No licensed malaria vaccine currently exists; however, final phase 3 testing results of a leading candidate vaccine are forthcoming. Continued challenges to malaria vaccine developers include genetically diverse strains found in nature and establishment of a vaccine correlate of protection.
Keywords: malaria, vaccine, P. falciparum, P. vivax
Abstract
Despite global efforts to control malaria, the illness remains a significant public health threat. Currently, there is no licensed vaccine against malaria, but an efficacious vaccine would represent an important public health tool for successful malaria elimination. Malaria vaccine development continues to be hindered by a poor understanding of antimalarial immunity, a lack of an immune correlate of protection, and the genetic diversity of malaria parasites. Current vaccine development efforts largely target Plasmodium falciparum parasites in the pre-erythrocytic and erythrocytic stages, with some research on transmission-blocking vaccines against asexual stages and vaccines against pregnancy-associated malaria. The leading pre-erythrocytic vaccine candidate is RTS,S, and early results of ongoing Phase 3 testing show overall efficacy of 46% against clinical malaria. The next steps for malaria vaccine development will focus on the design of a product that is efficacious against the highly diverse strains of malaria and the identification of a correlate of protection against disease.
Malaria remains a significant public health threat, with approximately half of the world's population at risk of infection. The disease is caused by parasites transmitted to humans by the bite of an infected mosquito. Those residing in the poorest countries are particularly vulnerable to death from malaria illness, especially children aged < 5 years in sub-Saharan African [1]. From 2000 to 2012, malaria mortality rates dropped by 45%, due in part to expanded funding for malaria control interventions including long-lasting insecticidal nets, indoor residual spraying programs, and access to artemisinin combination therapy [1].
Currently, there is no licensed vaccine against malaria. A malaria vaccine would represent a public health tool that is viewed by some experts to be necessary for successful malaria elimination. The World Health Organization (WHO) recently published strategic goals to license malaria vaccines by 2030 that target Plasmodium falciparum and Plasmodium vivax, have at least 75% protective efficacy against clinical malaria, and that reduce transmission to enable elimination [2]. The most advanced candidate vaccine to date, RTS,S/AS01, is currently in phase 3 testing in 7 African countries; final results are expected by 2015. Efforts to improve on the modest efficacy of RTS,S/AS01 include more than 20 malaria vaccine strategies currently in clinical testing; these include the use of candidate antigens (Table 1) in monovalent and multivalent formulations either alone or with other agents, viral vectors, and/or vaccine adjuvants. Here, we review the history of malaria vaccine development, then explain the malaria life cycle as a backdrop to our description of the challenges, approaches, and focus of current malaria vaccine development efforts.
Table 1.
Current Malaria Vaccine Projects
| Target | Antigen | Antigen Description | Vaccine Mechanism | Most Advanced Status |
|---|---|---|---|---|
| Plasmodium falciparum pre-erythrocytic | RTS,S | Circumsporozoite protein fused to hepatitis B surface antigen | Inhibit sporozoite motility; prevent hepatocyte invasion | Phase 3 clinical testing |
| ChAd63/MVA, ME-TRAP | Chimpanzee adenovirus 63/modified vaccinia Ankara, multiple epitope string with thrombospondin-related adhesion protein | Inhibit sporozoite motility; prevent hepatocyte invasion | Phase 2 clinical testing | |
| PfSPZ | Radiation-attenuated whole organism P. falciparum sporozoites | Inhibit sporozoite motility; prevent hepatocyte invasion | Phase 1 clinical testing | |
| PfCelTOS | P. falciparum cell-traversal protein for ookinetes and sporozoites | Inhibit sporozoite motility; prevent hepatocyte invasion | Phase 1 clinical testing | |
| Recombinant CSP | Recombinant circumsporozoite protein | Inhibit sporozoite mobility; prevent hepatocyte invasion | Preclinical testing | |
| Genetically attenuated sporozoites | Genetically attenuated whole organism P. falciparum sporozoites | Inhibit sporozoite motility; prevent hepatocyte invasion | Preclinical testing | |
| P. falciparum erythrocytic | EBA 175 | Erythrocyte-binding antigen 175 | Target merozoite ligand that mediates erythrocyte invasion | Phase 1 clinical testing |
| AMA1 | Apical membrane antigen 1 | Target the merozoite's invasion apparatus to prevent erythrocyte infection | Phase 2 clinical testing | |
| GMZ2 | Recombinant Lactococcus lactis hybrid glutamate-rich protein and merozoite surface protein 3 | Target merozoite surface to inhibit erythrocyte invasion | Phase 2 clinical testing | |
| P27A | P. falciparum malaria protein PFF0165c | Target merozoite surface to inhibit erythrocyte invasion | Phase 1 clinical testing | |
| MSP3 | Malaria surface protein 3 | Target merozoite surface to inhibit erythrocyte invasion | Phase 2 clinical testing | |
| SE36 | P. falciparum serine repeat antigen 5 | Target merozoite surface to inhibit erythrocyte invasion | Phase 1 clinical testing | |
| PfPEBS | P. falciparum pre-erythrocytic and blood stage | Inhibit sporozoite motility; prevent hepatocyte invasion; target merozoite surface to inhibit erythrocyte invasion | Phase 1 clinical testing | |
| MSP1 | Malaria surface protein 1 | Target merozoite surface to inhibit erythrocyte invasion | Preclinical testing | |
| Rh5 | Reticulocyte-binding protein homologue 5 | Target merozoite ligand that mediates erythrocyte invasion | Preclinical testing | |
| P. falciparum transmission-blocking | Pfs25 | P. falciparum surface protein 25 | Inhibit ookinete development in the mosquito midgut | Phase 1 clinical testing |
| Pfs48 | P. falciparum surface protein 48 | Inhibit ookinete development in the mosquito midgut | Preclinical testing | |
| Pfs45 | P. falciparum surface protein 45 | Inhibit ookinete development in the mosquito midgut | Preclinical testing | |
| Pfs230 | P. falciparum surface protein 230 | Inhibit ookinete development in the mosquito midgut | Preclinical testing | |
| P. falciparum Pregnancy-associated malaria | var2 CSA | Variant 2 chondroitin sulfate A | Inhibit parasite ligand that binds to placental matrix | Preclinical testing |
| P. vivax pre-erythrocytic | CSP | Circumsporozoite protein | Inhibit sporozoite motility; prevent hepatocyte invasion | Preclinical testing |
| P. vivax erythrocytic | PvDBP | P. vivax duffy-binding protein | Inhibit parasite ligand that binds to placental matrix | Phase 1 clinical testing |
Data source: http://www.who.int/vaccine_research/links/Rainbow/en/index.html last updated 7 July 2014; and [3].
ADVANCES IN MALARIA VACCINE DEVELOPMENT
Early malaria vaccine research began in the 1930s with a focus on inactivated or killed parasites that failed to generate a protective immune response. The addition of adjuvant systems demonstrated immunogenicity of malaria vaccine candidates in animal models; Jules Freund and colleagues demonstrated partial protection in ducklings [4]. Subsequent vaccine development efforts used rodent malaria models. This led to the first human malaria vaccine trial with demonstrated efficacy, a study that delivered irradiated P. falciparum sporozoites to vaccinees by mosquito bite [5]. This breakthrough was regarded as impractical for mass vaccination campaigns, and synthetic peptide vaccines based on immunogenic parasite proteins began to be developed in the 1980s. As there is no biological correlate of protection for malaria, continued efforts in vaccine development were painstakingly time consuming. A series of steps needed to be taken before phase 2 field testing in the target population of children in malaria-endemic areas could finally be performed to determine vaccine efficacy. These steps included initial development of a candidate vaccine in the laboratory, testing for safety and proof-of-concept in animal models, and age de-escalation phase 1 testing in adults and then in children for safety and reactogenicity. These multiple steps represent an arduous process, require significant funding support due to the lengthy product development timeline, and carry the risk of a negative end result. To abrogate this risk, controlled human malaria infection (CHMI), where participants are inoculated with sporozoites via the bite of infected female Anopheles mosquitoes in well-controlled settings, was used to obtain data on vaccine and drug efficacy in order to support or refute further clinical testing in malaria-endemic areas [6]. Early testing of the RTS,S vaccine using CHMI not only predicted efficacy in field studies, it also helped to refine the choice of adjuvant and support reformulation to a lyophilized form [7].
The first malaria immunization trials to use experimental challenge by infected mosquitoes were conducted in the mid-1970s [5, 8]. Field trials in which efficacy against clinical malaria was measured were conducted in the 1990s with the SPf66 vaccine, a subunit vaccine developed in Columbia that contained sequences from 3 P. falciparum blood-stage antigens and the circumsporozoite protein (CSP). These studies showed a modest reduction of P. falciparum parasitemia in South America but no protection in Africa [9]. Advances such as parasite cultivation methods and sequencing of the P. falciparum genome have increased hope for the development of a malaria vaccine [10]. However, after more than 35 years of laboratory research and field trials, the only vaccine that has progressed to phase 3 testing is the RTS,S vaccine, which showed efficacy of 30% in newborns and 50% in children aged 5–17 months in interim analyses from the ongoing phase 3 trial [11]. This limited success has called into question the likelihood of having a highly efficacious malaria vaccine available within the next few years. However, with funding agencies, the private sector, and international organizations joining forces to contain or even eradicate malaria, strategies are being scaled up in order to control the disease burden. In addition to effective treatment of clinical malaria and use of insecticide-impregnated barriers, malaria vaccines could play an important role in this initiative. Malaria vaccines can be divided into the following 3 groups based on the parasite developmental stages: pre-erythrocytic vaccines, blood-stage vaccines, and “other” vaccines including transmission-blocking vaccines and vaccines against pregnancy-associated malaria.
THE MALARIA LIFE CYCLE
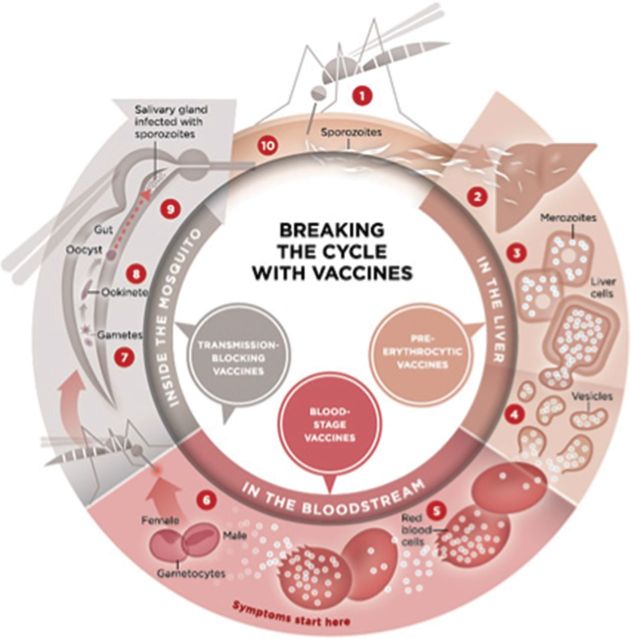
Malaria is caused by a unicellular eukaryotic parasite of the genus Plasmodium; 5 species including P. falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi cause human disease. Sporozoite-stage parasites are transmitted to humans by female Anopheline mosquitoes during a blood meal. These sporozoites invade hepatocytes and produce 30–40 000 progeny over a 6-day period. Those in the sporozoite and liver stages are collectively referred to as pre-erythrocytic parasites. When infected hepatocytes rupture and release progeny merozoites into the venous circulation, each merozoite will potentially invade a red blood cell and then propagate within 48–72 hours to produce 8–24 merozoites. When the infected erythrocyte ruptures, clinical symptoms present, including fever, headache, chills, and malaise. The severity of these symptoms has been correlated with parasite load [12]. Merozoites released during erythrocyte rupture will each potentially invade a new erythrocyte to continue the cycle, also known as the stage of erythrocyte parasite development. In the early stage of clinical manifestation, the fever attacks are periodic (24 hours for P. knowlesi; 48 hours for P. vivax, P. ovale, and P. falciparum; and 72 hours for P. malariae), corresponding with the release of a new generation of merozoites into the bloodstream (Figure 1).
Figure 1.
Life cycle of the malaria parasite. (1) Malaria infection begins when an infected female Anopheles mosquito bites a person, injecting Plasmodium parasites in the form of sporozoites, into the bloodstream. (2) The sporozoites pass quickly into the human liver. (3) The sporozoites multiply asexually in the liver cells over the next 7–10 days, causing no symptoms. (4) In an animal model, the parasites, in the form of merozoites, are released from the liver cells in vesicles, journey through the heart, and arrive in the lungs where they settle within lung capillaries. The vesicles eventually disintegrate, freeing the merozoites to enter the blood phase of their development. (5) In the bloodstream, the merozoites invade red blood cells (erythrocytes) and multiply again until the cells burst. Then they invade more erythrocytes. This cycle is repeated, causing fever each time parasites break free and invade blood cells. (6) Some of the infected blood cells leave the cycle of asexual multiplication. Instead of replicating, the merozoites in these cells develop into sexual forms of the parasite, called gametocytes, that circulate in the bloodstream. (7) When a mosquito bites an infected human, it ingests the gametocytes, which develop further into mature sex cells called gametes. (8) The fertilized female gametes develop into actively moving ookinetes that burrow through the mosquito's midgut wall and form oocysts on the exterior surface. (9) Inside the oocyst, thousands of active sporozoites develop. The oocyst eventually bursts, releasing sporozoites into the body cavity that travel to the mosquito's salivary glands. (10) The cycle of human infection begins again when the mosquito bites another person.
Source: PATH–Malaria Vaccine Initiative.
Factors that affect the severity of human malaria infection include host immune status and the general health and nutritional condition of the infected individual as well as the Plasmodium species [13]. Uncomplicated malaria is generally observed in adolescents and adults in high-transmission areas, whereas severe (complicated) malaria is seen in young children and primigravida and malaria-naive patients who travel to areas of malaria transmission. Severe and lethal malaria are primarily seen in infections due to P. falciparum. Other species are less commonly fatal. The ability of P. falciparum to produce high parasite loads, invade all stages of red blood cells, and sequester in end organ vasculature help to explain this extensive morbidity and mortality. Cytoadherence plays an important role in the pathogenesis of severe malaria due to P. falciparum [12] in that parasitized erythrocytes express surface cellular adhesion molecules that localize to end organs where pathologic effects manifest. Sequestration of infected red blood cells in the brain may result in cerebral malaria with convulsions, potentially followed by prostration, coma, and death. When sequestration occurs in the placenta during pregnancy, miscarriage or low birth weight may result.
IMMUNE RESPONSE TO MALARIA
Antimalarial immunity is poorly understood, and identification of an immune correlate of protection continues to elude malaria researchers, hindering vaccine development. In endemic areas, antimalarial immunity develops over a prolonged period but is incomplete. Even the most malaria-experienced persons remain susceptible to malaria infection (asymptomatic parasitemia) but not clinical illness. During infection, both humoral and cell-mediated immune responses initiate antibody production, cytokine release, regulatory and effector T-cell stimulation, and neutrophil and monocyte activation to control parasitemia [14–16]. This complex response does not permit results from a single immune assay to represent a threshold of protection, as is done for other vaccine-preventable illnesses.
PRE-ERYTHROCYTIC MALARIA VACCINES
An effective immune response must act quickly in order to thwart P. falciparum sporozoites in their minutes-long journey from the skin to the liver. Both humoral and T-cell responses are required to prevent hepatocyte invasion, which is the goal of pre-erythrocytic vaccines. Pre-erythrocytic vaccine targets include CSP that is expressed on the surface of sporozoites; the protein is composed of 412 amino acids [17] with 37 tetrapeptide repeats and a conserved central domain [18]. Anti-CSP antibodies inhibit sporozoite invasion in vitro, and anti-CSP monoclonal antibodies block experimental infection in animals [19].
RTS,S is the leading pre-erythrocytic malaria vaccine. It is comprised of hepatitis B surface antigen (HBsAg) particles fused to P. falciparum CSP central repeat and thrombospondin domains formulated in the adjuvant ASO1, a liposome formulation that contains immunostimulants 3-O-desacyl-4′-monophosphoryl lipid A and the saponin QS-21 from Quillaja saponaria extract. RTS,S is a recombinant antigen comprised of conserved sequences from the 3D7 standard laboratory strain of P. falciparum. It includes the “R” (repeat) portion, which is a single polypeptide chain that corresponds to a highly conserved tandem repeat tetrapeptide sequence from CSP (N-acetylneuraminic acid phosphatase [NANP] amino acid sequence repeats), and the “T” (T-cell epitope) portion, which includes T-lymphocyte epitopes separated by immunodominant CD4+ and CD8+ epitopes (Th2R and Th3R). This combined RT peptide is fused to the N-terminal of HBsAg, the “S” (surface) portion. A second “S” portion is an unfused HBsAg, hence, the name RTS,S.
In the first phase 3 clinical trial of a malaria vaccine, efficacy against clinical malaria in children during the 18 months following dose 3 was 46% overall, waned over time, was higher in older children than in infants, and showed the highest impact in areas with the greatest malaria prevalence [20]. This study is ongoing, with plans to submit the final phase 3 data in 2014/2015 to the European Medicines Agency and the WHO. Vaccine effectiveness models that simulate varying malaria transmission intensity and seasonality are being used to determine the epidemiological settings and age groups that would benefit most from RTS,S vaccination. In parallel, efforts to increase RTS,S efficacy are ongoing. These efforts include combining RTS,S with other antigens [21] and prime-boost strategies [22] where subsequent doses of vaccine antigen are delivered with a vector that is different from the initial vector in order to avoid immune recognition and senescence and to maximize response to the vaccine antigen. Continued challenges to the RTS,S vaccine developers include inducing a protective immune response to the genetically different strains found in nature and establishing a vaccine correlate of protection, obstacles considered central to all malaria vaccine development efforts. Field studies of RTS,S vaccine demonstrate mixed evidence of decreased malaria infections with vaccine-type CSP in vaccinees vs controls [23–25] and leave room for the rationale that RTS,S may provide protection against homologous strains with respect to key amino acid sequences, as has been shown with other malaria vaccine candidates [26]. However, difficulties in contiguous sequencing of the CSP protein through the central NANP repeat region limit the ability to test this hypothesis [27]. While anti-CSP antibody and CSP-specific CD4+ T-cell levels both increase after RTS,S vaccination, a threshold response that separates the protected from the unprotected cannot be defined, leaving refinements in vaccine formulation and adjuvant choice to be tested in CHMI studies or in field efficacy trials.
Other pre-erythrocytic vaccine strategies in development include the multiple epitope (ME) thrombospondin-related adhesion protein (TRAP) and whole-organism sporozoite strategies. ME-TRAP consists of fused B-cell and CD4 and CD8 T-cell epitopes of P. falciparum liver-stage antigens. This vaccine failed to show protection in phase 2b trials conducted in Kenya [28]; however, other variants are now under development [29]. In a return to the scientific principles that guided the first malaria vaccine trial showing efficacy in humans, researchers at the National Institutes of Health Vaccine Research Center demonstrated 100% efficacy against CHMI in 6 of 6 North American volunteers who received the highest dose of a whole-organism radiation-attenuated sporozoite vaccine [30]. Follow-up safety testing of this highly promising candidate vaccine is underway, including a trial in Malian adults to evaluate vaccine efficacy against diverse strains of naturally occurring malaria. Because this vaccine is currently administered intravenously, some malaria vaccine experts are skeptical that intravenous delivery is practical for mass administration, especially to infants and young children. Studies to test alternative routes of delivery are ongoing.
ERYTHROCYTIC MALARIA VACCINES
Clinical manifestations of malaria result from parasite blood-stage infection. Blood-stage vaccines are therefore intended to prevent disease and death without necessarily preventing infection. The gradual acquisition of natural protection against clinical disease following repeated infections in areas of malaria transmission indicates that a blood-stage malaria vaccine strategy is feasible, provided that it mimics acquired immunity to malaria in endemic areas. Immune protection during the erythrocytic stage is essentially mediated through neutralizing antibodies, as confirmed by studies of passive antibody transfer that protect against blood-stage infection [31, 32]. Antigens expressed on the surface of the merozoite and infected red blood cells are considered erythrocytic malaria vaccine candidates and include merozoite surface proteins 1, 2, and 3 (MSP1, MSP2, and MSP3); serine-repeat antigen; erythrocyte-binding antigen; ring-infected erythrocyte surface antigen (RESA); glutamate-rich protein (GLURP); and apical membrane antigen 1 (AMA1).
In malaria-endemic areas, protective immune responses are acquired over time following repeated infections by multiple alleles of multiple antigens of the malaria parasite. This suggests that the immune response may be specific to the genetic sequence of the infecting strain. Because of this specific immune response, an infecting parasite with a genetic sequence that is different from the vaccine antigen may result in malaria disease. In a field study in the Gambia, the protective effect of antibodies to genetically diverse regions of MSP3 was stronger than that of antibodies targeted to conserved regions [33]. Furthermore, a vaccine trial conducted in Papua New Guinea using combination B vaccine, a mixture of MSP1, MSP2, and RESA protein, showed an increased incidence of clinical infections with nonvaccine-type parasites with respect to MSP2 in vaccinated individuals compared with patients who received the control vaccine [34].
In recent years, only 4 blood-stage antigens (AMA1, MSP1, MSP3, and GLURP) have been tested in phase 2 vaccine trials. None of the vaccines based on the 4 antigens tested were efficacious based on the primary endpoint of clinical malaria. However, 1 AMA1-based vaccine tested in Mali demonstrated significant efficacy against clinical malaria infections that shared the identical genetic sequence with the vaccine strain with respect to key immunologically relevant amino acid positions [35]. The strain-specific efficacy and genetic diversity analyses of these malaria vaccine candidates demonstrate that in the likely event that there is too much diversity to be covered by a manageable number of allelic variants, specific amino acid residues and clusters of residues that are associated with immune protection against clinical disease can be identified, narrowing the diversity that must be considered in multivalent vaccine formulations. These analyses give insight into how current and potential vaccine candidate antigens can be designed to provide broad protection against diverse parasites.
TRANSMISSION-BLOCKING VACCINES
Recent increased interest in halting parasite spread to other persons has led to advances in transmission-blocking vaccines. These are sometimes called altruistic vaccines as there is no direct benefit to vaccinees. A successful transmission-blocking vaccine would induce neutralizing antibody responses against the malaria parasite's gametocyte and/or ookinete sexual stages, thereby blocking fertilization and halting reproduction [36]. Targeted antigens currently in early development include ookinete surface proteins P25 and P28, with phase 1 testing of P. falciparum and P. vivax P25 antigens completed [37, 38]. Efficacy testing of transmission-blocking vaccines can be measured by assays of Anopheles mosquito feeding directly on humans or on human blood via a membrane-feeding assay. Compared with control sera, plasma from participants immunized with a P25-based vaccine mixed with P. falciparum-infected blood reduced oocyte density of geographically distinct parasites in membrane-feeding assay testing [39]. The limited genetic polymorphism of the P25 encoding gene [40] may explain this cross-protective efficacy. A P25-based candidate vaccine is currently being evaluated in a phase 2 trial in Malian adults.
VACCINES AGAINST PREGNANCY-ASSOCIATED MALARIA
Pregnancy-associated malaria occurs when erythrocytes sequester to placental endothelial cells. Binding of infected erythrocytes to placental endothelium is mediated by the interaction between P. falciparum erythrocyte membrane protein 1 (PfEMP1), a ligand expressed on the surface of the infected erythrocyte, and receptors on the placental matrix, mainly, chondroitin sulfate antigen. This binding results in reduced placental blood supply and subsequent increased risk for both low-birth-weight babies and preterm delivery. The condition disproportionately affects primigravid women who have not yet developed an immune response to PfEMP1 proteins that presumably provide protection in subsequent pregnancies. Women with high anti-PfEMP1 antibody titers demonstrate reduced risk of delivering low-birth-weight babies than women with low antibody titers [41]. The durability of B-cell immunity generated to PfEMP1 antigens without reexposure lends promise to PfEMP1 as a vaccine candidate that targets females of prereproductive age with the aim to prevent pregnancy-associated malaria. The first PfEMP1-based vaccine is currently in preclinical development [42].
CONCLUSION
The renewed worldwide effort to eliminate malaria is underway, and experts agree that this goal cannot be achieved without new tools such as a malaria vaccine that can interrupt malaria transmission (VIMT) [43]. This concept of VIMT is described as any malaria vaccine that can impact transmission, including vaccines that target the sexual and oocyte stages, but also pre-erythrocytic and erythrocytic vaccines that reduce transmission. To show promise, candidate malaria vaccines must demonstrate reduced transmission of malaria as a result of vaccination, a new challenge for malaria vaccine clinical trial design.
What are the next steps for malaria vaccine development? A vaccine with at least 75% efficacy against clinical malaria, as outlined in the malaria vaccine technology road map [2], must be efficacious against the highly diverse strains of malaria that circulate in endemic areas. A multiantigen vaccine, similar to the approach used for vaccines against Streptococcus pneumoniae, may be necessary. Antigens selected for inclusion should also be highly immunogenic and provide immunity that lasts at least 2 years [2]. Alternatively, a highly efficacious, whole organism approach can potentially transcend strain-specific diversity constraints, and is currently being tested in malaria-endemic areas. Novel vaccine delivery systems and adjuvants that increase vaccine immunogenicity should continue to be developed and evaluated. Concurrent with the clinical trials that evaluate vaccine efficacy, studies of transmission reduction and cross-protection against endemic malaria that attempt to determine correlates of protection against malaria, especially vaccine-induced protection, should be performed. Research and development of a laboratory-based correlate using screening tools such as microarray-based methods would propel malaria vaccine development efforts and facilitate refinements in dosing and adjuvant formulation.
If scientific and donor interest in malaria vaccine development continues at or above current levels, the difficult task to develop a highly efficacious malaria vaccine is achievable. Modeling studies that take cost, malaria transmission, overall malaria burden of disease, and other relevant scientific evidence into account will help to determine where vaccine is deployed based on public health priorities at the local and national levels. Ongoing research and evaluation will help to overcome challenges of vaccine delivery and integrate insecticide-treated bed net use and other malaria control initiatives to reduce and eventually eliminate malaria burden.
Notes
Acknowledgments. We thank Dr Christopher V. Plowe for critical review of this manuscript.
Financial support. A. O. and M. B. L. are supported by grants from the US National Institutes of Health. In addition, M. B. L. is supported by the Howard Hughes Medical Institute.
Potential conflict of interest. Both authors: No reported conflicts.
Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.World Health Organization. Geneva, Switzerland: World Health Organization; World Malaria Report: 2013. [Google Scholar]
- 2.Malaria Vaccine Technology Roadmap. Malaria Vaccine Funders Group. World Health Organization. 2013. Available at: http://www.who.int/immunization/topics/malaria/vaccine_roadmap/en/
- 3.Schwartz L, Brown GV, Genton B, Moorthy VS. A review of malaria vaccine clinical projects based on the WHO rainbow table. Malar J. 2012;11:11. doi: 10.1186/1475-2875-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freund J, Thomson KJ, Sommer HE, Walter AW, Schenkein EL. Immunization of rhesus monkeys against malarial infection (P. knowlesi) with killed parasites and adjuvants. Science. 1945;102:202–4. doi: 10.1126/science.102.2643.202. [DOI] [PubMed] [Google Scholar]
- 5.Clyde DF, Most H, McCarthy VC, Vanderberg JP. Immunization of man against sporozite-induced falciparum malaria. Am J Med Sci. 1973;266:169–77. doi: 10.1097/00000441-197309000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Laurens MB, Roestenberg M, Moorthy VS. A consultation on the optimization of controlled human malaria infection by mosquito bite for evaluation of candidate malaria vaccines. Vaccine. 2012;30:5302–4. doi: 10.1016/j.vaccine.2012.04.088. [DOI] [PubMed] [Google Scholar]
- 7.Kester KE, Cummings JF, Ofori-Anyinam O, et al. Randomized, double-blind, phase 2a trial of falciparum malaria vaccines RTS,S/AS01B and RTS,S/AS02A in malaria-naive adults: safety, efficacy, and immunologic associates of protection. J Infect Dis. 2009;200:337–46. doi: 10.1086/600120. [DOI] [PubMed] [Google Scholar]
- 8.Clyde DF. Immunization of man against falciparum and vivax malaria by use of attenuated sporozoites. Am J Trop Med Hyg. 1975;24:397–401. doi: 10.4269/ajtmh.1975.24.397. [DOI] [PubMed] [Google Scholar]
- 9.Graves P, Gelband H. Vaccines for preventing malaria (blood-stage) Cochrane Database Syst Rev. 2006:CD006199. doi: 10.1002/14651858.CD006199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greenwood B, Targett G. Do we still need a malaria vaccine? Parasite Immunol. 2009;31:582–6. doi: 10.1111/j.1365-3024.2009.01140.x. [DOI] [PubMed] [Google Scholar]
- 11.Agnandji ST, Lell B, Fernandes JF, et al. A phase 3 trial of RTS,S/AS01 malaria vaccine in African infants. N Engl J Med. 2012;367:2284–95. doi: 10.1056/NEJMoa1208394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mackintosh CL, Beeson JG, Marsh K. Clinical features and pathogenesis of severe malaria. Trends Parasitol. 2004;20:597–603. doi: 10.1016/j.pt.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Miller LH, Baruch DI, Marsh K, Doumbo OK. The pathogenic basis of malaria. Nature. 2002;415:673–9. doi: 10.1038/415673a. [DOI] [PubMed] [Google Scholar]
- 14.Iriemenam NC, Khirelsied AH, Nasr A, et al. Antibody responses to a panel of Plasmodium falciparum malaria blood-stage antigens in relation to clinical disease outcome in Sudan. Vaccine. 2009;27:62–71. doi: 10.1016/j.vaccine.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 15.Iriemenam NC, Okafor CM, Balogun HA, et al. Cytokine profiles and antibody responses to Plasmodium falciparum malaria infection in individuals living in Ibadan, southwest Nigeria. Afr Health Sci. 2009;9:66–74. [PMC free article] [PubMed] [Google Scholar]
- 16.McCall MB, Roestenberg M, Ploemen I, et al. Memory-like IFN-gamma response by NK cells following malaria infection reveals the crucial role of T cells in NK cell activation by P. falciparum. Eur J Immunol. 2010;40:3472–7. doi: 10.1002/eji.201040587. [DOI] [PubMed] [Google Scholar]
- 17.Kappe SH, Buscaglia CA, Nussenzweig V. Plasmodium sporozoite molecular cell biology. Annu Rev Cell Dev Biol. 2004;20:29–59. doi: 10.1146/annurev.cellbio.20.011603.150935. [DOI] [PubMed] [Google Scholar]
- 18.Dame JB, Williams JL, McCutchan TF, et al. Structure of the gene encoding the immunodominant surface antigen on the sporozoite of the human malaria parasite Plasmodium falciparum. Science. 1984;225:593–9. doi: 10.1126/science.6204383. [DOI] [PubMed] [Google Scholar]
- 19.Potocnjak P, Yoshida N, Nussenzweig RS, Nussenzweig V. Monovalent fragments (Fab) of monoclonal antibodies to a sporozoite surface antigen (Pb44) protect mice against malarial infection. J Exp Med. 1980;151:1504–13. doi: 10.1084/jem.151.6.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agnandji ST, Lell B, Fernandes JF, et al. Efficacy and safety of the RTS,S/AS01 malaria vaccine during 18 months after vaccination: a phase 3 randomized, controlled trial in children and young infants at 11 African sites. PLoS Med. 2014;11:e1001685. doi: 10.1371/journal.pmed.1001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heppner DG, Jr, Kester KE, Ockenhouse CF, et al. Towards an RTS,S-based, multi-stage, multi-antigen vaccine against falciparum malaria: progress at the Walter Reed Army Institute of Research. Vaccine. 2005;23:2243–50. doi: 10.1016/j.vaccine.2005.01.142. [DOI] [PubMed] [Google Scholar]
- 22.Dunachie SJ, Walther M, Vuola JM, et al. A clinical trial of prime-boost immunisation with the candidate malaria vaccines RTS,S/AS02A and MVA-CS. Vaccine. 2006;24:2850–9. doi: 10.1016/j.vaccine.2005.12.041. [DOI] [PubMed] [Google Scholar]
- 23.Alloueche A, Milligan P, Conway DJ, et al. Protective efficacy of the RTS,S/AS02 Plasmodium falciparum malaria vaccine is not strain specific. Am J Trop Med Hyg. 2003;68:97–101. [PubMed] [Google Scholar]
- 24.Enosse S, Dobano C, Quelhas D, et al. RTS,S/AS02A malaria vaccine does not induce parasite CSP T cell epitope selection and reduces multiplicity of infection. PLoS Clin Trials. 2006;1:e5. doi: 10.1371/journal.pctr.0010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waitumbi JN, Anyona SB, Hunja CW, et al. Impact of RTS,S/AS02(A) and RTS,S/AS01(B) on genotypes of P. falciparum in adults participating in a malaria vaccine clinical trial. PLoS One. 2009;4:e7849. doi: 10.1371/journal.pone.0007849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouattara A, Takala-Harrison S, Thera MA, et al. Molecular basis of allele-specific efficacy of a blood-stage malaria vaccine: vaccine development implications. J Infect Dis. 2013;207:511–9. doi: 10.1093/infdis/jis709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gandhi K, Thera MA, Coulibaly D, et al. Next generation sequencing to detect variation in the Plasmodium falciparum circumsporozoite protein. Am J Trop Med Hyg. 2012;86:775–81. doi: 10.4269/ajtmh.2012.11-0478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bejon P, Ogada E, Mwangi T, et al. Extended follow-up following a phase 2b randomized trial of the candidate malaria vaccines FP9 ME-TRAP and MVA ME-TRAP among children in Kenya. PLoS One. 2007;2:e707. doi: 10.1371/journal.pone.0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ewer KJ, O'Hara GA, Duncan CJ, et al. Protective CD8+ T-cell immunity to human malaria induced by chimpanzee adenovirus-MVA immunisation. Nat Commun. 2013;4:2836. doi: 10.1038/ncomms3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seder RA, Chang LJ, Enama ME, et al. Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science. 2013;341:1359–65. doi: 10.1126/science.1241800. [DOI] [PubMed] [Google Scholar]
- 31.Sabchareon A, Burnouf T, Ouattara D, et al. Parasitologic and clinical human response to immunoglobulin administration in falciparum malaria. Am J Trop Med Hyg. 1991;45:297–308. doi: 10.4269/ajtmh.1991.45.297. [DOI] [PubMed] [Google Scholar]
- 32.Cohen S, McGregor IA, Carrington S. Gamma-globulin and acquired immunity to human malaria. Nature. 1961;192:733–7. doi: 10.1038/192733a0. [DOI] [PubMed] [Google Scholar]
- 33.Polley SD, Tetteh KK, Lloyd JM, et al. Plasmodium falciparum merozoite surface protein 3 is a target of allele-specific immunity and alleles are maintained by natural selection. J Infect Dis. 2007;195:279–87. doi: 10.1086/509806. [DOI] [PubMed] [Google Scholar]
- 34.Genton B, Betuela I, Felger I, et al. A recombinant blood-stage malaria vaccine reduces Plasmodium falciparum density and exerts selective pressure on parasite populations in a phase 1–2b trial in Papua New Guinea. J Infect Dis. 2002;185:820–7. doi: 10.1086/339342. [DOI] [PubMed] [Google Scholar]
- 35.Thera MA, Doumbo OK, Coulibaly D, et al. A field trial to assess a blood-stage malaria vaccine. N Engl J Med. 2011;365:1004–13. doi: 10.1056/NEJMoa1008115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matuschewski K, Mueller AK. Vaccines against malaria—an update. FEBS J. 2007;274:4680–7. doi: 10.1111/j.1742-4658.2007.05998.x. [DOI] [PubMed] [Google Scholar]
- 37.Malkin EM, Durbin AP, Diemert DJ, et al. Phase 1 vaccine trial of Pvs25H: a transmission blocking vaccine for Plasmodium vivax malaria. Vaccine. 2005;23:3131–8. doi: 10.1016/j.vaccine.2004.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu Y, Ellis RD, Shaffer D, et al. Phase 1 trial of malaria transmission blocking vaccine candidates Pfs25 and Pvs25 formulated with montanide ISA 51. PLoS One. 2008;3:e2636. doi: 10.1371/journal.pone.0002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Da DF, Dixit S, Sattabonkot J, et al. Anti-Pfs25 human plasma reduces transmission of Plasmodium falciparum isolates that have diverse genetic backgrounds. Infect Immun. 2013;81:1984–9. doi: 10.1128/IAI.00016-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niederwieser I, Felger I, Beck HP. Limited polymorphism in Plasmodium falciparum sexual-stage antigens. Am J Trop Med Hyg. 2001;64:9–11. doi: 10.4269/ajtmh.2001.64.9. [DOI] [PubMed] [Google Scholar]
- 41.Salanti A, Dahlback M, Turner L, et al. Evidence for the involvement of VAR2CSA in pregnancy-associated malaria. J Exp Med. 2004;200:1197–203. doi: 10.1084/jem.20041579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Srivastava A, Durocher Y, Gamain B. Expressing full-length functional PfEMP1 proteins in the HEK293 expression system. Methods Mol Biol. 2013;923:307–19. doi: 10.1007/978-1-62703-026-7_22. [DOI] [PubMed] [Google Scholar]
- 43.A research agenda for malaria eradication: vaccines. PLoS Med. 2011;8:e1000398. doi: 10.1371/journal.pmed.1000398. [DOI] [PMC free article] [PubMed] [Google Scholar]