Abstract
Background:
Immunization remains one of the most important public health interventions and a cost-effective strategy to reduce both the morbidity and mortality associated with infectious diseases. Over two million deaths are delayed through immunization each year worldwide.
Aims:
This study sought to identify specific factors associated with immunization coverage in order to advance improved intervention, policies/strategies therefore raising overall immunization coverage.
Materials and Methods:
A cross-sectional study was conducted among a total of 198 children aged 12-23 months at Urban Health and Training Centre (UHTC), Era's Lucknow Medical College, Lucknow, over a period of 6 months i.e., from July 2012-December 2012. Data were collected, compiled and tabulated using Microsoft Excel and analyzed using SPSS 17.0 version.
Results:
A total of 198 children of age 12-23 months were included in this study, of which 74.7% of children were fully immunized, 11.1% were partially immunized and 14.1% were not immunized at all. The most common reason for partial or non-immunization was family problems (24%) of the respondents followed by lack of knowledge of immunization (20%), and fear of side effects (16%). The odds of risk of partial/non-immunization in illiterate women is 5.78 more than the graduate women (P = 0.039).
Conclusions:
Although in the present study, majority of the children were immunized, it is still not up to the mark. We have to make it 100%, so that we can reduce mortality due to vaccine-preventable diseases. Increasing awareness and reducing fear of side effects of immunization among parents through health education, counseling, etc. can increase the percentage of immunized children.
Keywords: Children, Determinants, Immunization, Mothers, Urban areas
Introduction
Immunization remains one of the most important public health interventions and a cost-effective strategy to reduce both the morbidity and mortality associated with infectious diseases. Over two million deaths are delayed through immunization each year worldwide.[1] Despite this, vaccine-preventable diseases remain the most common cause of childhood mortality with an estimated three million deaths each year.[2] Uptake of vaccination services is dependent not only on provision of these services, but also on other factors including knowledge and attitude of mothers.[3,4]
According to the Global Routine Vaccination Coverage (GAVI) 2010, about 19.3 million children were not fully vaccinated and remained at risk for diphtheria, tetanus and pertussis, and other vaccine-preventable causes of morbidity and mortality, and about 50% of these children are from India, Nigeria, and Congo.[5] The most important indicators mentioned in the Millennium Development Goals (MDGs) are the under-5 mortality rate (U5MR), infant mortality rate (IMR) and proportion of 1-year-old children immunized against measles (P1MV). About one-quarter, or 25%, of under-5 mortality is due to vaccine-preventable diseases.[6]
The World Health Organization (WHO) launched the Expanded Program on Immunization (EPI) in 1974 globally with the focus on prevention of the six childhood vaccine-preventable diseases by the year 2000. This was endorsed by the Government of India in 1978.[7] Later, on November 19, 1985, the Universal Immunization Program (UIP) was introduced in India with the objective to cover at least 85% of all infants by 1990.[8] Further, a national socio-demographic goal was set up in National Population Policy (NPP) 2000 to achieve universal immunization of children against all vaccine-preventable diseases by 2010.[9] In addition, evaluation of immunization coverage provides evidence whether substantial progress toward achieving vaccination targets is being made. Such positive evidence is required for continuing support from donor supported initiatives like the Global Alliance for Vaccines and Immunizations (GAVI).[10]
The current study seeks to determine whether the situation has improved since and to more fully identify risk groups and reasons for under-immunization. This study sought to identify specific factors associated with immunization coverage in order to advance improved intervention, policies/strategies and therefore raising overall immunization coverage.
Materials and Methods
The present study is a cross-sectional study conducted among children aged 12-23 months at Urban Health and Training Centre (UHTC), Era's Lucknow Medical College, Lucknow, for a period of six months i.e., from July 2012 to December 2012.
Sampling technique
The present study was conducted during July 2012 -December 2012. A total of 198 children aged 12-23 months attending outpatient department (OPD) at Urban Health and Training Centre (UHTC), Era's Lucknow Medical College, Lucknow were included in the study. This study was conducted after the ethical clearance from the ethical committee of Era's Lucknow Medical College, Lucknow.
Tools of data collection
The investigating tool used is a preformed, pretested questionnaire. Questions regarding biosocial characteristics and immunization status of the children were asked from the mother accompanying the child. In case the mother was not present, then any other person accompanying the child was interviewed regarding biosocial characteristics and immunization status. As this study was conducted among mothers attending OPD at urban health center, so the immunization status was determined on the basis of mother's recall and record at the urban health center. Definitions of key indicators were taken from NFHS-3, India.
Statistical analysis
Data were collected, compiled and tabulated using Microsoft Excel and analyzed using SPSS 17.0 version for calculation of percentages, and Chi-square test was applied to find out various statistical associations.
Results
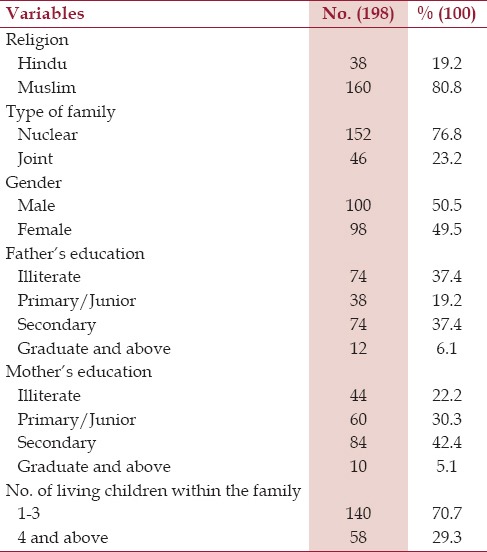
A total of 198 children of 12-23 months of age were included in this study of which 100 were males and 98 were females. Total 80.8% of children were Muslims and 19.2% were Hindus. In all, 76.8% of children belonged to nuclear families and 23.2% belonged to joint families. Parents of most of the children were educated. Only 37.4% of fathers and 22.2% of mothers were illiterate [Table 1].
Table 1.
Socio-demographic characteristics of children between 12-23 months
Among immunized children, majority (83.8%) of the children were delivered at government/private hospital and only 16.2% of the children were delivered at home [Table 2].
Table 2.
Place of birth

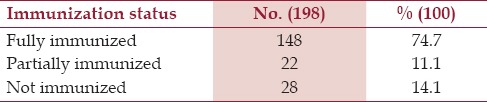
Immunization status was ascertained by mother's recall accompanying the child. In present study 74.7% of children were fully immunized, 11.1% partially immunized and 14.1% were not immunized at all. The percentage of non-immunized children were more among female children (20%) [Table 3].
Table 3.
Immunization status of children between 12-23 months
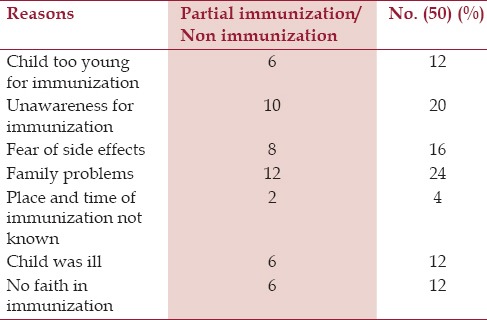
Most common reason for partial or non-immunization was family problems (24%) of the respondents followed by unawareness of immunization (20%), and fear of side effects (16%). Other reasons were child too young for immunization, illness of child and parents have no faith in immunization (12%) [Table 4].
Table 4.
Reasons for partial immunization and non-immunization of the children according to respondents
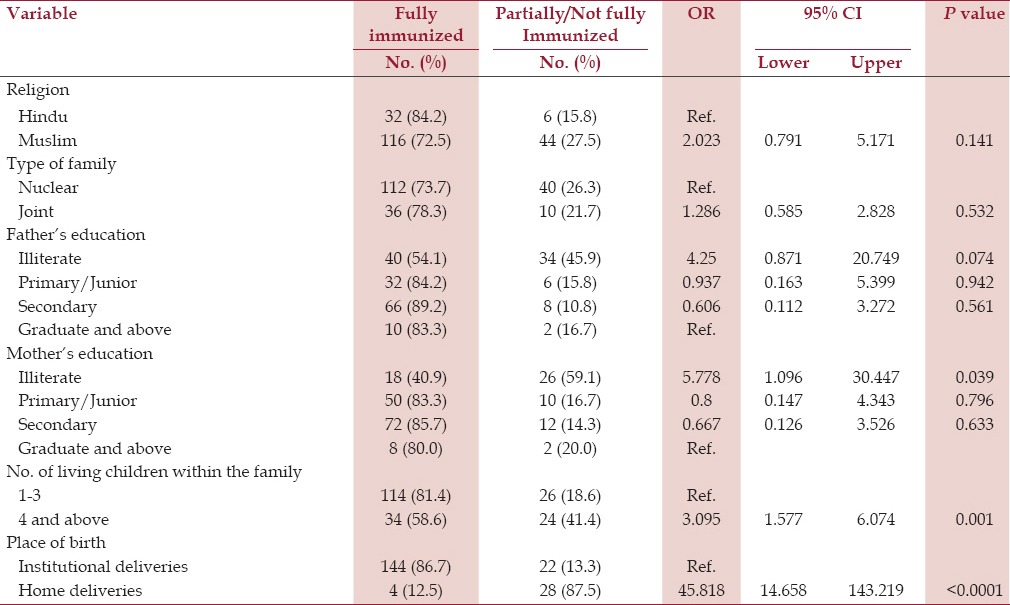
The odds of risk of partial/non-immunization in illiterate women is 5.78 more than the graduate women (P = 0.039). The odds of risk of partial/non-immunization of the families having 4 or more children are 6.074 more than the families having 1-3 children (P < 0.0001). The odds of risk of partial/non-immunization is 45.818 in home deliveries than in institutional deliveries (P = 0.0001) [Table 5].
Table 5.
Immunization status in relation to socio-demographic characteristics of the children
Discussion
In present study, we have tried to find out various reasons responsible for partial or non-immunization and compared it with findings of various other studies. In the present study, 74.7% of children were fully immunized, 11.1% partially immunized and 14.1% were not immunized at all. In a study by Nath et al in Lucknow,[11] only 44.1% of children were completely immunized, which is way less than observed in our study. In a study by Joshi et al.,[12] in Bareilly district, only 50% were fully immunized and 22.5% were non-immunized. In contrast to our findings, as per NFHS-III[13] only 23% children were fully immunized in Uttar Pradesh and 33.6% were not immunized at all. Kar et al.,[14] in their study in a slum of Delhi and Yadav et al.,[15] in the state of Madhya Pradesh reported a higher percentage (above 60%) of fully immunized children, which is similar to our study.
In the present study, the most common reason for partial or non-immunization was family problems (24%) of the respondents followed by unawareness of immunization (20%), and fear of side effects (16%). Other reasons were child too young for immunization, illness of child, and parents having no faith in immunization (12%). In a study by Joshi et al[12], important reasons for non-immunization were lack of awareness in both the urban (28.6%) and rural (78.6%) areas and lack of availability of services in rural areas (87.2%). In a study by Nandan et al.,[16] and Chaturvedi et al[17], non-availability of services was reported to be the single most common reason for non-immunization.
According to another study by Nath et al[11], the commonest reason for the partial immunization of the child was the unavailability of both the parents (17.2%) to fulfill the child's health needs, as they were preoccupied in the livelihood-generation activities. This reflects the unmet needs of the community, which require organization of outreach services on fixed date and timing with prior information to the locality. Other reasons for partial immunization were missing of the dose due to visit to native place/village (14.7%) compared to 23.1% in the study done by Kar et al[14], carelessness (11.7%), apprehensiveness due to sickness of the child or an elder sibling as a result of vaccination (11.7%) and lack of knowledge (10.4% vs. 23.1% by Kar et al[14]).
In the present study, illiteracy was found to be significantly associated with partial or non-immunization. Similarly Nath et al.,[11] also reported that illiteracy of the mother was significantly associated with partial immunization, and this has also been documented in other studies.[18,19] Interestingly in this study, higher illiteracy rate in male compared to female was found, which seems to be unusual according to other studies in India.
Maina et al.,[20] in their study found that maternal education was one of the factors that was significantly associated with immunization coverage. In Kaptembwo, the proportion of fully immunized children of mothers/guardians who had attained secondary school education and above was 81.6%, which is higher than those who had attained primary school education (76.7%) and even those with no formal education (42.9%). Previous studies have shown a significant association between immunization coverage and residing in an area with high levels of maternal/guardian education.[21]
In the present study, children born at home were either non-immunized or partially immunized than those born in hospital. Similar findings were also observed by, Nath et al.[11] Mothers who deliver at home may be non-users of health services in general and have to be targeted for utilization of health services. In a study in Kenya, Maina et al.,[20] found that a child who was delivered in a health facility was 2.26 times more likely to receive full immunization compared to one delivered at home (by self) or by a traditional birth attendant. Other investigators have also found similar associations between the place of birth of the child and immunization.[22] In the present study, high birth order is significantly associated with risk of partial or non-immunization. Similar findings were also observed by Nath et al.,[11] in their study. In this study, participants have been recruited among health services users who have better vaccination status compared to the whole population. This was the limitation for the study as well for the comparability with population or community-based studies.
Conclusion
Although in the present study, a majority of the children were immunized, it is still not up to the mark. We have to make it 100%, so that we can reduce mortality due to vaccine-preventable diseases. Increasing awareness and reducing fear of side effects of immunization among parents through health education, counseling, etc. can increase the percentage of immunized children. Making immunization services easily available to beneficiaries is again an important aspect for increasing immunization among children. There is need to strengthen communication, education and information skills of health workers to improve service provision and health education among mothers/guardians. The surveillance and referral systems in the area also need reinforcing so as to identify defaulters of immunization and reduce the drop-out rate.
Acknowledgment
We thank all the members of management committee and staff of Era's Lucknow Medical College, Lucknow, UP, India, and the patients attending OPD at UHTC for their support throughout the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.World Health Organization (WHO) Immunization, vaccines and biologicals [Google Scholar]
- 2.Washington DC: Centre for Global Development; 2005. Centre for Global Development. Making Markets for vaccines: From ideas to actions. [Google Scholar]
- 3.Matsumura T, Nakayama T, Okamoto S, Ito H. Measles vaccine coverage and factors related to uncompleted vaccination among 18-month-old and 36-month-old children in Kyoto, Japan. BMC Public Health. 2005;5:59. doi: 10.1186/1471-2458-5-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torun SD, Bakirci N. Vaccination coverage and reasons for non-vaccination in a district of Istanbul. BMC Public Health. 2006;6:125. doi: 10.1186/1471-2458-6-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centre for Disease Control and Prevention (CDC) Global Routine Vaccination Coverage, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1520–2. [PubMed] [Google Scholar]
- 6.Kalaivani K, Mathiyazhagan T, Patro BC. Editorial. News Lett Nat Inst Hlth Fam Welfare. 2006;8:1–2. [Google Scholar]
- 7.Park K. Principles of epidemiology and epidemiologic methods. Text Book of Preventive and Social Medicine Jabalpur, India. 2005:103. [Google Scholar]
- 8.Chapter VI. New Delhi: Ministry of Health and family Welfare; 1992-93. Annual report; p. 2. [Google Scholar]
- 9.New Delhi: Government of India; 2000. National Population policy 2000, Ministry of Health and Family Welfare. [Google Scholar]
- 10.Brugha R, Starling M, Walt G. GAVI, the first steps: Lessons for the Global Fund. Lancet. 2002;359:435–8. doi: 10.1016/S0140-6736(02)07607-9. [DOI] [PubMed] [Google Scholar]
- 11.Nath B, Singh JV, Awasthi S, Bhushan V, Kumar V, Singh SK. A study on determinants of immunization coverage among 12-23 months old children in urban slums of Lucknow district, India. Indian J Med Sci. 2007;61:598–606. [PubMed] [Google Scholar]
- 12.Joshi HS, Gupta R, Singh A, Mahajan V. Assessment of immunization status of children between 12-23 months in Bareilly District. Nepal J Epidemiol. 2011;1:47–50. [Google Scholar]
- 13.National Family Health Survey (NFHS-3) India, Mumbai: Key Findings, IIPS; 2005-06. International Institute for Population Sciences (IIPS) and Macro International. 2007. [Google Scholar]
- 14.Kar M, Reddaiah VP, Kant S. Primary immunization status of children in slum areas of South Delhi — The challenge of reaching the urban poor. Indian J Community Med. 2001;26:151–4. [Google Scholar]
- 15.Yadav JR, Singh P. Immunization status of children and mothers in the state of Madhya Pradesh. Indian J Community Med. 2004;29:147–8. [Google Scholar]
- 16.Nandan D, Dabral SB. Agra: SN Medical College; 1995-96. Report-Multi Indicator Rapid Assessment Survey, Uttar Pradesh -District Etah, Mathura and Almorah Department of SPM. [Google Scholar]
- 17.Chaturvedi M, Nandan D, Gupta SC. Rapid assessment of immunization practices in Agra District. Indian J Public Health. 2007;51:132–4. [PubMed] [Google Scholar]
- 18.Singh P, Yadav RJ. Immunization status of children of India. Indian Pediatr. 2000;37:1194–9. [PubMed] [Google Scholar]
- 19.Suresh K, Saxena D. Trends and determinants of immunization coverage in India. J Indian Med Assoc. 2000;98:10–4. [PubMed] [Google Scholar]
- 20.Maina LC, Karanja S, Kombich J. Immunization coverage and its determinants among children aged 12-23 months in a peri-urban area of Kenya. Pan Afr Med J. 2013;14:3. doi: 10.11604/pamj.2013.14.3.2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kamau N, Esamai FO. Determinants of immunization coverage among children in Mathare Valley, Nairobi. East Afr Med J. 2001;78:590–4. doi: 10.4314/eamj.v78i11.8949. [DOI] [PubMed] [Google Scholar]
- 22.Jani JV, De-Schacht C, Jani IV, Bjune G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health. 2008;8:161. doi: 10.1186/1471-2458-8-161. [DOI] [PMC free article] [PubMed] [Google Scholar]


