bacteremia. Summary statistics were used to describe all study variables, and chi-square tests of association or Wilcoxon rank sum tests were used to compare the distribution between infants who did or did not receive empirical vancomycin. All predictors significantly associated with the primary outcome were included in the full model. A hierarchical backwards variable selection (significance level for removal = 0.25) was used to select the most parsimonious model. Testing for interactions between empirical vancomycin therapy and all relevant covariates included in the final model was performed. We used the Hausman specification test to evaluate the correlation between a NICU-specific effect and the included covariates. Given that the test failed to reject the null hypothesis for each outcome modelled, we opted to use mixed models with random effects for site for our primary analysis. The following main effects were included in the final model as covariates: gestational age, small-for-gestational age status, postnatal age on the day of first positive culture, oxygen requirement, ventilator support, and inotropic support on the day the first positive culture was obtained. Statistical significance was set at p<0.05. Statistical analyses were performed using Stata 12 (College Station, TX). This study was approved by the Duke University Institutional Review Board.
RESULTS
Infant Characteristics
We identified 4364 (0.5%) infants with CoNS BSI out of a total of 887,910 infants. Over half of all infants were treated with empirical vancomycin (2848/4364, 65%) (Table 1). Of the 1516 (35%) infants who received delayed vancomycin therapy, 1016/1516 (67%) were started on vancomycin after 1 day, 292/1516 (19%) after 2 days, 96/1516 (6%) after 3 days, and 34/1516 (2%) after 4 days from the day of the first positive culture. Among infants receiving delayed treatment, vancomycin was started at a median of 1 day (interquartile range 1, 2) following collection of the first positive blood culture. The most common antibiotics used empirically in the delayed vancomycin therapy group were ampicillin, oxacillin, and gentamicin.
TABLE 1.
Demographics
| Delayed therapy N=1516 (%) |
Empirical therapy N=2848 (%) |
|
|---|---|---|
| Gestational age, weeks | ||
| <25 | 517 (34) | 1028 (36) |
| 26–28 | 590 (39) | 1058 (37) |
| 29–32 | 311 (20) | 605 (21) |
| 33–36 | 61 (4) | 102 (4) |
| >37 | 37 (2) | 52 (2) |
| Birth weight, g | ||
| <1000 | 966 (64) | 1842 (65) |
| 1000–1499 | 375 (25) | 741 (26) |
| 1500–2499 | 129 (9) | 205 (7) |
| 2500–3499 | 33 (2) | 39 (1) |
| >3500 | 11 (1) | 21 (1) |
| Age at positive blood culture, days | ||
| <7 | 286 (12) | 90 (3) |
| 7–14 | 969 (41) | 1298 (44) |
| 15–28 | 736 (31) | 1071 (37) |
| >28 | 397 (17) | 467(16) |
| Race/ethnicity | ||
| White | 667 (46) | 1254 (46) |
| African-American | 372 (25) | 735 (27) |
| Hispanic | 360 (24) | 652 (24) |
| Other | 67 (4) | 107 (4) |
| Male | 803 (53) | 1534 (54) |
| Inborn | 1185 (79) | 2297 (82) |
| Cesarean section | 1038 (69) | 2006 (71) |
| Small for gestational age | 276 (18) | 547 (19) |
| Inotropic support on day of culture | 121 (8) | 302 (11) |
| Oxygen support on day of culture | 1049 (69) | 2058 (72) |
| Ventilator support on day of culture | 733 (49) | 1565 (55) |
The difference in median postnatal age at the time of the first positive blood culture for CoNS in infants treated with empirical vancomycin versus infants with CoNS sepsis who received delayed vancomycin was statistically significant: 14 days (10, 22) vs. 13 days (9, 21), respectively, p<0.001. Gestational age at birth and birth weight were similar between empirical vancomycin and delayed vancomycin groups: 27 weeks (25, 29) vs. 27 weeks (25, 29), p=0.21, and 860 g (673, 1130) vs. 865 g (685, 1145), p=0.18, respectively. The majority of infants in both groups were very-low-birth-weight with 2583/2848 (91%) infants who received empirical vancomycin and 1341/1514 (88%) who received delayed vancomycin therapy weighing <1500 g at birth.
Outcomes
On multivariable analysis, the odds of mortality at 30 days were not different between the infants who received delayed vancomycin therapy vs. those who received empirical vancomycin therapy (odds ratio [OR]: 1.14 [95% confidence interval {CI}: 0.84, 1.56]) (Table 2). Odds of mortality at 7 days and at hospital discharge were not significantly different in infants treated with delayed vs. empirical vancomycin (OR: 1.10 [0.67, 1.82] and OR: 1.06 [0.81, 1.39], respectively) (Table 2). A sensitivity analysis that included infants with CoNS BSI who received vancomycin 5 or more days after the culture was obtained and those who never received vancomycin resulted in similar odds of mortality at 30 days (OR: 0.96 [0.62, 1.49]), at 7 days (OR: 0.83 [0.35, 1.96]), and at hospital discharge (OR: 0.92 [0.63, 1.35]). The median duration of bacteremia was 1 day less for infants receiving empirical therapy (3 days [2, 5]) compared with those receiving delayed vancomycin therapy (4 days [2, 6]; p<0.0001). The median duration of vancomycin therapy was 2 days longer for infants receiving empirical vancomycin therapy (15 days [11, 22]) compared with those receiving delayed vancomycin therapy (13 days [11, 19]; p<0.0001). Median length of stay was similar for infants in both groups: 78 days (52, 106) for empirical vancomycin vs.77 days (50, 106) for delayed vancomycin, p=0.35.
TABLE 2.
Mortality by Type
| Delayed therapy N=1516 (%) |
Empirical therapy N=2848 (%) |
Adjusted odds ratio (95% CI)* | |
|---|---|---|---|
| Death within 30 days of 1st culture | 69 (4) | 166 (6) | 1.14 (0.84, 1.56) |
| Death within 7 days of 1st culture | 23 (2) | 54 (2) | 1.10 (0.67, 1.82) |
| Death before hospital discharge | 100 (8) | 236 (9) | 1.06 (0.81, 1.39) |
Odds for empirical vancomycin therapy compared to delayed vancomycin therapy.
CI, confidence interval.
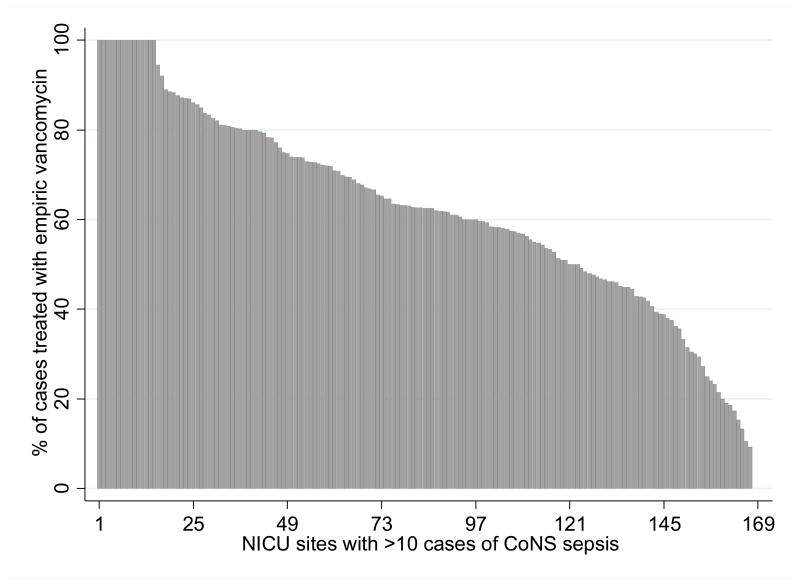
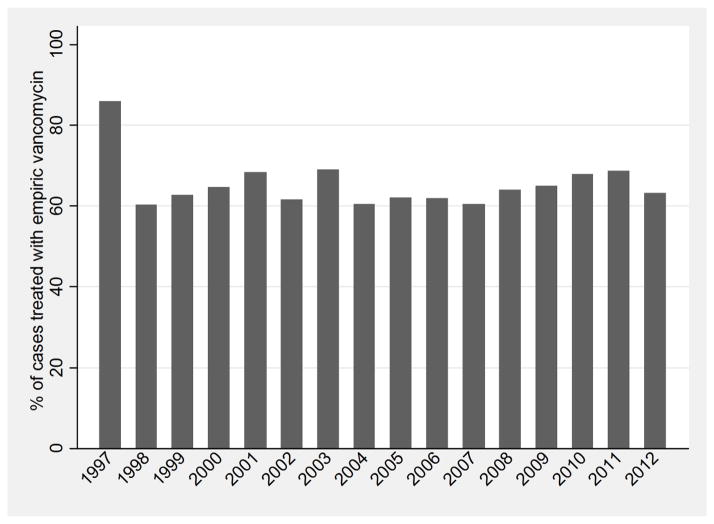
Variation by NICU and Discharge Year
Empirical vancomycin use for CoNS BSI varied greatly by NICU site. At sites with >10 episodes of CoNS BSI, use of empirical vancomycin ranged from 8–100% (Figure 1). Small NICUs (570/822 [69%]) used empirical vancomycin for treatment of CoNS sepsis more often than medium-sized (895/1406 [64%]) or large NICUs (1383/2136 [65%]) (p=0.02). The year of discharge did not significantly affect the use of empirical vancomycin (Figure 2). In 1998, 41/74 (55%) of CoNS sepsis episodes were treated with empirical vancomycin. In 2012, 119/189 (63%) received empirical vancomycin (p=0.05).
FIGURE 1.
Proportion of CoNS BSI cases treated with empirical vancomycin at NICU sites with >10 cases of CoNS sepsis.
FIGURE 2.
Proportion of CoNS BSI cases treated with empirical vancomycin by year of discharge.
DISCUSSION
Vancomycin is often necessary for treatment of CoNS due to frequent resistance to beta-lactam antibiotics.10,11 However, vancomycin exposure is associated with renal dysfunction, hearing loss, and other side effects.17–19 Additionally, widespread use of vancomycin is associated with vancomycin-resistant Enterococcus, invasive Candida infections, and more frequent colonization with resistant gram-negative rods.12,20,21 As much as 32% of vancomycin use in the NICU is inappropriate, largely due to continuation in the setting of negative cultures.22 Vancomycin is commonly used in the NICU and is the third most commonly used drug in infants <32 weeks gestation.23 Limiting unnecessary vancomycin use is a priority.13 For infants in this nationally representative cohort, the use of empirical vancomycin did not improve mortality following an episode of CoNS BSI. The duration of bacteremia was 1 day longer for infants receiving delayed vancomycin therapy.
A prior study evaluating outcomes following sepsis comparing adequate empirical antibiotic therapy to inadequate therapy found that adequate empirical therapy significantly increased the number of infants who survived, from 12/33 (36%) to 7/12 (75%) (OR=5.3 [1.2, 23.2]).24 However, this study considered all organisms, including gram-negative rods, together, and vancomycin was part of the standard empirical protocol for all infants >7 days of age. CoNS sepsis occurred in 43% of infants included in the study. Our study evaluated CoNS BSI separately and sought to determine if adequate empirical therapy affects mortality and hospital length of stay for this disease in particular. Empirical vancomycin did not improve mortality or hospital length of stay for our cohort.
Our findings are consistent with other studies of outcomes following CoNS BSI. A multicenter study found that mortality is not increased following gram-positive infections, including CoNS.25 One center retrospectively evaluated infant outcomes following CoNS BSI after changing their standard empirical antibiotic regimen for late-onset sepsis from vancomycin and cefotaxime to oxacillin and gentamicin.26 They found no difference in the incidence of death at 48 hours, with 1 death per 141 sepsis cases when vancomycin was used empirically and 1 death per 136 sepsis cases when oxacillin was used empirically. The duration of bacteremia was also the same between the 2 periods.
Another study, conducted in the era of increased methicillin-resistant Staphylococcus aureus (MRSA) colonization and disease, demonstrated that vancomycin use could be significantly restricted in the NICU without increasing mortality or morbidity.27 The incidence of late-onset sepsis was 2.15 per 1000 infant-days prior to vancomycin restriction and 2.65 per 1000 infant-days after the protocol was implemented. The number of deaths due to late-onset sepsis decreased with vancomycin restriction (8.1% to 5.8%). These investigators used an algorithm for vancomycin use that waited until CoNS susceptibility results were available prior to starting vancomycin. Our current study supports this practice.
We expected the year of discharge to be associated with increasing empirical vancomycin use. With the incidence of community-acquired MRSA increasing since the 1990s, some centers moved to include vancomycin therapy as part of their standard antibiotic protocol for late-onset sepsis.9 We observed a trend toward increased use of empirical vancomycin for infants with CoNS BSI over the 16-year study period but this did not reach statistical significance. As annual use was analyzed in aggregate, this may not reflect increases in use at individual centers or in communities with higher burdens of MRSA disease.
Balancing the opposing goals of providing the narrowest antimicrobial coverage possible while potentially treating the yet-unknown infecting organism is difficult. Use of broad-spectrum antibiotics for empirical therapy in the NICU has been linked to adverse outcomes and increased mortality.28–30 Increased incidence of resistant organisms is also a known consequence of routine broad-spectrum antibiotic use.31 However, inadequate early antibiotic coverage may increase mortality and sequelae from certain pathogens. For example, late-onset sepsis caused by Pseudomonas species or Candida species significantly increases the odds of death (OR: 14 and OR: 6, respectively).32 Many empirical antimicrobial regimens lack significant coverage for these organisms, which may contribute to this increased mortality. In the case of Candida, empirical antifungal therapy reduces the risk of death and neurodevelopmental impairment (OR: 0.27).33
The current study demonstrates that empirical therapy for CoNS BSI does not significantly improve mortality. This large sample size allowed us to control for important cofounders. We were limited in our ability to assess for long-term complications such as neurodevelopmental impairment, which is associated with CoNS BSI in premature infants. Another limitation is the lack of dosing information; it is possible that different doses of vancomycin could affect mortality. Additionally, the absence of vancomycin therapy was used as a surrogate for inappropriate antibiotic therapy for CoNS due to frequent resistance to beta-lactam antibiotics. However, this resistance pattern is not universal, and this assumption may lead to an underestimation of the difference between the 2 groups. Lack of sensitivity data prevented us from making a direct comparison of appropriate to inappropriate therapy.
Conclusion
Empirical vancomycin therapy does not improve short-term mortality or reduce hospital length of stay following CoNS BSI. This finding can inform decision-making for clinicians seeking to strike a balance between the risks of vancomycin exposure and potential complications of delayed therapy for this common pathogen. Empirical use of vancomycin should be limited to cases when MRSA is suspected. In most cases, culture and sensitivity data should guide use.
Acknowledgments
Source of funding:
This research was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award number UM1AI104681.
Dr. Ericson receives support from the National Institute of Child Health and Human Development of the National Institutes of Health under award number 5T32HD060558. Dr. Benjamin receives support from the United States government for his work in pediatric and neonatal clinical pharmacology (1R01HD057956-05, 1K24HD058735-05, UL1TR001117, and NICHD contract HHSN275201000003I) and the nonprofit organization Thrasher Research Fund for his work in neonatal candidiasis (www.thrasherresearch.org); he also receives research support from industry for neonatal and pediatric drug development (www.dcri.duke.edu/research/coi.jsp). Dr. Fowler receives salary support for research from the National Institutes of Health (K24AI093969, 2R01AI068804, and NO1AI90023); he also served as chair of V710 Scientific Advisory Committee (Merck), has received grant support from Cerexa, Pfizer, Advanced Liquid Logic, MedImmune, and Cubist (grant pending), has been a paid consultant for Merck, Astellas, Affinium, Theravance, Bayer, Cubist, Cerexa, Durata, Pfizer, NovaDigm, Novartis, Medicines Company, Biosynexus, MedImmune, and Inimex, and has received honoraria from Merck, Astellas, Cubist, Pfizer, Theravance, and Novartis. Dr. Hornik receives salary support for research from the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR001117). Dr. Cohen-Wolkowiez receives support for research from the National Center for Advancing Translational Sciences (UL1TR001117), the Food and Drug Administration (1U01FD004858-01), the Biomedical Advanced Research and Development Authority (BARDA) (HHSO100201300009C), the nonprofit organization Thrasher Research Fund (www.thrasherresearch.org), and from industry for drug development in adults and children (www.dcri.duke.edu/research/coi.jsp). Dr. Smith receives salary support for research from the National Institutes of Health and the National Center for Advancing Translational Sciences of the NIH (HHSN267200700051C, HHSN275201000003I, and UL1TR001117); he also receives research support from industry for neonatal and pediatric drug development (www.dcri.duke.edu/research/coi.jsp).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Boghossian NS, Page GP, Bell EF, et al. Late-onset sepsis in very low birth weight infants from singleton and multiple-gestation births. J Pediatr. 2013;162:1120–1124. doi: 10.1016/j.jpeds.2012.11.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ascher SB, Smith PB, Clark RH, et al. Sepsis in young infants with congenital heart disease. Early Hum Dev. 2012;88 (Suppl 2):S92–97. doi: 10.1016/S0378-3782(12)70025-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2 Pt 1):285–291. doi: 10.1542/peds.110.2.285. [DOI] [PubMed] [Google Scholar]
- 4.Mularoni A, Madrid M, Azpeitia A, Valls ISA. The role of coagulase-negative staphylococci in early-onset sepsis in a large European cohort of very low birth weight infants. Pediatr Infect Dis J. 2014;33:e121–125. doi: 10.1097/INF.0000000000000175. [DOI] [PubMed] [Google Scholar]
- 5.Liljedahl M, Bodin L, Schollin J. Coagulase-negative staphylococcal sepsis as a predictor of bronchopulmonary dysplasia. Acta Paediatr. 2004;93:211–215. doi: 10.1080/08035250310008168. [DOI] [PubMed] [Google Scholar]
- 6.Stoll BJ, Hansen NI, Adams-Chapman I, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004;292:2357–2365. doi: 10.1001/jama.292.19.2357. [DOI] [PubMed] [Google Scholar]
- 7.Payne NR, Carpenter JH, Badger GJ, Horbar JD, Rogowski J. Marginal increase in cost and excess length of stay associated with nosocomial bloodstream infections in surviving very low birth weight infants. Pediatrics. 2004;114:348–355. doi: 10.1542/peds.114.2.348. [DOI] [PubMed] [Google Scholar]
- 8.Freeman J, Epstein MF, Smith NE, Platt R, Sidebottom DG, Goldmann DA. Extra hospital stay and antibiotic usage with nosocomial coagulase-negative staphylococcal bacteremia in two neonatal intensive care unit populations. Am J Dis Child. 1990;144:324–329. doi: 10.1001/archpedi.1990.02150270074029. [DOI] [PubMed] [Google Scholar]
- 9.Rubin LG, Sanchez PJ, Siegel J, Levine G, Saiman L, Jarvis WR. Evaluation and treatment of neonates with suspected late-onset sepsis: a survey of neonatologists’ practices. Pediatrics. 2002;110:e42. doi: 10.1542/peds.110.4.e42. [DOI] [PubMed] [Google Scholar]
- 10.Qu Y, Daley AJ, Istivan TS, Garland SM, Deighton MA. Antibiotic susceptibility of coagulase-negative staphylococci isolated from very low birth weight babies: comprehensive comparisons of bacteria at different stages of biofilm formation. Ann Clin Microbiol Antimicrob. 2010;9:16. doi: 10.1186/1476-0711-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawrence SL, Roth V, Slinger R, Toye B, Gaboury I, Lemyre B. Cloxacillin versus vancomycin for presumed late-onset sepsis in the neonatal intensive care unit and the impact upon outcome of coagulase-negative staphylococcal bacteremia: a retrospective cohort study. BMC Pediatr. 2005;5:49. doi: 10.1186/1471-2431-5-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ofek-Shlomai N, Benenson S, Ergaz Z, Peleg O, Braunstein R, Bar-Oz B. Gastrointestinal colonization with ESBL-producing Klebsiella in preterm babies—is vancomycin to blame? Eur J Clin Microbiol Infect Dis. 2012;31:567–570. doi: 10.1007/s10096-011-1348-1. [DOI] [PubMed] [Google Scholar]
- 13.Recommendations for preventing the spread of vancomycin resistance. Recommendations of the Hospital Infection Control Practices Advisory Committee (HICPAC) MMWR. 1995;44(RR-12):1–13. [PubMed] [Google Scholar]
- 14.Spitzer AR, Ellsbury DL, Handler D, Clark RH. The Pediatrix BabySteps Data Warehouse and the Pediatrix QualitySteps improvement project system—tools for “meaningful use” in continuous quality improvement. Clin Perinatol. 2010;37:49–70. doi: 10.1016/j.clp.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 15.Jean-Baptiste N, Benjamin DK, Jr, Cohen-Wolkowiez M, et al. Coagulase-negative staphylococcal infections in the neonatal intensive care unit. Infect Control Hosp Epidemiol. 2011;32:679–686. doi: 10.1086/660361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–224. doi: 10.1542/peds.2009-0913. [DOI] [PubMed] [Google Scholar]
- 17.McKamy S, Hernandez E, Jahng M, Moriwaki T, Deveikis A, Le J. Incidence and risk factors influencing the development of vancomycin nephrotoxicity in children. J Pediatr. 2011;158:422–426. doi: 10.1016/j.jpeds.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 18.Vella-Brincat JW, Begg EJ, Robertshawe BJ, Lynn AM, Borrie TL, Darlow BA. Are gentamicin and/or vancomycin associated with ototoxicity in the neonate? A retrospective audit. Neonatology. 2011;100:186–193. doi: 10.1159/000324857. [DOI] [PubMed] [Google Scholar]
- 19.Robertson CM, Tyebkhan JM, Peliowski A, Etches PC, Cheung PY. Ototoxic drugs and sensorineural hearing loss following severe neonatal respiratory failure. Acta Paediatr. 2006;95:214–223. doi: 10.1080/08035250500294098. [DOI] [PubMed] [Google Scholar]
- 20.Iosifidis E, Evdoridou I, Agakidou E, et al. Vancomycin-resistant Enterococcus outbreak in a neonatal intensive care unit: epidemiology, molecular analysis and risk factors. Am J Infect Control. 2013;41:857–861. doi: 10.1016/j.ajic.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Zaoutis TE, Prasad PA, Localio AR, et al. Risk factors and predictors for candidemia in pediatric intensive care unit patients: implications for prevention. Clin Infect Dis. 2010;51:e38–45. doi: 10.1086/655698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel SJ, Oshodi A, Prasad P, Delamora P, Larson E, Zaoutis T, Paul DA, Saiman L. Antibiotic use in neonatal intensive care units and adherence with Centers for Disease Control and Prevention 12 step campaighn to prevent antimicrobial resistance. Pediatr Infect Dis J. 2009;28:1047–51. doi: 10.1097/INF.0b013e3181b12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark RH, Bloom BT, Spitzer AR, Gerstmann DR. Reported medication use in the neonatal intensive care unit: data from a large national data set. Pediatrics. 2006;117:1979–1987. doi: 10.1542/peds.2005-1707. [DOI] [PubMed] [Google Scholar]
- 24.Apisarnthanarak A, Holzmann-Pazgal G, Hamvas A, Olsen MA, Fraser VJ. Antimicrobial use and the influence of inadequate empiric antimicrobial therapy on the outcomes of nosocomial bloodstream infections in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2004;25:735–741. doi: 10.1086/502469. [DOI] [PubMed] [Google Scholar]
- 25.Benjamin DK, DeLong E, Cotten CM, Garges HP, Steinbach WJ, Clark RH. Mortality following blood culture in premature infants: increased with gram-negative bacteremia and candidemia, but not gram-positive bacteremia. J Perinatol. 2004;24:175–180. doi: 10.1038/sj.jp.7211068. [DOI] [PubMed] [Google Scholar]
- 26.Karlowicz MG, Buescher ES, Surka AE. Fulminant late-onset sepsis in a neonatal intensive care unit, 1988–1997, and the impact of avoiding empiric vancomycin therapy. Pediatrics. 2000;106:1387–1390. doi: 10.1542/peds.106.6.1387. [DOI] [PubMed] [Google Scholar]
- 27.Chiu CH, Michelow IC, Cronin J, Ringer SA, Ferris TG, Puopolo KM. Effectiveness of a guideline to reduce vancomycin use in the neonatal intensive care unit. Pediatr Infect Dis J. 2011;30:273–278. doi: 10.1097/INF.0b013e3182011d12. [DOI] [PubMed] [Google Scholar]
- 28.Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK., Jr The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics. 2006;118:717–722. doi: 10.1542/peds.2005-2677. [DOI] [PubMed] [Google Scholar]
- 29.Cotten CM, Taylor S, Stoll B, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66. doi: 10.1542/peds.2007-3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clark RH, Bloom BT, Spitzer AR, Gerstmann DR. Empiric use of ampicillin and cefotaxime, compared with ampicillin and gentamicin, for neonates at risk for sepsis is associated with an increased risk of neonatal death. Pediatrics. 2006;117:67–74. doi: 10.1542/peds.2005-0179. [DOI] [PubMed] [Google Scholar]
- 31.de Man P, Verhoeven BA, Verbrugh HA, Vos MC, van den Anker JN. An antibiotic policy to prevent emergence of resistant bacilli. Lancet. 2000;355:973–978. doi: 10.1016/s0140-6736(00)90015-1. [DOI] [PubMed] [Google Scholar]
- 32.Tsai MH, Hsu JF, Chu SM, et al. Incidence, clinical characteristics and risk factors for adverse outcome in neonates with late-onset sepsis. Pediatr Infect Dis J. 2014;33:e7–13. doi: 10.1097/INF.0b013e3182a72ee0. [DOI] [PubMed] [Google Scholar]
- 33.Greenberg RG, Benjamin DK, Jr, Gantz MG, et al. Empiric antifungal therapy and outcomes in extremely low birth weight infants with invasive candidiasis. J Pediatr. 2012;161:264–269. doi: 10.1016/j.jpeds.2012.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]