Abstract
Background & Objective
Multiple Breath Washout (MBW) systems are designed to minimize equipment dead space volume (Vd). Animal and infant studies have demonstrated the impact of increased Vd on MBW measurements. In this study we investigate the effect of Vd of a N2MBW system affects MBW measurements in preschool children.
Methods
N2MBW measurements were performed in healthy adults under standard conditions; Vd was added to match the relationship between Vd and lung volumes observed in preschool children. Subsequently, subjects were measured on a SF6MBW system under standard conditions, and with Vd added to match that of the N2MBW system. Healthy preschool children and children with cystic fibrosis were tested on both the N2MBW and SF6MBW in random order on the same day. A correction equation was derived based on the adult experiments and tested on the preschool data.
Results
Increasing the Vd of the N2MBW system resulted in a higher Lung Clearance Index (LCI). A strong non-linear relationship between N2LCI and the Vd/Vt was observed. When the Vd was equivalent between systems, LCI measured by the SF6MBW system was similar to that measured by the N2MBW. LCI was higher on the N2MBW than the SF6MBW in preschool children. Correcting for the equipment Vd of the N2MBW resulted in better agreement.
Conclusions
Equipment Vd affects LCI measurements, especially in young children where Vd is large relative to lung volumes.
Keywords: Multiple breath washout, Lung clearance index, Dead space, Preschool children, Cystic fibrosis
INTRODUCTION
The multiple breath inert gas washout (MBW) technique is a tidal breathing test that assesses ventilation distribution uniformity. The most commonly reported MBW outcome is the Lung Clearance Index (LCI), which represents the cumulative sum of tidal volumes (Vt) required to clear the lungs of an inert marker gas. In diseases such as cystic fibrosis (CF), the LCI has been shown to be abnormal early in the course of disease, and to be more sensitive to detect early lung function abnormalities than traditional outcome parameters such as the FEV1 (1–4). The MBW test requires minimal passive co-operation and can be performed in young children, making it ideal for preschool age children who stand to benefit most from early intervention.
Most evidence in support of MBW has been collected on a respiratory mass spectrometer based system, that runs on non-commercial commissioned software and uses sulfur hexafluoride (SF6) as a tracer gas (4). More recently less expensive and commercially available nitrogen (N2) based MBW systems have become available. Jensen et al., showed that one of the available N2 MBW systems is a feasible, but nonequivalent, alternative to the SF6 MBW, and that LCI measured by N2 MBW was systematically higher (5). The difference in observed LCI values may be the result of N2 gas from slowly ventilated lung regions not captured using an exogenous tracer gas such as SF6, the diffusion of tissue N2 from the blood into the alveoli, or the differences in equipment design, including differences in equipment dead space volume (Vd).
In MBW systems, equipment Vd represents the volume of the breathing circuit between the subject and the flow stream of fresh gas (2, 6). Equipment Vd is distinct from anatomic Vd, which is in principal the volume of the conductive airways(6). The volume of gas that reaches the lung with each breath is relative to the volume of equipment Vd, such that a high equipment Vd means that less fresh gas reaches the lung with each breath. Therefore MBW systems are designed to minimize equipment Vd, and measured respiratory volumes (i.e. tidal volume (Vt) and functional residual capacity (FRC)) are corrected for equipment Vd. However, Vd corrections are fixed equipment-dependent volumes and therefore do not consider the Vd relative to the subjects’ size (7–10). In adults and older children the equipment Vd is relatively small compared to lung volumes and therefore may have minimal impact on the measurement. In young children with small lung volumes, the proportion of equipment Vd to total lung volume is relatively large, and may impact breathing patterns and /or LCI values. Previous animal(11) and infant(12) studies have demonstrated the impact of increasing Vd on MBW measurements. Whether this is the case for MBW measurements in preschool children is currently unclear.
In this study we investigate: 1) whether altering Vd of the N2 MBW over the range observed in preschool children affects LCI measurements, 2) whether differences in equipment Vd between SF6 MBW and N2 MBW explain the differences observed in LCI, 3) how equipment Vd impacts MBW measurements performed in preschool children, and 4) whether the Vd experiments could be utilized to estimate a correction factor for the effect of Vd in preschool children.
METHODS
Healthy adults, with no history of respiratory disease or current respiratory symptoms, were recruited at the Hospital for Sick Children. Detailed inclusion and exclusion criteria can be found in the online supplement (Online Supporting Information). This study was approved by the research ethics board at the Hospital for Sick Children, Toronto, Canada (1000019445). Informed written consent was obtained from parents or guardians of healthy children and children with CF, and from adult subjects.
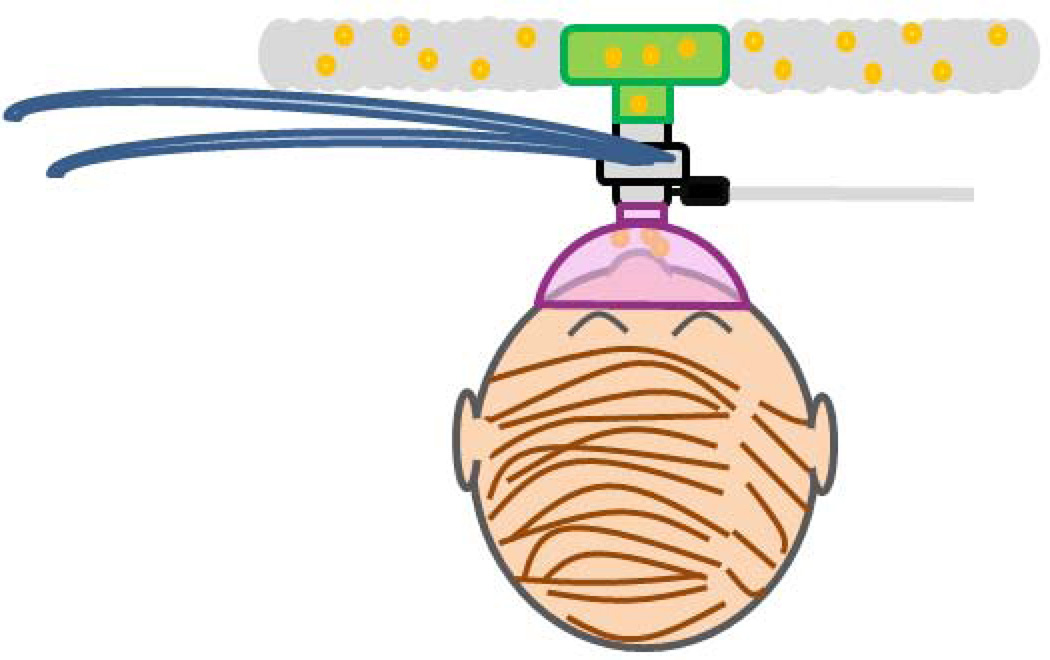
N2 MBW was performed using an open circuit, bias flow system (Exhalyzer D®, EcoMedics AG, Duernten, Switzerland) and associated software (Spiroware® 3.1 EcoMedics AG). Vd was added to the standard equipment set-up (Figure 1a) using a series of airtight resin boxes placed between the filter and the gas sampling point (Supplementary Figure S1). Each of the four boxes systematically increased the pre gas sampling point Vd of the system by approximately 50ml. Subjects were assigned to perform MBW measurements, in triplicate, for each of the four Vd conditions in random order; testing with the standard set-up was always done first. All subjects adhered to individual weight dependent visual tidal volume targets (10–15 ml/kg body weight), as such tidal volume was constant across the equipment Vd condition.
Figure 1.
a) N2 MBW set up b) SF6 MBW set up
SF6 MBW was performed on a mass spectrometer (AMIS 200; Innovision A/S, Odense, Denmark) system using a pneumotachograph (3700 series Hans Rudolph, Shawnee, KS, USA). Subjects were tested on the standard SF6 MBW set up (Total Vd 15.4ml; Figure 1b) and with the Vd increased to match the pre and post sampling point Vd of the N2 MBW (58.2 ml). Pre sampling point Vd was added by connecting a plastic connector and a filter in sequence between the mouthpiece and the pneumotachograph. Post gas sampling point Vd was added by connecting a plastic connector in sequence after the pneumotachograph. Standard SF6 MBW, standard N2 MBW, and SF6 MBW with Vd equivalent to the N2 system was measured in all 10 participants in triplicate, and in random order.
Calculation of LCI
N2 MBW results were calculated in Spiroware® with measured volumes corrected for fixed standard pre (33.3 ml) and post (24.9 ml) sampling point Vd. SF6 MBW data files were analyzed by a single trained observer using custom written analysis software written by one of the authors; PG (Test-Point, Capital Equipment Corp., Billerica, MA, USA). Measured volumes on the SF6 MBW were corrected for the standard 15.4 ml of post-cap Vd. Trials from both systems were evaluated for quality control criteria including identification of leaks, breath pattern stability and appropriate tidal volume for size as outlined in the inert gas washout consensus statement (4).
Estimating a correction factor for Vd
Using data from the adult N2 Vd experiments we investigated the relationship between LCI and Vd using three Vd corrections (Vd/ body weight, Vd/Vt and Vd/FRC); total Vd was measured by water displacement for each added Vd condition. Based on these observations, we investigated linear and non-linear regression equation until the one with best fit was identified. Generalized estimating equation models were used to adjust for repeated measurements within the same subject. We subsequently tested whether the resulting regression equation could be used to re-calculate LCI observed in adults under added Vd conditions and if this result would better match the LCI observed under standard Vd conditions (58.2ml). We also tested whether the equations could be used to recalculate LCI to a standard Vd/Vt ratio (e.g. 0.1)
Preschool MBW Testing
Children with a diagnosis of CF between the ages of 2.5 and 6 years, and age matched healthy controls were recruited into a cross-sectional comparison study. Inclusion and exclusion criteria are detailed in the Online Supporting Information document. Measurements in preschool children were performed as previously described (5). Briefly, children performed N2 MBW and SF6 MBW in triplicate on the same day in random order. All children were tested using standard, size appropriate N2 MBW equipment (Set 2) and settings (48.7 ml Vd). In addition all measurements were made using an appropriately sized facemask filled with therapeutic putty; maximum amount of putty was added to each facemask to minimize Vd without entirely obstructing the mask opening. Mask Vd was not accounted in the equipment Vd. LCI values were calculated in the same manner as described above.
Statistical Analysis
Measurements were summarized as mean, standard deviation (SD) and percent coefficient of variation (%CV), defined as the standard deviation of a measure divided by the mean times 100. N2 MBW and SF6 MBW outcomes were compared between systems using Bland-Altman plots.
RESULTS
The effect of Vd on MBW in Controlled Experiments
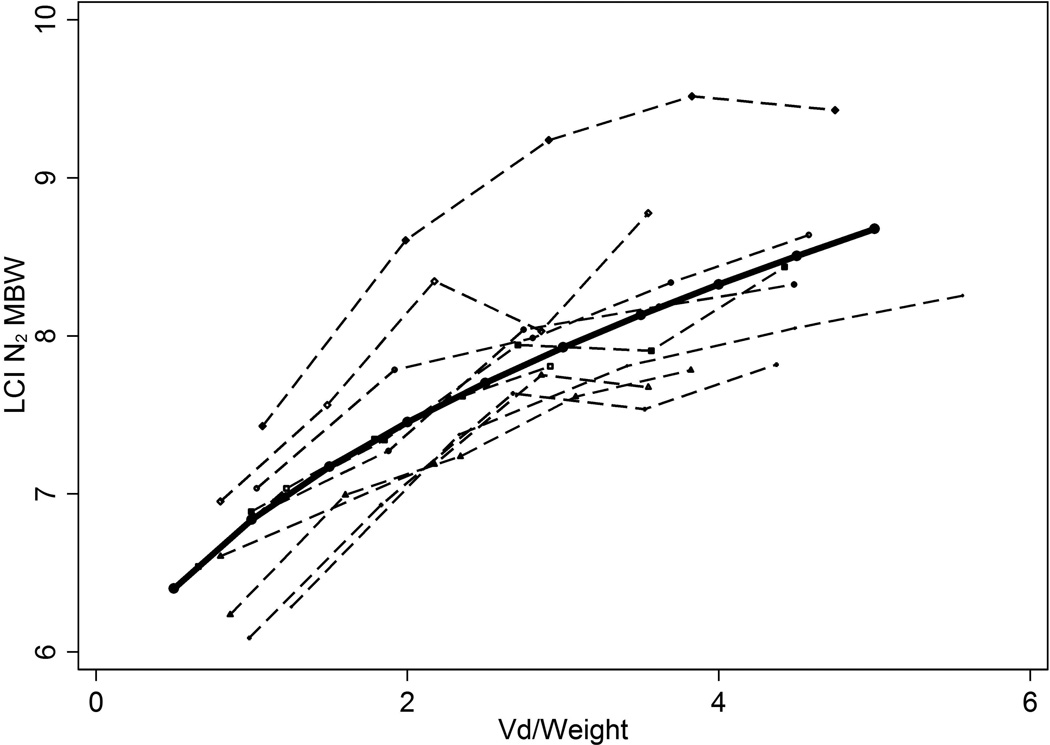
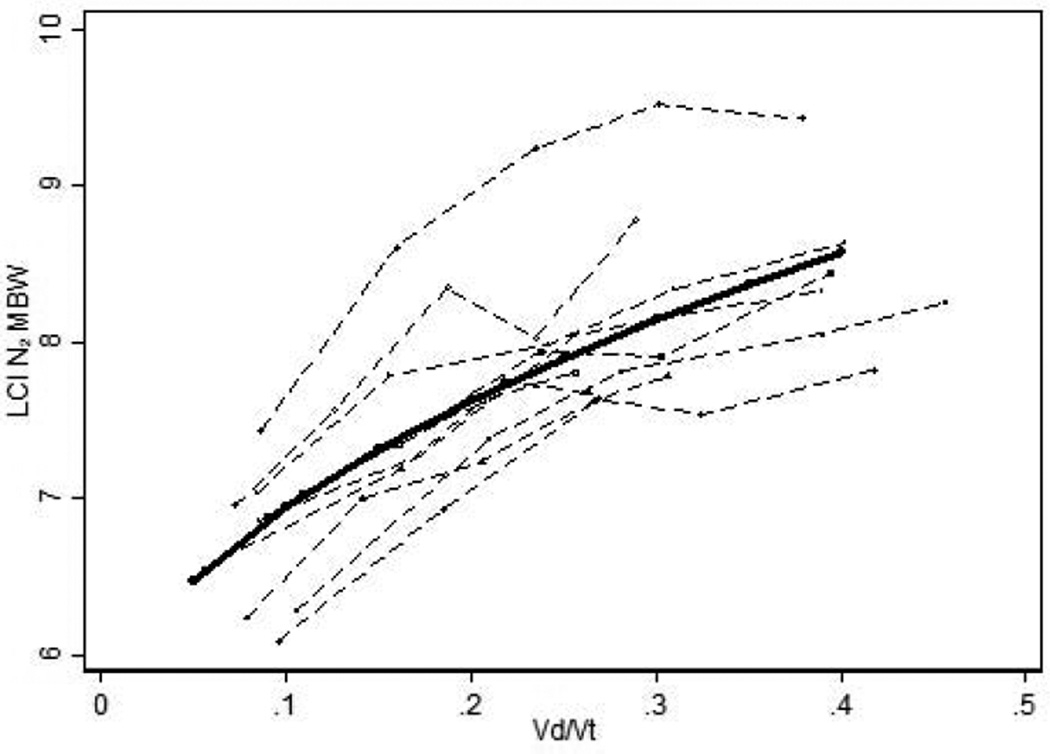
Ten healthy adults (24.7 years (SD 9.5); 6 females) completed the controlled experiments. As the Vd of the N2 system increased (58.2 ml + box volume), so did the N2 LCI (Table 1). The within-test occasion variability (%CV) of N2 LCI was similar for all Vd conditions. The FRC was constant across the added Vd conditions, whereas the CEV and number of breaths required to complete the washout increased. Vt and respiratory rate were not affected by increasing Vd, and thus minute ventilation did not change. There was a strong non-linear relationship whereby the N2 LCI increased as a function of Vd/weight (Figure 2a), Vd/Vt (Figure 2b) and Vd/FRC (Figure 2c).
Table 1.
Summary of Vd experiments performed in adult subjects on both the N2 MBW and SF6 MBW systems
| N2 MBW | ||||||
|---|---|---|---|---|---|---|
| Standard Vd | + 50ml Vd | + 100 ml Vd | +150 ml Vd | + 200 ml Vd | P value | |
| Pre sampling point Vd (ml) | 33.3 | 89.3 | 144.8 | 187.8 | 236.5 | - |
| Total Vd (ml) | 58.2 | 114.2 | 169.7 | 212.8 | 261.4 | - |
| LCI | 6.69 (0.42) | 7.43 (0.52) | 7.90 (0.64) | 8.05 (0.58) | 8.30 (0.55) | <0.001 |
| LCI % CV mean | 3.45 | 2.60 | 2.78 | 2.64 | 3.54 | 0.973 |
| FRC | 3.56 (0.93) | 3.08 (0.67) | 3.41 (0.79) | 3.40 (0.78) | 3.43 (0.84) | 0.582 |
| CEV | 25.83 (6.58) | 25.04 (5.74) | 29.13 (6.4) | 29.65 (6.48) | 30.78 (7.32) | <0.001 |
| Number of Breaths | 36.6 (6.86) | 36.0 (8.52) | 40.53 (7.8) | 40.17 (7.67) | 41.6 (8.13) | <0.001 |
| Vt | 734.0 (148.0) | 712.3 (145.4) | 732.7 (152.7) | 751.32 (152.7) | 753.6 (160.4) | 0.193 |
| Respiratory Rate | 12.2 (2.2) | 12.5 (1.72) | 12.70 (2.62) | 12.49 (2.3) | 12.6 (2.14) | 0.354 |
| SF6 MBW | ||||||
| Standard Vd | + N2 Vd | P value | ||||
| Pre sampling point Vd (ml) | 0 | 33.3 | ||||
| Post sampling point Vd (ml) | 15.4 | 24.9 | ||||
| Total Vd (ml) | 15.4 | 58.2 | ||||
| LCI | 6.58 (0.83) | 6.76 (0.79) | 0.087 | |||
| LCI % CV mean | 2.78 | 3.02 | 0.758 | |||
| FRC | 2.42 (0.64) | 2.56 (0.78) | 0.0142 | |||
| CEV | 15.97 (4.53) | 17.2 (5.0) | <0.001 | |||
| Number of Breaths | 31.16 (14.0) | 31.4 (13.18) | 0.3894 | |||
| Vt | 584.24 (171.8) | 607.86 (169.54) | 0.0767 | |||
| Respiratory Rate | 15.0 (5.36) | 13.90 (6.52) | 0.0329 | |||
Data presented as mean (SD) unless otherwise indicated.
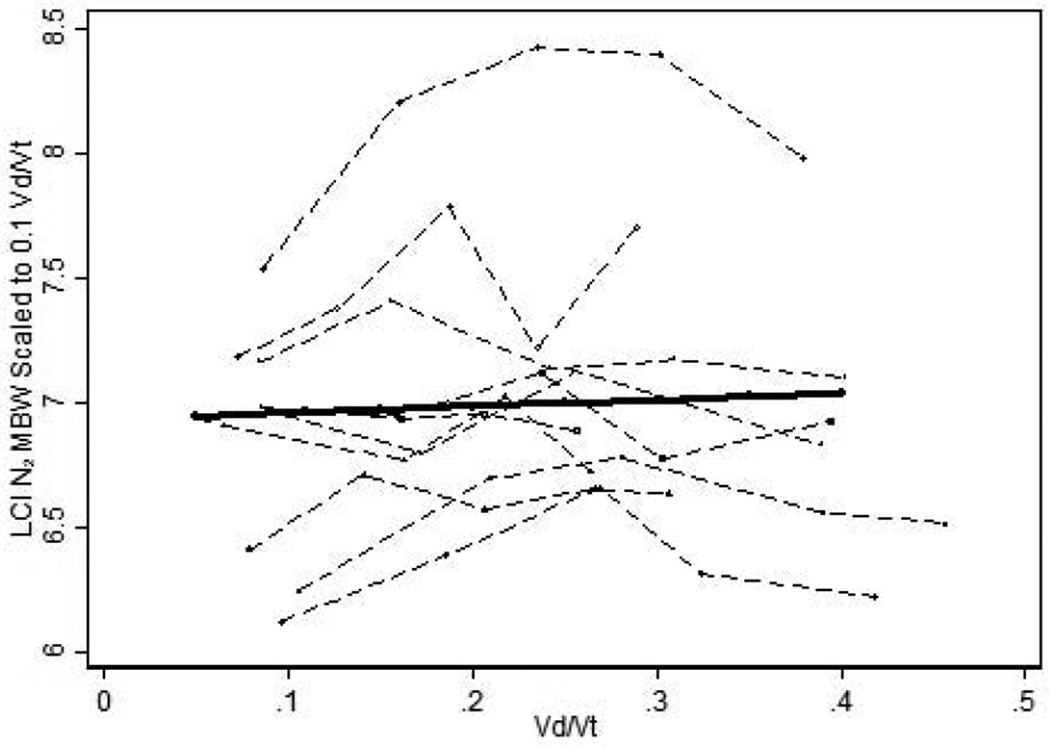
Figure 2.
The relationship between LCI and a) Vd/weight b) Vd/Vt and c) Vd/FRC. Each point represents the average LCI of at least two measurements, each dashed line represents one individual and the solid black line is the model of best fit of the entire dataset.
Under standard conditions (Figure 1), LCI measured by the N2 MBW was on average 0.14 unit (95% CI - −0.53; 0.25) higher than that measured on the SF6 MBW. When the Vd of the SF6 system was increased to match that of the N2 MBW, the LCI increased by 0.18 units, such that the SF6 LCI measured with N2 Vd was slightly higher (mean difference 0.05 (95% CI −0.36; 0.45)) than N2 LCI.
Estimating a correction factor for Vd
Based on the observed relationships we estimated a correction factor based on Vd/Vt. This relationship was best described by a nonlinear square root model (Equation 1).
| Equation 1: |
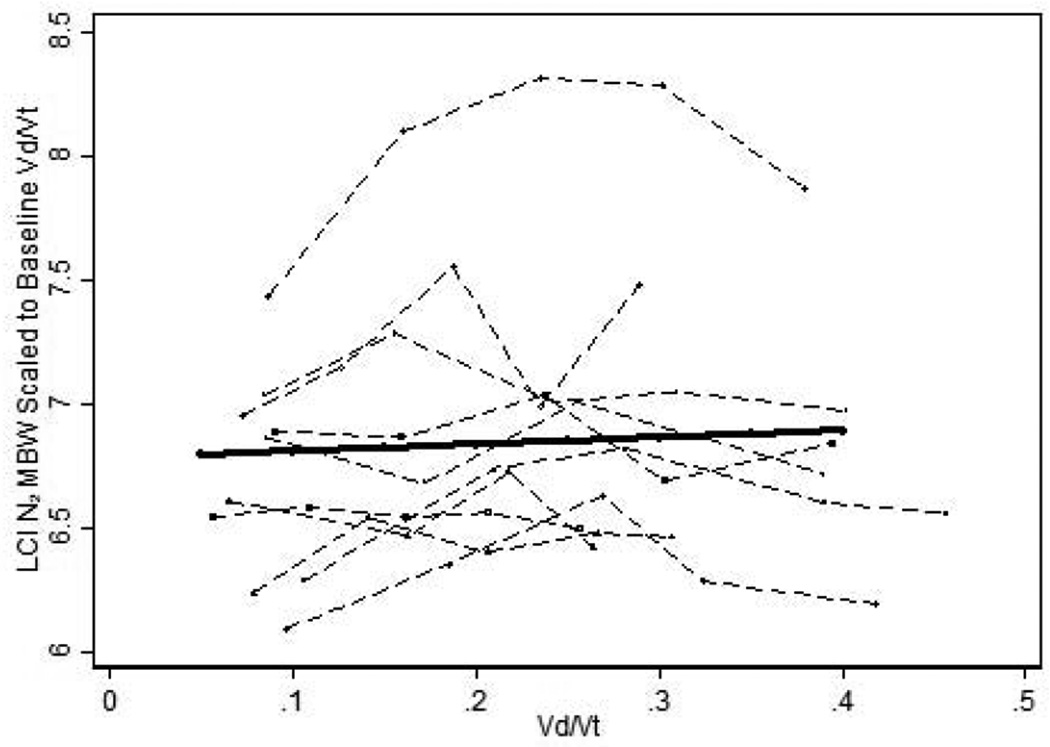
Using a subjects’ own observed Vd/Vt at baseline, we re-calculated LCI for each of the added Vd conditions to this known baseline value using Equation 1 (for details see Online Supporting Information). Correcting the Vd attenuated the observed effect of Vd on N2 LCI values (Figure3a). Since in non-experimental conditions the baseline Vd/Vt will not be known, we also corrected LCI values to a common reference point (0.1) using Equation 1. This value was chosen as it is the average Vd/Vt ratio observed in our sample of adults at baseline. Similar to what we observed with baseline values, it was also possible to correct LCI values using a common reference point (Figure 3b).
Figure 3.
a) N2 LCI scaled to baseline Vd/Vt and b) scaled to 0.1 Vd/Vt. Each dashed line represents one individual. The solid black line is the generalized estimation equation model adjusted for repeated measures.
The effect of Vd on MBW in Preschool Children
Twenty-four healthy children and twenty-seven children with CF were enrolled for the comparison study, of which twenty healthy children (83.3%) and nineteen children with CF (70.4%) completed both N2 MBW and SF6 MBW testing and met quality control standards (Table 2). Baseline characteristics for both groups were similar except healthy children were taller and heavier (Table 2). LCI measured by both the N2 and SF6 systems distinguished between health and CF, but LCI was consistently higher on the N2 MBW system (mean difference N2 - SF6 (1.26 (95% CI 1.01; 1.59)). N2 MBW testing required more time and a greater number of breaths to clear the tracer gas
Table 2.
Characteristics of the preschool study population and summary of their MBW outcomes.
| Health (n=20) | CF (n=18) | Mean difference (CI) | P value | |
|---|---|---|---|---|
| % females | 55.0% | 66.67% | 11.67 (−19%; 42%) | 0.462 |
| Age (years) mean(range) | 4.2 (2.8–5.9) | 4.5 (3.3–5.9) | 0.28 (−0.34; 0.89) | 0.371 |
| Weight centile-for-age mean(SD) | 66.56 (16.98) | 49.68 (24.59) | −16.88 (−30.67; −3.09) | 0.018 |
| Height centile-for-age mean(SD) | 64.48 (21.88) | 46.75 (24.91) | −17.73 (−33.12; −2.33) | 0.025 |
| SF6 Vd/weight (ml/kg) mean (range) | 0.88 (0.64–1.08) | 0.92 (0.69–1.13) | 0.03 (0.05; 0.12) | 0.431 |
| N2 Vd/weight (ml/kg) mean (range) | 1.87 (1.49–2.55) | 2.10 (0.89–3.15) | 0.24 (−0.07; 0.54) | 0.122 |
| Mean difference (CI) SF6-N2 | 0.99 (0.84; 1.13) | 1.19 (0.91; 1.47) | ||
| SF6 Vd/Vt mean (SD) | 0.08 (0.01) | 0.08 (0.01) | 0.003 (−0.01; 0.01) | 0.486 |
| N2 Vd/Vt mean (SD) | 0.17 (0.02) | 0.18 (0.05) | −0.01 (−0.03; 0.01) | 0.548 |
| Mean difference (CI) SF6-N2 | 0.08 (0.07; 0.10) | 0.10 (0.07; 0.12) | ||
| SF6 LCI mean (SD) | 5.99 (0.36) | 7.83 (1.56) | 1.84 (1.12; 2.55) | <0.001 |
| N2 LCI mean (SD) | 7.05 (0.39) | 9.38 (1.61) | 2.33 (1.58; 3.08) | <0.001 |
The Vd/weight and Vd/Vt were both much greater on the N2 MBW system, but did not differ between health and CF (Table 2). There were minor differences in the Vt, respiratory rate, and minute ventilation with increasing Vd, but average breathing pattern was unaffected.
When healthy preschool N2 LCI data were scaled to the Vd/Vt each subject experienced for on the SF6 MBW, the observed mean difference in LCI was reduced to 0.68 (95% CI 0.36; 1.01 ). When healthy preschool N2 LCI data were scaled to the common reference point (Vd/Vt = 0.1), the mean difference in LCI was similar 0.84 (95%CI 0.51; 1.12) (Supplementary Figure S2).
DISCUSSION
Equipment Vd has an impact on LCI values when the Vd is large relative to the size of the subjects lung volumes. These results have important implications for longitudinal studies involving children, as a reduction of LCI with age, previously attributed solely to an improvement in ventilation homogeneity(13), may be in part due to lung growth. In young children increased equipment Vd increased the length of the washout requiring more breaths to clear the tracer gas. Until equipment Vd can be reduced or eliminated, correcting LCI values using an equation derived from controlled experiments in adults provides an interim solution to interpret longitudinal LCI measurements in young children.
The effects of increased Vd on LCI measurements have previously been reported in animal(11) and infant studies(12). Schulzke et al., suggest that only the functional Vd, the portion of Vd through which the breath travels, affects LCI measurement (12). In the adult experiments, we tried to minimize turbulent flow, but could not distinguish between functional and total Vd. In addition the “common dead space effect” also makes it difficult to accurately correct for external Vd volumes. At the end of an expiration, gas in the trachea and external Vd represent the gas composition in the slowest ventilated lung units. In the subsequent inspiration this gas will be distributed preferentially to the best ventilated regions. The “common dead space effect” thus results in slowing the clearance of the better ventilated units and speeding that of the slower. In the individual case, the effect of an imposed external Vd therefore cannot be predicted with high accuracy. In preschool children where a facemask is typically used during testing, the distinction between functional and total Vd is even more difficult to define. In accordance with current standards we chose to correct for known Vd and did not correct for the Vd of the mask, as this volume is unknown and will vary both between and within a given individual.
We previously described differences between N2 and SF6 LCI and offered as possible explanations the physiological difference between the gases, the potential incomplete equilibration of exogenous tracer gas in the wash in phase of SF6 MBW and the possible contribution of tissue nitrogen (5). The current study would suggest Vd also contributes to the observed differences between the two systems. The differences between the systems are more pronounced in disease, therefore factors such as inadequate mixing of inhaled tracer gas and tissue nitrogen are likely important in explaining the observed differences. Other factors such as differences in the software used for both systems could also contribute to the differences between the two systems.
Initial MBW studies had assumed that LCI was independent of age (2, 3, 14); however, more recent data have challenged this concept, showing an inverse relationship between LCI and height in early childhood(13) The reasons for the observed pattern in young children have been difficult to explain as infants are measured sedated in a supine position, while older children and adults are measured awake in the seated position. Based on our observations, the effect of relative equipment Vd likely also contributes to higher LCI observed in younger children. The ideal solution is for the equipment Vd to be zero, or as close to zero as possible. We did not observe a specific threshold for Vd, rather even the current standard 2ml/kg cut off may be too high, particularly when young patients are included in studies. Until it is possible to eliminate, or further minimize the Vd of the N2 MBW system, the correction factor proposed in this study may be necessary to interpret LCI correctly, particularly in longitudinal studies that track the progression of lung disease in young children.
This is the first study to systematically evaluate the effects of equipment Vd on MBW measurements as it pertains to preschool children. The correction equation was derived in a healthy adult population and may not be appropriate for preschool children, and/or children with CF, however it provides a practical solution to interpretation of measurements until the equipment can be modified to further eliminate Vd or Vd correction can be further explored in preschool children. Ideally, the described experiments should be repeated in preschool children, but the limited attention span of preschool children would limit the feasibility to perform these experiments in this age group. In addition the current study also does not account for Vd of the facemask used as an interface in preschool MBW testing. Although every effort was made to minimize Vd in the mask by using putty, it was not possible to accurately measure the functional Vd within the mask for each individual. Minimizing dead space including using mouth pieces rather than masks may be a suitable alternative strategy in some age groups. Furthermore, size adjusted Vt targets were used in all N2 MBW measurements in adults, as per current consensus guidelines (4), which may have impacted our interpretation of the Vt results. Finally, we did focus on LCI as the most commonly used MBW outcome; whether the same findings apply for other MBW outcomes was not addressed in the current study.
In summary, in young children where equipment Vd is large relative to lung volumes, the increased Vd likely affect LCI measurements and thus likely impact the interpretation of repeated measurements in young children. In addition, equipment Vd explained some of the observed differences between LCI measured using SF6 MBW and N2 MBW. While this study provides proof of principle that adjustments for dead space may be feasible, further evidence is needed to determine whether adjusting for equipment Vd increases the accuracy of ventilation inhomogeneity assessment in longitudinal studies.
Supplementary Material
Acknowledgments
We would like to thank the families, children and adults who volunteered to participate in our study and the CF Clinical Research Team at the Hospital for Sick Children. This study was funded by the Sellers Chair of Cystic Fibrosis, NHLBI (1R01HL116232-01) and the Lyn and Arnold Irwin Foundation.
Abbreviations
- CF
Cystic fibrosis
- CI
95 percent confidence interval
- %CV
Percent coefficient of variation
- FRC
Functional Residual Capacity
- LCI
Lung clearance index at 1/40th of starting concentration
- MBW
Multiple breath inert gas washout
- N2
Nitrogen
- SD
Standard deviation
- SF6
Sulphur hexafluoride
- Vd
Dead space volume
- Vt
Tidal volume
Footnotes
Summary at a Glance
In this study we demonstrate that equipment dead space affects multiple breath washout measurements. Equipment dead space affects measurements especially in children when dead space is large relative to the lung volumes. We propose a correction equation that can be used to track longitudinal measurements.
REFERENCES
- 1.Kraemer R, Blum A, Schibler A, Ammann RA, Gallati S. Ventilation inhomogeneities in relation to standard lung function in patients with cystic fibrosis. Am J Respir Crit Care Med. 2005 Feb 15;171(4):371–378. doi: 10.1164/rccm.200407-948OC. [DOI] [PubMed] [Google Scholar]
- 2.Aurora P, Bush A, Gustafsson P, Oliver C, Wallis C, Price J, Stroobant J, Carr S, Stocks J London Cystic Fibrosis C. Multiple-breath washout as a marker of lung disease in preschool children with cystic fibrosis. American journal of respiratory and critical care medicine. 2005;171:249–256. doi: 10.1164/rccm.200407-895OC. [DOI] [PubMed] [Google Scholar]
- 3.Gustafsson PM, Aurora P, Lindblad A. Evaluation of ventilation maldistribution as an early indicator of lung disease in children with cystic fibrosis. Eur Respir J. 2003;22:972–979. doi: 10.1183/09031936.03.00049502. [DOI] [PubMed] [Google Scholar]
- 4.Robinson PD, Latzin P, Verbanck S, Hall GL, Horsley A, Gappa M, Thamrin C, Arets HG, Aurora P, Fuchs SI, King GG, Lum S, Macleod K, Paiva M, Pillow JJ, Ranganathan S, Ratjen F, Singer F, Sonnappa S, Stocks J, Subbarao P, Thompson BR, Gustafsson PM. Consensus statement for inert gas washout measurement using multiple- and single- breath tests. The European respiratory journal. 2013;41:507–522. doi: 10.1183/09031936.00069712. [DOI] [PubMed] [Google Scholar]
- 5.Jensen R, Stanojevic S, Gibney K, Salazar JG, Gustafsson P, Subbarao P, Ratjen F. Multiple breath nitrogen washout: a feasible alternative to mass spectrometry. PloS one. 2013;8:e56868. doi: 10.1371/journal.pone.0056868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fowler WS. Lung Function Studies. II. The Respiratory Dead Space. American Journal of Physiology -- Legacy Content. 1948;154:405–416. doi: 10.1152/ajplegacy.1948.154.3.405. [DOI] [PubMed] [Google Scholar]
- 7.Frey U, Stocks J, Coates A, Sly P, Bates J. Specifications for equipment used for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/ American Thoracic Society. The European respiratory journal. 2000;16:731–740. doi: 10.1034/j.1399-3003.2000.16d28.x. [DOI] [PubMed] [Google Scholar]
- 8.Gustafsson PM. Inert gas washout in preschool children. Paediatric respiratory reviews. 2005;6:239–245. doi: 10.1016/j.prrv.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Beydon N, Davis SD, Lombardi E, Allen JL, Arets HG, Aurora P, Bisgaard H, Davis GM, Ducharme FM, Eigen H, Gappa M, Gaultier C, Gustafsson PM, Hall GL, Hantos Z, Healy MJ, Jones MH, Klug B, Lodrup Carlsen KC, McKenzie SA, Marchal F, Mayer OH, Merkus PJ, Morris MG, Oostveen E, Pillow JJ, Seddon PC, Silverman M, Sly PD, Stocks J, Tepper RS, Vilozni D, Wilson NM. American Thoracic Society/European Respiratory Society Working Group on I, Young Children Pulmonary Function T. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. American journal of respiratory and critical care medicine. 2007;175:1304–1345. doi: 10.1164/rccm.200605-642ST. [DOI] [PubMed] [Google Scholar]
- 10.Arborelius M, Rosberg HE, Wiberg R. Multiple breath nitrogen dead space. Clinical physiology. 1988;8:561–576. doi: 10.1111/j.1475-097x.1988.tb00221.x. [DOI] [PubMed] [Google Scholar]
- 11.Schmalisch G, Proquitte H, Roehr CC, Wauer RR. The effect of changing ventilator settings on indices of ventilation inhomogeneity in small ventilated lungs. BMC pulmonary medicine. 2006;6:20. doi: 10.1186/1471-2466-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schulzke SM, Deeptha K, Sinhal S, Baldwin DN, Pillow JJ. Nasal versus face mask for multiple-breath washout technique in preterm infants. Pediatric pulmonology. 2008;43:858–865. doi: 10.1002/ppul.20862. [DOI] [PubMed] [Google Scholar]
- 13.Lum S, Stocks J, Stanojevic S, Wade A, Robinson P, Gustafsson P, Brown M, Aurora P, Subbarao P, Hoo AF, Sonnappa S. Age and height dependence of lung clearance index and functional residual capacity. The European respiratory journal. 2013;41:1371–1377. doi: 10.1183/09031936.00005512. [DOI] [PubMed] [Google Scholar]
- 14.Aurora P, Stocks J, Oliver C, Saunders C, Castle R, Chaziparasidis G, Bush A London Cystic Fibrosis C. Quality control for spirometry in preschool children with and without lung disease. American journal of respiratory and critical care medicine. 2004;169:1152–1159. doi: 10.1164/rccm.200310-1453OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.