Abstract
Influenza A virus (IAV) has its natural reservoir in wild waterfowl, and emerging human IAVs often contain gene segments from avian viruses. The active drug metabolite of oseltamivir (oseltamivir carboxylate [OC]), stockpiled as Tamiflu for influenza pandemic preparedness, is not removed by conventional sewage treatment and has been detected in river water. There, it may exert evolutionary pressure on avian IAV in waterfowl, resulting in the development of resistant viral variants. A resistant avian IAV can circulate among wild birds only if resistance does not restrict viral fitness and if the resistant virus can persist without continuous drug pressure. In this in vivo mallard (Anas platyrhynchos) study, we tested whether an OC-resistant avian IAV (H1N1) strain with an H274Y mutation in the neuraminidase (NA-H274Y) could retain resistance while drug pressure was gradually removed. Successively infected mallards were exposed to decreasing levels of OC, and fecal samples were analyzed for the neuraminidase sequence and phenotypic resistance. No reversion to wild-type virus was observed during the experiment, which included 17 days of viral transmission among 10 ducks exposed to OC concentrations below resistance induction levels. We conclude that resistance in avian IAV that is induced by exposure of the natural host to OC can persist in the absence of the drug. Thus, there is a risk that human-pathogenic IAVs that evolve from IAVs circulating among wild birds may contain resistance mutations. An oseltamivir-resistant pandemic IAV would pose a substantial public health threat. Therefore, our observations underscore the need for prudent oseltamivir use, upgraded sewage treatment, and surveillance for resistant IAVs in wild birds.
INTRODUCTION
Influenza A virus (IAV) can infect many mammalian and avian species, although wild waterfowl, primarily dabbling ducks, are the principal reservoir host (1, 2). New human IAVs, including pandemic viruses, may contain gene segments of avian origin (1, 3). IAV infection in waterfowl is mainly gastrointestinal and generates very limited symptoms (1, 4). In contrast to mammalian IAVs, where relatively limited numbers of subtypes circulate, avian viruses are genetically variable, with multiple subtype combinations cocirculating and with a high rate of genome reassortment (1, 5). At the interface between wild and domesticated waterfowl, poultry, swine, and humans, new IAV strains evolve. New strains can emerge through reassortment of gene segments in coinfected individuals and by subsequent point mutations under immunologic or host-adaptive selective pressure (1, 3, 6).
There are limited means for responding to a severe influenza pandemic, and currently, preparedness plans worldwide rely almost entirely on the neuraminidase inhibitor (NAI) oseltamivir (Tamiflu) (7, 8). Viral resistance to anti-influenza drugs is well known to emerge in humans under treatment. All currently circulating human H3N2 and H1N1 lineages are largely resistant to adamantanes, which are no longer recommended for the treatment of seasonal influenza (9). Oseltamivir exerts its inhibitory effect through the active metabolite oseltamivir carboxylate (OC) by binding to the active enzymatic site of neuraminidase (NA). Resistance to OC is caused primarily by mutations that change the shape of the catalytic site, by changes in either active-site residues or framework supportive residues. The two phylogenetic groups of NAs (N1 and N2) differ slightly in sensitivity to the drug and have distinct resistance mutations; H274Y (N2 numbering) is most common in N1, while R292K and E119V are most common in N2 (10). Treatment of IAV-infected individuals with an NAI can generate resistant viruses, as has been reported in infections with both human (11) and avian H5N1 (12) and H7N9 (13) strains. Of more concern, however, is the circulation of NAI-resistant human influenza A (H1N1) virus strains in the absence of selective drug pressure, which has been reported primarily for the seasonal influenza A (H1N1) 2008-2009 virus (14) and for clusters of influenza A (H1N1)/pdm2009 viruses (15).
To date, surveillance of antiviral resistance in avian IAVs from wild birds has been limited. There is, however, accumulating evidence that waterfowl can be exposed to NAIs in the environment, which may cause selection of resistant IAV variants in the natural reservoir. OC, the drug primarily studied, is inefficiently removed by conventional sewage water treatment (16, 17). Consequently, OC can be discharged to water environments where waterfowl reside, and OC concentrations as high as 865 ng/liter have been detected in surface water (18–20). If avian IAV is exposed to OC in its natural host and acquires resistance, there is a risk that emerging human-pathogenic IAV strains carrying avian gene segments may be resistant (21). NAI resistance in an emerging pandemic virus would be a substantial public health concern, especially in the early phase of a pandemic, before new, efficient vaccines could be distributed (22).
In vivo experiments have demonstrated that OC resistance evolves in avian IAVs of both the N1 and N2 neuraminidase groups when infected mallards (Anas platyrhynchos) are exposed to 0.95 to 12 μg/liter OC in their water (23–25). However, a fundamental question for the persistence of NAI resistance in the environment is whether a resistance mutation is retained without continuous selective drug pressure. To address this question, we examined the persistence of OC resistance in an avian influenza A (H1N1)/NA-H274Y virus strain during natural transmission and replication in mallard ducks.
MATERIALS AND METHODS
Virus.
In our experiments, we used an avian H1N1 isolate with the H274Y resistance mutation in NA, Influenza A/Mallard/Sweden/51833/2006 (H1N1)/NA-H274Y (referred to below as A/51833/H274Y). This isolate originated from the wild-type (wt) Influenza A/Mallard/Sweden/51833/2006 (H1N1) isolate (referred to below as A/51833/wt), which had been recovered from a wild mallard in southern Sweden (4) (GenBank accession number of NA, AEA02276). The A/51833/wt isolate had previously been isolated, subtyped, and experimentally exposed to OC in the same mallard model as that used in these experiments, as described in reference 23. The experimentally evolved A/51833/H274Y virus (23) was propagated in specific-pathogen-free embryonated chicken eggs as described in detail in reference 24 and was titrated based on the 50% embryo infective dose (EID50) (26), to 108.4 EID50/ml allantoic fluid, which was used as the viral stock solution.
Drugs.
OC and deuterium-labeled OC were obtained from F. Hoffmann-La Roche Ltd., Basel, Switzerland. Zanamivir (ZA) was purchased locally as Relenza (GlaxoSmithKline). The drugs were dissolved in MilliQ water and were stored at −20°C.
Mallard model.
Male mallards, 2 to 3 months old, were purchased from a Swedish game farm and were kept isolated indoors at the animal facilities of the National Veterinary Institute of Sweden, after ethical approval by the Ethical Committee on Animal Experiments in Uppsala (permit C201/11) and in accordance with legislation and recommendations from the Swedish Agricultural Board. Before the start of the experiment, the ducks tested negative for present or previous IAV infection. Serological tests (Avian Influenza Virus Antibody test kit; IDEXX Laboratories Europe, The Netherlands) were carried out on blood samples taken from all ducks upon arrival at the facility, and fecal samples, collected on the day of entry into the experiment, were tested by real-time reverse transcriptase PCR (RRT-PCR) targeting the IAV matrix gene (see below).
At the start of the experiment, two mallard ducks (“generation 1”) were infected by inoculation of 1 ml of the A/51833/H274Y viral stock solution into the esophagus and were placed in an experimental room that contained a single 170-liter water pool for swimming and drinking, as well as feed ad libitum. Prior to the experiment, OC was added to the water to a final concentration of 79 μg/liter (278 nM); thereafter, the water was changed daily, and OC was added according to the intended concentrations. Three days postinoculation (p.i.), the OC concentration was reduced to 30 μg/liter (106 nM); two uninfected ducks (generation 2) were introduced and were housed in the experimental room together with generation 1 for 2 days, to allow viral transmission. At 5 days p.i., generation 1 was euthanized by intravenous injection of sodium pentobarbital (100 mg Pentobarbital vet. [100 mg/ml] per kg of body weight). At 6 days p.i., the OC concentration was reduced to 11 μg/liter (39 nM), and two new mallards were introduced and were housed together with generation 2. This procedure, with overlapping generations and decreasing OC concentrations, was repeated for 10 generations of ducks over 32 days (Table 1). OC concentrations were successively reduced (to 2.5, 0.93, 0.26, 0.069, 0.027, and 0.0083 μg/liter) until 26 days p.i., after which no OC was added to the water (days 27 to 32 p.i.) (Table 1).
TABLE 1.
Experimental model with decreasing OC exposure of IAV-infected mallards
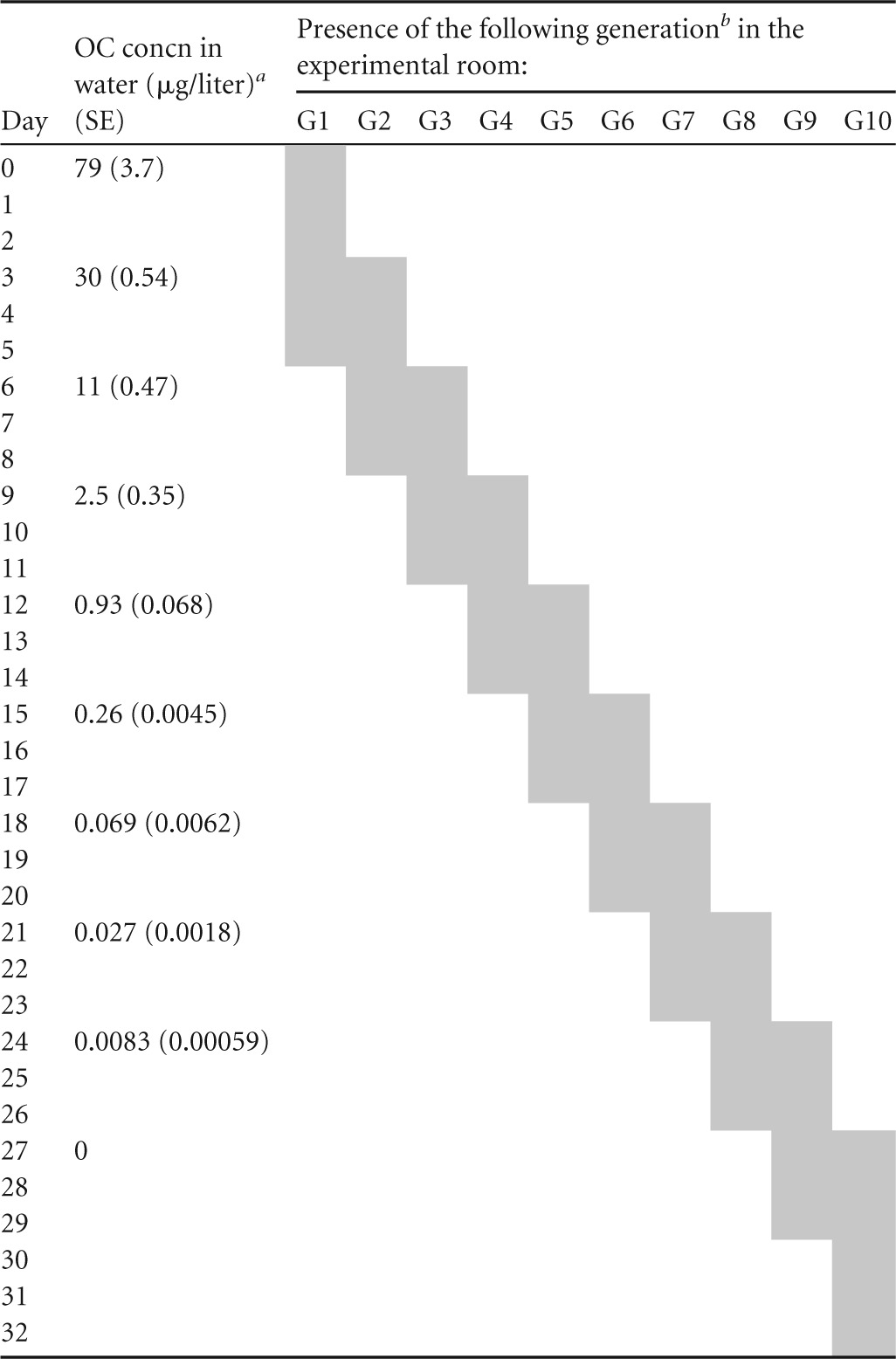
Mean concentration for three experimental days.
Shading indicates presence. G, generation. Each generation consisted of two mallard ducks.
Fecal samples from individual birds were collected daily by putting each bird in a clean box for 5 to 20 min and then swabbing feces from the box. On a few occasions, when birds did not defecate, samples were obtained by cloacal swabbing. Water samples for viral detection were taken daily. Although the individual mallards were successively replaced, the experiment was designed to allow continuous propagation and evolution of the viral population under decreasing drug pressure. Naïve individuals were introduced at peak viral shedding, after 2 days, to facilitate transmission. Between the euthanasia of one generation and the introduction of a new one, there was a 1-day gap to ensure continuous virus transmission between generations (e.g., generation 1 was removed 1 day before generation 3 was introduced, to make sure that generation 3 was infected by virus from generation 2 and not from generation 1). OC exposure levels ranging from approximately 80 μg/liter (a concentration at which the mutant A/51833/H274Y virus was known to dominate completely [23]) to zero were chosen, and half of the concentrations were lower than the resistance induction level of 0.95 μg/liter (23).
Viral detection and sequencing of neuraminidase.
Viral RNA was extracted from fecal samples, water isolates, and egg isolates in a Magnatrix 8000 extraction robot (Magnetic Biosolutions) with a Vet Viral NA kit (NorDiag ASA). IAV was detected and quantified by RRT-PCR targeting the IAV matrix gene (27) using an iScript one-step reverse transcriptase PCR (RT-PCR) kit for probes (Bio-Rad); 25-μl reaction mixtures were run in a Rotor-Gene 2000 real-time thermocycler (Corbett Research) as described in detail in reference 24.
NA was amplified from IAV-positive fecal samples by one-step RT-PCR using primers designed previously for amplifying and sequencing the NA of A/51833/wt (Thermo Hybaid, Interactiva Division) and a SuperScript III One-Step RT-PCR system with Platinum Taq High Fidelity DNA polymerase (Life Technologies) as described in reference 23, with 1 μl enzyme mixture and 400 nM each primer. PCR products were confirmed by gel electrophoresis and were purified by ExoSAP-IT treatment (Affymetrix Inc.); 2 µl of the reagent was used to purify 24 μl of PCR product. Amplicons were sequenced by Macrogen Inc. in South Korea or The Netherlands using two forward primers (primers 1 and 5) and two reverse primers (primers 2 and 6) as presented in Table 2 of reference 23. The sequencing results were analyzed in SeqScape software, version 2.7 (Applied Biosystems), with the NA sequence of A/51833/wt as the reference.
To further evaluate the possible reemergence of wild-type virus at a proportion too small to discover by standard Sanger sequencing, deep sequencing was performed on three early (generations 1 and 2) and three late (generation 10) fecal samples from the experiment. RNA was extracted with TRIzol (Life Technologies), reverse transcribed, and PCR amplified using the PathAmp FluA Reagents with high-fidelity polymerase (revision B.0; Life Technologies). The resulting amplicons were purified using the Agencourt AMPure XP reagent (Beckman Coulter) and were quantified, and libraries were prepared with the Ion Xpress Plus fragment library kit (Life Technologies). After size selection on the BluePippin instrument (Sage Science), samples were quantified using the Fragment Analyzer instrument (Advanced Analytical Technologies) and were pooled, followed by emulsion PCR on the Ion OneTouch 2 system with Ion PGM Template OT2 400 kit (Life Technologies) chemistry. Enrichment was carried out using the Ion OneTouch enrichment system (ES) (Life Technologies). Samples were loaded onto an Ion 316 chip and were sequenced on the Ion PGM system using Ion PGM Sequencing 400 kit (read length, 400 bp; Life Technologies) chemistry.
Phenotypic resistance testing.
To test NA inhibition by OC and ZA, 16 fecal samples (eight from generation 1 or 2 and eight from generation 10) were propagated in embryonated chicken eggs as described above. The obtained isolates were subjected to standard Sanger sequencing (as described above for fecal samples) to confirm resistance after egg propagation. NA inhibition by OC and ZA was determined from duplicate samples in 96-well plates using the fluorogenic substrate 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA; Sigma) (28) and serial dilutions (0.015 to 4,000 nM) of OC and ZA; the fluorescent product was detected in a GloMax-Multi microplate multimode reader (Promega) as described in reference 23. Fifty percent inhibitory concentrations (IC50) were calculated in GraphPad Prism software, version 5 (GraphPad).
OC concentration in water.
Water samples were collected daily after 24 h of exposure (when the water was changed). To verify the stability of the OC concentration over 24 h, water samples were also collected directly after OC addition during the periods of highest (79-μg/liter) and lowest (0.008-μg/liter) OC exposure. An on-line solid-phase extraction–liquid chromatography–tandem mass spectrometry (SPE–LC–MS-MS) system was used to verify the OC concentrations during the experiment. The SPE–LC–MS-MS system used was the same as that described in detail in reference 23, except that an Oasis HLB extraction column (length, 20 mm; inside diameter, 2.1 mm; particle size, 15 μm; Waters S.A.S., Saint-Quentin-en-Yvelines, France) was used here. Briefly, 10 ml of each water sample was filtered and acidified (0.1% formic acid by volume), and 1 ml was then analyzed by the SPE–LC–MS-MS system (for the highest exposure level, the samples were diluted 1/10 with water). Samples were quantified by an internal standard method with deuterated OC as the internal standard and with six calibration points.
RESULTS
Quantification of OC in water.
Table 1, presenting the mean OC concentration (n = 3) and standard error (SE) at each exposure level, shows that the daily OC concentration at each level was relatively stable. The differences in the average OC concentration between freshly prepared water and water tested after 24 h were low (5% at 79 μg/liter and 8% at 0.008 μg/liter), showing that the OC concentrations were stable over a 24-h exposure period. Thus, the variation in OC concentrations within and between experimental days was low. The limit of quantification (LOQ) for the SPE–LC–MS-MS method was 1 ng/liter, and the linearity (R2) of the calibration curve was 1.0000.
Viral detection and NA genotype.
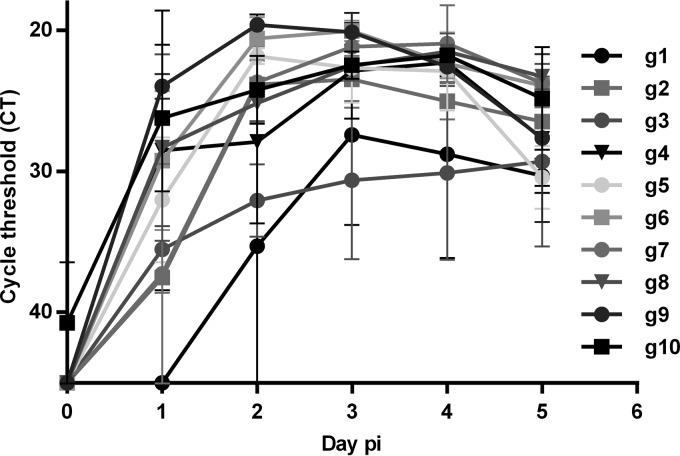
All birds in the experiment were successfully infected, as determined by IAV shedding in fecal samples, which was detected from 2 days p.i. in generation 1 and from the first day after introduction in all following generations (Fig. 1). Virus was detected in experimental water from 2 days p.i. all through the experiment, with a mean RRT-PCR cycle threshold (CT) value of 31 (SE, 0.56).
FIG 1.
Viral shedding in feces from mallards was quantified by RRT-PCR of the IAV matrix gene. CT values of >45 were considered to indicate a negative sample. Whiskers indicate standard errors of the means for two samples. The number of days after inoculation (for generation 1 [g1]) or after introduction to the experimental room (for g2 to g10) is shown along the x axis. Each generation consisted of two mallard ducks.
Standard sequencing of 103 fecal samples from all generations of the experiment showed that all contained the NA H274Y mutation, with no visible wild-type residue at position 274. At NA amino acid residue 222, the A/51833/H274Y virus, like the original A/51833/wt virus, had asparagine (N), which differs from the more common residue at this site, isoleucine (I).
The results of targeted deep sequencing of the codon for NA amino acid 274 did not differ between early fecal samples, from 4 and 6 days p.i., and late samples, from 30 and 31 days p.i. The CAC codon codes for the wild-type amino acid histidine (H), and TAC codes for tyrosine (Y); the latter dominated by more than 99% in all samples from the experiment. The total numbers of reads at the NA-274 site were 205 to 869 for experimental samples and viral inoculants. Both early and late experimental samples had <1% nonthymine (non-T) nucleotide reads and no more cytosine (C) reads than the sequencing noise of adenine (A) and guanine (G) combined (Table 2).
TABLE 2.
Targeted deep sequencing of the codon for NA amino acid residue 274
| Virus or sample | Time of sampling (days p.i.) | No. of reads at bp 820 of the NA gene |
Consensus codon for NA aa 274 | |||
|---|---|---|---|---|---|---|
| A | C | G | T | |||
| Viruses | ||||||
| A/51833 (H1N1)/wt | 0 | 550 | 0 | 3 | CAC | |
| A/51833 (H1N1)/H274Y | 3 | 4 | 1 | 742 | TAC | |
| Samplesa | ||||||
| g 1:1 | 4 | 2 | 2 | 0 | 283 | TAC |
| g 2:1 | 6 | 2 | 1 | 0 | 202 | TAC |
| g 2:2 | 6 | 5 | 3 | 3 | 423 | TAC |
| g 10:1 | 30 | 4 | 1 | 1 | 654 | TAC |
| g 10:2 | 30 | 3 | 0 | 3 | 863 | TAC |
| g 10:1 | 31 | 1 | 1 | 0 | 606 | TAC |
Fecal samples from mallards, labeled by generation and mallard number (e.g., “g 2:1” stands for mallard number 1 of generation 2).
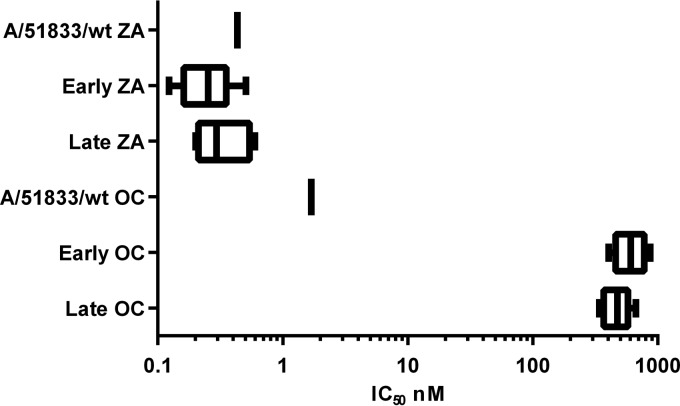
Phenotypic resistance results.
The mean IC50 of OC for the 16 duplicate samples tested was 549 nM (SE, 38.5 nM), with no significant difference between early and late samples (P = 0.081; 95% confidence interval [95% CI] for differences in means, −18.9 to 286 nM, with a two-sided t test for independent samples) (Fig. 2). There was no reduction in sensitivity to ZA (IC50, 0.31 nM [SE, 0.038 nM]). For the original A/51833/wt virus, the mean IC50 of OC from 6 repeated assays was 1.6 nM (SE, 0.22 nM), and that of ZA was 0.43 nM (SE, 0.099 nM) (Fig. 2).
FIG 2.
Inhibition of early and late samples of the mutated A/51833/H274Y virus and of the original A/51833/wt virus by OC and ZA. Results for early (generations 1 and 2) and late (generation 10) samples are shown as mean IC50 for 8 duplicate samples. The IC50 for the original virus are means from 6 repeated assays. Boxes indicate the 95% CIs of the means, and whiskers indicate minimum and maximum values.
DISCUSSION
In order for a resistant avian IAV to retain its resistance trait when exposed to little or no drug, and hence to circulate in a wild bird population, the virus has to harbor the resistance mutation(s) with no loss of viral fitness. In this in vivo study, when we gradually decreased the level of OC exposure for mallards infected with an OC-resistant avian influenza A (H1N1)/NA-H274Y virus, and finally removed OC altogether, we found no genotypic or phenotypic decrease in resistance and no reversion to wild-type virus. Targeted deep sequencing of the resistance point mutation did not indicate any tendency for the wild-type virus to reemerge when the drug pressure was below the level of induction of the NA-H274Y mutation (0.95 μg/liter [23]) or when OC had been removed. Based on the number of reads and the fact that the wild-type genotype was never more prevalent than the sequencing noise, we can rule out a wild-type subpopulation with a prevalence higher than 1%. By calculations of the mutation frequency per replicative viral cycle (10−5 per site) and the exponential replication in a new host (29), a subpopulation of viruses with substantially superior fitness would already be noticeable when the replication plateau was reached, after 2 days. This time perspective is supported by results from a previous study in this mallard model where the resistant A/51833/H274Y virus emerged rapidly and dominated over the A/51833/wt virus at a high drug pressure (23). The possibility that minimally decreased fitness of the mutant would go unnoticed under our experimental conditions cannot be excluded, but we argue that substantial evolutionary space for reversion was provided. We could not observe any wild-type virus in 10 individuals after 17 days of successive propagation at OC concentrations below the resistance-inducing level (including 14 days and 8 individuals at <10% of the resistance-inducing level), or in 4 individuals after 5 days without OC. Furthermore, the NA-H274Y mutation was retained in all fecal samples through the OC-free propagation process in embryonated chicken eggs, prior to phenotypic testing.
Phenotypic testing confirmed the picture of retained resistance in the A/51833/H274Y virus, with 340-fold lower sensitivity to OC than the A/51833/wt virus, and with no significant difference between early and late samples. This level of OC sensitivity is the same as that observed previously for this mutant (23). Infectivity or transmissibility between mallards, evaluated by fecal shedding of IAV, was not reduced when drug pressure was removed (Fig. 1), and the level of IAV shedding was not lower than that of the original A/51833/wt virus in previous studies (30). Based on the retention of infectivity and transmissibility between mallards, and on the persistence of the resistance mutation without drug pressure, we conclude that viral fitness was not significantly impaired in this NA-H274Y resistant avian influenza A (H1N1) virus.
Permissive or compensatory mutations in an IAV are clearly important for the ability of a virus to harbor a selected resistance mutation (15, 31, 32). Several amino acid variants at NA position 222 can have both permissive and additive effects with NA-H274Y in human influenza A (H1N1) virus (31, 33, 34), and it is possible that the NA-N222 variant in this avian influenza A (H1N1) virus might have had a permissive function for the acquisition and retention of NA-H274Y.
The highest OC concentrations detected in the environment to date (0.86 μg/liter [18]) are lower than the lowest resistance-inducing concentration in the mallard model (0.95 μg/liter [23]) but in the same order of magnitude. Furthermore, occasional peak concentrations may exceed detected levels, especially during pandemics, and different IAVs acquire resistance mutations at different OC exposure levels. Therefore, we believe that OC in water environments should not be ignored as a risk factor for the development of resistant IAVs. The results in this study support the hypothesis that if an avian IAV with a suitable genetic makeup acquires drug resistance during occasional OC exposure in the environment, it may retain the resistance in periods without drug pressure, i.e., between influenza outbreaks. The release of active anti-influenza drugs to aquatic environments might thus contribute to the evolution of resistant circulating avian IAV strains that are potentially pathogenic to humans. If a pandemic caused by an IAV with inherent oseltamivir resistance were to occur, global stockpiles of Tamiflu (7, 8) would offer a poor response. Our results underscore the need for prudent use of NAIs, for the implementation of modern sewage treatment procedures that degrade drug metabolites (17, 35), and for active NAI resistance surveillance of IAVs in wild birds.
ACKNOWLEDGMENTS
We acknowledge the Swedish Research Council Formas, the Swedish Research Council (Vetenskapsrådet), and the Family Olinder-Nielsen's Foundation for financial support. We also acknowledge the National Genomics Infrastructure (NGI)/Uppsala Genome Center and UPPMAX for providing assistance in massive parallel sequencing and computational infrastructure. Work performed at the NGI/Uppsala Genome Center has been funded by RFI/VR and Science for Life Laboratory, Sweden.
Susanne Bloemberg and the rest of the staff at the animal facility of the National Veterinary Institute, Uppsala, Sweden, are gratefully acknowledged for excellent animal care. F. Hoffman-La Roche Ltd. is acknowledged for providing OC, including the deuterium-labeled isotope.
REFERENCES
- 1.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. 1992. Evolution and ecology of influenza A viruses. Microbiol Rev 56:152–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olsen B, Munster VJ, Wallensten A, Waldenström J, Osterhaus AD, Fouchier RA. 2006. Global patterns of influenza A virus in wild birds. Science 312:384–388. doi: 10.1126/science.1122438. [DOI] [PubMed] [Google Scholar]
- 3.Brockwell-Staats C, Webster RG, Webby RJ. 2009. Diversity of influenza viruses in swine and the emergence of a novel human pandemic influenza A (H1N1). Influenza Other Respir Viruses 3:207–213. doi: 10.1111/j.1750-2659.2009.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Latorre-Margalef N, Gunnarsson G, Munster VJ, Fouchier RA, Osterhaus AD, Elmberg J, Olsen B, Wallensten A, Haemig PD, Fransson T, Brudin L, Waldenström J. 2009. Effects of influenza A virus infection on migrating mallard ducks. Proc Biol Sci 276:1029–1036. doi: 10.1098/rspb.2008.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dugan VG, Chen R, Spiro DJ, Sengamalay N, Zaborsky J, Ghedin E, Nolting J, Swayne DE, Runstadler JA, Happ GM, Senne DA, Wang R, Slemons RD, Holmes EC, Taubenberger JK. 2008. The evolutionary genetics and emergence of avian influenza viruses in wild birds. PLoS Pathog 4:e1000076. doi: 10.1371/journal.ppat.1000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu D, Shi W, Shi Y, Wang D, Xiao H, Li W, Bi Y, Wu Y, Li X, Yan J, Liu W, Zhao G, Yang W, Wang Y, Ma J, Shu Y, Lei F, Gao GF. 2013. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: phylogenetic, structural, and coalescent analyses. Lancet 381:1926–1932. doi: 10.1016/S0140-6736(13)60938-1. [DOI] [PubMed] [Google Scholar]
- 7.Patel A, Gorman SE. 2009. Stockpiling antiviral drugs for the next influenza pandemic. Clin Pharmacol Ther 86:241–243. doi: 10.1038/clpt.2009.142. [DOI] [PubMed] [Google Scholar]
- 8.Wan Po AL, Farndon P, Palmer N. 2009. Maximizing the value of drug stockpiles for pandemic influenza. Emerg Infect Dis 15:1686–1687. doi: 10.3201/eid1510.090844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. 2012. Meetings of the WHO working group on surveillance of influenza antiviral susceptibility—Geneva, November 2011 and June 2012. Wkly Epidemiol Rec 87:369–374. [PubMed] [Google Scholar]
- 10.Samson M, Pizzorno A, Abed Y, Boivin G. 2013. Influenza virus resistance to neuraminidase inhibitors. Antiviral Res 98:174–185. doi: 10.1016/j.antiviral.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Kiso M, Mitamura K, Sakai-Tagawa Y, Shiraishi K, Kawakami C, Kimura K, Hayden FG, Sugaya N, Kawaoka Y. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759–765. doi: 10.1016/S0140-6736(04)16934-1. [DOI] [PubMed] [Google Scholar]
- 12.de Jong MD, Tran TT, Truong HK, Vo MH, Smith GJ, Nguyen VC, Bach VC, Phan TQ, Do QH, Guan Y, Peiris JS, Tran TH, Farrar J. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N Engl J Med 353:2667–2672. doi: 10.1056/NEJMoa054512. [DOI] [PubMed] [Google Scholar]
- 13.Hu Y, Lu S, Song Z, Wang W, Hao P, Li J, Zhang X, Yen HL, Shi B, Li T, Guan W, Xu L, Liu Y, Wang S, Zhang X, Tian D, Zhu Z, He J, Huang K, Chen H, Zheng L, Li X, Ping J, Kang B, Xi X, Zha L, Li Y, Zhang Z, Peiris M, Yuan Z. 2013. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 381:2273–2279. doi: 10.1016/S0140-6736(13)61125-3. [DOI] [PubMed] [Google Scholar]
- 14.Moscona A. 2009. Global transmission of oseltamivir-resistant influenza. N Engl J Med 360:953–956. doi: 10.1056/NEJMp0900648. [DOI] [PubMed] [Google Scholar]
- 15.Butler J, Hooper KA, Petrie S, Lee R, Maurer-Stroh S, Reh L, Guarnaccia T, Baas C, Xue L, Vitesnik S, Leang SK, McVernon J, Kelso A, Barr IG, McCaw JM, Bloom JD, Hurt AC. 2014. Estimating the fitness advantage conferred by permissive neuraminidase mutations in recent oseltamivir-resistant A(H1N1)pdm09 influenza viruses. PLoS Pathog 10:e1004065. doi: 10.1371/journal.ppat.1004065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fick J, Lindberg RH, Tysklind M, Haemig PD, Waldenström J, Wallensten A, Olsen B. 2007. Antiviral oseltamivir is not removed or degraded in normal sewage water treatment: implications for development of resistance by influenza A virus. PLoS One 2:e986. doi: 10.1371/journal.pone.0000986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghosh GC, Nakada N, Yamashita N, Tanaka H. 2010. Occurrence and fate of oseltamivir carboxylate (Tamiflu) and amantadine in sewage treatment plants. Chemosphere 81:13–17. doi: 10.1016/j.chemosphere.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 18.Takanami R, Ozaki H, Giri RR, Taniguchi S, Hayashi S. 2010. Detection of antiviral drugs oseltamivir phosphate and oseltamivir carboxylate in Neya River, Osaka, Japan. J Water Environ Technol 8:363–372. doi: 10.2965/jwet.2010.363. [DOI] [Google Scholar]
- 19.Söderström H, Järhult JD, Olsen B, Lindberg RH, Tanaka H, Fick J. 2009. Detection of the antiviral drug oseltamivir in aquatic environments. PLoS One 4:e6064. doi: 10.1371/journal.pone.0006064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Azuma T, Nakada N, Yamashita N, Tanaka H. 2012. Synchronous dynamics of observed and predicted values of anti-influenza drugs in environmental waters during a seasonal influenza outbreak. Environ Sci Technol 46:12873–12881. doi: 10.1021/es303203c. [DOI] [PubMed] [Google Scholar]
- 21.Järhult JD. 21 June 2012. Oseltamivir (Tamiflu®) in the environment, resistance development in influenza A viruses of dabbling ducks and the risk of transmission of an oseltamivir-resistant virus to humans—a review. Infect Ecol Epidemiol 2:10.3402/iee.v2i0.18385. doi: 10.3402/iee.v2i0.18385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monto AS, Webster RG. 2013. Influenza pandemics: history and lessons learned, p 20–34. In Webster RG, Monto AS, Braciale TJ, Lamb RA (ed), Textbook of influenza, 2nd ed. John Wiley & Sons, Ltd, Oxford, United Kingdom. [Google Scholar]
- 23.Järhult JD, Muradrasoli S, Wahlgren J, Söderström H, Orozovic G, Gunnarsson G, Bröjer C, Latorre-Margalef N, Fick J, Grabic R, Lennerstrand J, Waldenström J, Lundkvist A, Olsen B. 2011. Environmental levels of the antiviral oseltamivir induce development of resistance mutation H274Y in influenza A/H1N1 virus in mallards. PLoS One 6:e24742. doi: 10.1371/journal.pone.0024742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillman A, Muradrasoli S, Söderström H, Nordh J, Bröjer C, Lindberg RH, Latorre-Margalef N, Waldenström J, Olsen B, Järhult JD. 2013. Resistance mutation R292K is induced in influenza A(H6N2) virus by exposure of infected mallards to low levels of oseltamivir. PLoS One 8:e71230. doi: 10.1371/journal.pone.0071230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Achenbach JE, Bowen RA. 2013. Effect of oseltamivir carboxylate consumption on emergence of drug-resistant H5N2 avian influenza virus in mallard ducks. Antimicrob Agents Chemother 57:2171–2181. doi: 10.1128/AAC.02126-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am J Hyg 27:493–497. [Google Scholar]
- 27.Spackman E, Suarez DL. 2008. Type A influenza virus detection and quantitation by real-time RT-PCR. Methods Mol Biol 436:19–26. doi: 10.1007/978-1-59745-279-3_4. [DOI] [PubMed] [Google Scholar]
- 28.Potier M, Mameli L, Belisle M, Dallaire L, Melancon SB. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-α-d-N-acetylneuraminate) substrate. Anal Biochem 94:287–296. doi: 10.1016/0003-2697(79)90362-2. [DOI] [PubMed] [Google Scholar]
- 29.Russell CA, Fonville JM, Brown AE, Burke DF, Smith DL, James SL, Herfst S, van Boheemen S, Linster M, Schrauwen EJ, Katzelnick L, Mosterin A, Kuiken T, Maher E, Neumann G, Osterhaus AD, Kawaoka Y, Fouchier RA, Smith DJ. 2012. The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 336:1541–1547. doi: 10.1126/science.1222526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bröjer C, Järhult JD, Muradrasoli S, Söderström H, Olsen B, Gavier-Widen D. 2013. Pathobiology and virus shedding of low-pathogenic avian influenza virus (A/H1N1) infection in mallards exposed to oseltamivir. J Wildl Dis 49:103–113. doi: 10.7589/2011-11-335. [DOI] [PubMed] [Google Scholar]
- 31.Bloom JD, Gong LI, Baltimore D. 2010. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328:1272–1275. doi: 10.1126/science.1187816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duan S, Govorkova EA, Bahl J, Zaraket H, Baranovich T, Seiler P, Prevost K, Webster RG, Webby RJ. 2014. Epistatic interactions between neuraminidase mutations facilitated the emergence of the oseltamivir-resistant H1N1 influenza viruses. Nat Commun 5:5029. doi: 10.1038/ncomms6029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pizzorno A, Abed Y, Bouhy X, Beaulieu E, Mallett C, Russell R, Boivin G. 2012. Impact of mutations at residue I223 of the neuraminidase protein on the resistance profile, replication level, and virulence of the 2009 pandemic influenza virus. Antimicrob Agents Chemother 56:1208–1214. doi: 10.1128/AAC.05994-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang L, Cao Y, Zhou J, Qin K, Zhu W, Zhu Y, Yang L, Wang D, Wei H, Shu Y. 2014. A conformational restriction in the influenza A virus neuraminidase binding site by R152 results in a combinational effect of I222T and H274Y on oseltamivir resistance. Antimicrob Agents Chemother 58:1639–1645. doi: 10.1128/AAC.01848-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Azuma T, Nakada N, Yamashita N, Tanaka H. 2013. Mass balance of anti-influenza drugs discharged into the Yodo River system, Japan, under an influenza outbreak. Chemosphere 93:1672–1677. doi: 10.1016/j.chemosphere.2013.05.025. [DOI] [PubMed] [Google Scholar]