Abstract
Background
Mosquito-borne Rift Valley fever virus (RVFV) causes acute, often severe, disease in livestock and humans. To determine the exposure factors and range of symptoms associated with human RVF, we performed a population-based cross-sectional survey in six villages across a 40 km transect in northeastern Kenya.
Methodology/Principal Findings:
A systematic survey of the total populations of six Northeastern Kenyan villages was performed. Among 1082 residents tested via anti-RVFV IgG ELISA, seroprevalence was 15% (CI95%, 13–17%). Prevalence did not vary significantly among villages. Subject age was a significant factor, with 31% (154/498) of adults seropositive vs. only 2% of children ≤15 years (12/583). Seroprevalence was higher among men (18%) than women (13%). Factors associated with seropositivity included a history of animal exposure, non-focal fever symptoms, symptoms related to meningoencephalitis, and eye symptoms. Using cluster analysis in RVFV positive participants, a more severe symptom phenotype was empirically defined as having somatic symptoms of acute fever plus eye symptoms, and possibly one or more meningoencephalitic or hemorrhagic symptoms. Associated with this more severe disease phenotype were older age, village, recent illness, and loss of a family member during the last outbreak. In multivariate analysis, sheltering livestock (aOR = 3.5 CI95% 0.93–13.61, P = 0.065), disposing of livestock abortus (aOR = 4.11, CI95% 0.63–26.79, P = 0.14), and village location (P = 0.009) were independently associated with the severe disease phenotype.
Conclusions/Significance
Our results demonstrate that a significant proportion of the population in northeastern Kenya has been infected with RVFV. Village and certain animal husbandry activities were associated with more severe disease. Older age, male gender, herder occupation, killing and butchering livestock, and poor visual acuity were useful markers for increased RVFV infection. Formal vision testing may therefore prove to be a helpful, low-technology tool for RVF screening during epidemics in high-risk rural settings.
Author Summary
Rift Valley fever virus (RVFV) causes serious disease in both animals and humans. Large-scale outbreaks result in devastating economic losses and create many urgent public health concerns. Among humans, the symptoms of RVF are variable, having a broad spectrum of disease that ranges from mild to severe fever symptoms, and can include ocular complications, encephalitis, and sometimes hemorrhagic disease. In this study, 1082 at-risk Kenyan subjects were serum antibody-tested for evidence of prior RVFV infection and their demographic, health, and exposure data were collated. Seroprevalence was moderately high across the study area (15%) but did not differ significantly among villages across the study region. Age, gender, and herding occupation were all significantly associated with being RVFV seropositive. Older age, village and certain animal husbandry activities were associated with more severe disease. Poor visual acuity was more likely in the seropositive group. This better definition of risk factors and associated symptom complexes should prove helpful for RVF screening during future outbreaks in high-risk rural settings.
Introduction
Rift Valley fever virus (RVFV) is a mosquito-borne zoonotic disease that poses a significant risk to human health in endemic regions of Africa and the Middle East [1]. Epizootics usually precede epidemics and can result in large-scale abortion storms in local livestock populations [2]. These RVFV outbreaks in human and animal populations result in significant economic damage from trade embargos and significant livestock losses in affected areas [3]. Recent data also demonstrate that RVFV can be transmitted to humans during interepidemic periods [4–6]. RVFV infection is categorized as a neglected tropical disease due to the fact that RVFV disproportionately affects resource-limited semi-nomadic herding communities, is poverty promoting, and has long-lasting sequelae [5]. Additionally, RVF is expanding its range, threatening other areas of the world as an emerging infectious disease; notably, both Europe and the United States have the necessary vectors and livestock reservoirs to sustain autochthonous RVFV transmission [7,8]. The severity of RVFV manifestation, its devastating economic and public health effects, and its potential to be sustained in new regions make the study of RVFV transmission and disease a high priority.
Clinically, most often RVFV causes no symptoms or a mild illness manifesting with fever and liver abnormalities [4]. More rarely, RVFV is known to cause cases of retinitis, encephalitis, or hemorrhagic diathesis with hepatitis during epidemics [9], but these manifestations are variable and currently unpredictable. Most primary infections are thought to cause only self-limited febrile illness followed by complete recovery. It is not yet clear why severe cases occur- these consist of patients with neurologic dysfunction (up to 8%), and hemorrhagic cases (up to 1%, which is then associated with mortality of up to 50%) [2,4]. Furthermore, RVFV causes visual disturbances including reversible anterior uveitis (up to 30% of cases), and permanent retinitis (up to 20%) [10]. This broad spectrum of human RVF disease has been most recently confirmed in investigations of the 2006–2007 epidemics in East Africa [9]. Outbreaks in NE Kenya (Garissa County) were reported during the last epidemic [2], but RVFV activity in nearby Ijara constituency (Masalani and Sangailu), was not specifically monitored. Other reports have shown evidence of interepidemic human RVFV transmission in Ijara constituency (Masalani)[5–6]. It has been suggested that clinical phenotype of disease may be in part determined by the route of RVFV transmission, with animal-related transmission likely to be more severe than mosquito borne disease [1]. To expand this knowledge, the goal of the present study was to identify the exposures and other risk factors associated with human RVFV transmission and disease severity in a typical East African endemic setting, the Ijara constituency, Sangailu location, Kenya.
Methods
Ethics statement
All participants provided written consent under a protocol approved by the Human Investigations Review Board of University Hospitals Case Medical Center (No. 11–09–01) and the Ethical Review Committee of the Kenya Medical Research Institute, Nairobi, Kenya (Non-SSC Protocol No. 195). Before participation, written informed consent was obtained from adult study subjects, and parents provided written informed consent for their participating children. Children over 7 years of age also provided individual assent.
Location
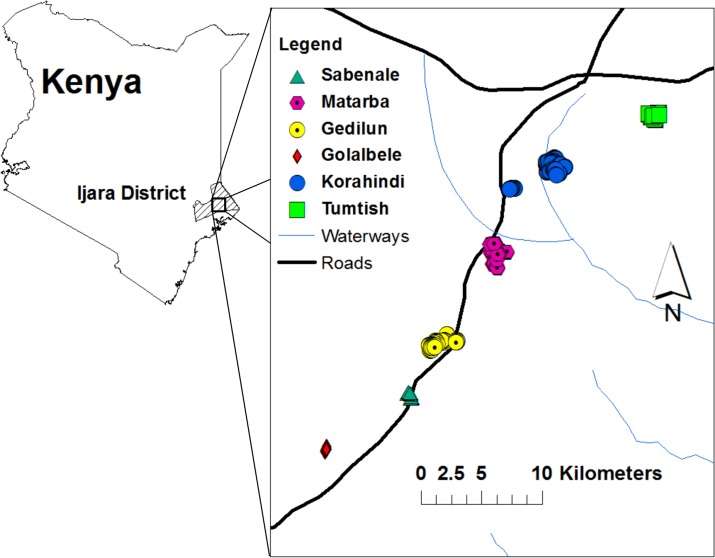
This study was performed in the semi-arid Sangailu Location of Ijara constituency, Kenya. Six villages (Golabele, Sabenale, Gedilun, Matarba, Korahindi, and Tumtish) were sampled for demographic, epidemiological, and health information during area-wide household surveys performed from August through November of 2011, five years after the last known RVF epidemic in the area (2006–2007). The villages are located off a main road across a span of approximately 40 Km, in a transect running southwest to northeast (Fig. 1) centered around coordinates 1 deg. 19 min S, 40 deg. 44 min E. The northern-most village, Tumtish, is located 39 Km from the border with Somalia. The participating populations studied were comprised predominantly of herders and semi-nomadic pastoralists of Somali ethnicity. A typical household landscape is shown in Fig. 2. For unique identification and subsequent analysis of the spatial distribution of RVFV serostatus, participating household locations were geo-referenced by Global Positioning System with the use of a Garmin eTrex handheld device (Garmin, Schaffhausen, Switzerland).
Fig 1. Map showing the location of the Sangailu study area in Northeastern Province in Kenya.
The country map, left, indicates the boundaries of Ijara District, the health administration unit at the time of the study (the Sangailu location is now part of Garissa County, Ijara constituency). The inset, right, shows the locations of the six community clusters that were included in the study. These were distributed in a 40 km transect along a main road of the Sangailu area.
Fig 2. Typical peri-domestic landscape in the Sangailu area of Kenya.
Shown are traditional wicker and grass-mat domed houses and outbuildings, surrounded by a planted compound perimeter and local dense brush vegetation.
Participants
Study recruitment began after consultation and approval by local leaders and administrators. After an initial demographic census was performed to determine the current local population and its distribution, a systematic survey of the total populations of six Northeastern Kenyan villages was performed. The villages were systematically surveyed in sequence to reach the desired sample size of >1000 enrolled individuals. All residents were eligible for inclusion, except that those residing in the area for <2 years, and children less than 1 year of age were excluded. The study sample was representative of the local ethnic mix of 99% Kenyan Somali and < 1% Bantu, Indian, or other Asian.
Examination procedures
Participants had formal interviews to detail their demographics, occupation, mosquito exposure, and animal exposure within the last 6 months, and any previous nonspecific symptoms related to RVF in the last 30 days, or severe symptoms at any time (see Supporting S1 Text). Visual acuity testing by use of the Snellen chart and physical exams were performed, with an emphasis on signs of recent or remote RVF. Children under 5 yrs. old (N = 358) were excluded from visual acuity testing. Poor visual acuity was defined as a score less than or equal to 6/9 meters in either eye by standard Snellen eye chart testing. A stratified subset (118) of visually symptomatic and asymptomatic subjects also underwent dilated fundoscopic eye exam and imaging using a retinal camera. Peripheral blood was then collected for serological testing for anti-RVFV IgG.
Laboratory testing
Sera were tested for IgG against RVFV by standardized ELISA protocol [11,12] and confirmed by plaque reduction neutralization testing (PRNT), as previously described [5,6,12–14]. Specimens having an ELISA OD of >0.25 and a PRNT titer of ≥1:20 were considered positive. The confirmatory plaque reduction neutralization testing (PRNT) was performed at the University of Texas, Medical Branch at Galveston.
Statistical methods
Statistical analysis examined the association of subject demographic and exposure factors with two primary outcomes: i) odds of seropositivity and ii) odds of having had the more severe symptoms of RVF. Initial chi-square tests were performed to identify the association of categorical factors with RVFV seropositivity and t-tests were used for continuous variables. A series of nested multivariable logistic regression models were next developed that initially included predictors significant in bivariate comparisons, as well as those considered of biological relevance prior to conduct of the study. Bivariate results and stepwise regression models were used to aid in the selection of variables to be included in the final models. Non-significant variables (p > = 0.10) were removed in stepwise fashion to help identify the variables with the greatest multiply adjusted links to RVFV seropositivity or symptom score. For this analysis, statistical significance was set at the 0.05 level. Following analysis of individual symptoms, a relative RVF severity score was developed using the two-step cluster algorithm in SPSS v. 21 (IBM, Armonk NY, USA) to empirically define significant constellations of milder, moderate, and more severe symptom states among RVFV seropositive subjects [15]. The severe disease phenotype was defined as having somatic symptoms of acute fever plus eye symptoms and possibly one or more meningoencephalitic or hemorrhagic symptoms (S1 Fig). Mild disease phenotype was defined as RVFV seropositivity with few to no symptoms. Multivariate logistic regression models were run using severe vs. mild disease categories and significant variables from bivariate analysis, excluding those variables used to define disease severity. These statistical models were performed using SAS software (SAS Institute Inc. version 9.3, Cary, NC, USA).
Statistical analysis of spatial patterns of seropositivity among the participating households was performed with the use of Point Pattern Analysis software [16] and Clusterseer 2.0 software (Biomedware, Ann Arbor, MI)
Results
Associations with RVFV seropositivity
Of the 1134 participants enrolled in the study, 1082 completed all phases of the examination and were tested for RVFV infection. Of these, 164 were RVFV seropositive (15%; CI95% 13–17%). Males were more likely to be RVFV infected: 18% (79/433) were seropositive compared to 13% (85/646) of females (P = 0.023; Table 1). Adults (≥16 years old) were also more likely than children to be RVFV infected: Thirty-one percent (152/487) of adults were seropositive compared to 2% (12/595) of children (P < 0.001). The average age of seropositive people was 42 ± 19.5 years (range 6–85 years) vs. 17 ± 17 for seronegatives (range 1–84 years). No significant differences in seropositivity were seen among the six villages studied in the Sangailu region: Golabele (17.6%; 15/85), Korahindi (17.0%; 49/288); Sabenale (15.6%; 10/64); Matarba (14.3%; 33/231); Gedilun (13.9%; 32/230), and Tumtish (13.6%; 25/184). This was not surprising given the uniformity of landscape and environmental features, and the socioeconomic homogeneity within pastoralist communities of this region.
Table 1. Results of bivariate analysis to determine the significant relative odds of having anti-RVFV seropositivity according to demographic data, clinical signs, symptoms, and exposure factors.
| Significant Variables | Number tested (N)** | Variable Present (N) | Variable Absent (N) | Variable Missing | Odds Ratio (95% Confidence Interval) | P- Value† |
|---|---|---|---|---|---|---|
| Age (continuous) | 1134 | 1082 | 0 | 0 | 1.06 (1.05–1.07) | <0.0001 |
| Sex (Male as reference) | 1129 | 431 | 646 | 5 | 1.45 (1.07–2.08) | 0.023 |
| Herder Occupation | 1134 | 122 | 960 | 4.95 (3.25–7.54) | <0.0001 | |
| Poor Visual Acuity* | 1134 | 111 | 599 | 372 | 5.08 (3.30–7.82) | <0.0001 |
| Recent ^ Sickness | 1132 | 548 | 533 | 1 | 1.95 (1.37–2.77) | 0.0001 |
| Recent ^ Backache | 1132 | 480 | 601 | 1 | 6.76 (4.48–10.20) | <0.0001 |
| Recent ^ Nausea | 1132 | 290 | 791 | 1 | 2.03 (1.42–2.90) | <0.0001 |
| Recent ^ Malaise | 1132 | 356 | 725 | 1 | 3.87 (2.69–5.55) | <0.0001 |
| History of < Severe Bruising | 1132 | 5 | 1076 | 1 | 8.99 (1.48–54.51) | 0.005 |
| History of < Red Eyes | 1132 | 146 | 935 | 1 | 4.05 (2.70–6.06) | <0.0001 |
| History of < Poor Vision | 1132 | 112 | 969 | 1 | 4.71 (3.01–7.36) | <0.0001 |
| History of < Eyes Sensitive to Light | 1132 | 159 | 922 | 1 | 4.20 (2.71–6.51) | <0.0001 |
| History of < Eye Pain | 1132 | 164 | 917 | 1 | 5.47 (3.66–8.19) | <0.0001 |
| History of < Spinning Feeling | 1132 | 164 | 917 | 1 | 3.13 (2.09–4.69) | <0.0001 |
| History of < Mental confusion | 1132 | 11 | 1070 | 1 | 10.19 (2.90–35.73) | <0.0001 |
| History of < Sleepy Feeling | 1134 | 64 | 1017 | 1 | 1.89 (1.04–3.43) | 0.024 |
| History of < Stiff neck | 1132 | 24 | 1057 | 1 | 5.61 (2.39–13.14) | <0.0001 |
| History of < Seizures | 1132 | 6 | 1075 | 1 | 5.91 (1.17–29.80) | 0.017 |
| Personal history of RVF | 1132 | 11 | 1070 | 1 | 4.81 (1.45–16.01) | 0.005 |
| Sheep contact | 1130 | 959 | 118 | 5 | 2.57 (1.24–5.34) | 0.014 |
| Goat contact | 1130 | 959 | 118 | 5 | 2.57 (1.24–5.34) | 0.014 |
| Cow contact | 1130 | 855 | 221 | 6 | 3.06 (1.74–5.40) | <0.0001 |
| Sheltered livestock | 1130 | 709 | 370 | 3 | 6.10 (3.59–10.35) | <0.0001 |
| Sheltered sheep | 1130 | 698 | 381 | 3 | 5.95 (3.54–9.99) | <0.0001 |
| Sheltered goat | 1130 | 704 | 375 | 3 | 5.82 (3.46–9.80) | <0.0001 |
| Sheltered cow | 1130 | 620 | 459 | 3 | 4.94 (3.15–7.76) | <0.0001 |
| Killed livestock | 1130 | 352 | 727 | 3 | 5.50 (3.65–8.30) | <0.0001 |
| Killed sheep | 1130 | 328 | 751 | 3 | 4.35 (2.90–6.52) | <0.0001 |
| Killed goat | 1130 | 290 | 789 | 3 | 3.53 (2.31–5.39) | <0.0001 |
| Killed cow | 1130 | 271 | 859 | 4 | 2.87 (1.85–4.45) | <0.0001 |
| Butchered livestock | 1130 | 510 | 569 | 3 | 5.20 (3.44–7.85) | <0.0001 |
| Butchered sheep | 1130 | 476 | 603 | 3 | 3.39 (2.32–4.96) | <0.0001 |
| Butchered goat | 1130 | 387 | 692 | 3 | 2.36 (1.62–3.43) | <0.0001 |
| Butchered cow | 1130 | 338 | 741 | 3 | 1.74 (1.18–2.56) | 0.004 |
| Handled raw meat | 1130 | 886 | 193 | 3 | 2.32 (1.33–4.05) | 0.004 |
| Consumed sheep meat | 1130 | 882 | 197 | 3 | 2.40 (1.38–4.19) | 0.003 |
| Consumed goat meat | 1130 | 880 | 199 | 3 | 2.43 (1.39–4.24) | 0.002 |
| Consumed cow meat | 1130 | 805 | 274 | 3 | 1.94 (1.24–3.04) | 0.005 |
| Milked livestock | 1130 | 708 | 371 | 3 | 4.92 (2.97–8.14) | <0.0001 |
| Milked sheep | 1130 | 699 | 380 | 3 | 4.61 (2.83–7.51) | <0.0001 |
| Milked goat | 1130 | 737 | 393 | 4 | 4.88 (2.98–8.01) | <0.0001 |
| Milked cow | 1130 | 606 | 473 | 3 | 4.79 (3.08–7.43) | <0.0001 |
| Cared for birthing animal | 1130 | 632 | 447 | 3 | 5.88 (3.66–9.46) | <0.0001 |
| Birthed sheep | 1130 | 627 | 452 | 3 | 6.07 (3.77–9.77) | <0.0001 |
| Birthed goat | 1130 | 630 | 449 | 3 | 6.35 (3.92–10.31) | <0.0001 |
| Birthed cow | 1130 | 499 | 580 | 3 | 6.02 (3.97–9.15) | <0.0001 |
| Disposed of livestock fetus | 1130 | 608 | 471 | 3 | 5.31 (3.39–8.32) | <0.0001 |
| Disposed of sheep fetus | 1130 | 604 | 475 | 3 | 5.16 (3.31–8.04) | <0.0001 |
| Disposed of goat fetus | 1130 | 607 | 472 | 3 | 5.38 (3.43–8.42) | <0.0001 |
| Disposed of cow fetus | 1130 | 479 | 600 | 3 | 5.05 (3.38–7.54) | <0.0001 |
| Recent family death | 1132 | 65 | 1016 | 1 | 3.22 (1.84–5.64) | <0.0001 |
† As determined by bivariate Χ2 testing
*Poor visual acuity defined functionally at >6/9 meters using a Snellen eye chart
^ “Recent” defined as symptoms reported in the last 30 days
< “History of” defined as symptom reported at any time
** N = number of participants with data collected in survey
From initial bivariate analysis, RVFV seropositivity was significantly associated with multiple environmental exposures, as well as certain physical signs and reported symptoms (see Table 1). After multivariable adjustment, our most parsimonious logistic model of seropositive status found that older age (4% increase per year CI95% 2–9%, p<0.0001), male gender (adjusted Odds Ratio (aOR) = 1.8, CI95% 1.2–2.7, P < 0.01), poor measured visual acuity (aOR = 1.7, CI95% 1.01–3.0, P < 0.05), a history of malaise (aOR = 1.6, CI95% 1.06–2.5, P < 0.03), and a history of killing livestock (aOR = 2.0, CI95% 1.4–3.3, P < 0.001) were each independently associated with seropositivity (Table 2).
Table 2. Significant associations for RVFV seropositivity identified by multivariable logistic regression modeling.
| Variables | Variable Present (N) | Variable Absent (N) | Variable Missing (N) | Multiply-adjusted Odds Ratio (95% Confidence Interval) | P Value |
|---|---|---|---|---|---|
| Age (continuous) | 1082 | 0 | 0 | 1.04 (1.02–1.05) | <.0001 |
| Sex (female as reference) | 431 | 646 | 5 | 1.71 (1.13–2.60) | 0.012 |
| Poor* visual acuity | 111 | 599 | 372 | 1.71 (0.99–2.96) | 0.054 |
| Killed livestock | 352 | 727 | 3 | 1.98 (1.31–3.00) | 0.001 |
| Model R2 = 0.25, Akaike’s information criterion (AIC) = 634.6; Condition index 10.6 | |||||
*Poor visual acuity defined at less than or equal to 6/9
Ten percent (112/1081) of people surveyed self-reported poor vision. Those who were RVFV-infected were more likely to report poor vision: 26% (43/164), as compared to 7.5% (69/917) among uninfected (P < 0.0001). Sixteen percent (111/710) of tested subjects had poor measured visual acuity. Those who were anti-RVFV positive were more likely to have poor measured visual acuity, 36% (57/159) compared to 9.8% (54/551) of seronegatives (P < 0.0001). Fundoscopic exams were performed on 118 study participants. Here, objective eye disease was defined as having uveitis, retinitis, retinal scar or retinal hemorrhage. Overall, 26% (30/118) were found to have eye disease defined as retinitis or retinal hemorrhage. Of those serologically tested for RVFV seropositivity, 21% (6/28) were RVFV seropositive.
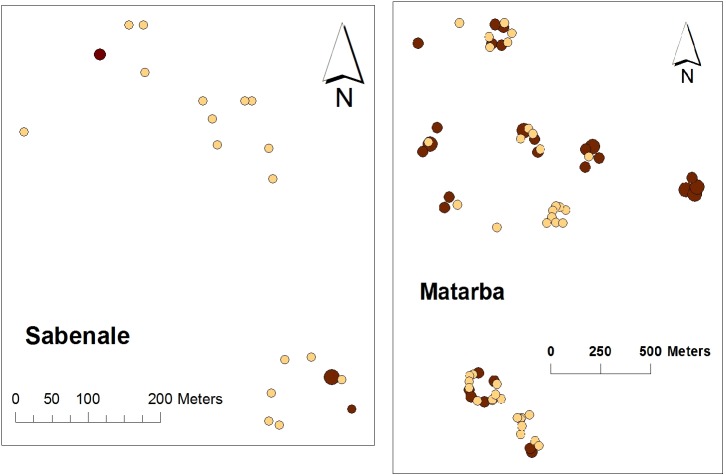
Across the study landscape, we did not find any significant global pattern of clustering for anti-RVFV serostatus beyond the underlying distribution of households in each village (using Ripley’s weighted K-function testing [17] over a range from 50 to 850 meters). However, within Korahindi, Matarba, Tumtish, and Sabenale there was evidence (using the Getis G-statistic [18]) of significant local clustering, at the 25–100 m scale, of greater per-household density of cases within the certain sections of these communities. Most remarkably, it was noted that all of the confirmed RVFV-positive subjects in Sabenale came from just 3 of 20 houses sampled (Fig. 3, left panel). One of these three seropositive houses in Sabenale had 7 seropositive people out of 11 total household residents. Fig. 3‘s right panel indicates the clustering pattern within the Sangailu area’s central village of Matarba.
Fig 3. Map of the distribution of RVFV seropositives for study villages Sabenale and Matarba.
Within each village, circles represent the location of study subjects’ households. Darker shaded circles indicate houses with RVFV seropositive residents. Larger circles indicate that > 50% of residents were seropositive.
Associations with RVF disease severity
One hundred sixty-four people were RVFV exposed and included in this analysis. Ninety-three percent (152/164) were adults and 52% (85/164) were female. Thirty percent (49/164) were from Korahindi, 20% (33/164) from Matarba, 20% (32/164) from Gedilun, 15% (25/164) from Tumtish, 9% (15/164) from Golalbele, and 6% (10/164) from Sabenale. Those in the moderate/severe group (N = 111) were more likely to be older (p = 0.007; mean age 44.9 years vs. 36.13 years) than those in the mild group (N = 53). In bivariate analysis, the most severe of the RVF symptom-cluster phenotypes was associated with older age, village, recent illness, and death of a family member (Table 3). In a multivariable logistic model controlling for age and village, it was found that those who sheltered livestock or disposed of livestock fetuses were at significantly greater risk for having this more severe illness complex (Table 4). Sheltering livestock put one at three and a half times the risk for more severe disease (aOR = 3.5 CI95% 0.93–13.61, P = 0.064). Disposing of livestock abortus put one at four times risk of having a severe disease phenotype (aOR = 4.11, CI95% 0.63–26.79, P = 0.140).
Table 3. Results of bivariate analysis to determine significant relative odds of high RVF disease severity according to demographic data, clinical signs, symptoms, and exposure factors.
| Variable | Variable Present (N) | Variable Absent (N) | Variable Missing (N) | Odds Ratio (95% Confidence Interval) for more severe disease | P Value† |
|---|---|---|---|---|---|
| Age (continuous) | 164 | 0 | 0 | 1.03 (1.01–1.04) | 0.007 |
| Adults (≥16 years old) vs. Children | 152 (adults) | 12 (kids) | 0 | 2.23 (0.69–7.29) | 0.205 |
| Gender (male as reference) | 79 (male) | 85 (female) | 0 | 0.85 (0.44–1.63) | 0.738 |
| Village | 164 | 0 | 0 | 0.010 | |
| Gedilun | 2.10 (0.72–6.12) | ||||
| Golalbele | 1.94 (0.48–7.86) | ||||
| Matarba | 0.85 (0.34–2.14) | ||||
| Sabenale | 4.36 (0.51–37.48) | ||||
| Tumtish | 0.32 (0.12–0.88) | ||||
| Korahindi (ref) | |||||
| Herder occupation | 48 | 116 | 0 | 0.72 (0.36–1.46) | 0.366 |
| Father deceased | 94 | 70 | 0 | 1.84 (0.95–3.57) | 0.091 |
| Mother deceased | 68 | 96 | 0 | 1.41 (0.72–2.78) | 0.397 |
| Recent illness | 106 | 58 | 0 | 3.87 (1.94–7.72) | .0001 |
| Personal history of RVF | 5 | 159 | 0 | 0.71 (0.12–4.37) | 0.659 |
| Sheep contact | 154 | 8 | 2 | 0.59 (0.12–2.97) | 0.280 |
| Goat contact | 154 | 8 | 2 | 0.59 (0.12–2.97) | 0.280 |
| Cow contact | 148 | 14 | 2 | 0.76 (0.23–2.50) | 0.108 |
| Camel contact | 34 | 122 | 8 | 1.13 (0.49–2.58) | 0.956 |
| Sheltered livestock | 143 | 20 | 1 | 1.90 (0.73–4.92) | 0.204 |
| Sheltered sheep | 142 | 21 | 1 | 1.73 (0.68–4.40) | 0.316 |
| Sheltered goat | 142 | 21 | 1 | 1.73 (0.68–4.40) | 0.316 |
| Sheltered cow | 133 | 30 | 1 | 1.08 (0.47–2.52) | 0.832 |
| Killed livestock | 97 | 66 | 1 | 0.88 (0.45–1.73) | 0.736 |
| Killed sheep | 87 | 76 | 1 | 0.97 (0.50–1.88) | 1.00 |
| Killed goat | 73 | 90 | 1 | 0.82 (0.43–1.59) | 0.614 |
| Killed cow | 62 | 101 | 1 | 0.87 (0.44–1.70) | 0.730 |
| Butchered livestock | 124 | 39 | 1 | 1.09 (0.51–2.34) | 0.845 |
| Butchered sheep | 109 | 54 | 1 | 1.10 (0.55–2.21) | 0.859 |
| Butchered goat | 84 | 79 | 1 | 1.09 (0.57–2.11) | 0.867 |
| Butchered cow | 67 | 96 | 1 | 1.04 (0.53–2.04) | 1.00 |
| Handled meat | 147 | 16 | 1 | 0.46 (0.13–1.70) | 0.275 |
| Consumed livestock | 34 | 129 | 1 | 0.51 (0.23–1.11) | 0.100 |
| Consumed sheep | 109 | 54 | 1 | 0.69 (0.21–2.24) | 0.859 |
| Consumed goat | 147 | 16 | 1 | 0.69 (0.21–2.24) | 0.778 |
| Consumed cow | 136 | 27 | 1 | 0.70 (0.28–1.80) | 0.508 |
| Milked an animal | 143 | 20 | 1 | 0.90 (0.33–2.50) | 1.000 |
| Milked sheep | 141 | 22 | 1 | 0.77 (0.28–2.11) | .0806 |
| Milked goat | 142 | 21 | 1 | 0.84 (0.30–2.29) | 0.807 |
| Milked cow | 133 | 30 | 1 | 0.74 (0.30–1.78) | 0.665 |
| Drank animal milk | 159 | 4 | 1 | 2.18 (0.30–15.92) | 0.593 |
| Drank sheep milk | 160 | 3 | 1 | 1.07 (0.09–12.06) | 1.000 |
| Drank goat milk | 161 | 2 | 1 | 2.16 (0.13–35.17) | 0.538 |
| Drank cow milk | 158 | 5 | 1 | 1.44 (0.23–8.89) | 0.654 |
| Birthed an animal | 140 | 23 | 1 | 0.72 (0.27–1.95) | 0.633 |
| Birthed sheep | 140 | 23 | 1 | 0.55 (0.19–1.57) | 0.337 |
| Birthed goat | 141 | 22 | 1 | 0.59 (0.21–1.69) | 0.461 |
| Birthed cow | 125 | 38 | 1 | 0.84 (0.38–1.85) | 0.696 |
| Disposed of fetus | 136 | 27 | 1 | 0.88 (0.36–2.17) | 1.000 |
| Disposed of sheep fetus | 135 | 28 | 1 | 1.01 (0.42–2.42) | 1.000 |
| Disposed of goat fetus | 136 | 27 | 1 | 0.88 (0.36–2.17) | 1.000 |
| Disposed of cow fetus | 118 | 45 | 1 | 1.09 (0.53–2.27) | 0.852 |
| Mosquito net use | 33 | 131 | 0 | 0.68 (0.31–1.49) | 0.405 |
| Recent mosquito bites | 13 | 151 | 0 | 1.08 (0.32–3.68) | 1.000 |
| Mosquito control | 4 | 160 | 0 | 1.44 (0.15–14.22) | 1.000 |
| Lost Family member | 22 | 142 | 0 | 5.60 (1.26–24.95) | 0.013 |
† As determined by bivariate Χ2 testing
Table 4. Significant associations for greater RVF disease severity determined by multivariable logistic regression modeling.
| Variable | Variable Present (N) | Variable Absent (N) | Variable Missing (N) | Multiply-adjusted Odds Ratio (95% Confidence Interval) | P Value |
|---|---|---|---|---|---|
| Age (continuous) | 163 | 0 | 1 | 2.72 (0.74–9.95) | 0.133 |
| Village (Korahindi as reference village) | 163 | 0 | 1 | Gedilun 1.98 (0.64–6.16) | 0.009 |
| Golalbele 1.84 (0.41–8.24) | |||||
| Matarba 1.25 (0.41–3.86) | |||||
| Sabenale 7.34 (0.74–72.73) | |||||
| Tumtish 0.25 (0.09–0.72) | |||||
| Disposed of fetus | 136 | 27 | 1 | 4.11 (0.63–26.79) | 0.140 |
| Birthed livestock | 140 | 23 | 1 | 0.17 (0.02–1.43) | 0.104 |
| Sheltered livestock | 143 | 20 | 1 | 3.55 (0.93–13.61) | 0.065 |
| Model R2 = 0.22, Akaike’s information criterion (AIC) = 196.22; Condition index 12.0; Hosmer and Lemeshow p = 0.50 | |||||
Discussion
A significant proportion of the population in the semi-arid areas of northeastern Kenya have been infected with RVFV. Other than older age, most of the factors significantly associated with anti-RVFV seropositivity and RVF disease severity were related to pastoralist lifestyles and animal exposures. These included the common practices of livestock shelter at home and livestock fetus disposal, as typically observed in this region. During epizootics, RVFV-infected herds will experience abortion storms and affected virus-contaminated abortus is often handled by herders, significantly increasing their risk for RVFV infection by aerosol and direct contact, and possibly, their risk for more severe RVF disease [1]. Similarly, infected animals brought to slaughter provide potential avenues for transmission via direct blood contact or aerosolization. Animal husbandry exposures were similar in each of the studied villages, which may explain the lack of difference in seropositivity among villages. No empiric global clustering effect was observed for household anti-RVFV seroprevalence across the study landscape, but within some villages, significant local clustering of seropositive households was documented and severe disease manifestations were more common in certain villages than others. It seems that, within certain communities, a few high-risk households carry the burden of RVFV infection, perhaps defined by combined eco-social landscape factors. Between the identified high-risk households, differences in animal husbandry practices could not be determined, but their (unmeasured) animal herd seropositivity could have differed, leading to greater individual household exposures. Other factors such as socioeconomic status and local landscape (vegetation and soil) may have also played a role in exposure risk variation as seen in the last RVFV Kenyan outbreak [19], but these were not measured in our study.
As noted in other studies, RVFV seropositivity rates were much lower among children [5,6,12]. Although there is a built-in age/time bias, in that older people have had a longer time to be exposed to RVFV infected mosquitoes and livestock, the present study and past studies suggest a significant step in RVFV infection risk over the age of 15 years [5,6]. Cultural practices may have limited children’s exposure, as they may be less likely to directly handle infectious materials before the age of 16 years.
Of the subject symptoms we elicited, backache was the most strongly associated with RVFV seropositivity. Among confirmed, hospitalized RVF patients, an initial syndrome consisting of severe headache, fever, arthralgias, and general malaise has been described that occurs prior to the onset of delirium and mental confusion and/or hemorrhagic manifestations [9]. Among encephalitis-related symptoms, photophobia, mental confusion, and meningismus were all associated with evidence of past RVFV infection (Table 1). This is significant because longitudinal case-series in West Africa have noted that RVF may result in long-term schizophrenic or dementia-like manifestations [20]. Our observed association between mental confusion symptoms and RVFV seropositivity is consistent with this previously documented RVFV-related finding.
Self-reported visual impairment and reduced measured visual acuity were both correlated with RVFV seropositivity. Uveitis and/or retinitis are two of the most common sequelae of human RVF [6]. In our study, a history of eye pain, red eyes, or photophobia (eyes sensitive to light) were significantly associated with RVFV seropositivity, which may have been due to RVF uveitis at the time of acute infection. Of the subset of subjects who had retinitis on fundoscopic examination, only one quarter were seropositive, demonstrating a larger burden of unrelated retinal disease in this community.
The analysis of RVF disease severity (Tables 3 and 4) suggests that exposure factors have only a minimal impact on the risk for disease severity, even though they increase risk for infection (as seen in Table 1). This agrees with a recent paper from Anyangu et al [1], in which four exposure factors were associated with severe disease versus nonsevere RVF disease during bivariate analyses (animal contact/herding animals, caring for animals during birthing, touching an aborted animal fetus, and being a herdsperson); however, only one factor (touching an aborted animal fetus) was associated with disease severity in the multivariable model. Our study found that sheltering livestock and disposal of a livestock fetus were associated with severity of disease, but these were not statistically significant in our model. The lack of statistical significance may be due to the small study number (164) in this analysis and could be affected by the remote timing of our study in relation to the last outbreak. It is likely that individual level factors (genes, co-morbidities) also determine risk of disease severity, and only not mode of infection.
This study was limited by the self-reported nature of the exposures and symptom data, which are subject to recall bias. Other prevalent infections, such as malaria, may have accounted for the reported fever-related symptoms. In particular, other arbovirus infections, such as West Nile virus, chikungunya virus, and dengue, might have accounted for reported ocular symptoms, as they, too, are known to cause uveitis and retinitis [21–23]. Because those local residents who had experienced severe RVFV disease in 2006–2007 could have had up to a 50% chance of dying, a survival bias is inherent in our study, and the factors associated with the most severe RVFV disease phenotype (hemorrhagic fever and death) may not have been identified. Also we performed our analysis of severe disease with a small sample size of only 164 participants. This limited sample size may have prevented the elucidation of some factors associated with severe RVF disease.
In conclusion, RVFV infection in northeastern Kenya is significantly associated with older age, male gender, livestock harvesting, and poor vision. Spatial analysis suggests that very high-risk households exist within at-risk communities, which appear to harbor most of the RVFV infection burden. Animal exposure factors were linked to severity of human RVF disease symptoms, as suggested in previous studies [1]. Finally, the prominence of vision-related symptoms and ocular findings suggests that these may prove to be useful indicators of active or recent RVF disease in at-risk settings where serological or PCR RVFV testing is not available.
Supporting Information
(DOC)
(PDF)
The relative weights for presence or absence of a given symptom used in the classification are indicated in the left-hand panel. As indicated the right side columns, subjects classified as severe RVF had multiple eye-related symptoms plus systemic symptoms of acute febrile illness. Those with moderate RVF reported systemic symptoms, but not eye complaints. Subjects with mild disease had seropositivity but reported no symptoms. Ten additional symptoms were scored and entered into the analysis, but did not differ among the three groups.
(TIFF)
(XLS)
Acknowledgments
We thank the survey participants and the Kenyan field team, without whom the study could not have been performed. Thanks also to Grace Mathenge, Christine Lucas, and Dave Bertsch for their assistance with the data processing and Julie Brichard for graphics assistance.
Data Availability
We ask very detailed information about age, sex, occupation and take the X and Y coordinates of the household by GPS, so in essence someone with that data could unmask all of our participants. A dataset containing data that does not contain any PHI has been uploaded as S1 Dataset.
Funding Statement
This study was supported by National Institutes of Health Midwest Regional Center of Excellence Program Project Award: U54AI057160 for ADL, AGH, CHK, and JWK. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Anyangu AS, Gould LH, Sharif SK, Nguku PM, Omolo JO, et al. (2010) Risk factors for severe Rift Valley fever infection in Kenya, 2007. Am J Trop Med Hyg 83: 14–21. 10.4269/ajtmh.2010.09-0293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Woods CW, Karpati AM, Grein T, McCarthy N, Gaturuku P, et al. (2002) An outbreak of Rift Valley fever in Northeastern Kenya, 1997–98. Emerg Infect Dis 8: 138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Breiman RF, Minjauw B, Sharif SK, Ithondeka P, Njenga MK (2010) Rift Valley Fever: scientific pathways toward public health prevention and response. Am J Trop Med Hyg 83: 1–4. 10.4269/ajtmh.2010.83s2a01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC (2007) Rift Valley Fever. Viral Hemorrhagic Fevers: Fact Sheets. pp.1–3.
- 5. LaBeaud AD, Muchiri EM, Ndzovu M, Mwanje MT, Muiruri S, et al. (2008) Interepidemic Rift Valley fever virus seropositivity, northeastern Kenya. Emerg Infect Dis 14: 1240–1246. 10.3201/eid1408.080082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. LaBeaud AD, Muiruri S, Sutherland LJ, Dahir S, Gildengorin G, et al. (2011) Postepidemic analysis of Rift Valley fever virus transmission in northeastern Kenya: a village cohort study. PLoS Negl Trop Dis 5: e1265 10.1371/journal.pntd.0001265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Food Safety Authority (2005) Opinion of the scientific panel on animal health and welfare on a request from the Commission related to "The risk of a rift valley fever incursion and its persistence within the community". EFSA Journal. pp. 1–128.
- 8. Hartley DM, Rinderknecht JL, Nipp TL, Clarke NP, Snowder GD (2011) Potential effects of Rift Valley fever in the United States. Emerg Infect Dis 17: e1 10.3201/eid1709.110506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kahlon SS, Peters CJ, Leduc J, Muchiri EM, Muiruri S, et al. (2010) Severe Rift Valley fever may present with a characteristic clinical syndrome. Am J Trop Med Hyg 82: 371–375. 10.4269/ajtmh.2010.09-0669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Al-Hazmi A, Al-Rajhi AA, Abboud EB, Ayoola EA, Al-Hazmi M, et al. (2005) Ocular complications of Rift Valley fever outbreak in Saudi Arabia. Ophthalmology 112: 313–318. [DOI] [PubMed] [Google Scholar]
- 11. Niklasson B, Grandien M, Peters CJ, Gargan TP 2nd (1983) Detection of Rift Valley fever virus antigen by enzyme-linked immunosorbent assay. J Clin Microbiol 17: 1026–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. LaBeaud AD, Ochiai Y, Peters CJ, Muchiri EM, King CH (2007) Spectrum of Rift Valley fever virus transmission in Kenya: insights from three distinct regions. Am J Trop Med Hyg 76: 795–800. [PMC free article] [PubMed] [Google Scholar]
- 13. Meadors GF 3rd, Gibbs PH, Peters CJ (1986) Evaluation of a new Rift Valley fever vaccine: safety and immunogenicity trials. Vaccine 4: 179–184. [DOI] [PubMed] [Google Scholar]
- 14. Morrill JC, Carpenter L, Taylor D, Ramsburg HH, Quance J, et al. (1991) Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine 9: 35–41. [DOI] [PubMed] [Google Scholar]
- 15. Norusis MJ (2008) Cluster Analysis SPSS Statistics 17- Statistical Procedures Companion. Upper Saddle River, NJ: Prentice Hall; pp. 359–388. [Google Scholar]
- 16. Chen D, Getis A (1998) Point Pattern Analysis. San Diego State University; San Diego, CA. [Google Scholar]
- 17. Getis A (1984) Interaction modeling using second-order analysis. Environment and Planning A 16 173–183. [Google Scholar]
- 18. Getis A, Ord J (1996) Local spatial statistics: an overview; Longley P, Batty M, editors. Spatial Analysis: Modelling in a GIS Environment. Cambridge: Geoinformation International. 261–277 p. [Google Scholar]
- 19. Nguku PM, Sharif SK, Mutonga D, Amwayi S, Omolo J, Mohammed O, Farnon EC, Gould LH, Lederman E, Rao C, Sang R, Schnabel D, Feikin DR, Hightower A, Njenga MK, Breiman RF. An investigation of a major outbreak of Rift Valley fever in Kenya: 2006–2007. Am J Trop Med Hyg. 2010. Aug;83(2 Suppl):5–13. 10.4269/ajtmh.2010.09-0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Riou O, Philippe B, Jouan A, Coulibaly I, Mondo M, et al. (1989) [Neurologic and neurosensory forms of Rift Valley fever in Mauritania]. Bull Soc Pathol Exot Filiales 82: 605–610. [PubMed] [Google Scholar]
- 21. Anninger W, Lubow M (2004) Visual loss with West Nile virus infection: a wider spectrum of a "new" disease. Clin Infect Dis 38: e55–56. [DOI] [PubMed] [Google Scholar]
- 22. Khairallah M, Chee SP, Rathinam SR, Attia S, Nadella V (2010) Novel infectious agents causing uveitis. Int Ophthalmol 30: 465–483. 10.1007/s10792-009-9319-6 [DOI] [PubMed] [Google Scholar]
- 23. Koevary SB (2005) Ocular involvement in patients infected by the West Nile virus. Optometry 76: 609–612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(PDF)
The relative weights for presence or absence of a given symptom used in the classification are indicated in the left-hand panel. As indicated the right side columns, subjects classified as severe RVF had multiple eye-related symptoms plus systemic symptoms of acute febrile illness. Those with moderate RVF reported systemic symptoms, but not eye complaints. Subjects with mild disease had seropositivity but reported no symptoms. Ten additional symptoms were scored and entered into the analysis, but did not differ among the three groups.
(TIFF)
(XLS)
Data Availability Statement
We ask very detailed information about age, sex, occupation and take the X and Y coordinates of the household by GPS, so in essence someone with that data could unmask all of our participants. A dataset containing data that does not contain any PHI has been uploaded as S1 Dataset.