Abstract
Objective
We aimed to compare blood pressure (BP) levels recorded using the semiautomatic oscillometric Omron i-C10 BP device in patients with or without hypertension in three different settings: (a) when used by a doctor or a nurse at the office (OBP); (b) when used for self-measurement by the patient at the office (SMOBP); and (c) when used for 7 consecutive days at home (HBP).
Materials and methods
A total of 247 individuals were invited to participate, but 78 of these individuals declined and a further seven were excluded, leaving a final cohort of 162 participants.
Results
The mean OBP was higher than HBP (difference 8.1±14/3.1±8.8 mmHg, P<0.0001) and so was SMOBP compared with HBP (difference 7.0±13/4.2±7.3 mmHg, P<0.0001). Sixteen participants (9.9%) had at least 10 mmHg higher systolic SMOBP than OBP and 28 (17%) participants had at least 10 mmHg lower systolic SMOBP than OBP. Participants who were current smokers had a larger mean difference between systolic OBP and SMOBP than nonsmokers (OBP−SMOBP in smokers: 6.6±9.4 mmHg, OBP−SMOBP in nonsmokers: 0.5±9.2 mmHg, P=0.011 between groups).
Conclusion
Self-measurement of BP in the office does not preclude an increase in BP when levels in the individual patients are compared with HBP using the same equipment. Thus, SMOBP with a semiautomatic device does not lead to a reduction in the white-coat effect in the same manner as fully automatic devices.
Keywords: home blood pressure, hypertension, office blood pressure, oscillometric, smoking
Introduction
Many patients show a temporary increase in blood pressure (BP) levels at the office when this is recorded by a doctor or a nurse 1,2. Accordingly, ambulatory BP recordings or self-measurements of BP at home (HBP) are often recommended for a final diagnosis of hypertension when there is suspicion of this so-called ‘white-coat effect’ of the office blood pressure (OBP) recording 3,4. It is not entirely clear whether the increase in OBP is induced by the presence of the provider of care, the nurse or doctor, or whether it is the setting that is most important. However, studies using the BpTRU monitor have shown that self-measurement of blood pressure at the office (SMOBP) by the patient yields values of mean BP that are similar to those measured as awake ambulatory BP, suggesting that the white-coat effect is eliminated 5,6. In Canada, use of the fully automatic BpTRU equipment for BP recordings at the office in routine care is quite prevalent 6. In Sweden, however, many primary healthcare centers use traditional semiautomatic HBP monitors that are considerably cheaper than the BpTRU monitor for the same purpose. These measurements are usually performed in dedicated ‘self-healthcare rooms’ in which the patients measure the BP without supervision, but are instructed to rest alone for 5 min ahead of BP recordings, and then to leave a note with the actual BP measured to the provider of care, for a diagnosis or for the follow-up of hypertension. This supposedly saves time for the patient and also costs for the primary healthcare center as no personnel are needed for the BP measurement. Furthermore, the patient does not need to book any particular appointment for the BP measurement. We are aware of only one dedicated study that has compared SMOBP with BP recordings by the provider of care using the same equipment when this is done using a semiautomatic oscillometric BP device that has been validated and found to provide BP recordings with high quality 7. However, as this earlier study was of a limited size (n=30) detailed analyses of the potential confounders of differences between OBP and SMOBP were challenging 7.
We aimed to investigate and compare BP levels recorded with the same oscillometric BP recorder, the Omron i-C10 BP device (derivative of Omron M-7), in patients with or without known hypertension, in three different settings: (a) when used by a doctor or a nurse at the office; (b) when used for self-measurement by the patient at the healthcare center; and (c) when used for 7 consecutive days for self-measurement of BP at home. We wanted not only to compare the mean values at the different settings and correlations between recordings but also to study whether there were any more systematic interactions between differences in BP levels measured in the three settings and anthropometrics or risk factors for cardiovascular disease. In contrast to most earlier studies 7,8, our cohort included patients with and without established hypertension. The study aimed to investigate whether conventional manual BP can be replaced with the use of a semiautomatic HBP recorder to obtain readings that are similar to the HBP and less affected by the white-coat effect associated with conventional manual BP.
Materials and methods
The study was carried out in two primary health care centers in the city of Motala, which is located in southeastern Sweden. The participants were invited to participate in the BP study between June and October 2013. The invitation was provided either during a regular visit to the primary healthcare center or by a letter to patients with an established diagnosis of hypertension. Exclusion criteria were atrial fibrillation and recent start (<3 months) of treatment with antihypertensive drugs to reduce BP in hypertension. A questionnaire was filled out by each participant including information on smoking, concomitant diseases, and medications.
Participants were assigned randomly to one out of two groups, one in which the participants began with BP measurement at the health care center by a doctor or a nurse and one in which the participants began with SMOBP in the designated room at the health care center. A semiautomatic Omron i-C10 Blood Pressure Monitor (OMRON Corporation, Kyoto, Japan) was used for all BP measurements at the offices and at home.
All BP measurements in the office and at home were performed after 5 min of rest. The first measurements were performed three times in each arm and the arm with the highest BP (any difference) was then used for subsequent recordings at OBP and HBP measurements. There was a 1-min interval between the three BP recordings performed. For the self-measurements, the patients were alone without any health professional in the room and after 5 min of rest, seated with bilateral armrests, and the upper arm in which BP was measured to be positioned at the heart level, they started the semiautomatic device for the three recordings. At home, the BP measurements were performed by the patients in the same manner and arm as at the office, in the morning and in the evening, for 7 consecutive days. The results of the recordings were noted on a dedicated sheet of paper by the patients. The mean values of the last two measurements on each BP recording (at the office and at home in both the morning and evening) were calculated and used in the results presented here. Thus, HBP consisted of 2+2 recordings on each day (morning and evening) for 7 days (i.e. a total of 28 BP measurements).
Ethics
All participants provided written informed consent before participating in the study. The study, which complied with the Declaration of Helsinki, was approved by the Regional Ethical Review Board in Linköping, Sweden.
Statistics
IBM SPSS statistics 21 and 22 (IBM Corporation, Somers, New York, USA) were used for statistics. Linear correlations were calculated; comparisons within and between groups were carried out using the Student paired and an unpaired two-tailed t-test. Mean (SD) is presented unless otherwise stated. Statistical significance was considered at the 5% level (P≤0.05).
Results
A total of 247 individuals were invited to participate, but 78 of these declined and a further seven were excluded on the basis of study criteria, leaving a final cohort of 162 participants who successfully underwent and performed BP measurements in the office, in the self-measurement room at the healthcare center, and who also performed BP recordings at home for 7 days. No participants were lost to follow-up.
All participants had arm circumferences that allowed use of the standard BP ‘one-size 22–42 cm’ cuff, which has been validated for use also on large arms with circumferences from 32 to 42 cm 9,10.
The first measured systolic BP was on average 1–2 mmHg higher than the following two BP measurements (comparison of all measurements, P<0.0001) when the three BP were recorded by either OBP, SMOBP, or HBP. The corresponding diastolic BP differences were numerically smaller, varying from 0.4 to 0.6 mmHg (P<0.0001). All data are presented here after disregarding this first recorded BP on each occasion, that is as mean values of the remaining two BP recordings.
Table 1 shows the characteristics of the participants including the mean BP levels at the three settings. The mean HBP levels were lower than both SMOBP and OBP, whereas the mean OBP and SMOBP did not differ significantly (mean systolic difference 1.1±9.4 mmHg, P=0.14, mean diastolic difference −1.1±7.9 mmHg, P=0.085, see Table 1). There were strong correlations between SMOBP and OBP (systolic BP: r=0.87, P<0.0001, diastolic BP: r=0.73, P<0.0001). OBP correlated with HBP (systolic BP: r=0.69, P<0.0001, diastolic BP: r=0.63, P<0.0001) and correspondingly SMOBP correlated with HBP (systolic BP: r=0.72, P<0.0001, diastolic BP: r=0.72, P<0.0001).
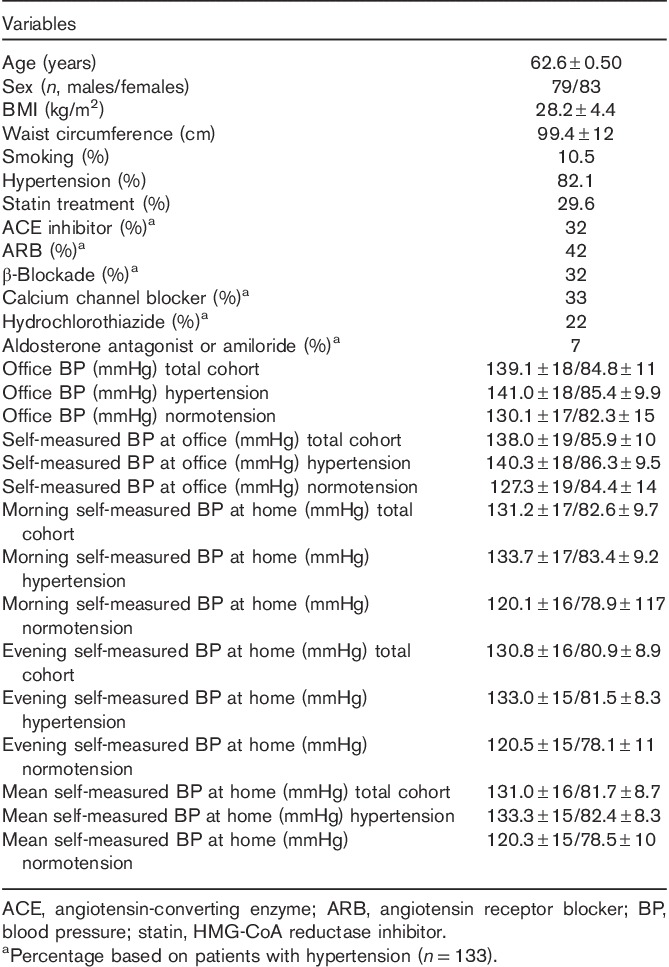
Table 1.
Baseline characteristics of the participants
The mean difference between OBP and HBP was 8.1±14/3.1±8.8 mmHg (P<0.0001 for both systolic and diastolic levels) and the corresponding level of difference between SMOBP and HBP was 7.0±13/4.2±7.3 mmHg (P<0.0001 for both systolic and diastolic levels). On an individual level, some patients showed large differences between BP measurements at the different settings, as shown by histograms for systolic OBP−SMOBP, OBP−HBP, and SMOBP−HBP (Fig. 1a–c). Sixteen participants (9.9%) had at least 10 mmHg higher systolic SMOBP than OBP, and conversely, 28 (17%) participants had at least 10 mmHg lower systolic SMOBP than OBP.
Fig. 1.
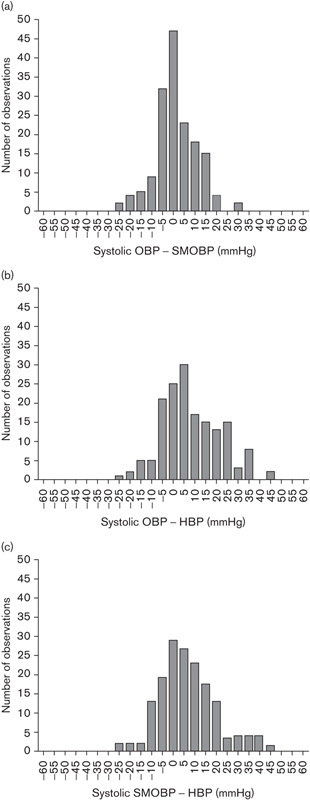
(a–c) Frequency distribution of individual differences between self-measured systolic blood pressure at office (SMOBP), office blood pressure (OBP), and mean home blood pressure (HBP) during 7 days. Data are presented for 162 participants, three BP were recorded at each instance but the first BP that was recorded has been omitted out of three, and the mean value of the remaining two BP has been used in the analyses. HBP was measured three times in the morning and three times in the afternoon for 7 days. (a) Frequencies of levels of systolic OBP−SMOBP. (b) Systolic OBP−HBP. (c) Systolic SMOBP−HBP.
There were no significant correlations between the differences in systolic BP measured at the three settings with BMI, sex, diagnosis of hypertension, or age. However, the magnitude of the OBP−SMOBP difference correlated positively with OBP levels (systolic: r=0.18, P=0.019, diastolic r=0.45, P<0.0001), that is at higher OBP levels, there was also a larger difference compared with SMOBP levels. Correspondingly, there was a negative correlation between the OBP−SMOBP difference with SMOBP (systolic values r=−0.33, P<0.0001, diastolic values r=−0.28, P<0.0001). Figure 2 shows the relationships between HBP and the SMOBP−HBP difference and also that of HBP in relation to the OBP−HBP difference, that is so-called Bland–Altman plots.
Fig. 2.
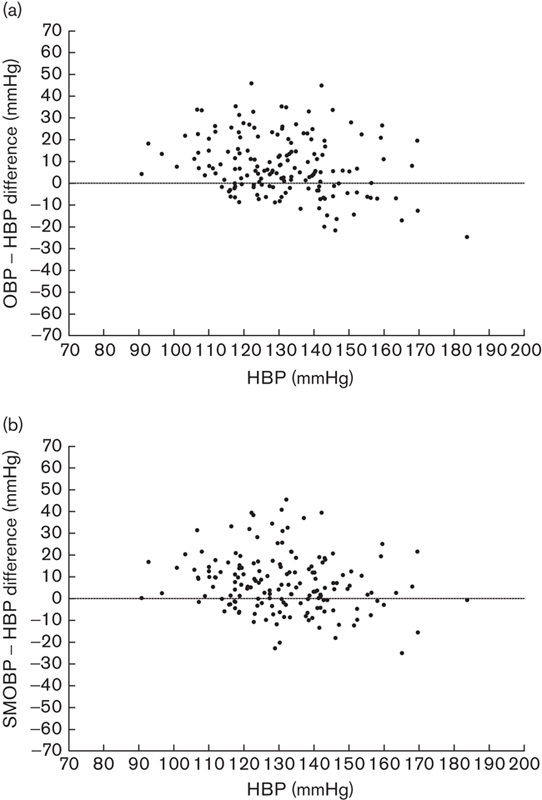
(a, b) Bland–Altman plots of the relation between the mean home blood pressure (HBP) measured during 7 days with the differences with self-measured systolic blood pressure at office (SMOBP) or office blood pressure (OBP). Data are presented for 162 participants, three BP were recorded at each instance but the first BP that was recorded has been omitted out of three, and the mean value of the remaining two BP has been used in the analyses. HBP was measured three times in the morning and three times in the afternoon for 7 days. (a) A plot for mean systolic HBP on the x-axis compared with systolic OBP−systolic HBP on the y-axis. (b) The corresponding analysis of systolic SMOBP−systolic HBP on the y-axis.
The mean BPs at home or at the office did not differ when levels in current smokers (n=17) were compared with nonsmokers, but there was a nonsignificant trend for a higher mean systolic SMOBP in nonsmokers than in smokers (smokers: 132.3±16 mmHg, nonsmokers: 138.6±19 mmHg, P=0.19). Participants who were current smokers had a larger mean difference between systolic OBP and SMOBP than nonsmokers (OBP−SMOBP in smokers: 6.6±9.4 mmHg, OBP−SMOBP in nonsmokers: 0.5±9.2 mmHg, P=0.011 between groups) whereas there was no such difference between OBP and HBP (P=0.78 between groups). Smokers had similar systolic self-measured BP at the office and at home whereas nonsmokers had comparatively lower systolic HBP (SMOBP−HBP in smokers: 0.64±14 mmHg, SMOBP−HBP in nonsmokers: 7.7±13 mmHg, P=0.034 between groups).
Corresponding analyses for diastolic BP showed higher levels of OBP compared with SMOBP in smokers (diastolic OBP−SMOBP in smokers: 3.8±4.6 mmHg, diastolic OBP−SMOBP in nonsmokers −1.7±8.0 mmHg, P=0.007 between groups).
Discussion
Using the semiautomatic Omron i-C10 device, we did not obtain similar results of studies of SMOBP using the fully automatic BpTRU device, indicating that the white-coat effect of being at the office is generally absent 6,8. Rather, our findings are similar to the first studies of SMOBP that found the setting to be of greater importance than whether the measurement is performed by the patient or by others 7,11. Our findings are thus in line with the first specific investigations of the importance of the setting for BP levels when an Omron Hem 705CP was used 7, an apparatus very similar to the one used in our study. Stergiou et al. 7 investigated the importance of the setting for the BP recordings and on the basis of their findings, similar to ours, suggested that ‘HBP’ is a more correct term than ‘self-measured BP’. Stergiou et al. 7 also reported that self-measured BP in the home did not differ markedly from HBP recorded by a relative 7, a finding that also suggests the importance of the setting as compared with the particular individual who records the BP.
In Canada, the BpTRU device is used commonly for SMOBP and it has been shown to reduce the white-coat effect in the office when this has been compared with manual BP recordings 8. This device is considerably more expensive than the Omron i-C10 that we have used in our study, and we know of no study in which the BpTRU has been compared in different settings in a manner similar to ours. Although it is convenient in many ways to allow patients to visit the office and record BP using semiautomatic BP measuring equipment in a flexible manner without having to book an appointment, our findings suggest that this yields BP values that often differ considerably from those measured by a doctor or a nurse using the same technique for the actual BP recording. Thus, our data suggest that manual OBP should preferably be replaced with fully automatic BP recordings and not semiautomatic SMOBP to achieve similar mean values as HBP.
Previous studies on the importance of the setting for self-measurement of BP have focused mainly on correlations and on the mean values of BP levels in the different settings 8. Although the mean values of SMOBP and OBP did not differ in our study, we found 26.9% of recorded systolic BP to differ 10 mmHg or more (being higher or lower) when SMOBP and OBP were compared. This level of difference is clinically relevant and could potentially lead to different antihypertensive medication depending on how BP is recorded.
When studying potential confounders with respect to differences between OBP and SMOBP, we found that the difference correlated positively with the actual OBP level. This suggests that in particular, patients with a high OBP, that is those likely to be attributed to a change in medication, the SMOBP would have been considerably lower. These findings are in line with an earlier finding of a positive trend for the systolic BP difference between automated readings at the office and awake ambulatory BP reaching 78 mmHg in the upper 95% confidence interval 12. We also found that smokers showed a larger difference between OBP and SMOBP than nonsmokers. This difference was clinically relevant, amounting to 7.7±13/3.8±4.6 mmHg on average; however, the subgroup of current smokers was small in size. Thus, knowledge of smoking habits is important when interpreting BP measured in these different settings. Somewhat speculatively, it is possible that the higher levels of OBP relative to SMOBP in smokers could be a specific white-coat effect that is linked to the smoking habit itself, inducing an uncomfortable sense of being in an environment in which antismoking advices are common. The habit of smoking could increase BP because of the worry of criticism of this particular life-style. In fact, the particular room used for SMOBP is often equipped with visible antismoking pamphlets as this room contains general information on how to improve different health aspects. The comparatively small difference between SMOBP and HBP in smokers could be a result of increases in BP at home following the acute BP elevation induced by smoking a cigarette 13. It is also possible that smoking frequently occurred before HBP and OBP recordings, and thus increased BP levels in these instances. Our results of lower HBP than SMOBP in general were not in agreement with a trial by Myers et al. 14 of three oscillometric automatic BP recorders designed for use at home in which similar levels of BP were found in both environments. However, the prevalence of smoking was not reported in this study by Myers et al. 14, and if it was high, this would fit with our finding of similar levels of HBP and SMOBP in smokers.
In contrast to earlier investigations on the topic, our cohort included normotensive as well as hypertensive participants. However, the difference between BP measured in the different settings did not differ in hypertensive and normotensive participants, and this makes it less likely that it was better compliance with antihypertensive drug therapy that reduced HBP during 7 days compared with BP measured in the office. A limitation in this respect was that we did not measure compliance in the trial.
Traditional OBP measured by the manual technique has been shown to be lower when recorded by specially trained staff during clinic studies compared with measurements in routine practice 8,15. Taking extra precaution in measurement techniques in trials, when being observed, compared with routine practice has been termed the ‘Hawthorne effect’ 16,17. As the measurement technique, the BP recorder, in our study was identical in the two settings, our results of similar BP, whether measured by SMOPB or OBP, suggest that the higher BP recorded manually in other studies could to some extent be dependent on the lack of expertise. Thus, our finding that there, in general, is no increase in BP when the same technical semi-automated equipment is used by a doctor or a nurse when compared with self-measurement is in line with the fact that technical issues can affect, that is increase, recorded BP levels during routine manual recordings 16.
A limitation of the generalizability of the results was that the participants were only moderately obese and that hence none had an arm circumference above 42 cm. Further limitations were that we did not obtain traditional auscultatory readings for comparisons and that patients made manual notes of the self-measured BP. However, this again was based on the idea of studying SMOBP and HBP in the same manner as is often the case clinically in Sweden. Also, we acknowledge that results in a trial such as the one presented here were performed with ‘research quality’ and hence different results may be obtained under regular clinic conditions.
Conclusion
In summary, our study confirms previous investigations on the importance of the setting rather than the technique, including personnel, for the BP recordings. SMOBP with a semiautomatic device does not preclude a considerable increase in BP when levels in the individual patient are compared with self-measurement at home using the same equipment as shown with histograms as well as Bland–Altman plots (Figs 1 and 2). Our data would support the use of HBP for follow-up of BP in patients with hypertension, and this is in line with the fact that HBP is a better predictor of risk than office BP measured by the conventional technique 18. The semiautomatic Omron i-C10 device did not eliminate the WCE in the same manner as fully automated devices designed specifically for professional use such as the BpTRU, Omron 907, and Microlife WatchBP Office. A manual BP performed according to guidelines is just as good as BPs measured in the office/clinic either by a patient or a health professional using a semiautomatic device, but neither technique eliminates the white-coat effect.
Acknowledgements
The study was supported by Linköping University and the County Council of Östergötland, Sweden.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Isam Al-Karkhi and Raad Al-Rubaiy contributed equally to the writing of this article.
References
- 1.Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Porcellati C. White-coat hypertension. Lancet 1996; 348:1444–1445author reply 1445–1446. [DOI] [PubMed] [Google Scholar]
- 2.Nyström F, Aardal E, Ohman KP. A population-based study of the white-coat blood pressure effect: positive correlation with plasma cortisol. Clin Exp Hypertens 1998; 20:95–104. [DOI] [PubMed] [Google Scholar]
- 3.Flynn C, Bakris GL. Role of ambulatory blood pressure monitoring in hypertension and diabetes. Curr Hypertens Rep 2013; 15:137–142. [DOI] [PubMed] [Google Scholar]
- 4.Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31:1281–1357. [DOI] [PubMed] [Google Scholar]
- 5.Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Grant FC, Kaczorowski J. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ 2011; 342:d286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myers MG, Godwin M. Automated office blood pressure. Can J Cardiol 2012; 28:341–346. [DOI] [PubMed] [Google Scholar]
- 7.Stergiou GS, Efstathiou SP, Alamara CV, Mastorantonakis SE, Roussias LG. Home or self blood pressure measurement? What is the correct term? J Hypertens 2003; 21:2259–2264. [DOI] [PubMed] [Google Scholar]
- 8.Myers MG, Kaczorowski J, Dawes M, Godwin M. Automated office blood pressure measurement in primary care. Can Fam Physician 2014; 60:127–132. [PMC free article] [PubMed] [Google Scholar]
- 9.El Feghali RN, Topouchian JA, Pannier BM, El Assaad HA, Asmar RG. European Society of Hypertension. Validation of the OMRON M7 (HEM-780-E) blood pressure measuring device in a population requiring large cuff use according to the International Protocol of the European Society of Hypertension. Blood Press Monit 2007; 12:173–178. [DOI] [PubMed] [Google Scholar]
- 10.Coleman A, Steel S, Freeman P, de Greeff A, Shennan A. Validation of the Omron M7 (HEM-780-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit 2008; 13:49–54. [DOI] [PubMed] [Google Scholar]
- 11.Myers MG, Meglis G, Polemidiotis G. The impact of physician vs automated blood pressure readings on office-induced hypertension. J Hum Hypertens 1997; 11:491–493. [DOI] [PubMed] [Google Scholar]
- 12.Andreadis EA, Agaliotis GD, Angelopoulos ET, Tsakanikas AP, Chaveles IA, Mousoulis GP. Automated office blood pressure and 24-h ambulatory measurements are equally associated with left ventricular mass index. Am J Hypertens 2011; 24:661–666. [DOI] [PubMed] [Google Scholar]
- 13.Kim JW, Park CG, Hong SJ, Park SM, Rha SW, Seo HS, et al. Acute and chronic effects of cigarette smoking on arterial stiffness. Blood Press 2005; 14:80–85. [DOI] [PubMed] [Google Scholar]
- 14.Myers MG, Valdivieso M, Chessman M, Kiss A. Can sphygmomanometers designed for self-measurement of blood pressure in the home be used in office practice? Blood Press Monit 2010; 15:300–304. [DOI] [PubMed] [Google Scholar]
- 15.Head GA, Mihailidou AS, Duggan KA, Beilin LJ, Berry N, Brown MA, et al. Ambulatory Blood Pressure Working Group of the High Blood Pressure Research Council of Australia. Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: prospective cohort study. BMJ 2010; 340:c1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens 2009; 27:280–286. [DOI] [PubMed] [Google Scholar]
- 17.Feil PH, Grauer JS, Gadbury-Amyot CC, Kula K, McCunniff MD. Intentional use of the Hawthorne effect to improve oral hygiene compliance in orthodontic patients. J Dent Educ 2002; 66:1129–1135. [PubMed] [Google Scholar]
- 18.Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension 2010; 55:1346–1351. [DOI] [PubMed] [Google Scholar]


