Abstract
Objectives. We investigated the association between posttraumatic stress disorder (PTSD) and incident heart failure in a community-based sample of veterans.
Methods. We examined Veterans Affairs Pacific Islands Health Care System outpatient medical records for 8248 veterans between 2005 and 2012. We used multivariable Cox regression to estimate hazard ratios and 95% confidence intervals for the development of heart failure by PTSD status.
Results. Over a mean follow-up of 7.2 years, veterans with PTSD were at increased risk for developing heart failure (hazard ratio [HR] = 1.47; 95% confidence interval [CI] = 1.13, 1.92) compared with veterans without PTSD after adjustment for age, gender, diabetes, hyperlipidemia, hypertension, body mass index, combat service, and military service period. Additional predictors for heart failure included age (HR = 1.05; 95% CI = 1.03, 1.07), diabetes (HR = 2.54; 95% CI = 2.02, 3.20), hypertension (HR = 1.87; 95% CI = 1.42, 2.46), overweight (HR = 1.72; 95% CI = 1.25, 2.36), obesity (HR = 3.43; 95% CI = 2.50, 4.70), and combat service (HR = 4.99; 95% CI = 1.29, 19.38).
Conclusions. Ours is the first large-scale longitudinal study to report an association between PTSD and incident heart failure in an outpatient sample of US veterans. Prevention and treatment efforts for heart failure and its associated risk factors should be expanded among US veterans with PTSD.
Posttraumatic stress disorder (PTSD) is a psychiatric illness that affects approximately 7.7 million Americans aged older than 18 years.1 PTSD typically results after the experience of severe trauma, and veterans are at elevated risk for the disorder. The National Vietnam Veterans Readjustment Study reported the prevalence of PTSD among veterans who served in Vietnam as 15.2% among men and 8.1% among women.2 In fiscal year 2009, nearly 446 045 Veterans Administration (VA) patients had a primary diagnosis of PTSD, a threefold increase since 1999.3 PTSD is of growing clinical concern as evidence continues to link psychiatric illnesses to conditions such as arthritis,4 liver disease,5 digestive disease,6 and cancer.6 When the postwar health status of Vietnam veterans was examined, those with PTSD had higher rates of diseases of the circulatory, nervous, digestive, musculoskeletal, and respiratory systems.7
The evidence linking PTSD to coronary heart disease (CHD) is substantial.8–10 Veterans with PTSD are significantly more likely to have abnormal electrocardiograph results, myocardial infarctions, and atrioventricular conduction deficits than are veterans without PTSD.11 In a study of 605 male veterans of World War II and the Korean War, CHD was more common among veterans with PTSD than among those without PTSD.12 Worldwide, adults exposed to the disaster at Chernobyl experienced increased rates of CHD up to 10 years after the event,13 and studies of stressors resulting from the civil war in Lebanon found elevated CHD mortality.14,15
Although the exact biological mechanism by which PTSD contributes to CHD remains unclear, several hypotheses have been suggested, including autonomic nervous system dysfunction,16 inflammation,17 hypercoagulability,18 cardiac hyperreactivity,19 altered neurochemistry,20 and co-occurring metabolic syndrome.16 One of the hallmark symptoms of PTSD is hyperarousal,21 and the neurobiological changes brought on from sustained sympathetic nervous system activation affect the release of neurotransmitters and endocrine function.22 These changes have negative effects on the cardiovascular system, including increased blood pressure, heart rate, and cardiac output.22,23
Most extant literature to date examining cardiovascular sequelae has shown a positive association between PTSD and coronary artery disease.8–10 Coronary artery disease is well documented as one of the most significant risk factors for future development of heart failure.24 Despite burgeoning evidence for the role of PTSD in the development of coronary artery disease, there are few studies specifically exploring the relationship between PTSD and heart failure. Limited data suggest that PTSD imparts roughly a threefold increase in the odds of developing heart failure in both the general population5 and in a sample of the elderly.25 These investigations, however, have been limited by cross-sectional study design, a small proportion of participants with PTSD, and reliance on self-reported measures for both PTSD and heart failure.5,25 Heart failure is a uniquely large public health issue, as nearly 5 million patients in the United States are affected and there are approximately 500 000 new cases each year.26 Identifying predictors of heart failure can aid in early detection efforts while simultaneously increasing understanding of the mechanism behind development of heart failure.
To mitigate the limitations of previous investigations, we undertook a large-scale prospective study to further elucidate the role of prevalent PTSD and development of incident heart failure among veterans, while controlling for service-related and clinical covariates. Many studies investigating heart failure have relied on inpatient records; we leveraged outpatient records to more accurately reflect the community burden of disease.
METHODS
The Veterans Affairs Pacific Islands Health Care System (VAPIHCS) spans an area of 4.8 million square miles, from Hawaii in the east to Guam in the west, and serves approximately 130 000 veterans. We first examined VAPIHCS outpatient administrative records to assemble an appropriate cohort of eligible veterans for study. We identified all veterans who had received care prior to January 1, 2002, yielding 43 286 records. We then identified veterans with more than 1 visit between January 1, 2002, and December 31, 2004. We queried data from this period for 2 reasons: (1) to ensure that study participation was restricted to veterans receiving continuous care in the VAPIHCS system prior to the study start and (2) to ascertain baseline assessment data. We used the 2-year assessment period to determine each eligible veteran’s most proximal VAPIHCS visit before our study start date of January 1, 2005; data from this visit were our baseline data. Among this group, we included individuals who were at least 45 years of age as of January 1, 2005, but no older than 89 years at the study’s conclusion (December 31, 2012). To ensure that all cases of heart failure in our study were incident cases, we excluded all veterans with a diagnosis of heart failure in the VAPIHCS record as of baseline assessment. To prevent inclusion of veterans who already had heart failure before they developed PTSD, we excluded any veteran with an heart failure diagnosis antedating the PTSD diagnosis. We employed an 8-year follow-up period (January 1, 2005 to December 31, 2012) for the ascertainment of heart failure.
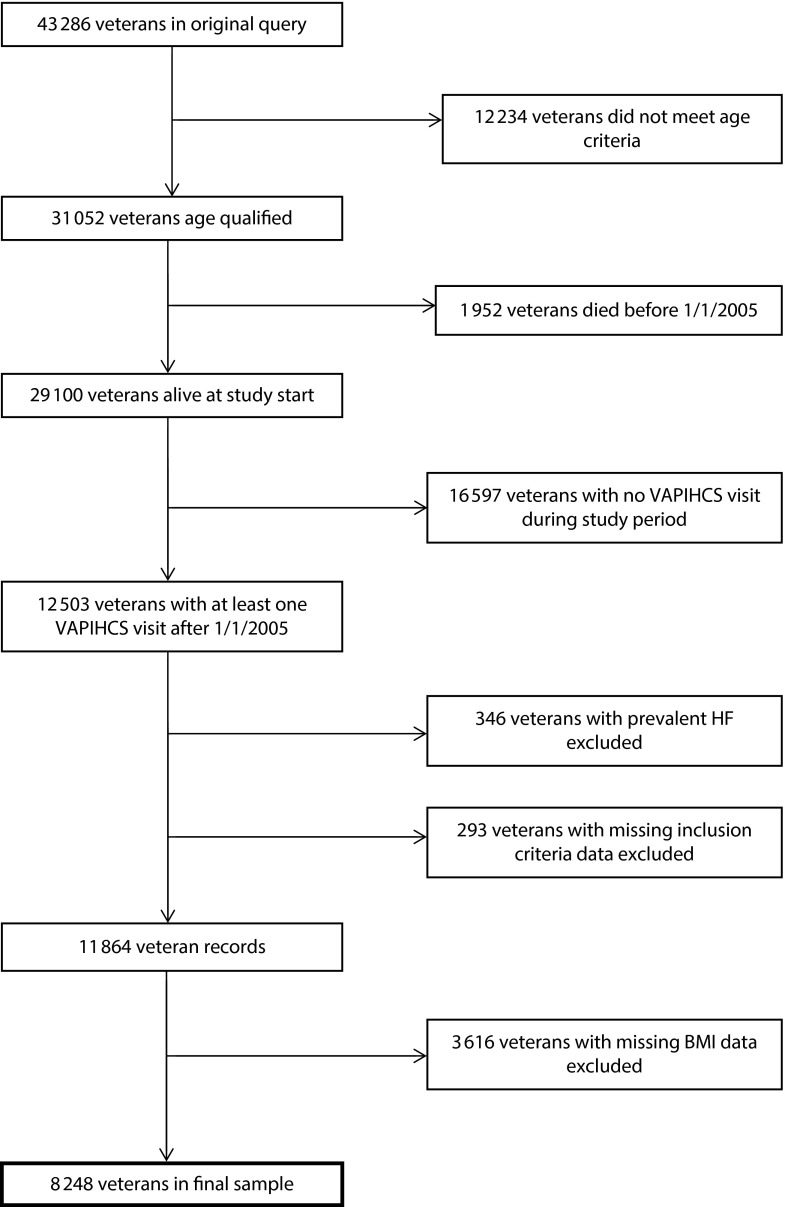
Application of these inclusion and exclusion criteria resulted in a preliminary sample of 11 864 veterans (Figure 1). We further excluded 3616 veterans with missing values for body mass index (BMI; defined as weight in kilograms divided by height in meters squared), because BMI has been consistently shown to predict heart failure.27–29 Applying these exclusion criterion yielded a final sample of 8248 veterans (Figure 1).
FIGURE 1—
Participant flow diagram of US veterans seen at the Veterans Affairs Pacific Islands Health Care System, 2005–2012.
Note. BMI = body mass index; HF = heart failure; VAPIHCS = Veterans Affairs Pacific Islands Health Care System.
Measures
The primary outcome was incident heart failure, operationalized as the first heart failure diagnosis recorded in the veteran’s administrative record. We used International Classification of Diseases, Ninth Revision (ICD-9)30 codes to define an outpatient diagnosis of heart failure (Table A, available as a supplement to the online version of this article at http://www.ajph.org). To classify PTSD status, we obtained VAPIHCS records of all outpatient visits yielding a PTSD diagnostic code (ICD-9 309.81), and we considered the first occurrence as a proxy for PTSD diagnosis date.
We identified comorbid conditions from the outpatient administrative record at baseline (most proximal VAPIHCS visit before January 1, 2005). We included conditions that were (1) associated with heart failure (age, BMI, diabetes, hyperlipidemia, and hypertension), (2) associated with PTSD (depression adjustment disorder and anxiety disorder), and (3) associated with both heart failure and PTSD (tobacco use and substance use disorder). (Associated diagnosis codes are listed in Table A.) Using American Heart Association guidelines, we classified veterans as normal weight (BMI < 25.0), overweight (BMI = 25.0–29.9), or obese (BMI ≥ 30.0).31 We additionally collected information on veterans’ medications for comorbid conditions as of study baseline (for related medication classes, see Table A). We categorized medications by the VA Drug Class Code.
We classified veterans as married or not married on the basis of the most recent marital status indicated in the medical record. We used marital status as a proxy for social support, given increasing evidence for the role of sociodemographic variables in both PTSD32 and CHD.33 We also assessed variables related to veterans’ military time, such as combat service (yes or no) and period of military service. Combat service has been shown to be related to PTSD in veterans,34 and we used period of military service to further characterize the population. We classified veterans chronologically by service period; the earliest conflict represented in our sample was World War II and the most recent was the Persian Gulf Wars.
Time-to-Event Analyses
We calculated time at risk for heart failure as of January 1, 2005. We estimated hazard ratios and 95% confidence intervals for the association between PTSD and heart failure using a Cox proportional hazards model. We censored observations at the time of an heart failure diagnosis, at the time of death, or at study end for those who did not develop heart failure or die. We assessed the proportional hazards assumption for each predictor to determine that the relative risk of heart failure between veterans with PTSD and veterans without PTSD remained constant over time. We used backward selection for multivariable regression, with a P value cutoff of .05 for variable selection. We chose backward selection over more manual variable inclusion methods in an attempt to isolate significant associations with heart failure and evaluate the effect of PTSD within that framework. We evaluated tobacco use and substance use as potential effect measure modifiers in the analyses, as they can be both a predictor35 and outcome36 (for associated ICD-9 codes, see Table A). We created interaction terms and used a likelihood ratio test to assess the statistical significance of the interaction terms, and used a P value cutoff of .2 for variable selection.37
We conducted 3 sensitivity analyses to assess the limitations of our data. The first was to determine the effect of a PTSD diagnosis during the study period. Although the number of veterans with PTSD diagnosed after baseline was a small fraction of the total sample (5%), these veterans represented roughly one quarter of the PTSD group. Thus, we excluded veterans with PTSD diagnoses occurring after the study baseline to determine whether there was a substantive change in the direction or magnitude of the observed associations. Next, we ran a posthoc analysis with a broader definition for comorbid illnesses. To achieve this, we identified the comorbid illnesses (i.e., diabetes, hypertension, hyperlipidemia, depression, anxiety disorder, and adjustment disorder) by the presence of either a diagnosis in the outpatient medical record or pharmaceutical treatment of each illness. This allowed us to examine our data in a more clinically relevant, yet less specific, context. We assessed this sensitivity analysis for a meaningful change in the direction or magnitude of the observed associations. Finally, we conducted analyses to determine the potential effect of multicollinearity between predictive variables.
RESULTS
A total of 8248 veterans were followed for an average of 2633 days (7.2 years), and 1712 (20.8%) were diagnosed with PTSD. Table 1 shows the baseline characteristics of veterans with and without diagnosed PTSD. Compared with veterans without PTSD, veterans with PTSD were more likely to have experienced combat service (20.6% vs 8.4%), comorbid depression (24.8% vs 6.9%), anxiety (14.8% vs 2.7%), adjustment disorders (21.7% vs 4.7%), tobacco use (32.0% vs 12.9%), and substance use (33.5% vs 13.3%). Differences between the 2 groups in terms of biological risk factors of heart failure (such as diabetes, hyperlipidemia, and hypertension) were modest in comparison (Table 1).
TABLE 1—
Baseline Characteristics of US Veterans Seen at the Veterans Affairs Pacific Islands Health Care System, 2005–2012
| Characteristic | No PTSD (n = 6536), Mean ±SD or No. (%) | PTSD (n = 1712), Mean ±SD or No. (%) | P |
| Age, y | 65 ±11.1 | 59 ±8.0 | < .001 |
| Male | 6238 (95.4) | 1640 (95.8) | .53 |
| Race | < .001 | ||
| White | 917 (14.0) | 422 (24.6) | |
| Asian | 1256 (19.2) | 472 (27.6) | |
| Black, non-Hispanic | 98 (1.5) | 34 (2.0) | |
| White, Hispanic | 33 (0.5) | 12 (0.7) | |
| Native American | 40 (0.6) | 2 (0.1) | |
| Black, Hispanic | 7 (0.1) | 4 (0.2) | |
| Missing | 4185 (64.0) | 766 (44.7) | |
| Body mass index | < .001 | ||
| Normal | 1993 (30.5) | 427 (24.9) | |
| Overweight | 2571 (39.3) | 656 (38.3) | |
| Obese | 1972 (30.2) | 629 (36.7) | |
| Married | 3837 (58.7) | 877 (51.2) | < .001 |
| Diabetesa | .48 | ||
| Diagnosis | 885 (13.5) | 243 (14.2) | |
| Diagnosis or medication | 1166 (17.8) | 293 (17.1) | |
| Hypertensiona | < .001 | ||
| Diagnosis | 3984 (61.0) | 954 (55.7) | |
| Diagnosis or medication | 4253 (65.1) | 1115 (65.1) | |
| Hyperlipidemiaa | .055 | ||
| Diagnosis | 3170 (48.5) | 875 (51.1) | |
| Diagnosis or medication | 3337 (51.1) | 910 (53.3) | |
| Depressiona | < .001 | ||
| Diagnosis | 452 (6.9) | 425 (24.8) | |
| Diagnosis or medication | 452 (6.9) | 425 (24.8) | |
| Adjustment disordera | < .001 | ||
| Diagnosis | 306 (4.7) | 371 (21.7) | |
| Diagnosis or medication | 306 (4.7) | 371 (21.7) | |
| Anxiety disordera | < .001 | ||
| Diagnosis | 178 (2.7) | 253 (14.8) | |
| Diagnosis or medication | 580 (8.9) | 560 (32.7) | |
| Period of service | < .001 | ||
| World War II | 902 (13.8) | 64 (3.7) | |
| Korean War | 1122 (17.2) | 103 (6.0) | |
| Post-Korean War | 506 (7.7) | 22 (1.3) | |
| Vietnam era | 2659 (40.7) | 1260 (73.6) | |
| Post-Vietnam War | 819 (12.5) | 131 (7.7) | |
| Persian Gulf | 456 (7.0) | 127 (7.4) | |
| Other or unknown | 72 (1.1) | 5 (0.3) | |
| Combat service indicated | 549 (8.4) | 352 (20.6) | < .001 |
| Smoker | 843 (12.9) | 547 (32.0) | < .001 |
| Substance use disorder | 869 (13.3) | 573 (33.5) | < .001 |
Note. PTSD = posttraumatic stress disorder.
P value represents test of diagnosis.
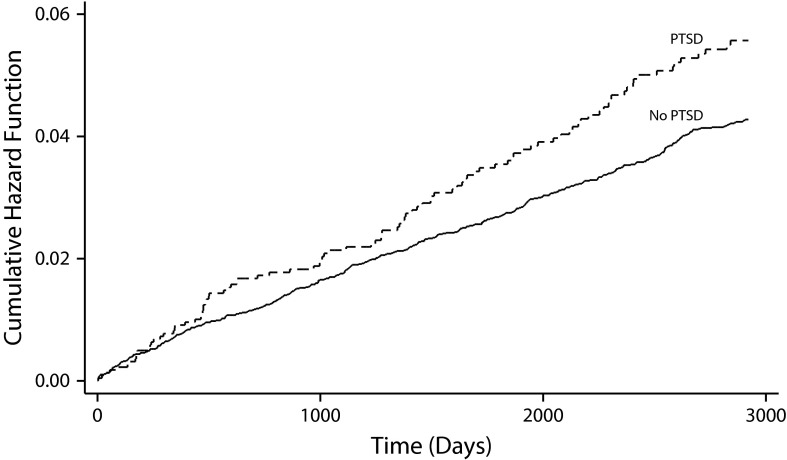
Over the study period, 371 veterans (4.5%) developed heart failure: 287 cases among veterans without PTSD and 84 cases among veterans with PTSD. Figure 2 shows the Nelson–Aalen estimated cumulative hazard function for heart failure in each group. The log-rank test indicated a difference between the PTSD and non-PTSD groups that was not statistically significant (χ21 = 1.88; P = .17).
FIGURE 2—
Estimated cumulative hazard of heart failure, by PTSD status, among US veterans seen at the Veterans Affairs Pacific Islands Health Care System, 2005–2012.
Note. PTSD = posttraumatic stress disorder; VAPIHCS = Veterans Affairs Pacific Islands Health Care System.
Combat service violated the proportional hazards assumption (χ21 = 7.35; P < .001), indicating that the relative risk of incident heart failure explained by combat service was not constant over the course of follow-up. To correct for this, we included in the model an interaction term between combat service and log time (number of days to heart failure or censoring). After we included this interaction in the model, combat service no longer violated the proportional hazards assumption. Investigation into this violation found that over the course of the study period, veterans with combat service were at higher risk for development of heart failure during the first 5.75 years of follow-up, after which time their risk of heart failure was lower than in veterans without combat service. Effect measure modification of the PTSD– heart failure relationship did not exist because of other variables. The full multivariable model contained PTSD, age, gender, BMI, diabetes, hypertension, hyperlipidemia, period of military service, combat service, and combat service × log time. Over the study period, veterans with PTSD were almost 50% more likely to develop heart failure than veterans without PTSD (hazard ratio [HR] = 1.47; 95% confidence interval [CI] = 1.13, 1.92; Table 2).
TABLE 2—
Adjusted Risk Estimates for Incident Heart Failure Among US Veterans Seen at the Veterans Affairs Pacific Islands Health Care System, 2005–2012
| Characteristic | Risk of Heart Failure (n = 8248), HR (95% CI) |
| Posttraumatic stress disorder | 1.47 (1.13, 1.92) |
| Demographic, clinical, and service characteristics | |
| Age | 1.05 (1.03, 1.07) |
| Male | 1.95 (0.92, 4.15) |
| Diabetes | 2.54 (2.02, 3.20) |
| Hypertension | 1.87 (1.42, 2.46) |
| Hyperlipidemia | 0.82 (0.66, 1.01) |
| Combat service | 4.99 (1.29, 19.38) |
| Period of military service | |
| World War II (Ref) | 1.00 |
| Korean War | 0.71 (0.49, 1.02) |
| Post-Korean War | 0.48 (0.27, 0.85) |
| Vietnam era | 0.89 (0.58, 1.37) |
| Post-Vietnam era | 0.97 (0.52, 1.80) |
| Gulf War | 0.46 (0.20, 1.07) |
| Other | 1.48 (0.73, 3.00) |
| Body mass index | |
| Normal (Ref) | 1.00 |
| Overweight | 1.72 (1.25, 2.36) |
| Obese | 3.43 (2.50, 4.70) |
| Time-varying covariate: combat × log time | 0.73 (0.59, 0.91) |
Note. HR = hazard ratio; CI = confidence interval.
Additional predictors for heart failure (Table 2) included age (HR = 1.05; 95% CI = 1.03, 1.07), diabetes (HR = 2.54; 95% CI = 2.02, 3.20), hypertension (HR = 1.87; 95% CI = 1.42, 2.46), overweight (HR = 1.72; 95% CI = 1.25, 2.36), obesity (HR = 3.43; 95% CI = 2.50, 4.70), and combat service (HR = 4.99; 95% CI = 1.29, 19.38). Although the effect of gender in our model did not reach statistical significance (HR = 1.95; 95% CI = 0.92, 4.15), the estimate suggested that male veterans were at greater risk for developing heart failure were than female veterans.
Our first sensitivity analysis, which excluded veterans diagnosed with PTSD during the study period, resulted in an unstable model in which the standard errors became wildly inflated, resulting in inappropriate coefficient estimates. We believe this occurred primarily because of the increased imbalance in class distribution coupled with thinning of the number of veterans in the PTSD group, as well as the reduction in number of heart failure diagnoses. Our second posthoc analysis, in which we classified comorbid illnesses using either diagnosis or current use of pharmacological therapy for treatment, did not result in any substantive changes to the estimates shown in Table 2. Our final sensitivity analyses investigating possible collinearity between covariates in the model showed that multicollinearity was not an issue in our data. All covariates resulted in a variance inflation factor of less than 2, with the exception of modest factors for age (2.43) and period of military service (2.22).
DISCUSSION
To our knowledge, our longitudinal investigation of the association between PTSD and heart failure in an outpatient sample is the first to investigate this relationship among US veterans. We found that over the course of the study period, the risk of developing heart failure was higher among veterans with PTSD than among veterans without PTSD, even after controlling for known clinical risk factors as well as military-specific factors such as combat service and period of military service.
Our results add to the literature demonstrating that PTSD significantly increases the likelihood of heart failure.5,25 They also reinforce results from several previous studies suggesting that age, gender, hypertension, diabetes, and obesity are important factors in predicting heart failure.38–41 Notably, period of military service was not a significant predictor of heart failure. A cohort effect likely explains the high correlation between age and period of military service (e.g., Vietnam era, World War II). Our finding of a dose–response relationship across categories of BMI is consistent with obesity being a risk factor for development of heart failure.27–29,42 Furthermore, our study suggests that military-specific factors, such as combat exposure, are important predictors to consider when assessing heart failure in veterans. Although the hazard of developing heart failure by gender was trending toward significance in our analysis, the heart failure estimate did not reach statistical significance. We believe this was primarily because the sample was mostly male (> 95%). The small number of women in our sample likely reduced our power to detect differences by gender and also precluded our ability to investigate gender as a potential modifier of the association between PTSD and heart failure.
One unexpected finding from our analysis was that hyperlipidemia trended toward being a protective factor. Although this was consistent with findings from the Physicians’ Health Study, in which hyperlipidemia was not a risk factor for incident heart failure,43 we suspect that our estimate for hyperlipidemia may have been biased toward the null because of the inclusion of related factors in the statistical model, such as BMI, hypertension, and diabetes.44 Investigating further, we found that hyperlipidemia was a significant predictor of heart failure when the other related variables were not included in the model.
Our study had many strengths, such as a longitudinal study design, large sample size, and military-specific variables, which allowed for the assessment of confounding by these factors. It also leveraged outpatient data to capture the community burden of heart failure, which likely resulted in the identification of a greater number of less severe cases of heart failure than in a hospital-based inpatient sample. As a result, we may have more accurately captured the time of incident heart failure, our primary outcome. Studies that investigate heart failure typically rely on hospital discharge data, and hospitalized patients may be less representative of the general population because they likely overrepresent severe cases of heart failure, not the incident diagnosis. Future studies should attempt to leverage both outpatient and inpatient records for analysis to achieve maximum sensitivity and specificity.
Our study includes several important limitations. The VAPIHCS does not include an inpatient VA medical center, instead relying on contracting agreements with military treatment facilities or community hospitals for inpatient care of its veterans. Therefore, our reliance on outpatient VAPIHCS data obscures clinical information resulting from inpatient stays, as these data may not be readily or reliably incorporated into the veteran’s outpatient medical record. The result is the potential for underreporting heart failure in this population, since we were unable to ascertain the extent to which hospitalized heart failure occurred in our sample over the course of follow-up. Furthermore, our administrative data were limited by a medical record diagnosis as a proxy for incidence, a potential for misdiagnosis, and unknown severity of PTSD. The lack of PTSD severity assessment in particular resulted in an inability to show a dose–response between PTSD severity and heart failure. This finding may have important causal implications, and future studies should investigate this possibility.
We were also unable to assess for time-varying covariates, such as tobacco use, substance use, BMI, and marital status, that may have changed over the course of our study period. Although nearly all veterans had a listed period of military service, the classification system groups together veterans who served in the first Gulf War (1990–1991) with those who served in the more recent operations in Afghanistan and Iraq (2001 to the present). As a result, we were unable to make a distinction between these military cohorts in our analyses. Finally, because of the separation of records between the VA and Department of Defense, we were unable to account for (1) time between military or combat service and first date of PTSD, (2) military rank, or (3) any specific characterization of trauma experienced.
A substantial proportion of missing data limited our ability to consider important potential confounders. With over 60% of participants missing relevant data for race and ethnicity, we were unable to assess racial and ethnic differences in the PTSD– heart failure association. Given the unique diversity among Pacific Island populations, there may be some important, yet unmeasured, differences in the development of heart failure by race or ethnicity in this population. Additionally, because myocardial infarction is typically coded during an inpatient stay, we were unable to reliably acquire these data. A meta-analysis of 24 studies and over 2300 participants found that 12% of acute coronary syndromes, including myocardial infarction, resulted in clinically significant PTSD,39 even though other studies have demonstrated that those with PTSD have increased risk of future adverse cardiovascular events.45 Despite these limitations, we were able to assess the temporality of the PTSD– heart failure association in our data, and we account for the diagnosis and treatment of several important clinical factors strongly associated with myocardial infarction.
Our results have important clinical and public health implications for veterans with PTSD. They support the increasing body of literature suggesting a relationship between mental illness and physical comorbidity. Epidemiological studies have consistently demonstrated a significant prospective relationship between depression and cardiac events in both healthy patients46,47 and patients with preexisting cardiovascular disease.48 Anxiety-related psychiatric diagnoses have also been found to be associated with cardiac events.49 The INTERHEART study of over 25 000 participants in 52 countries found that people reporting “permanent stress” at work or home were more than twice as likely to develop cardiovascular disease (OR = 2.14; 95% CI = 1.73, 2.64).50 Our results add to this body of literature that suggests a relationship between anxiety and detrimental cardiovascular outcomes; however, the number of studies investigating this association has been sparse, and more research is needed to elucidate the specific mechanisms involved in the development of cardiovascular events.51
As the focus of health policy shifts toward management of chronic disease, the need to understand relationships between comorbidities becomes vital. The Affordable Care Act specifically lists management of mental health as an “essential health benefit.”52 To comply with this provision and provide the highest quality of care requires greater understanding of associations between mental health and physical illness. The VA and others treating veterans could apply our findings to target screenings, interventions, and treatment programs for risk factors and early-stage heart failure in this high-risk population. From a public health perspective, the results contribute to the overall understanding of the total heart failure burden faced by those with PTSD.
Although ours is one of the first prospective studies examining the role of PTSD in the development of heart failure, it is consistent with newly emerging scientific information implicating psychological illness as a vital determinant of physical health. Given the ongoing involvement of US military personnel in combat operations, the high prevalence of PTSD in veterans, and the increasing incidence of heart failure in the United States, outpatient care must include both mental health and chronic disease management. Our findings provide support for the redoubling of heart failure prevention and treatment efforts among US veterans with PTSD.
Acknowledgments
The material presented in this article is the result of work supported by the National Center for PTSD, with resources and the use of facilities at the VA Pacific Islands Health Care System, Honolulu, HI.
Note. The opinions expressed are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States government.
Human Participant Protection
This study was approved by the institutional review boards of the Veterans Administration Pacific Islands Healthcare System and of Ohio State University.
References
- 1. National Institute of Mental Health. The numbers count: mental disorders in America. October 1, 2013. Available at: http://www.lb7.uscourts.gov/documents/12-cv-1072url2.pdf. Accessed November 12, 2014.
- 2.Kulka RA, Schlenger WA, Fairbanks JA . Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, NY: Brunner/Mazel; 1990. [Google Scholar]
- 3.Lund BC, Bernardy NC, Alexander B, Friedman MJ. Declining benzodiazepine use in veterans with posttraumatic stress disorder. J Clin Psychiatry. 2012;73(3):292–296. doi: 10.4088/JCP.10m06775. [DOI] [PubMed] [Google Scholar]
- 4.Qureshi SU, Pyne JM, Magruder KM, Schulz PE, Kunik ME. The link between posttraumatic stress disorder and physical comorbidities: a systematic review. Psychiatr Q. 2009;80(2):87–97. doi: 10.1007/s11126-009-9096-4. [DOI] [PubMed] [Google Scholar]
- 5.Spitzer C, Barnow S, Volzke H, John U, Freyberger HJ, Grabe HJ. Trauma, posttraumatic stress disorder, and physical illness: findings from the general population. Psychosom Med. 2009;71(9):1012–1017. doi: 10.1097/PSY.0b013e3181bc76b5. [DOI] [PubMed] [Google Scholar]
- 6.Norman SB, Means-Christensen AJ, Craske MG, Sherbourne CD, Roy-Byrne PP, Stein MB. Associations between psychological trauma and physical illness in primary care. J Trauma Stress. 2006;19(4):461–470. doi: 10.1002/jts.20129. [DOI] [PubMed] [Google Scholar]
- 7.Boscarino JA. Diseases among men 20 years after exposure to severe stress: implications for clinical research and medical care. Psychosom Med. 1997;59(6):605–614. doi: 10.1097/00006842-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Ahmadi N, Hajsadeghi F, Mirshkarlo HB, Budoff M, Yehuda R, Ebrahimi R. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol. 2011;108(1):29–33. doi: 10.1016/j.amjcard.2011.02.340. [DOI] [PubMed] [Google Scholar]
- 9.Kang HK, Bullman TA, Taylor JW. Risk of selected cardiovascular disease and posttraumatic stress disorder among former World War II prisoners of war. Ann Epidemiol. 2006;16(5):381–386. doi: 10.1016/j.annepidem.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Kubzansky LD, Koenen KC, Spiro A, III, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64(1):109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- 11.Boscarino JA, Chang J. Electrocardiogram abnormalities among men with stress-related psychiatric disorders: implications for coronary heart disease and clinical research. Ann Behav Med. 1999;21(3):227–234. doi: 10.1007/BF02884839. [DOI] [PubMed] [Google Scholar]
- 12.Schnurr PP, Spiro A, Paris A. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans. Health Psychol. 2000;19(1):91–97. doi: 10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- 13.Cwikel J, Abdelgani A, Goldsmith JR, Quastel M, Yevelson II. Two-year follow up study of stress-related disorders among immigrants to Israel from the Chernobyl area. Environ Health Perspect. 1997;105(suppl 6):1545–1550. doi: 10.1289/ehp.97105s61545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sibai AM, Armenian HK, Alam S. Wartime determinants of arteriographically confirmed coronary artery disease in Beirut. Am J Epidemiol. 1989;130(4):623–631. doi: 10.1093/oxfordjournals.aje.a115384. [DOI] [PubMed] [Google Scholar]
- 15.Sibai AM, Fletcher AF, Armenian HK. Variations in the impact of long-term wartime stressors on mortality among the middle-aged and older population in Beirut, Lebanon, 1983–1993. Am J Epidemiol. 2001;154(2):128–137. doi: 10.1093/aje/154.2.128. [DOI] [PubMed] [Google Scholar]
- 16.Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Ann Behav Med. 2010;39(1):61–78. doi: 10.1007/s12160-010-9165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman MJ, Schnurr PP. The relationship between trauma, PTSD, and physical health. In: Friedman MJ, Charney DS, Deutch AY, editors. Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to PTSD. New York, NY: Lippincott-Raven; 1995. pp. 507–524. [Google Scholar]
- 18.von Känel R, Hepp U, Buddeberg C et al. Altered blood coagulation in veterans with posttraumatic stress disorder. Psychosom Med. 2006;68(4):598–604. doi: 10.1097/01.psy.0000221229.43272.9d. [DOI] [PubMed] [Google Scholar]
- 19.Sloan RP, Shapiro PA, Bagiella E, Myers MM, Gormon JM. Cardiac autonomic control buffers blood pressure variability responses to challenge: a psychophysiologic model of coronary artery disease. Psychosom Med. 1999;61(1):58–68. doi: 10.1097/00006842-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 20.de Kloet CS, Vermetten E, Geuze E, Wiegant VM, Westenberg HG. Elevated plasma arginine vasopressin levels in veterans with posttraumatic stress disorder. J Psychiatr Res. 2008;42(3):192–198. doi: 10.1016/j.jpsychires.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 22.Krantz DS, Manuck SB. Acute psychophysiologic reactivity and risk of cardiovascular disease: a review and methodological critique. Psychol Bull. 1984;96(3):435–464. [PubMed] [Google Scholar]
- 23.Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues Clin Neurosci. 2011;13(3):263–278. doi: 10.31887/DCNS.2011.13.2/jsherin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glaesmer H, Brahler E, Gundel H, Riedel-Heller SG. The association of traumatic experiences and posttraumatic stress disorder with physical morbidity in old age: a German population-based study. Psychosom Med. 2011;73(5):401–406. doi: 10.1097/PSY.0b013e31821b47e8. [DOI] [PubMed] [Google Scholar]
- 26.Hunt SA, Baker DW, Chin MH et al. ACC/AHA Guidelines for the evaluation and management of chronic heart failure in the adult: executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2001;104(24):2996–3007. doi: 10.1161/hc4901.102568. [DOI] [PubMed] [Google Scholar]
- 27.Ebong IA, Goff DC, Jr, Rodriguez CJ et al. The relationship between measures of obesity and incident heart failure: the multi-ethnic study of atherosclerosis. Obesity (Silver Spring) 2013;21(9):1915–1922. doi: 10.1002/oby.20298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Djoussé L, Bartz TM, Ix JH et al. Adiposity and incident heart failure in older adults: the cardiovascular health study. Obesity (Silver Spring) 2012;20(9):1936–1941. doi: 10.1038/oby.2011.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Loehr LR, Rosamond WD, Poole C et al. Association of multiple anthropometrics of overweight and obesity with incident heart failure: The Atherosclerosis Risk in Communities Study. Circ Heart Fail. 2009;2(1):18–24. doi: 10.1161/CIRCHEARTFAILURE.108.813782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 31.Lloyd-Jones D, Hong Y, Labarthe D et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 32.Nillni Y, Nosen E, Williams PA, Tracy M, Coffey SF, Galea S. Unique and related predictors of major depressive disorder, posttraumatic stress disorder, and their comorbidity after Hurricane Katrina. J Nerv Ment Dis. 2013;201(10):841–847. doi: 10.1097/NMD.0b013e3182a430a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Compare A, Zarbo C, Manzoni GM et al. Social support, depression, and heart disease: a ten year literature review. Front Psychol. 2013;4:384. doi: 10.3389/fpsyg.2013.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Owens GP, Baker DG, Kasckow J, Ciesla JA, Mohamed S. Review of assessment and treatment of PTSD among elderly American armed forces veterans. Int J Geriatr Psychiatry. 2005;20(12):1118–1130. doi: 10.1002/gps.1408. [DOI] [PubMed] [Google Scholar]
- 35.Lemke S, Schaefer JA. VA nursing home residents with substance use disorders: mental health comorbidities, functioning, and problem behaviors. Aging Ment Health. 2010;14(5):593–602. doi: 10.1080/13607860903586169. [DOI] [PubMed] [Google Scholar]
- 36.Mason AE, Boden MT, Cucciare MA. Prospective associations among approach coping, alcohol misuse and psychiatric symptoms among veterans receiving a brief alcohol intervention. J Subst Abuse Treat. 2014;46(5):553–560. doi: 10.1016/j.jsat.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Selvin S. Statistical Analysis of Epidemiologic Data. New York, NY: Oxford University Press; 1996. pp. 213–214. [Google Scholar]
- 38.Kannel WB, D’Agostino RB, Silbershatz H, Belanger AJ, Wilson PW, Levy D. Profile for estimating risk of heart failure. Arch Intern Med. 1999;159(11):1197–1204. doi: 10.1001/archinte.159.11.1197. [DOI] [PubMed] [Google Scholar]
- 39.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275(20):1557–1562. [PubMed] [Google Scholar]
- 40.Chen YT, Vaccarino V, Williams CS, Butler J, Berkman LF, Krumholz HM. Risk factors for heart failure in the elderly: a prospective community-based study. Am J Med. 1999;106(6):605–612. doi: 10.1016/s0002-9343(99)00126-6. [DOI] [PubMed] [Google Scholar]
- 41.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I Epidemiologic Follow-up Study. Arch Intern Med. 2001;161(7):996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 42.Kenchaiah S, Evans JC, Levy D et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347(5):305–313. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 43.Dhingra R, Sesso HD, Kenchaiah S, Gaziano JM. Differential effects of lipids on the risk of heart failure and coronary heart disease: The Physicians’ Health Study. Am Heart J. 2008;155(5):869–875. doi: 10.1016/j.ahj.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 44.Edmondson D, Richardson S, Falzon L et al. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One. 2012;7(6):e38915. doi: 10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.von Känel R, Hari R, Schmid JP et al. Non-fatal cardiovascular outcome in patients with posttraumatic stress symptoms caused by myocardial infarction. J Cardiol. 2011;58(1):61–68. doi: 10.1016/j.jjcc.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 46.Aromaa A, Raitasalo R, Reunanen A et al. Depression and cardiovascular diseases. Acta Psychiatr Scand Suppl. 1994;377:77–82. doi: 10.1111/j.1600-0447.1994.tb05807.x. [DOI] [PubMed] [Google Scholar]
- 47.Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction: prospective data from the Baltimore ECA follow-up. Circulation. 1996;94(12):3123–3129. doi: 10.1161/01.cir.94.12.3123. [DOI] [PubMed] [Google Scholar]
- 48.Barefoot JC, Helms MJ, Mark DB. Depression and long-term mortality risk in veterans with coronary artery disease. Am J Cardiol. 1996;78(6):613–617. doi: 10.1016/s0002-9149(96)00380-3. [DOI] [PubMed] [Google Scholar]
- 49.Kawachi I, Colditz GA, Ascherio A et al. Prospective study of phobic anxiety and risk of coronary heart disease in men. Circulation. 1994;89(5):1992–1997. doi: 10.1161/01.cir.89.5.1992. [DOI] [PubMed] [Google Scholar]
- 50.Rosengren A, Hawken S, Ounpuu S et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 646 controls from 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364(9438):953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 51.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 52. Patient Protection and Affordable Care Act, 42 USC §18001 et seq. (2010)