Abstract
Most population studies on physical activity and health have involved largely inactive men and women, thus making it difficult to infer if health benefits occur at exercise levels above the current minimum guidelines. The aim was to examine associations between cycling volume and classical cardiovascular risk markers, including hypertension and hypercholesterolemia, in a population sample of habitual cyclists. A nationwide sample comprising 6949 men and women (aged 47.6 years on average) completed questions about their cycling levels, demographics and health. Nearly the entire sample (96.3%) achieved the current minimum physical activity recommendation through cycling alone. There was a dose–response association between cycling volume and risk of diagnosed hypertension (P-trend =0.001), with odds ratios of 0.98 (95% confidence interval (CI), 0.80–1.21), 0.86 (0.70, 1.06), 0.67 (95% CI, 0.53–0.83) across categories of 23–40, 40–61 and >61 metabolic equivalent hours/week (MET-h/week) compared with <23 MET-h/week. These associations persisted in models adjusted for age, sex, smoking, alcohol, body mass index (BMI) and other moderatevigorous physical activities. We also observed inverse associations between cycling volume and other risk factors including BMI and hypercholesterolemia. In summary, results from a population sample of cyclists suggest that additional cardiovascular health benefits can be achieved beyond the current minimum physical activity recommendation.
Introduction
Physical inactivity is thought to account for over £8 billion per year in healthcare costs in the UK alone.1 In order to minimise the public health implications of physical inactivity, it is important to understand the relationship between physical activity and the associated health benefits; central to this is the determination of dose–response relationships. The majority of population-based evidence to date on the cardiovascular health benefits of physical activity has been generated using broad physical activity questionnaires that have rarely considered effects for specific types of activities.2,3
Cycling is an affordable, environmentally friendly and accessible means of activity,4 but our understanding of the health benefits are limited. Lusk et al.5 demonstrated a direct relationship between weight loss and cycling 0–5 and 15–45 min per day, while others have shown consistent increases in fitness measurements during the first 6 months of cycling interventions.6 However, cycling beyond these parameters were not associated with added health benefits. Indeed, Hoevenaar-Blom et al.,7 found no added cardiovascular health benefits cycling less than 3.5 h/week versus cycling more than 3.5 h/week. The small numbers of participants and artificial study environments used in these studies both limit their statistical power and relevance to current cycling habits, which has prevented the determination of a dose–response relationship between cycling and health outcome. However, large observational cross-sectional studies into the health of recreational runners have been successful in demonstrating such dose–response relationships.8, 9, 10, 11, 12 The National Runners' Health Study, which recruited over 100 000 participants, observed significant associations between high weekly mileage and lower usage of anti-hypertensive and cholesterol-lowering medications8 in addition to lower incidence of type II diabetes mellitus,9 coronary heart disease10 and stroke.11 Furthermore, higher running intensities were also associated with reduced risk factors for cardiovascular disease.12
The Cycling for Health UK Study aimed to conduct an observational cross-sectional study to analyse cycling activity in a large cohort of cyclists to determine dose–response associations between cycling activity and classical cardiovascular risk markers, including body mass index (BMI), hypertension and hypercholesterolemia.
Materials and Methods
Study design and participants
The study design was based on The National Runners' Health Study.8 We designed an online survey and participants were recruited into the study in 2013. A link to the survey was advertised via various national UK cycling bodies including the national cycling charity, the CTC, British Cycling, Sky Ride, Cycling Weekly and Cycling Fitness magazine. In addition we used other forms of social media, such as a study twitter account (@cyclinghealthUK) to recruit participants into the study. The aim was to capture participants from a variety of cycling backgrounds ranging from commuters to amateur racing cyclists. The study gained ethical approval from the University College London Graduate School Ethics Committee. By completing the questionnaire participants implied their consent to take part in the study.
Survey measures
The survey included questions on demographics (age, sex and education), cycling history (number of years cycling, average weekly total cycling distance, time, speed and best times for various standard distance competitive cycling races), weight, height, resting heart rate (self-recorded at the radial artery from the ventral aspect of the wrist), alcohol intake, current and past cigarette use, history of cardiovascular events (heart attacks, stroke) and cancer and medications/ physician diagnosis for hypertension, high cholesterol or diabetes. Participation in non-cycling physical activities was also collected using the International Physical Activity Questionnaire.13
Statistical analysis
Average cycling speed was converted into MET using the compendium of physical activities,14 and further multiplied by weekly cycling time to provide a measure of total cycling volume (MET-h/week). We used linear regression to examine associations between cycling volume and continuous dependent variables. We used multiple logistic regression to compute odds ratios (ORs) with accompanying 95% confidence intervals (CIs) for the association between cycling volume and diagnosed hypertension/hypercholesterolemia. For these analyses cycling volume was further categorised into four equal groups. The models were adjusted for potential confounding factors, including age (categorised into 10 year age bands), sex, smoking (never; previous; current), weekly alcohol intake (0 units; 1–10 units; 11–21 units; above 21 units), BMI (normal weight, BMI<25; overweight, BMI 25–30; obese, BMI ⩾30 kg m−2) and lastly for other moderate–vigorous physical activities (zero h/week; 1–3; >3–7; >7). Analyses were conducted using SPSS version 21 (Chicago, IL, USA).
Results
Participant characteristics
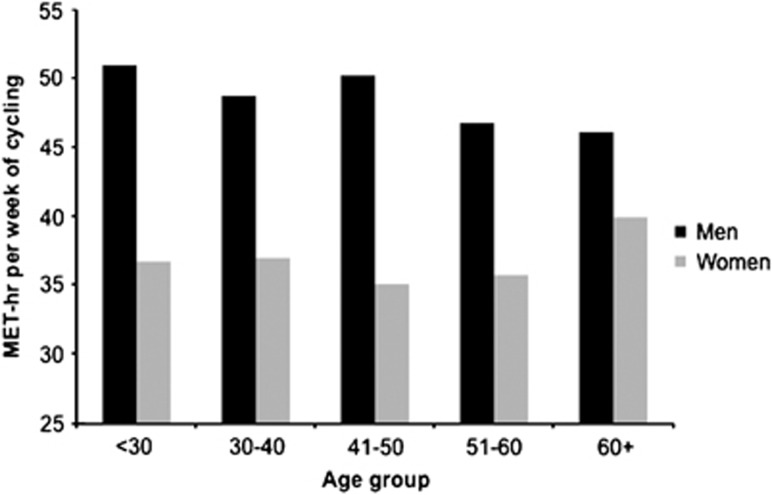
7006 participants completed the survey and after cleaning the data a sample size of 6949 was used in the present analysis. Participants providing implausible data (for example, cycling >56 h/week) were removed. The characteristics of the sample are provided in Table 1. The age of the sample ranged from 16–88 years old, they were largely male (75.6%), and on average cycled 4 days per week expending 45.5 MET-h/week on cycling alone (Table 1). Nearly the entire sample (96.3%) achieved the current minimum physical activity recommendation (7.5 MET-h/week) through cycling alone. Men consistently replorted higher cycling volumes than women across the age strata. There was a trend for decreasing cycling volume with age in men, but this pattern was not observed in women (Figure 1). The age differences were largely explained by lower cycling speed (see Supplementary Table S1).
Table 1. Descriptive characteristics of the sample (N=6949).
| Characteristic | Mean average | Range |
|---|---|---|
| Age | 47.6 | 16–88 |
| % Men | 75.6 | |
| % smokers | 3.6 | |
| Body mass index | 25.02 | 15–76 |
| Days per week cycling | 4.2 | 1–7 |
| Years of cycling | 21.6 | 0–78 |
| MET-h/week cycling | 45.5 | 0–300 |
| Other moderate–vigorous physical activity (h/week) | 3.4 | 0–28 |
Abbreviation: MET-h/week, metabolic equivalent hours/week.
Figure 1.
Average weekly cycling volume measured by metabolic equivalent (MET-h per week) in men and women in <30, 30–40, 41–50, 51–60 and 60+ age groups.
Validation of cycling activity
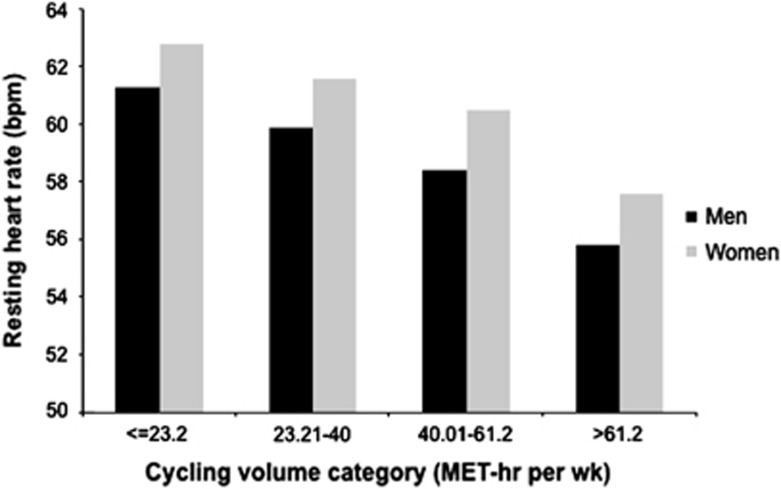
Resting heart rate is commonly used to validate physical activity assessment, since bradycardia is a cardiac manifestation of aerobic conditioning. We observed a statistically significant inverse relationship between reported cycling volume and resting heart rate (Figure 2). Each MET-h/week of cycling was associated with −0.07 beats per min (bpm) (95% CI, −0.08, −0.06) reduction after adjusting for age and sex.
Figure 2.
Average resting heart rate measured by beats per min (bpm) in men and women organised by cycling volume ⩽23.3, 23.21–40, 40.01–61.2 and >61.2 MET-h/week. Data adjusted for age.
Association with cardiovascular risk factors
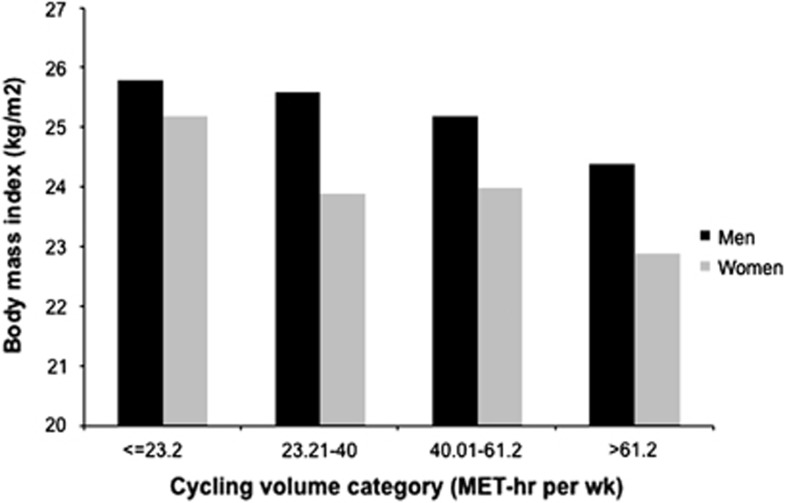
We observed a significant inverse relationship between reported cycling volume and BMI (Figure 3). Each MET-h/week of cycling was associated with 0.020 kg m−2 (95% CI, 0.023–0.017) lower BMI after adjusting for age and sex. There was a dose-dependent association between cycling volume and risk of diagnosed hypertension (Table 2), and the highest category of cycling was associated with a 0.67 (95% CI, 0.53–0.83) lower odds in age and sex adjusted analyses. These associations persisted in fully adjusted models. A similar pattern of results was obtained in relation to hypercholesterolemia (Table 3). To ensure results were not confounded by differences in contact with health-care services, we analysed associations between cycling activity and visits to primary care over the previous year. We did not demonstrate any association between cycling activity and visits to primary care, suggesting our results were not confounded by differences in health-care usage.
Figure 3.
Body mass index (kg m−2) in men and women organised by cycling volume ⩽ 23.3, 23.21–40, 40.01–61.2 and >61.2 MET-h/week. Data adjusted for age.
Table 2. Association between cycling volume and risk of diagnosed hypertension.
| Cycling volume (MET-h/week) | Cases/N | Model 1 OR (95% CI) | Model 2 OR (95% CI) |
|---|---|---|---|
| <23.2 | 233/1832 | 1.00 (ref) | 1.00 (ref) |
| 23.21–40.0 | 230/1791 | 0.98 (0.80–1.21) | 1.08 (0.88–1.33) |
| 40.01–61.2 | 193/1652 | 0.86 (0.70–1.06) | 0.94 (0.76–1.16) |
| >61.2 | 163/1674 | 0.67 (0.53–0.83) | 0.79 (0.63–0.99) |
Abbreviations: BMI, body mass index; CI, confidence interval; MET-h/week, metabolic equivalent hours/week.
Model 1: analyses adjusted for age and sex; Model 2: analyses adjusted for age, sex, BMI, smoking, alcohol and other moderate–vigorous physical activity.
Table 3. Association between cycling volume and risk of high cholesterol.
| Cycling volume (MET-h/week) | Cases/N | Model 1 OR (95% CI) | Model 2 OR (95% CI) |
|---|---|---|---|
| <23.2 | 260/1832 | 1.00 (ref) | 1.00 (ref) |
| 23.21–40.0 | 226/1791 | 0.84 (0.69–1.03) | 0.89 (0.73–1.10) |
| 40.01–61.2 | 205/1652 | 0.81 (0.66–0.99) | 0.85 (0.69–1.05) |
| >61.2 | 189/1674 | 0.70 (0.56–0.86) | 0.78 (0.63–0.97) |
Abbreviations: BMI, body mass index; CI, confidence interval; MET-h/week, metabolic equivalent hours/week.
Model 1: Analyses adjusted for age and sex; Model 2: analyses adjusted for age, sex, BMI, smoking, alcohol and other moderate–vigorous physical activity.
Sensitivity analyses
We repeated the analysis after removing 186 participants reporting prior history of a cardiovascular event or angina, although the associations remained largely unchanged. For example, the highest cycling volume category was associated with a 0.66 (95% CI, 0.52–0.83) lower odds of diagnosed hypertension and 0.70 (95% CI, 0.56–0.88) lower odds of hypercholesterolemia in age and sex adjusted models.
We ran additional models to explore associations between ‘other physical activities' and hypertension. In age and sex adjusted models there was an inverse association between moderate—vigorous physical activity and risk of hypertension (P-trend=0.04). For example, in relation to 0 h per week (reference), participants reporting 1–3, 3–7, and >7 h/week demonstrated odds of 0.82 (95% CI, 0.65–1.03), 0.71 (0.56–0.90), 0.81 (0.61–1.07). Nevertheless, these associations did not persist after adjusting for other covariables and cycling volume (P-trend =0.13).
We also explored associations between ‘cycle commuting' and hypertension. A sub-sample of N=2253 reported using their bike to commute. In models adjusted for age, sex, smoking, weekly alcohol intake, BMI and other physical activities, there was an inverse association between commuting and risk of hypertension. For example, in relation to <15.75 MET-h/week (reference), participants reporting 15.8–27, 27.1–40 and >40 MET-h/week demonstrated odds of 0.78 (95% CI, 0.51–1.17), 0.74 (0.48–1.13) and 0.65 (0.42–1.01), respectively. We did not, however, observe any associations between commuting and BMI (data not shown).
Lastly, we modelled age and sex interaction terms by cycling volume although they were not significant. For example, we observed similar dose–response trends for anti-hypertensive effects of cycling in both sexes; men (age adjusted OR= 0.71, 0.56–0.90) and women (0.42, 0.20–0.87) that reported the highest cycling volumes were at the lowest risk of hypertension.
Discussion
We analysed data from 6949 regular cyclists regarding cycling volume and cardiovascular risk factors. According to the current physical activity guidelines, the vast majority (96.3%) of the sample met the criteria for adequate physical activity based on cycling alone. Despite this, we demonstrated clear health benefits of physical activity over and above the minimum guidelines. Indeed, we demonstrated an inverse, dose–response relationship between cycling volume and risk of diagnosed hypertension and hypercholesterolemia suggesting that higher cycling volumes offer greater health benefits. The associations for cycling were independent of other forms of physical activity.
Our study population were exclusively regular cyclists with high-activity levels. The extent to which this can be applied to the wider population is limited. However, even within this active population we managed to identify key trends in cardiovascular risk factors in relation to cycling activity. This is in contrast to previous experimental studies that have failed to demonstrate sustained trends in health benefits for increasing doses.5,6 It must be acknowledged that our data relies on self-reported cardiovascular risk factors and cycling activity, which may have invited bias. The validity of self-reported height and weight as a continuous variable is mixed,15 and the specificity for recall of hypertension and hypercholesterolemia is good.16 Nevertheless, we cannot rule out the possibility of undiagnosed hypertension. We cannot completely control for biases regarding participants' personal health perception; however, following analysis of visits to primary care services, we did not find any evidence to show a link between cycling activity and usage of primary care suggesting more active cyclists were not less likely to seek medical treatment. It has been problematic to validate self-reported cycling activity largely because of the inability of objective movement sensors (accelerometers) to accurately detect cycling; however, our demonstration of decreasing resting heart rate with increasing cycling volume is suggestive of a physiological bradycardia, which reflects higher levels of cardiovascular fitness. In addition, many cyclists use cycling computers and are thus able to recall speed, distance and time more accurately. It is important to acknowledge the limitations of our observational cross-sectional design. Our statistical analyses help to control for important confounding variables, but our observational (cross-sectional) design prevent us from inferring causality. Despite this, the Bradford-Hill considerations describe the importance of biological gradients in describing causality in epidemiological data,17 and thus our findings make an important contribution to the field.
After taking into consideration a number of caveats, our results represent one of the most detailed studies of the association between cardiovascular risk factors and cycling activity. BMI, hypertension and hypercholestrolaemia are well-recognised risk factors for coronary heart disease18 and thus the implications of increased cycling activity in the population may have profound effects on mortality and morbidity secondary to cardiac disease. Few studies have specifically examined associations between cycling and cardiovascular disease, and the results are inconsistent. For example, in the Shanghai Women's Health Study, cycling was associated with lower risk of all cause mortality but not incident cardiovascular disease after accounting for other types of physical activities.19 However, cycling volumes were relatively low as the threshold for the highest category (>3.5 MET-h/day) barely reached the cut-off for the lowest category in the present study. In a sample of Dutch adults where 75% reported regular cycling, there was an inverse association between cycling and cardiovascular disease although no dose–response was observed.7 And data from a large general population sample of English adults provided mixed support for benefits of cycling in relation to mortality.20 Numerous studies have examined associations between active commuting and cardiovascular disease risk21,22 although the analyses have often combined cycling with walking thus making it difficult to dissect the specific effects of cycling. Taken together, extrapolating data on the health benefits of cycling from general population studies is problematic because of insufficient participation in cycling and relatively low cycling volumes. The major strength of our study was the recruitment of cyclists enabling us to examine detailed dose–response associations. Nevertheless, caution should be taken when extrapolating these data to the general population as the present sample of habitual cyclists are unrepresentative in numerous ways, including other favourable lifestyle habits (for example, low rates of smoking~3.6%). In the National Runners' Health Study a similar dose–response reduction in BMI, hypertension and hypercholestrolemia was observed with increased running-miles per week.8 However, where running may prohibit some people with existing injuries or lifestyle limitations, cycling may be used as a reasonable substitute.
In 2008, based on self-report survey just 39% of English men and 29% of women who took part in the Health Survey for England met physical activity guidelines.23 Cycling is accessible to most of the population and offers a potentially low cost, environmentally friendly solution to increase physical activity levels, since it can be incorporated into people's daily lives as means of transport.4,24 Nevertheless, there is little emphasis on the benefits of exceeding minimum physical activity recommendations or guidance regarding the volume and type of exercise required. This data, in addition to existing evidence, demonstrate the benefits of physical activity in reducing cardiovascular disease risk factors in the population and emphasise the role of cycling in this endeavour.
Acknowledgments
We thank the national cycling charity, the CTC, British Cycling, Sky Ride, Cycling Weekly and Cycling Fitness magazine who helped to distribute the questionnaire to their members, subscribers and readers. Hamer is supported by The British Heart Foundation (RE/10/005/28296).
The authors declare no conflict of interest. The CTC, British Cycling, Sky Ride, Cycling Weekly and Cycling Fitness magazine were solely involved in the distribution of the questionnaire and they had no role in the funding, design or analysis of the study. The funders had no role in the study design; in the collection, analysis and interpretation of data; in writing of the report; or in the decision to submit the paper for publication.
Footnotes
Supplementary Information accompanies this paper on the Journal of Human Hypertension website (http://www.nature.com/jhh)
Supplementary Material
References
- National Institute of Health and Clinical Excellence. National Costing Report. Physical activity and the environment 2008 (Last accessed 02/12/13): http://www.nice.org.uk/nicemedia/live/11917/38990/38990.pdf.
- Huai P, Xun H, Reilly KH, Wang Y, Ma W, Xi B. Physical activity and risk of hypertension: a meta-analysis of prospective cohort studies. Hypertension 2013; 62(6): 1021–1026. [DOI] [PubMed] [Google Scholar]
- Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation 2011; 124(7): 789–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell J, Cohen JM, Watkins S, Tyler N. Synergies between low-carbon and healthy transport policies. Proc Inst Civil Eng 2011; 164: 127–139. [Google Scholar]
- Lusk AC, Mekary RA, Feskanich D, Willett WC. Bicycle riding, walking, and weight gain in premenopausal women. Arch Int Med 2010; 170: 1050–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriksen IJM, Zuiderveld B, Kemper HCG, Bezemer PD. Effect of commuter cycling on physical performance of male and female employees. Med Sci Sports Exerc 2000; 32: 504–510. [DOI] [PubMed] [Google Scholar]
- Hoevenaar-Blom MP, Wendel-Vos GCV, Spijkerman AMW, Kromhout D, Verschuren WMM. Cycling and sports, but not walking, are associated with 10-year cardiovascular disease incidence: the MORGEN study. Eur J Cardiovasc Prev Rehab 2011; 18(1): 41–47. [DOI] [PubMed] [Google Scholar]
- William P. Relationship of distance in per week to coronary heart disease risk factors in 8283 male runners. Arch Intern Med 1997; 157(2): 191–198. [PMC free article] [PubMed] [Google Scholar]
- Williams PT. Changes in vigorous physical activity and incident diabetes in male runners. Diabetes Care. 2007; 30(11): 2838–2842. [DOI] [PubMed] [Google Scholar]
- Williams PT. Reductions in incident coronary heart disease risk above guideline physical activity levels in men. Atherosclerosis 2010; 209(2): 524–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PT. Reduction in incident stroke risk with vigorous physical activity: evidence from 7.7-year follow-up of the national runners' health study. Stroke 2009; 40(5): 1921–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PT. Relationship of running intensity to hypertension, hypercholesterolemia, and diabetes. Med Sci Sports Exerc 2008; 40(10): 1740–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Park I, Kang M. Convergent validity of the international physical activity questionnaire (IPAQ): meta-analysis. Public Health Nutr 2013; 16(3): 440–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C et al. Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc 2011; 43(8): 1575–1581. [DOI] [PubMed] [Google Scholar]
- Lassale C, Péneau S, Touvier M, Julia C, Galan P, Hercberg S et al. Validity of web-based self-reported weight and height: results of the Nutrinet-Santé study. J Med Internet Res 2013; 15(8): e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med 2000; 18(3): 215–218. [DOI] [PubMed] [Google Scholar]
- Hill AB. The Environment and Disease: Association or Causation? Proc Roy Soc Med 1965; 58(5): 295–300. [PMC free article] [PubMed] [Google Scholar]
- Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998; 97(18): 1837–1847. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Jurj AL, Shu XO, Li HL, Yang G, Li Q et al. Influence of exercise, walking, cycling, and overall nonexercise physical activity on mortality in Chinese women. Am J Epidemiol 2007; 165(12): 1343–1350. [DOI] [PubMed] [Google Scholar]
- Sahlqvist S, Goodman A, Simmons RK, Khaw KT, Cavill N, Foster C et al. The association of cycling with all-cause, cardiovascular and cancer mortality: findings from the population-based EPIC-Norfolk cohort. BMJ Open 2013; 3(11): e003797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Chida Y. Active commuting and cardiovascular risk: a meta-analytic review. Prev Med 2008; 46(1): 9–13. [DOI] [PubMed] [Google Scholar]
- Laverty AA, Mindell JS, Webb EA, Millett C. Active travel to work and cardiovascular risk factors in the United Kingdom. Am J Prev Med 2013; 45(3): 282–288. [DOI] [PubMed] [Google Scholar]
- Health and Social Care Information Centre. Health, social care and lifestyles- Summary of key findings. in: Health Survey for England (Last Accessed 02/12/13): https://catalogue.ic.nhs.uk/publications/public-health/surveys/heal-surv-eng-2011/HSE2011-Sum-bklet.pdf (2011).
- Woodcock J, Tainio M, Cheshire J, O'Brien O, Goodman A. Health effects of the London bicycle sharing system: health impact modelling study. Brit Med J 2014; 348: g425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.