Abstract
Aims
To compare prevalences of self-reported temporomandibular joint and muscle disorders (TM]MD)-type pain in the 2001 US National Health Interview Survey (NHIS) by age and gender for non-Hispmric whites (Caucasians) and non-Hispanic blacks (African Americans).
Methods
Data from the 2002 NHIS included information on gender, age, race, ethnicity, education, and TMJMD-type pain. Rao-Scott survey chi-square and survey logistic regression analyses using sampling weights and accounting for the complex design were used to analyze variables relating to prevalences.
Results
A total of 30,978 people, 17,498 females and 13,480 males, 20,389 non-Hispanic whites and 4,179 non-Hispanic blacks, were included. The overall prevalence of TMJMD-type pain was 4.6%, with 6.3% for women and 1.8% for men. However, based on age, a significant but modest racial/ethnic difference emerged after adjusting for socioeconomic status. For non-Hispanic white women up to age 50, the prevalence was ~7% to 8%, but it decreased after age 55. Non-Hispanic black women had much lower prevalence at younger ages (~4% at 25 to 34 years), which increased thereafter up to 55 to 64 years of age. A similar racial pattern seemed to emerge for non-Hispanic black men, with the lowest prevalence at ages 25 to 34 years, while non-Hispanic white men had higher prevalences. Overall, however, age seemed to play more of a role in women than men.
Conclusion
This is the first report of findings from a nationally representative US sample for TMJMD-type pain by age and race/ethnicity TMJMD-type-pain differed significantly by race, age, and gender after adjusting for socioeconomic status.
Keywords: age, gender, health disparity, prevalence, race/ethnicity, self-report, temporomandibular joint disorders
Introduction
Temporomandibular joint and muscle disorders (TMJMDs) are a heterogeneous group of conditions characterized by pain in the temporomandibular joint and/or masticatory muscles and limited or painful jaw movements; pain is the chief complaint in more than 97% of cases(1). Progress has been made in diagnostic classification/epidemiology(3-9), and management (10-11) of these conditions. TMJMD patients are predominantly women around reproductive age. (3,8,9) Most information regarding TMJMDs comes from clinical samples from North America and Western Europe.(1-9) Those reported are often more severe cases, with greater psychological involvement, (3,12,13) which perhaps leads to interpretations relevant mostly to individuals seeking care and to insured Caucasians. Less is known about these conditions in community populations of different racial or ethnic backgrounds. Although not adjusted for socioeconomic status (SES) or gender, a 1993 study based on the National Health Interview Survey (NHIS) in the US reported a slightly lower prevalence of jaw joint and facial (TMJMD-type) pain for African Americans compared to Caucasians(14); although diagnoses were not confirmed clinically, the NHIS used a reliable, valid question to assess TMJMD-type pain.(15-16) The authors’ studies of a biracial community cohort of young women have shown significant racial differences in TMJMDs – about double prevalence in non-Hispanic Caucasians versus non-Hispanic African Americans. (17-18) However, that cohort consisted of young women, so it is necessary to determine whether those TMJMD-type pain patterns exist in non-Hispanic white and non-Hispanic black adults of other ages and both genders. The aim of this investigation was to compare prevalences of self-reported TMJMD-type pain in the 2002 NHIS by age and gender for non-Hispanic whites (Caucasians) and non-Hispanic blacks (African Americans). This is the first report of findings from a nationally representative US sample for TMJMD-type pain by age and race/ethnicity.
Materials and Methods
Data Source
The NHIS, which is 1 of the major data collection systems of the National Center for Health Statistics, Centers for Disease Control and Prevention, assesses many health conditions.(19) The NHIS uses a stratified multistage probability design. The NHIS was redesigned in 1995. The new design included increasing the number of primary sampling units from 198 in 1994 to 358 in 1995, with a more complicated nonresponse adjustment based on household screening and oversampling of black and Hispanic persons for more precise estimates of these groups.(19) In this investigation, 2 racial/ethnic groups in the 2002 NHIS were included: non-Hispanic whites and non-Hispanic blacks. The NHIS provides current estimates of health and disability status, health-related behaviors, and healthcare utilization. Basic health and demographic information, including SES and education, were collected on all household members. Household variables included type of living quarters, number of families in household, and geographic region. Person variables included gender, age, race, ethnicity, and education. Additional information was collected on 1 randomly selected adult (age 18 years or over) and 1 randomly selected child (age 0 to 17 years) per family. TMJMD-type Pain Instrument Adult NHIS participants were asked the following validated question(15) for TMJMD: “During the past 3 months, did you have facial ache or pain in the jaw muscles or the joint in front of the ear?” This validated question has been used extensively in TMJMD research. (1,15-18,20,21) Persons responding “yes” or “no” to this question were included in these analyses; missing and “don’t know” responses were excluded. Thus, this question assessed the 3-month period prevalence of self-reported TMJMD-type pain.
Statistical Analyses
Prevalences and 95% confidence intervals (CIs) were estimated with SUDAAN software (Research Triangle Institute, Research Triangle Park, NC) using sampling weights and accounting for the complex design. Survey χ2 tests compared gender and age-specific prevalences between racial/ethnic groups. Analyses that included only non-Hispanic whites or blacks who answered the TMJMD-type pain question used proper sampling weights for this subdomain. Sample survey logistic regression accounting for the sampling weights and design with SUDAAN assessed prevalences of TMJMD-like pain as a function of combining age, gender, and race/ethnicity after adjusting for SES in the form of education. Gender x age x race/ethnicity and age X race/ethnicity interactions assessed possible effect modification of the relationship between race/ethnicity and prevalence by age (ie, if racial/ethnic effects differ by age). P<0.05 was considered statistically significant.
Results
The 2002 NHIS consisted of a total of 30,978 people: 17,498 females and 13,480 males. Table 1 presents the demographic characteristics of this sample based on age, gender, and race/ethnicity. The racial/ethnic composition of the cohort was 20,389 non-Hispanic whites and 4,179 non-Hispanic blacks. The first age cohort was 18 to 24 years; adults were thereafter grouped in 10-year increments (eg, 25 to 34 years) to allow comparison of these findings with other studies.
TABLE 1.
Selected Demographic Characteristics of the Sample: 2002 National Health Interview Survey (N=30,978)
| VARIABLE | Sample Size | Percent | SE |
|---|---|---|---|
| GENDER | |||
| Male | 13,480 | 48.0 | 0.37 |
| Female | 17,498 | 52.0 | 0.37 |
| RACE / ETHNICITY | |||
| Non-Hispanic White | 20,389 | 73.1 | 0.44 |
| Hispanic | 5268 | 11.0 | 0.27 |
| Non-Hispanic Black | 4179 | 11.4 | 0.33 |
| Non-Hispanic Other | 1142 | 4.4 | 0.19 |
| AGE (years) | |||
| 18 to 24 | 3358 | 13.3 | 0.34 |
| 25 to 34 | 5863 | 17.9 | 0.27 |
| 35 to 44 | 6482 | 21.4 | 0.28 |
| 45 to 54 | 5472 | 18.9 | 0.29 |
| 55 to 64 | 3967 | 12.5 | 0.22 |
| 65 to 74 | 2957 | 8.6 | 0.20 |
| 75+ | 2879 | 7.4 | 0.19 |
SE = standard error
Three-month point prevalences of TMJMD-type pain for the 2 racial/ethnic groups overall and by gender are shown in Table 2. The overall prevalence of TMJMD-type pain was 4.6%. Overall, women had significantly higher TMJMD-type pain prevalence (6.3%) than men (2.8%) (Rao-Scott survey chi-square P<0.001), with non-Hispanic white women having a slightly higher prevalence compared to non-Hispanic black women (6.7% in non-Hispanic whites versus 5.1% in non-Hispanic blacks; Rao-Scott survey chi-square P=0.014); prevalences were not very different in men with respect to race (3.0% in non-Hispanic whites versus 2.8% in non-Hispanic blacks; Rao-Scott survey chi-square P=0.775).
TABLE 2.
Prevalence of TMJMD-Type Pain among US Adults in2002, by Gender and Race/Ethnicity (N=24,568)
| RACE / ETHNICITY | FEMALES % SE |
MALES % SE |
TOTAL % SE |
|---|---|---|---|
| Non-Hispanic White | 6.7 0.29 | 3.0 0.21 | 4.9 0.19 |
| Non-Hispanic Black | 5.1 0.50 | 2.8 0.51 | 4.1 0.34 |
| Combined | 6.3 0.24 | 2.8 0.17 | 4.6 0.16 |
SE = standard error
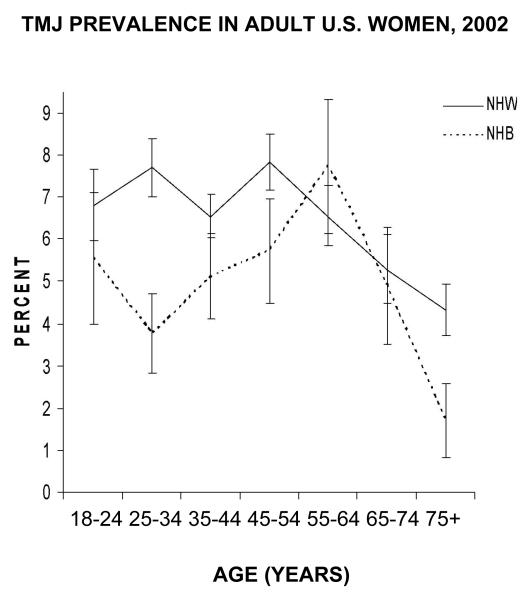
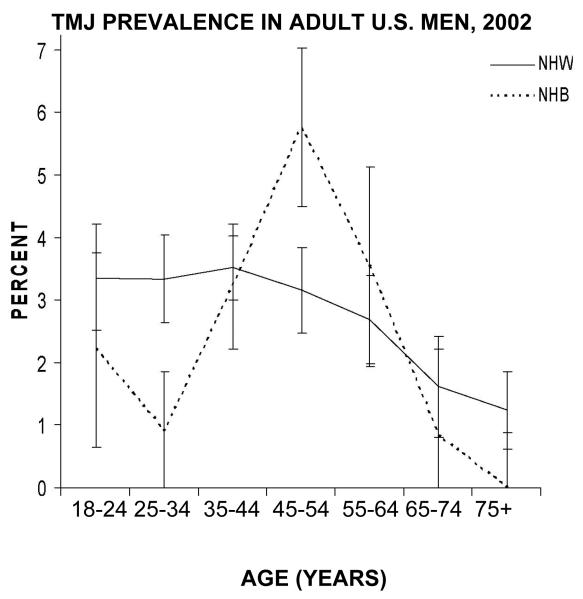
Figure 1 graphically displays prevalences of TMJMD-type pain in women by age group and race/ethnicity. Interestingly, racial/ethnic differences in prevalence depended on the age group. Up to age 50, the prevalence for non-Hispanic white females was about 7% to 8%; after age 55, the prevalence decreased. Non-Hispanic black women demonstrated a different pattern: much lower prevalence at younger ages (~4% at 25 to 34 years), but increasing prevalences thereafter up to 55 to 64 years of age. Thus, a racial difference in the age effect is apparent. The prevalence pattern for non-Hispanic white men was similar to that for women (although apparently lower), showing fewer changes by age (Fig 2).
Figure 1.
TMJMD-type pain prevalences with 95% confidence intervals based on age and race for US adult women. NHW=non-Hispanic white; NHB=non-Hispanic black
Figure 2.
TMJMD-type pain prevalences with 95% confidence intervals based on age and race for US adult men. NHW=non-Hispanic white; NHB=non-Hispanic black
A similar racial pattern seemed to emerge for non-Hispanic black males: the lowest prevalences were observed at age 25 to 34 years; prevalence increased until ages 45 to 54. Statistical analyses of the TMJMD-type pain prevalences based on age, gender, and race/ethnicity are presented in Table 3. In both females and males, statistically significant racial differences exist, mostly for 25- to 34-year olds and people 75+ years of age, with the non-Hispanic whites having higher prevalences compared to non-Hispanic blacks (See aORs, Table 3). Survey logistic regression models showed highly significant gender x race/ethnicity X age effects (P<0.001) associated with TMJMD-type pain; even adjusting for SES (education) did not reduce the significance of the 3-way interaction (P<0.001). All three 2-way interactions were also significant (P<0.001), but the race/ethnicity X age statistic was larger than the sex X age χ2. Overall, however, age seemed to play more of a role in women than men (Table 3).
TABLE 3.
Age-Specific TMJMD-Type Pain Prevalence Comparisons between Non-Hispanic Whites and Non-Hispanic Blacks adjusting for Education
| FEMALES | MALES | |||||
|---|---|---|---|---|---|---|
| AGE (YEARS) |
aOR | 95% CI | P-value | aOR | 95% CI | P-value |
| 18 – 24 | 1.16 | 0.62-2.16 | 0.636 | 1.55 | 0.43-5.57 | 0.504 |
| 25 – 34 | 1.97 | 1.14-3.38 | 0.015 | 3.67 | 1.26-10.7 | 0.017 |
| 35 – 44 | 1.21 | 0.79-1.86 | 0.372 | 1.10 | 0.53-2.26 | 0.796 |
| 45 – 54 | 1.50 | 0.91-2.48 | 0.112 | 0.56 | 0.29-1.10 | 0.094 |
| 55 – 64 | 0.85 | 0.52-1.39 | 0.511 | 0.98 | 0.29-3.37 | 0.974 |
| 65 – 74 | 1.16 | 0.60-2.23 | 0.657 | 2.97 | 0.41-21.6 | 0.282 |
| 75+ | 3.66 | 1.09-12.3 | 0.036 | --- | --- | --- |
aOR = adjusted odds ratio
Discussion
This is the first study to report on TMJMD-type pain, where age, gender, and race/ethnicity were investigated on a large representative sample of the general US population. Results showed that regardless of gender, at young adult ages there was a significant racial difference in TMJMD-type pain, with non-Hispanic whites having moderately higher prevalences than non-Hispanic blacks, after adjusting for SES (education). Thus, these results confirmed the previous finding of racial differences of young women.(17) Surprisingly, however, this racial difference varied with age, with increased prevalences in non-Hispanic blacks at older ages (eg, 55 to 64 years versus 25 to 34 years).
This type of study has several limitations. First, these data were obtained from a cross-sectional study from self-reports based on questionnaires, not based on clinical examination; thus, information about clinical sub-types of TMJMDs was not available. However, this self-report has been found to be reliable and valid (sensitivity of 96% to 98% and specificity of 83% to 90%) in adolescents, (15) and a similar self-report item has been found reliable and valid (sensitivity of 100% and specificity of 80%) in middle-aged adults.(16) TMJMDs are a group of heterogeneous conditions for which persistent or recurrent pain of the joint and/or jaw muscles is the chief complaint (97% of TMJMD cases) with pain being the main reason for seeking treatment. (1) Therefore, non-pain cases such as nonpainful internal joint derangements and other nonpainful joint problems (~3% of TMJMD cases) would likely be missed in this format. Second, the instrument is designed to assess 3-month period prevalence, not lifetime prevalence. The present estimations are thus lower than lifetime or 6-month period prevalence due to the episodic nature of TMJMD pain.(1) Third, recall bias or unwillingness to report pain is an inherent drawback of this survey. Thus, these results might underestimate the real prevalence of these conditions, which would explain the somewhat lower values compared to those previously reported in Caucasians. However, only a cross-sectional approach to studying the effect of age was possible, instead of a longitudinal one, which is subject to possible cohort or secular effects.
However, the advantages of the data far outweigh the limitations. The NHIS is a nationally representative sample of US noninstitutionalized adults with an over-representation of minority groups. Most published epidemiologic TMJMD data from North America are from mostly white insured populations.(3-9) Less is known about other US racial/ethnic groups. Slightly lower prevale9nce of joint and facial pain for African Americans compared to Caucasians was previously reported using NHIS data. However, that report was based on the previous NHIS design, which did not oversample non-Hispanic blacks and had insufficient sample size to compare racial/ethnic groups adjusted for age. (14) The authors’ previous studies (17,21) of a biracial community sample of young women showed that 6-month period and lifetime prevalences of TMJMD-type pain were about twice as high for non-Hispanic whites compared to non-Hispanic blacks (6-month: 13% versus 6%; lifetime: 22% versus 12%, respectively). Non-Hispanic whites also had significantly higher incidence and persistence. These NHIS data confirmed a similar 2:1 ratio of racial prevalence in 25- to 34-year-old non-Hispanic white women (~8%) compared to 25- to 34-year-old non-Hispanic black women (~4%), although 3-month period prevalences were lower than 6-month period prevalences, as expected.
Large differences in prevalence have been reported among different epidemiologic studies. (8,9) The causes for these study-to-study differences were considered to be due to methodological differences, such as lack of standardized questionnaires and sample differences rather than the true population differences. For example, studies using questionnaires based on TMJMD signs and symptoms yielded much higher prevalences compared to studies using questionnaires regarding only pain experience. Furthermore, even for studies based on pain, large differences were found based on the time frame of the questionnaire items. Dworkin and LeResche(22) reported the effect of the time interval on the prevalence of TMJMD pain in a Caucasian population to range from 3.6% for point prevalence (current pain) to 12% for 6-month period prevalence to 34% for lifetime prevalence.
Based on a review of 6 adult white population based studies, the prevalence of self-reported pain in the temporomandibular region ranged from 8% to 15% for women and from 3% to 10% for men, with female-to-male ratios between 1.4 and 2.6 (ie, more common in women than men). (9) Similar gender ratios were found regardless of race (2.2 in non-Hispanic whites and 1.8 in non-Hispanic blacks). Thus, the NHIS data support previous reports on white populations.
However, most studies on Caucasian populations have reported different age-specific patterns of TMJMD pain prevalence. They were described either as a bell-shaped distribution, with greatest prevalence around reproductive ages and declining with age,(4-8) or not changing much with age. (23) The variability in these results is mostly explained by sample differences. Age- and gender-specific prevalences generally are considered to require relatively large samples of more than 1,000 subjects to provide meaningful estimates! The NHIS sample, at least for non-Hispanic whites, met this criterion. However, the non-Hispanic white adult women presented much less of a bell-shaped curve, showing from 18 to 24 until 55 to 60 years old a much less age variation, and a decline thereafter. The bell-shaped distribution (eg, peak prevalence around reproductive ages) findings come from either less representative population samples (4) or clinical samples of treatment-seeking women. (8-9) Perhaps the peak prevalence (12%) around reproductive ages is mostly explained by an age difference in the level of perceived pain and thus treatment-seeking behavior rather than a real pain prevalence. The increasing prevalence portion may be from puberty to adulthood, which was not an age group in this report. Around reproductive ages the severity of TMJMD pain may increase, increasing the treatment seeking, thus explaining this peak prevalence found in mostly insured whites.
However, the most interesting clinical and research finding of this study is the racial difference in the age pattern, which confirms our previous reports on young women.(17) Since our impetus for analyzing NHIS data was to use national data to externally validate overall and racial findings in 18- to 24-year-old female National Growth and Health Study (NGHS) participants, the first NHIS age category was selected to correspond to that group and 10-year ranges for subsequent age categories. However, the authors’ previous report using wider age ranges (18 to 24, 25 to 44, 45 to 64, 65+) showed similar results (24) – a sensitivity analysis of choice of age cutoffs. Therefore, not only was it confirmed that the significant racial difference in young adult women also extended to young men, but we also found that the lower prevalence of TMJMD-type pain in young non-Hispanic black women and men appears to increase with age. This finding is important not only for identifying that middle-aged non-Hispanic blacks may well experience a disparity in TMJMD treatment, but also may shed light on the mechanism and natural history of this type of pain, which presently is not well understood. TMJMD-type pain often co-exists with other chronic pain conditions in other areas of the body, (18,25) and pain persistence and incidence are highly related to other pains in the body.(21) A recent report on 6,000 older (50- to 60-year-old) Swedes showed a high (12. 7%) prevalence of pain in the temporomandibular joint region to be associated with other health-related factors and dissatisfaction with health. (23) Also a recent study investigating TMJMD pain in arthritis, osteoarthrosis, and fibromyalgia patients supported the view of jaw pain as a marker for general pain increase and symptom sensitivity.(26) Taken together, increased pain prevalence with age may be related to an increase in other comorbid painful conditions, and dissatisfaction with health; this may impact 1 race more than another. It has been reported previously that non-Hispanic black females present more generalized body pain than non-Hispanic white females. (18) Reports on racial health disparities show non-Hispanic black females tend to have worse health for many conditions than non-Hispanic black males; this increases with age, adjusting for SES.(27) Since little is known about the natural history of this type of pain, its risk factors and how this pain may affect different racial/ethnic groups, further explorations into this area are necessary. An upcoming study combining multiple years of NHIS data to increase sample size of African Americans will enable the examination of the roles of age, race, and health along with other factors to shed more light on these issues.
Acknowledgments
An earlier version of this research was presented at the 84th General Session of the lnternational Association for Dental Research, Brisbane, Australia July 1, 2006. Supported by US DHHS NIH/NIDCR & NCMHD U54 DE 014251. Dr Isong led the data analyses and manuscript preparation before she passed away suddenly in 2007. We dedicate this paper to her memory; she continues to inspire us to work toward making the world a better place.
Contributor Information
Umo Isong, Center to Address Disparities in Children’s Oral Health University of California, San Francisco San Francisco, California.
Stuart A. Gansky, Center to Address Disparities in Children· s Oral Health University of California, San Francisco San Francisco, California.
Octavia Plesh, Department of Preventive and Restorative Dental Sciences University of California, San Francisco San Francisco, California.
References
- 1.Dworkin SF, Huggins KH, LeResche L. Epidemiology of signs and symptoms in temporomandibular disorders: Clinical signs in cases and controls. J Am Dent Assoc. 1990;120:273–281. doi: 10.14219/jada.archive.1990.0043. [DOI] [PubMed] [Google Scholar]
- 2.Dworkin SF, LeResche L, editors. Research Diagnostic Criteria for Temporomandibular Disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 3.LeResche L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiological factors. Crit Rev Oral Bioi Med. 1997;8:291–305. doi: 10.1177/10454411970080030401. [DOI] [PubMed] [Google Scholar]
- 4.Goulet J-P, Levigne GJ, Lund JP. Jaw pain prevalence among French-speaking Canadians in Quebec and related symptoms of temporomandibular disorders. J Dent Res. 1995;74:1738–1744. doi: 10.1177/00220345950740110401. [DOI] [PubMed] [Google Scholar]
- 5.List T, Dworkin SF. Comparing TMD diagnoses and clinical findings at Swedish and US TMD Centers using research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 1996;10:240–253. [PubMed] [Google Scholar]
- 6.Wanman A. Longitudinal course of symptoms of craniamandibular disorders in men and women. A 10-year follow-up study of an epidemiological sample. Acta Odontol Seand. 1996;54:337–342. doi: 10.3109/00016359609003548. [DOI] [PubMed] [Google Scholar]
- 7.Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiological study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. 2000;14:310–319. [PubMed] [Google Scholar]
- 8.Drangsholt M, LeResche L. Temporomandibular disorder pain. In: Crombie I, Croft PR, Linton SJ, editors. Epidemiology of Pain. IASP Press; Seattle: 1999. pp. 203–233. [Google Scholar]
- 9.LeResche L. Epidemiology of orofacial pain. In: Lund JP, Levigne GJ, Dohner R, Sessle BJ, editors. Orofacial Pain: From Basic Science to Clinical Management. Quintessence; Chicago: 2001. pp. 15–25. [Google Scholar]
- 10.Dworkin SF, Huggins KH, Wilson L, et al. A randomized clinical trial using Research Criteria for Temporomandibular Disorders-Axis ll to target clinical cases for a tailored self-care treatment program. J Orofac Pain. 2001;16:48–63. [PubMed] [Google Scholar]
- 11.Dworkin SF, Turner JA, Mancl L, et al. A randomized clinical trial of a tailored comprehensive care treatment program for temporomandibular disorders. J Orofac Pain. 2002;16:256–276. [PubMed] [Google Scholar]
- 12.Epker J, Gatchel RJ. Coping profile differences in the biopsychosocial functioning of patients with temporomandibular disorders. Psychosom Med. 2000;62:69–75. doi: 10.1097/00006842-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Dworkin SF. Psychological and psychosocial assessment. In: Laskin DM, Greene CS, Hylander WL, editors. TMDs, An Evidence-Based Approach to Diagnosis and Treatment. Quintessence; Chicago’: 2006. pp. 203–217. [Google Scholar]
- 14.Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993;124:115–124. doi: 10.14219/jada.archive.1993.0200. [DOI] [PubMed] [Google Scholar]
- 15.Nilsson 1M, List T, Drangsholt M. The reliability and validity of self-reported temporomandibular disorder pain in adolescents. J Orofacial Pain. 2006;20:138–144. [PubMed] [Google Scholar]
- 16.Pinelli C, de Castro Monteiro Loffredo L. Reproducibility and validity of self-perceived oral health condition. Clin Oral lnvestig. 2007;11:431–437. doi: 10.1007/s00784-007-0133-0. [DOI] [PubMed] [Google Scholar]
- 17.Plesh O, Crawford PB, Gansky SA. Chronic pain in a biracial population of young women. Pain. 2002;99:515–523. doi: 10.1016/S0304-3959(02)00262-2. [DOI] [PubMed] [Google Scholar]
- 18.Gansky SA, Plesh O. Widespread pain and fibromyalgia in a biracial cohort stndy of young women. J Rheumatol. 2007;34:810–817. [PubMed] [Google Scholar]
- 19.The Centers for Disease Control and Prevention 2002 NHIS data document http://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentarion/NHIS/2002/srvydesc.pdf.
- 20.von Korff M, Dworkin SF, LeResche L. An epidemiological comparison of pain complaints. Pain. 1988;32:173–183. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- 21.Gansky SA, Plesh O. Chronic Pain in a biracial cohort study: Up to 5-years of follow-up [submitted]
- 22.Dworkin SF, LeResche L. Temporomandibular disorder pain: epidemiological data. APS Bulletin. 1993 Aprilmay;:12–13. [Google Scholar]
- 23.Johansson A, Unell L, Carlsson GE, Soderfeldt B, Halling A. Risk factors associated with symptoms of temporomandibular disorders in a population of 50- and 60-yearold subjects. J Oral Rebab. 2006;33:47.3481. doi: 10.1111/j.1365-2842.2005.01574.x. [DOI] [PubMed] [Google Scholar]
- 24.Isong U, Gansky SA, Plesh O. Facial pain in US adults: The National Health Interview Survey. J Dent Res. 2006;85(Spec Iss 8):2589. [PMC free article] [PubMed] [Google Scholar]
- 25.Turp JC, Kowalsky CJ, O’Leary N, Stohler CS. Pain maps from facial pain patients indicate a broad pain geography. J Dent Res. 1998;77:1465–1472. doi: 10.1177/00220345980770061101. [DOI] [PubMed] [Google Scholar]
- 26.Wolfe F, Katz RS, Michaud K. jaw pain: Its prevalence and meaning in patients with rheumatoid arthritis, osteoarthritis, and fibromyalgia. J Rheumatol. 2005;32:2421–2428. [PubMed] [Google Scholar]
- 27.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostaric load scores among blacks and whites in the United States. Am J Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]