Abstract
Background:
VAP is defined as pneumonia in patients who use ventilators. The acute physiology and chronic health evaluation (APACHE II) scoring system was originally developed for predicting mortality in patients who were admitted to the intensive care unit. Due to the complexity, a simpler score called IBMP-10 was developed. We designed the study to confirm and further investigate these two methods.
Materials and Methods:
This cross-sectional and analysis-descriptive study was done at the moment of VAP diagnosis on 60 patients in intensive care units. APACHE II and the IBMP-10 scores were calculated. ROC curves were generated to compare the new prediction rule with the APACHE II score. Results were reported as adjusted odds ratios with 95% confidence intervals (CIs). Analyses were performed using SPSS, version 20 and P values of 0.05 were considered to be statistically significant.
Results:
APACHE II Score means (P < 0.001) and IBMP-10 score (P < 0.001) means had significant increase in Non-survivor patient than in patients who survived. APACHE II can be used as a good prediction measure for mortality rate. In IBMP-10 method, specificity and PPV were greater than APACHE II, but in mc-nemar test, there was no significant difference between the two methods (P = 0.55). Both prediction rules had high NPV. In our study, survivors’ prediction value in APACHE II was 46.7%, and in IBMP-10, it was 46.7%.
Conclusion:
IBMP-10, compared to APACHE II, has greater sensitivity, specificity, and AUC to predict mortality. So the consequence of the use of IBMP-10 was better than APACHE II.
Keywords: Acute Physiology and Chronic Health Evaluation II, immunodeficiency, blood pressure, multilobar infiltrates, platelet count and 10-day hospitalization-10, mortality, scoring system, ventilator-associated pneumonia
INTRODUCTION
Ventilator-associated pneumonia (VAP) is defined as pneumonia in patients who use ventilators.[1,2] The incidence of ventilator-associated nosocomial pneumonia in patients who use ventilators for more than 48 h is between 10% and 30%.[3] Pneumonia is the second most common cause of nosocomial infection in critically ill patients.[4] It infects approximately 27% of these patients. 86% of the hospital-acquired pneumonias are pneumonias associated with the use of ventilators. VAP mortality of about 0–50% has been reported. About 20–60% case fatality rate of this infection has been considered.[5] The prevalence of the disease depends on factors such as the presence of study population or absence of risk factors and preventive measures of the type and severity used in the Intensive Care Unit (ICU). A diagnosis of VAP is difficult, and it still does not have a gold standard. Diagnosing the disease combines clinical and radiological findings. Microbiological criteria have been defined by the center of disease control.[6] These criteria have low sensitivity and specificity. An initial assessment of the patient is an important aspect of treating this type of pneumonia, although many scores for the assessment and prediction of the risk of death for patients with community-acquired pneumonia have been developed.[7,8,9,10] The Acute Physiology and Chronic Health Evaluation II (APACHE II) scoring system was originally developed for predicting mortality in patients who were admitted to the critical care unit. This prediction was also used in other states.[11] specific grading in predicting mortality in patients with VAP does not exist. APACHE II, considered in the diagnosis, is hardly effective due to many problems. Due to many variables used in calculating it, it is unlikely that physicians could use APACHE II as a research tool for scoring the risk of mortality. Due to this complexity, a simpler and more practical score called immunodeficiency, blood pressure, multilobar infiltrates, platelet count and 10-day hospitalization (IBMP-10) was developed. A similar study was conducted, in which two scoring systems of APACHE II and IBMP-10 were compared.[4] The APACHE II area under the curve (AUC) was 0.741, and the IBMP-10 score was 0.824 (P < 0.001) in the study. We designed the following study to confirm and further investigate these two methods.
MATERIALS AND METHODS
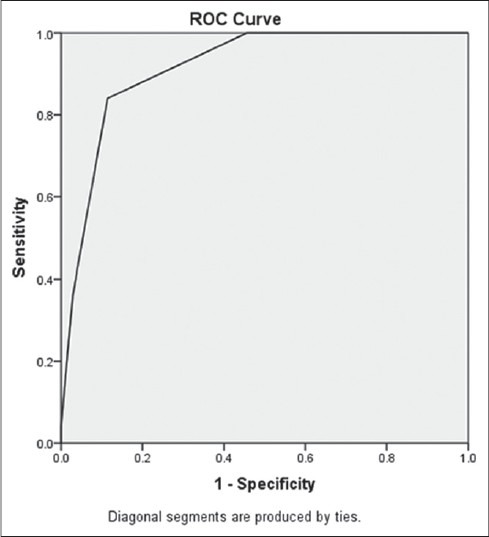
Our study was based on a cross-sectional and analysis-descriptive method. From early 2013 until the end of the sample collection, the location of our study was the ICU at Alzahra Hospital of Isfahan city (center of Iran). At the moment of diagnosis of VAP in ICU's patients, the APACHE II and the IBMP-10 scores were calculated. Patients enrolled in the study after meeting our inclusion criteria, and after the two scoring systems (IBMP-10 and APACHE II) had been evaluated. Scores obtained from each patient were recorded, the patients were monitored, and their mortality rate was determined. After that, sensitivity and specificity were calculated for each method. Receiver operating characteristic (ROC) curves [Figure 1] were generated to compare the new prediction rule with the APACHE II score. Results were reported as adjusted odds ratios with 95% confidence intervals. In this study, McNemar test, analysis of variance, and independent t-test were used. Analyses were performed using SPSS software for Windows, version 20 (SPSS), and P values of 0.05 were considered to be statistically significant.
Figure 1.
Immunodeficiency, blood pressure, multilobar infiltrates, platelet count and 10-day hospitalization
RESULTS
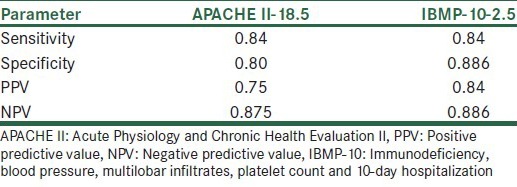
Sixty patients participated in our study (28 females and 32 males). The mean (±standard error) age was 52 ± 19 years (minimum age was 20 and maximum age was 92). Twenty-five (41.6%) patients died in this study. The independent t-test showed that APACHE II score means (P < 0.001), and IBMP score (immunodeficiency, blood pressure [<90 mm Hg], multi-lobar infiltrates [chest X-ray], platelets [<100 × 109/L], hospitalization [<10 days]), before the onset of VAP (P < 0.001) means, had significant increase in nonsurvivor patient than in patients that survived [Table 1]. We used ROC curve for the prediction of APACHE II mortality value [Figures 1 and 2]. From our results, AUC = 0.87% in APACHE II, and AUC = 0.915 in IBMP-10. APACHE II can be used as a good prediction measure for mortality rate. As we see in Table 2, in IBMP-10 method, the specificity and positive predictive values were greater than those in APACHE II, but in McNemar test, there was no significant difference between the two methods (P = 0.55). Both prediction rules had high negative predictive values. In our study, survivors’ prediction value in APACHE II was 46.7%, and in IBMP-10, it was 46.7%.
Table 1.
Comparing two scoring systems before the onset of VAP
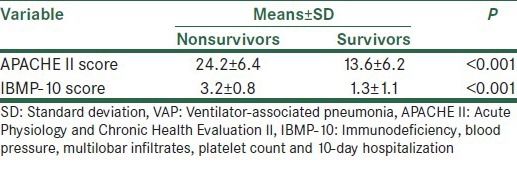
Figure 2.
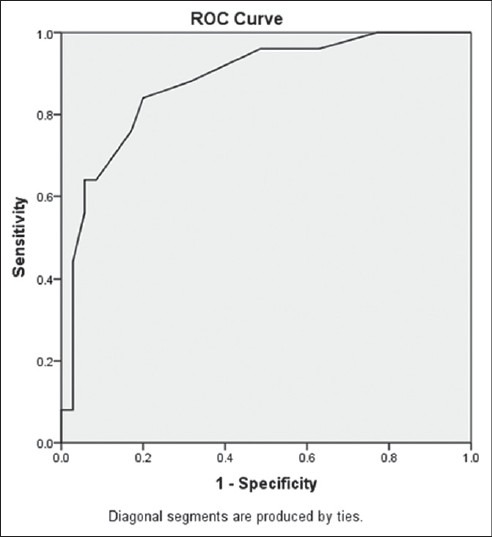
Acute physiology and chronic health evaluation II
Table 2.
Specificity and sensitivity and predictive values in two scoring systems
DISCUSSION
Our study shows that IBMP-10, compared to APACHE II, has greater sensitivity, specificity, and AUC to predict mortality. APACHE II has been designed for more accurate rating of patients’ mortality rate in the ICU. APACHE III and APACHE IV were created due to more precisions in the mortality rate of patients who were hospitalized in ICU.[12] These scores have an important role to play in the research. However, due to the need for complicated and time calculations, they are hard and time-consuming. Another reason why IMBP-10 scoring system was created is because it is easier to work on the mortality rate of hospitalized patients in ICU. This score consists of risk factors such as immunosuppression, hypotension, multi-lobar lung infiltrates, and thrombocytopenia that include VAP. IBMP-10 scoring system consists of (1) immunodeficiency; (2) blood pressure <90 mm Hg (systolic) or <60 mm Hg (diastolic); (3) multi-lobar infiltrates noted on a chest radiograph; (4) platelet count <100,000 platelets/mm3; and (5) duration of hospitalization before the onset of VAP of >10 days. The investigation was made 10 days after admission to ICU; there was a significant difference in patients’ mortality. In a similar study which was conducted by Mirsaeidi et al.[4] IBMP-10 score was compared to that of APACHEII. One hundred and seventy-six patients with VAP have been checked by two systems. The AUC was 0.743 for the APACHE II score and was 0.824 for the IBMP-10 score (P < 0.001). The results of our study are similar too. In another study by Dora E. Wiskirchen, which was conducted between 2004 and 2007, 168 patients were evaluated in a 14-day mortality rate of 15%. The APACHE II and IBMP-10 methods were compared.[13] The IBMP-10 score has been less reliable than APACHE II in patients with VAP. In another study conducted by Gursel and Demirtas, predictive values of APACHEII, SOFA, and CPIS, and in the patients connected to the ventilator, were compared.[10] This study has been a prospective observational cohort which consists of 63 patients. In this study, the mentioned APACHE II can be used to predict mortality more than the other methods.
According to the opposite result of articles in this area, we recommended the designing of a study with bigger sample size in order to increase the accuracy of the study. In our study, we determined that the consequence of the use of IBMP-10 was better than that of APACHEII. IBMP-10 is a strong predictor of mortality than APACHE II method.
ACKNOWLEDGMENTS
This research was supported by a grant (no. 392184) from Isfahan University of Medical Sciences, Isfahan, Iran.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Torres A, Ewig S, Lode H, Carlet J European HAP Working Group. Defining, treating and preventing hospital acquired pneumonia: European perspective. Intensive Care Med. 2009;35:9–29. doi: 10.1007/s00134-008-1336-9. [DOI] [PubMed] [Google Scholar]
- 2.Rea-Neto A, Youssef NC, Tuche F, Brunkhorst F, Ranieri VM, Reinhart K, et al. Diagnosis of ventilator-associated pneumonia: A systematic review of the literature. Crit Care Med. 2008;12:R56. doi: 10.1186/cc6877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torres A, Ferrer M, Badia JR. Treatment guidelines and outcomes of hospital-acquired and ventilator-associated pneumonia. Clin Infect Dis. 2010;51(Suppl 1):S48–53. doi: 10.1086/653049. [DOI] [PubMed] [Google Scholar]
- 4.Mirsaeidi M, Peyrani P, Ramirez JA Improving Medicine through Pathway Assessment of Critical Therapy of Hospital-Acquired Pneumonia (IMPACT-HAP) Investigators. Predicting mortality in patients with ventilator-associated pneumonia: The APACHE II score versus the new IBMP-10 score. Clin Infect Dis. 2009;49:72–7. doi: 10.1086/599349. [DOI] [PubMed] [Google Scholar]
- 5.Tejerina E, Frutos-Vivar F, Restrepo MI, Anzueto A, Abroug F, Palizas F, et al. Incidence, risk factors, and outcome of ventilator-associated pneumonia. J Crit Care. 2006;21:56–65. doi: 10.1016/j.jcrc.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Koenig SM, Truwit JD. Ventilator-associated pneumonia: Diagnosis, treatment, and prevention. Clin Microbiol Rev. 2006;19:637–57. doi: 10.1128/CMR.00051-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauer TT, Ewig S, Marre R, Suttorp N, Welte T CAPNETZ Study Group CRB-65 predicts death from community-acquired pneumonia. J Intern Med. 2006;260:93–101. doi: 10.1111/j.1365-2796.2006.01657.x. [DOI] [PubMed] [Google Scholar]
- 8.Renaud B, Coma E, Labarere J, Hayon J, Roy PM, Boureaux H, et al. Routine use of the pneumonia severity index for guiding the site-of-treatment decision of patients with pneumonia in the emergency department: A multicenter, prospective, observational, controlled cohort study. Clin Infect Dis. 2007;44:41–9. doi: 10.1086/509331. [DOI] [PubMed] [Google Scholar]
- 9.Charles PG, Wolfe R, Whitby M, Fine MJ, Fuller AJ, Stirling R, et al. SMART-COP: A tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis. 2008;47:375–84. doi: 10.1086/589754. [DOI] [PubMed] [Google Scholar]
- 10.Gursel G, Demirtas S. Value of APACHE II, SOFA and CPIS scores in predicting prognosis in patients with ventilator-associated pneumonia. Respiration. 2006;73:503–8. doi: 10.1159/000088708. [DOI] [PubMed] [Google Scholar]
- 11.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 12.Beck DH, Taylor BL, Millar B, Smith GB. Prediction of outcome from intensive care: A prospective cohort study comparing acute physiology and chronic health evaluation II and III prognostic systems in a United Kingdom intensive care unit. Crit Care Med. 1997;25:9–15. doi: 10.1097/00003246-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Wiskirchen DE, Kuti JL, Nicolau DP. Acute physiology and chronic health evaluation II score is a better predictor of mortality than IBMP-10 in patients with ventilator-associated pneumonia. Surg Infect (Larchmt) 2011;12:385–90. doi: 10.1089/sur.2010.096. [DOI] [PubMed] [Google Scholar]


