Abstract
Background:
Total hip arthroplasty may be performed under general or spinal anesthesia. The purpose of the current study was to compare perioperative outcomes between anesthetic types for patients undergoing primary elective total hip arthroplasty.
Methods:
Patients who had undergone primary elective total hip arthroplasty from 2010 to 2012 were identified from the American College of Surgeons National Surgical Quality Improvement Program database. Operating room times, length of stay, thirty-day adverse events, and readmission were compared between patients who had received general anesthesia and those who had received spinal anesthesia. Propensity-adjusted multivariate analysis was used to control for selection bias and baseline patient characteristics.
Results:
A total of 20,936 patients who had undergone total hip arthroplasty met inclusion criteria for this study. Of these, 12,752 patients (60.9%) had received general anesthesia and 8184 patients (39.1%) had received spinal anesthesia. On propensity-adjusted multivariate analyses, general anesthesia for total hip arthroplasty was associated with increased operative time (+12 minutes [95% confidence interval, +11 to +13 minutes]; p < 0.001) and postoperative room time (+5 minutes [95% confidence interval, +4 to +6 minutes]; p < 0.001). General anesthesia was also associated with the occurrence of any adverse event (odds ratio, 1.31 [95% confidence interval, 1.23 to 1.41]; p < 0.001), prolonged postoperative ventilator use (odds ratio, 5.81 [95% confidence interval, 1.35 to 25.06]; p = 0.018), unplanned intubation (odds ratio, 2.17 [95% confidence interval, 1.11 to 4.29]; p = 0.024), stroke (odds ratio, 2.51 [95% confidence interval, 1.02 to 6.20]; p = 0.046), cardiac arrest (odds ratio, 5.04 [95% confidence interval, 1.15 to 22.07]; p = 0.032), any minor adverse event (odds ratio, 1.35 [95% confidence interval, 1.25 to 1.45]; p = 0.001), and blood transfusion (odds ratio, 1.34 [95% confidence interval, 1.25 to 1.45]; p < 0.001). General anesthesia was not associated with any difference in preoperative room time, postoperative length of stay, or readmission.
Conclusions:
General anesthesia was associated with an increased rate of adverse events and mildly increased operating room times.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Total hip arthroplasty is considered one of the most successful orthopaedic procedures, and more than one million operations are performed each year worldwide1. Historically, general anesthesia has been the gold standard for major hip surgery; however, total hip arthroplasty is now commonly being performed under spinal anesthesia2. The optimal anesthetic technique remains debated.
Several studies have shown the relative benefits of neuraxial anesthesia compared with general anesthesia, such as decreased blood loss and need for transfusion, decreased rates of thromboembolic events, and reduced rates of surgical site infection3-8. The majority of these findings are from small, single-institution studies. There is a need for large, multicenter studies that directly compare perioperative outcomes between neuraxial and general anesthesia in patients undergoing total hip arthroplasty.
The present investigation aims to compare operating room times, length of stay, adverse events, and readmission following primary elective total hip arthroplasty between general and spinal anesthesia with use of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. The primary hypothesis of this study was that there would be differences in the rates of adverse events between patients who had undergone primary elective total hip arthroplasty with general anesthesia and those who had undergone primary elective total hip arthroplasty with spinal anesthesia that persists after adjustment for patient characteristics. By using high-quality, prospectively collected data from a large, national cohort of patients who had undergone hip arthroplasty, generalizable conclusions may guide clinical practice for this common surgery.
Materials and Methods
An exemption for this study was granted by our institutional review board. A retrospective cohort study was conducted with use of the ACS-NSQIP database, which collects data from more than 370 participating United States hospitals9. Patients are identified prospectively at eligible hospitals and more than 150 variables are recorded by trained clinical reviewers, using a combination of chart abstraction and patient interviews. Data are collected until the thirtieth postoperative day, including after discharge9,10. The ACS-NSQIP conducts routine auditing to ensure high-quality data and reports inter-rater disagreement of <2% for all variables.
The ACS-NSQIP database from 2010 to 2012 was queried to identify patients who had undergone total hip arthroplasty. We identified all patients who had undergone primary total hip arthroplasty (Current Procedural Terminology [CPT] code 27130) for osteoarthritis of the hip (International Classification of Diseases, Ninth Revision [ICD-9] codes 715.15, 715.35, or 715.95). For this study, general anesthesia had been performed with either tracheal intubation or laryngeal mask airway. Spinal anesthesia did not include cases that had been performed under epidural anesthesia. Patients who had received any form of anesthesia other than general or spinal were excluded from this study. Patients who had undergone nonelective surgery, those with previous evidence of infection, and those with missing perioperative data were also excluded from the analysis. After these exclusions, of an initial 23,342 patients, 20,936 remained for analysis.
Patient characteristics such as age, sex, height, and weight are available in the database. Body mass index (BMI) was calculated from height and weight. Based on the available comorbidity data, a modified Charlson Comorbidity Index11 was generated for each patient. Such modified Charlson Comorbidity Indexes have been shown to be similar in efficacy to the original Charlson Comorbidity Index12,13, and the modified Charlson Comorbidity Index employed in this study has been previously used with the ACS-NSQIP14.
The following comorbidities were used to calculate the modified Charlson Comorbidity Index (followed by corresponding point values): myocardial infarction (1 point), congestive heart failure (1 point), peripheral vascular disease or rest pain (1 point), transient ischemic attack or cerebrovascular accident (1 point), chronic obstructive pulmonary disease (1 point), diabetes mellitus (1 point), hemiplegia (2 points), end-stage renal disease (2), ascites or esophageal varices (3 points), and cancer (6 points). One point was also added for each decade more than forty years of age.
Operating Room Times and Length of Stay
Preoperative room time, operative time, and postoperative room time are available in the database. Preoperative room time was defined as the minutes between the patient entering the operating room and the opening incision. Operative time was defined as the minutes from opening incision to wound closure. Postoperative room time was defined as minutes from wound closure to the patient leaving the operating room. It is important to note that information on whether spinal anesthesia was initiated outside of the operating room or in the operating room was not available.
Length of stay was defined as the number of calendar days from operation to discharge. Operating room times and length of stay were treated as continuous variables for analysis.
Adverse Events and Readmission
The occurrence of individual adverse events within the first thirty postoperative days is recorded by the ACS-NSQIP on the basis of specific criteria (see Appendix). The occurrence of a serious adverse event was defined as follows: death; postoperative ventilator use for more than forty-eight hours; unplanned intubation; stroke or cerebrovascular accident; thromboembolic event (deep vein thrombosis or pulmonary embolism); surgical site infection (superficial surgical site infection, deep surgical site infection, organ or space infection); sepsis or septic shock; cardiac arrest; myocardial infarction; acute renal failure; return to the operating room; wound dehiscence; graft, prosthesis, or flap failure; or peripheral nerve injury.
The occurrence of a minor adverse event was defined as a blood transfusion, urinary tract infection, pneumonia, or progressive renal insufficiency. Any adverse event was defined as the occurrence of either a serious adverse event or a minor adverse event.
Since 2011, the ACS-NSQIP has also tracked readmissions following discharge for the first thirty postoperative days. Only patients who had undergone total hip arthroplasty in 2011 or 2012 were included in the readmission analyses.
Statistical Analysis
Bivariate logistic regression was used to compare age, sex, BMI, and modified Charlson Comorbidity Index between patients who had undergone total hip arthroplasty with general anesthesia and those who had undergone total hip arthroplasty with spinal anesthesia. To control for selection bias between the nonrandomized spinal and general anesthesia groups, propensity scores were used, with the propensity score defined as the conditional probability of receiving general anesthesia based on the observed patient demographic characteristics and comorbidities. The propensity score has been extensively used in the literature for this purpose15,16. Propensity-adjusted p values for preoperative patient demographic characteristics were reported. The model successfully reduced selection bias by eliminating significant differences in preoperative variables (the adjusted p value was >0.05 for all patient characteristics).
Bivariate and propensity-adjusted multivariate regressions were subsequently used to compare the rates of adverse outcomes that occurred with general anesthesia and spinal anesthesia, using spinal anesthesia cases as the reference. Multivariate regression adjusted for baseline differences in patient demographic characteristics and comorbidities as well as the propensity score. Continuous outcomes (operating room times and postoperative length of stay) were compared between anesthesia groups with use of linear regression. The binary outcomes (adverse events and readmission) were compared between spinal and general anesthesia groups with use of logistic regression. The level of significance was set at p < 0.05.
Source of Funding
One author (B.A.B.) in this study received a grant from the National Center for Advancing Translational Sciences of the National Institutes of Health (Award Number TL1TR000141). Funds were used to pay for salary and equipment.
Results
Study Population
Of the 20,936 patients who had undergone total hip arthroplasty and met inclusion criteria for this study, 12,752 patients (60.9%) received general anesthesia and 8184 patients (39.1%) received spinal anesthesia. Patient demographic characteristics and comorbidity status are compared between anesthesia groups in Table I. As seen in the table, there were significant differences in preoperative characteristics between groups. Patients who had received general anesthesia were younger (p < 0.001) and had increased BMI (p < 0.001) and decreased comorbidity burden (modified Charlson Comorbidity Index) (p < 0.001) compared with patients who had received spinal anesthesia.
TABLE I.
Patient Demographic Characteristics and Comorbidities
| All Patients* (N = 20,936) | General Anesthesia* (N = 12,752) | Spinal Anesthesia* (N = 8184) | Unadjusted P Value | Adjusted P Value† | |
| Overall | 100% | 60.9% | 39.1% | ||
| Age (yr) | <0.001 | 0.999 | |||
| Younger than fifty-five years | 15.7% | 17.0% | 13.7% | ||
| Fifty-five to sixty-four years | 29.6% | 29.8% | 29.2% | ||
| Sixty-five to seventy-four years | 31.0% | 30.8% | 31.2% | ||
| Seventy-five years or older | 23.8% | 22.4% | 25.9% | ||
| Male sex | 43.2% | 43.2% | 43.1% | 0.890 | 0.999 |
| BMI | <0.001 | 0.998 | |||
| <25 kg/m2 | 21.1% | 20.4% | 22.3% | ||
| 25 to 29.9 kg/m2 | 34.9% | 34.2% | 35.9% | ||
| 30 to 34.9 kg/m2 | 24.5% | 25.0% | 23.7% | ||
| ≥35 kg/m2 | 19.4% | 20.3% | 18.1% | ||
| Modified Charlson Comorbidity Index | <0.001 | 0.999 | |||
| 0 to 2 | 30.9% | 32.5% | 28.4% | ||
| 3 | 32.5% | 32.3% | 32.7% | ||
| ≥4 | 36.7% | 35.2% | 38.9% |
The values are given as the percentage of patients.
To control for selection bias between the spinal and general anesthesia groups, propensity scores were used, with the propensity score defined as the conditional probability of receiving general anesthesia based on the observed patient and operative characteristics. Propensity-adjusted p values for preoperative patient characteristics are reported. The model successfully reduced selection bias by eliminating significant differences in preoperative variables (the adjusted p value was >0.05 for all).
To control for selection bias between treatment groups, propensity scores were calculated for each patient on the basis of the demographic characteristics and comorbidities listed in Table I. The propensity score adjusts for the probability of a patient having received general anesthesia compared with the probability of a patient having received spinal anesthesia in this nonrandomized sample. The p values for propensity-adjusted comparisons between anesthesia groups are reported in Table I and indicate a successful reduction in selection bias (the adjusted p value was >0.05 for all patient characteristics).
Operating Room Times and Length of Stay
The unadjusted mean operating room times (in minutes) and the mean length of stay (in days) for each anesthesia type are reported in Table II. Operating room times and length of stay were compared between anesthesia groups with use of bivariate and propensity-adjusted multivariate linear regressions.
TABLE II.
Association of General Anesthesia with Operating Room Times and Length of Stay in Patients Who Had Undergone Hip Arthroplasty
| Bivariate Linear Regression |
Propensity-Adjusted Multivariate Linear
Regression§ |
|||||
| General Anesthesia* | Spinal Anesthesia* | Beta† | P Value‡ | Beta†# | P Value‡ | |
| Preoperative room time (min) | 46 ± 57 | 49 ± 76 | −2 (−5 to +1) | 0.131 | −2 (−5 to +1) | 0.100 |
| Operative time (min) | 99 ± 40 | 87 ± 38 | +12 (+11 to +13) | <0.001 | +12 (+11 to +13) | <0.001 |
| Postoperative room time (min) | 16 ± 14 | 12 ± 9 | +5 (4 to +6) | <0.001 | +5 (+4 to +6) | <0.001 |
| Postoperative length of stay (d) | 3.1 ± 2.3 | 3.1 ± 3.2 | 0.0 (−0.1 to +0.1) | 0.099 | 0.0 (−0.1 to +0.1) | 0.264 |
The values are given as the mean and the standard deviation.
The values are given as the mean with the 95% CI in parentheses.
Significant values were set at p < 0.05.
Each line represents a separate multivariate analysis for each variable to give an adjusted beta coefficient and p value by controlling for patient characteristics and propensity score.
Unstandardized beta coefficient represents unit change in the outcome variable if the predictor variable is positive. For example, a significant coefficient of +12 for operative time means that, on average, general anesthesia is associated with an increase in operative time of twelve minutes.
On bivariate analyses, general anesthesia was associated with increased operative time and postoperative room time. On multivariate analyses, general anesthesia continued to be associated with increased operative time (+12 minutes [95% confidence interval (95% CI), +11 to +13]; p < 0.001) and postoperative room time (+5 minutes [95% CI, +4 to +6 minutes]; p < 0.001). Bivariate and multivariate analyses found no association between anesthesia type and preoperative room time or postoperative length of stay.
Adverse Events and Readmission
The unadjusted rates of adverse events for each anesthesia type are reported in Table III. These rates were subsequently compared between anesthesia types using bivariate and propensity-adjusted multivariate logistic regressions.
TABLE III.
Association of General Anesthesia with Adverse Events and Readmission in Patients Who Had Undergone Hip Arthroplasty
| Bivariate Logistic Regression |
Propensity-Adjusted Multivariate Logistic
Regression§ |
|||||
| Outcome | General Anesthesia* | Spinal Anesthesia* | Odds Ratio† | P Value‡ | Odds Ratio† | P Value‡ |
| Any adverse event | 23.51% | 19.65% | 1.26 (1.17 to 1.35) | <0.001 | 1.31 (1.23 to 1.41) | <0.001 |
| Any severe adverse event | 3.81% | 3.69% | 1.03 (0.89 to 1.20) | 0.653 | 1.04 (0.90 to 1.20) | 0.618 |
| Death | 0.15% | 0.13% | 1.11 (0.52 to 2.33) | 0.786 | 1.19 (0.57 to 2.53) | 0.632 |
| Ventilator use for more than forty-eight hours | 0.14% | 0.02% | 5.78 (1.34 to 24.93) | 0.019 | 5.81 (1.35 to 25.06) | 0.018 |
| Unplanned intubation | 0.28% | 0.13% | 2.10 (1.07 to 4.13) | 0.031 | 2.17 (1.11 to 4.29) | 0.024 |
| Stroke or cerebrovascular accident | 0.17% | 0.07% | 2.35 (0.95 to 5.81) | 0.063 | 2.51 (1.02 to 6.20) | 0.046 |
| Thromboembolic event (deep vein thrombosis or pulmonary embolism) | 0.64% | 0.59% | 1.08 (0.76 to 1.55) | 0.661 | 1.10 (0.77 to 1.57) | 0.617 |
| Surgical site infection | 1.25% | 1.30% | 0.96 (0.76 to 1.24) | 0.798 | 0.94 (0.73 to 1.20) | 0.609 |
| Sepsis or septic shock | 0.38% | 0.34% | 1.12 (0.71 to 1.79) | 0.623 | 1.11 (0.70 to 1.77) | 0.662 |
| Cardiac arrest | 0.12% | 0.02% | 4.81 (1.10 to 21.1) | 0.037 | 5.04 (1.15 to 22.07) | 0.032 |
| Myocardial infarction | 0.26% | 0.24% | 1.06 (0.61 to 1.84) | 0.840 | 1.14 (0.65 to 1.99) | 0.648 |
| Acute renal failure | 0.08% | 0.06% | 1.28 (0.44 to 3.76) | 0.648 | 1.32 (0.45 to 3.86) | 0.617 |
| Return to the operating room | 1.76% | 1.88% | 0.93 (0.76 to 1.15) | 0.507 | 0.93 (0.76 to 1.14) | 0.489 |
| Wound dehiscence | 0.13% | 0.09% | 1.55 (0.65 to 3.76) | 0.323 | 1.53 (0.63 to 3.70) | 0.344 |
| Graft, prosthesis, or flap failure | 0.03% | 0.01% | 2.56 (0.29 to 22.98) | 0.399 | 2.67 (0.30 to 23.98) | 0.380 |
| Peripheral nerve injury | 0.07% | 0.06% | 1.15 (0.39 to 3.45) | 0.796 | 1.11 (0.37 to 3.31) | 0.857 |
| Any minor adverse event | 20.95% | 17.14% | 1.28 (1.19 to 1.38) | <0.001 | 1.35 (1.25 to 1.45) | <0.001 |
| Blood transfusion | 19.79% | 16.24% | 1.27 (1.18 to 1.37) | <0.001 | 1.34 (1.25 to 1.45) | <0.001 |
| Urinary tract infection | 1.29% | 1.04% | 1.24 (0.96 to 1.63) | 0.098 | 1.29 (0.99 to 1.68) | 0.056 |
| Pneumonia | 0.31% | 0.22% | 1.39 (0.79 to 2.43) | 0.247 | 1.45 (0.83 to 2.53) | 0.198 |
| Progressive renal insufficiency | 0.11% | 0.04% | 3.00 (0.86 to 10.43) | 0.085 | 2.92 (0.84 to 10.19) | 0.092 |
| Readmission# | 3.60% | 3.39% | 1.06 (0.91 to 1.25) | 0.444 | 1.09 (0.93 to 1.29) | 0.291 |
The values are given as the percentage of patients.
The values are given as the odds ratio, with the 95% CI in parentheses.
Significance was set at p < 0.05.
Each line represents a separate multivariate analysis for each variable to give an adjusted odds ratio and p value by controlling for patient characteristics and propensity score.
Readmission data were available only for 2011 and 2012: 18,128 patients, 10,988 (60.6%) of whom received general anesthesia.
On bivariate analyses, general anesthesia was associated with significantly increased rates of any adverse event, prolonged postoperative ventilator use, unplanned intubation, cardiac arrest, any minor adverse event, and blood transfusion. On multivariate analyses, any adverse event (odds ratio, 1.31 [95% CI, 1.23 to 1.41]; p < 0.001), prolonged postoperative ventilator use (odds ratio, 5.81 [95% CI, 1.35 to 25.06]; p = 0.018), unplanned intubation (odds ratio, 2.17 [95% CI, 1.11 to 4.29]; p = 0.024), stroke (odds ratio, 2.51 [95% CI, 1.02 to 6.20]; p = 0.046), cardiac arrest (odds ratio, 5.04 [95% CI, 1.15 to 22.07]; p = 0.032), any minor adverse event (odds ratio, 1.35 [95% CI, 1.25 to 1.45]; p = 0.001), and blood transfusion (odds ratio, 1.34 [95% CI, 1.25 to 1.45]; p < 0.001) were associated with general anesthesia.
No significant difference in the rate of readmission within thirty days was found between anesthesia types.
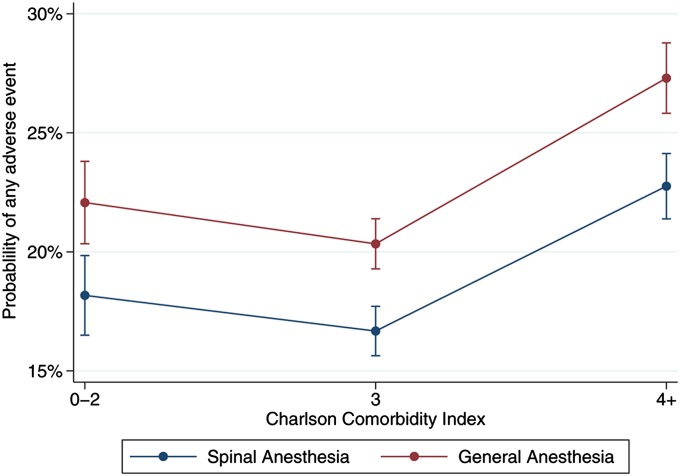
To compare outcomes between anesthesia types for patients with varying degrees of comorbidity, the predicted probability of any adverse event was calculated for each combination of anesthesia type and Charlson Comorbidity Index range, using the multivariate model for the occurrence of any adverse event. These results, with 95% CIs, are illustrated in Figure 1. Predicted probabilities represent the probability of any adverse event occurring given the observed anesthesia type and Charlson Comorbidity Index range, while holding other covariates in the model at their mean value. The predicted probability of any adverse event occurring was significantly increased with general anesthesia for all ranges of the Charlson Comorbidity Index. For the lowest Charlson Comorbidity Index category (0 to 2), the predicted probability of any adverse event was significantly greater (p < 0.001) for general anesthesia (22.1%) compared with spinal anesthesia (18.2%). Similarly, for a Charlson Comorbidity Index of 3, the predicted probability of any adverse event was also significantly greater (p < 0.001) for general anesthesia (20.3%) compared with spinal anesthesia (16.7%). For patients with the highest Charlson Comorbidity Index category (≥4), the predicted probability of any adverse event was also significantly greater (p < 0.001) for general anesthesia (27.3%) compared with spinal anesthesia (22.8%).
Fig. 1.
The predicted probability of any adverse event within thirty days of primary elective total hip arthroplasty, by anesthesia type and modified Charlson Comorbidity Index.
Discussion
General and spinal anesthesia are both commonly used during total hip arthroplasty; however, to our knowledge, no large, multicenter study has assessed the difference in short-term outcomes associated with either anesthesia type in patients undergoing total hip arthroplasty. The current investigation used prospectively collected data from a large, national cohort of patients who had undergone elective primary total hip arthroplasty to compare operating room times, length of stay, adverse events, and readmission between general and spinal anesthesia.
In this study, we found that general anesthesia was associated with increased odds of any adverse event, prolonged postoperative ventilator use, unplanned intubation, stroke, cardiac arrest, any minor adverse event, and blood transfusion following elective primary total hip arthroplasty. In addition, general anesthesia was associated with mild increases in operative time and postoperative room time. There was no association found between anesthesia type and postoperative length of stay or readmission.
The association of general anesthesia with any adverse event in this study is consistent with the results of several previous studies that have shown a benefit of neuraxial anesthesia relative to general anesthesia in terms of the risk of complications in orthopaedic patients3-8,17. However, to our knowledge, this is the largest study to date that has compared operating room times, length of stay, adverse events, and readmission between patients who had undergone elective primary total hip arthroplasty with general anesthesia and those who had undergone elective primary total hip arthroplasty with spinal anesthesia, further supporting the advantages of spinal anesthesia in these patients. In addition, we found that general anesthesia was associated with an increased predicted probability of any adverse event among all studied ranges of medical comorbidity. Spinal anesthesia has been previously associated with improved postoperative outcomes compared with general anesthesia in medically complex patients undergoing total joint arthroplasty16; however, this study indicates that these benefits may also extend to patients with fewer medical comorbidities.
Among individual adverse events, general anesthesia was associated with the occurrence of pulmonary complications, namely prolonged postoperative ventilator use and unplanned intubation. General anesthesia has been previously shown to be associated with pulmonary adverse events following total hip arthroplasty18.
Increased rates of stroke and cardiac arrest were also found to be associated with general anesthesia. These relationships have not been previously described in the literature. These adverse events may be associated with the increased incidence of intraoperative hypotension that has been described with general anesthesia compared with neuraxial anesthesia19. Another possible cause of this relationship is through the thrombotic pathway, as general anesthesia has been reported to increase the risk of thromboembolic events5,20,21. However, in the current study, although we found a very slight increase in the unadjusted rates of deep vein thrombosis or pulmonary embolism for patients who had received general anesthesia, this increase did not reach significance on either bivariate or multivariate analyses.
We also found a significantly increased rate of blood transfusion associated with general anesthesia. This relationship has been repeatedly described in the hip arthroplasty literature4,5,7,21-29. Blood loss during total hip arthroplasty performed under general anesthesia is often a function of how well a low blood pressure is maintained during the procedure28. Unfortunately, information on intraoperative blood pressure is not captured in the ACS-NSQIP database, so the effect of this variable on blood loss is unknown for this study.
General anesthesia was additionally found to be associated with slightly increased operating room times. Similar findings have been reported in the total hip arthroplasty literature5,7,21. This relationship may exist because high-volume surgical centers may be more likely to use spinal anesthesia and may have decreased operative time and room turnover time compared with other centers. In addition, patient extubation likely adds to the postoperative room time. However, despite the significance of these findings, there may be little clinical importance of these minor increases in operating room times.
Despite the reported benefits of spinal anesthesia relative to general anesthesia, it is notable that the majority of total hip arthroplasty cases (60.9%) included in this national sample utilized general anesthesia. We believe that this finding is likely due to patient and institutional factors. To provide the best perioperative care for patients undergoing total hip arthroplasty, it is important for patients, surgeons, anesthesiologists, and hospital administrators to be aware of the advantages of spinal anesthesia when planning these procedures.
It is also important to note that spinal anesthesia is not without risks. Permanent injury to the spinal cord or spinal nerves is a serious complication that can occur with neuraxial anesthesia; however, it is exceedingly rare, with a reported incidence of <4 in 100,00030. Transient postoperative neurologic deficits and postdural puncture headache are also associated with the use of spinal anesthesia31,32.
This study was limited by the characteristics of the ACS-NSQIP database. The ACS-NSQIP only collects the occurrence of adverse events up to thirty days postoperatively, so any events that occurred after this period would not have been captured. However, adverse outcomes due to anesthesia type are likely most evident in the short term, making this time period ideal for this study. In addition, orthopaedic-specific outcomes such as postoperative pain and functional outcomes are unknown. Despite this limitation, we believe that the large patient numbers and high-quality data collection process used by the ACS-NSQIP outweighs the lack of certain variables. Although the data were collected prospectively, patients were not randomized, thus introducing the possibility of bias into the data analysis. We attempted to correct for this by using propensity score-adjusted models. Although we were able to control for factors available in the database, we were unable to control for any demographic, logistical, or patient variables that were not available in the database. An additional limitation was that it is unknown whether spinal anesthesia was initiated outside of the operating room or in the operating room, a practice that differs based on institution. Although this could potentially influence the preoperative room time or the total room time, this would not affect the results of this study for operative time and postoperative room time.
Using prospectively collected data from a large, national cohort of patients who had undergone primary elective total hip arthroplasty, this study found that general anesthesia was associated with a significantly increased rate of adverse events compared with spinal anesthesia. Furthermore, the predicted probability of adverse events was elevated for general anesthesia across all comorbidity ranges. General anesthesia was also shown to be associated with a significant but relatively small increase in time spent in the operating room.
Appendix
A table showing definitions of adverse events is available with the online version of this article as a data supplement at jbjs.org.
A table showing definitions of adverse events.
Footnotes
Investigation performed at the Department of Orthopaedics and Rehabilitation, Yale University School of Medicine, New Haven, Connecticut
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
Disclaimer: The content of this publication is solely the responsibility of the authors and does not necessarily represent official views of the National Institutes of Health.
References
- 1.Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012November17;380(9855):1768-77 Epub 2012 Sep 26. [DOI] [PubMed] [Google Scholar]
- 2.Indelli PF, Grant SA, Nielsen K, Vail TP. Regional anesthesia in hip surgery. Clin Orthop Relat Res. 2005December;441:250-5. [DOI] [PubMed] [Google Scholar]
- 3.Davis FM, Laurenson VG, Gillespie WJ, Wells JE, Foate J, Newman E. Deep vein thrombosis after total hip replacement. A comparison between spinal and general anaesthesia. J Bone Joint Surg Br. 1989March;71(2):181-5. [DOI] [PubMed] [Google Scholar]
- 4.Rashiq S, Finegan BA. The effect of spinal anesthesia on blood transfusion rate in total joint arthroplasty. Can J Surg. 2006December;49(6):391-6. [PMC free article] [PubMed] [Google Scholar]
- 5.Hu S, Zhang ZY, Hua YQ, Li J, Cai ZD. A comparison of regional and general anaesthesia for total replacement of the hip or knee: a meta-analysis. J Bone Joint Surg Br. 2009July;91(7):935-42. [DOI] [PubMed] [Google Scholar]
- 6.Chang CC, Lin HC, Lin HW, Lin HC. Anesthetic management and surgical site infections in total hip or knee replacement: a population-based study. Anesthesiology. 2010August;113(2):279-84. [DOI] [PubMed] [Google Scholar]
- 7.Maurer SG, Chen AL, Hiebert R, Pereira GC, Di Cesare PE. Comparison of outcomes of using spinal versus general anesthesia in total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2007July;36(7):E101-6. [PubMed] [Google Scholar]
- 8.Gonano C, Leitgeb U, Sitzwohl C, Ihra G, Weinstabl C, Kettner SC. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply costs. Anesth Analg. 2006February;102(2):524-9 Epub 2006 Jan 24. [DOI] [PubMed] [Google Scholar]
- 9.American College of Surgeons. User Guide for the 2012 ACS NSQIP Participant Use Data File. 2013. http://site.acsnsqip.org/wp-content/uploads/2013/10/ACSNSQIP.PUF_.UserGuide.2012.pdf. Accessed 2014 Oct 20.
- 10.Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA Jr, Fink AS, Mentzer RM Jr, Neumayer L, Hammermeister K, Mosca C, Healey N; Principal Investigators of the Patient Safety in Surgery Study. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Ann Surg. 2008August;248(2):329-36 Epub 2008 Jul 25. [DOI] [PubMed] [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. [DOI] [PubMed] [Google Scholar]
- 12.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004December;57(12):1288-94. [DOI] [PubMed] [Google Scholar]
- 13.D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996December;49(12):1429-33. [DOI] [PubMed] [Google Scholar]
- 14.Ehlert BA, Nelson JT, Goettler CE, Parker FM, Bogey WM, Powell CS, Stoner MC. Examining the myth of the “July Phenomenon” in surgical patients. Surgery. 2011August;150(2):332-8 Epub 2011 Jun 30. [DOI] [PubMed] [Google Scholar]
- 15.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998October15;17(19):2265-81. [DOI] [PubMed] [Google Scholar]
- 16.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013February6;95(3):193-9 Epub 2012 Dec 28. [DOI] [PubMed] [Google Scholar]
- 17.Chakladar A, White SM. Cost estimates of spinal versus general anaesthesia for fractured neck of femur surgery. Anaesthesia. 2010August;65(8):810-4 Epub 2010 May 27. [DOI] [PubMed] [Google Scholar]
- 18.Hole A, Terjesen T, Breivik H. Epidural versus general anaesthesia for total hip arthroplasty in elderly patients. Acta Anaesthesiol Scand. 1980August;24(4):279-87. [DOI] [PubMed] [Google Scholar]
- 19.Borghi B, Casati A, Iuorio S, Celleno D, Michael M, Serafini P, Pusceddu A, Fanelli G; Study Group on Orthopedic Anesthesia of the Italian Society of Anesthesia, Analgesia, and Intensive Care (SIAARTI). Frequency of hypotension and bradycardia during general anesthesia, epidural anesthesia, or integrated epidural-general anesthesia for total hip replacement. J Clin Anesth. 2002March;14(2):102-6. [DOI] [PubMed] [Google Scholar]
- 20.Modig J, Borg T, Karlström G, Maripuu E, Sahlstedt B. Thromboembolism after total hip replacement: role of epidural and general anesthesia. Anesth Analg. 1983February;62(2):174-80. [PubMed] [Google Scholar]
- 21.Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesth Analg. 2006October;103(4):1018-25 Epub 2006 Sep 27. [DOI] [PubMed] [Google Scholar]
- 22.Keith I. Anaesthesia and blood loss in total hip replacement. Anaesthesia. 1977May;32(5):444-50. [DOI] [PubMed] [Google Scholar]
- 23.Thorburn J, Louden JR, Vallance R. Spinal and general anaesthesia in total hip replacement: frequency of deep vein thrombosis. Br J Anaesth. 1980November;52(11):1117-21. [DOI] [PubMed] [Google Scholar]
- 24.Davis FM, McDermott E, Hickton C, Wells E, Heaton DC, Laurenson VG, Gillespie WJ, Foate J. Influence of spinal and general anaesthesia on haemostasis during total hip arthroplasty. Br J Anaesth. 1987May;59(5):561-71. [DOI] [PubMed] [Google Scholar]
- 25.Modig J, Karlström G. Intra- and post-operative blood loss and haemodynamics in total hip replacement when performed under lumbar epidural versus general anaesthesia. Eur J Anaesthesiol. 1987September;4(5):345-55. [PubMed] [Google Scholar]
- 26.Flordal PA, Neander G. Blood loss in total hip replacement. A retrospective study. Arch Orthop Trauma Surg. 1991;111(1):34-8. [DOI] [PubMed] [Google Scholar]
- 27.Brinker MR, Reuben JD, Mull JR, Cox DD, Daum WJ, Parker JR. Comparison of general and epidural anesthesia in patients undergoing primary unilateral THR. Orthopedics. 1997February;20(2):109-15. [DOI] [PubMed] [Google Scholar]
- 28.Thompson GE, Miller RD, Stevens WC, Murray WR. Hypotensive anesthesia for total hip arthroplasty: a study of blood loss and organ function (brain, heart, liver, and kidney). Anesthesiology. 1978February;48(2):91-6. [PubMed] [Google Scholar]
- 29.Borghi B, Casati A, Iuorio S, Celleno D, Michael M, Serafini PL, Alleva R. Effect of different anesthesia techniques on red blood cell endogenous recovery in hip arthroplasty. J Clin Anesth. 2005March;17(2):96-101. [DOI] [PubMed] [Google Scholar]
- 30.Cook TM, Counsell D, Wildsmith JA; Royal College of Anaesthetists Third National Audit Project. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br J Anaesth. 2009February;102(2):179-90 Epub 2009 Jan 12. [DOI] [PubMed] [Google Scholar]
- 31.Kang XH, Bao FP, Xiong XX, Li M, Jin TT, Shao J, Zhu SM. Major complications of epidural anesthesia: a prospective study of 5083 cases at a single hospital. Acta Anaesthesiol Scand. 2014August;58(7):858-66 Epub 2014 Jun 24. [DOI] [PubMed] [Google Scholar]
- 32.Faridi Tazeh-Kand N, Eslami B, Ghorbany Marzony S, Abolhassani R, Mohammadian K. Injection of intrathecal normal saline in decreasing postdural puncture headache. J Anesth. 2014April;28(2):206-9 Epub 2013 Aug 2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A table showing definitions of adverse events.