Abstract
Physiological mechanisms promote weight gain after famine. Because eating disorders, obesity, and dieting limit food intake, they are famine-like experiences. The development of the concept of meeting an ideal weight was the beginning of increasing obesity. Weight stigma, the perception of being fat, lack of understanding of normal growth and development, and increased concern about obesity on the part of health providers, parents, and caregivers have reinforced each other to promote dieting. Because weight suppression and disinhibition provoke long-term weight increase, dieting is a major factor producing the obesity epidemic. The integrated eating disorder–obesity theory included in this article emphasizes that, contrary to dieters, lifetime weight maintainers depend on physiological processes to control weight and experience minimal weight change.
Since 1960, the Centers for Disease Control and Prevention has done periodic surveys of representative samples of the US population, which include measured heights and weights.1 From the 1960 to 1962 to the 1976 to 1980 measurement periods, there was little change in population weight. However, the next survey (1988–1994) showed increases in body mass index (BMI; defined as weight in kilograms divided by the square of height in meters [kg/m2]) that were unanticipated and inexplicable.2 Most of the increase occurred in those with BMI of 30 or greater.3 In 2006, a prominent Centers for Disease Control and Prevention researcher expressed frustration with her incapacity to explain why this happened.2
Losing weight and recuperating from that weight loss is part of the biological heritage of every human being.4–6 However, in the past 70 years, self-induced famine (dieting to achieve and maintain a lower weight)7 became the societal norm.8–11 This suggests that much of the behavior observed in people who perceive they are overweight and who diet, manage, control, maintain, or suppress their weight could be manifestations of starvation and recovery from starvation.4–6
We breathe in and out, our hearts beat steadily, our temperature is automatically maintained without our thinking about it. The human body has similar mechanisms that produce weight gain after weight loss5,6 or weight loss after weight gain.5 However, this control is more flexible than the control of breathing: short-term differences in food intake are extremely variable over a period of hours or days whereas the mechanisms to moderate weight to previous levels take effect over a period of weeks or months.5 These mechanisms work similarly and are equally efficacious in people of all weights.6
The researchers and practitioners who study energy balance, weight control, obesity, and eating disorders reflect different disciplinary viewpoints that function independently and publish their research in different genres of professional journals.5 In this article, I sought to integrate this literature and show how the physiology of weight control is of paramount importance in explaining why the long-term trend in obesity changed.
BIOLOGICAL MECHANISMS
The basic premise of this article is that dieting is a self-imposed, voluntary famine. The most definitive study of famine is the Minnesota Experiment.4 The validity of this study has been questioned because no formal control group was used.12,13 However, an autocontrol of baseline measurements of all the parameters included in the study was established during a 12-week period before the men were placed on the semistarvation diet.4(ch4) In addition, 12 men who lived under the same conditions as the Minnesota Experiment and participated in a similarly rigorous but non–weight-loss nutritional experiment presented no evidence of the weight loss or behavior changes found in the Minnesota Experiment.12
The average age for the men selected for the Minnesota Experiment was 25.5 (±3.5) years. They were sociable and in good physical and mental health. Their initial BMI was 22.1 (±2.0). During the 24-week semistarvation phase, their intake averaged 1570 kilocalories per day (45% of autocontrol kcal) producing an average weight loss of 37 pounds in 24 weeks. (1.5 lb/wk; 24% of autocontrol weight). During 12 weeks of limited rehabilitation they were divided into 4 different groups on the basis of distinct percentages of autocontrol caloric levels.4(ch4) The men in the group with the highest caloric intake (88% to 116% of autocontrol levels) regained an average of 19 pounds during this time (1.5 lb/wk) recuperating 60% of their lost weight. Those in the lowest group (55% autocontrol period kcal) remained essentially the same weight for 6 weeks, gained an average of 3 pounds during 4 weeks on 78% autocontrol caloric levels, and an additional 3 pounds during 2 weeks on 88% autocontrol caloric levels. No participant returned to his autocontrol weight during limited rehabilitation.4(pp1133–1140),12
To celebrate the end of the experiment, the men attended an all-you-can-eat banquet. The next day they began eating prodigious amounts of food and frequently felt powerless to stop. They ate large meals, and then snacks between meals even though they were not subjectively hungry.4(p846),12 Five months after terminating semistarvation, 4 men still reported cravings and excessive eating.4(p848)
Recent reviews report that binge eating and binge eating disorder (BED) exist as a continuum of symptoms that differ in magnitude but not in type of problem.14–18 The size of a binge varies from quite small to extremely large14–16 and the frequency of bingeing ranges from infrequent (<1/wk)14,15,17 to bingeing more than 2 hours in a day.15,17 Loss of control over eating is an important criterion for BED14–16 but the presence of overweight or obesity are not criteria.15,19 Those with low BMI and high weight suppression show the highest frequency of binge eating,20,21 rapidity of weight regain,22 and onset or maintenance of bulimic symptoms over a 5- or 10-year period.22,23
What links famines, eating disorders, and obesity is limitation of food intake. The behavior following semistarvation in the Minnesota Experiment complies with the more extreme descriptions of BED.14–17 This close relationship has been confirmed by 3 studies that used questionnaires based on poststarvation eating to assess behavior of people diagnosed with BED.24–26 Hagan et al.24,25 used diagnosed BED participants and people from a general population. Both studies decisively showed that BED behavior is a poststarvation response to food. Sibilia26 used descriptions of poststarvation eating interspersed with more neutral eating behaviors. High or low agreement with the question: “At times I feel an unbearable hunger”26(p347) was used to divide 311 college students into 2 groups. Only questions similar to those used in the Hagan studies showed statistically significant differences between the groups.
Table 1 shows the physiological, behavioral, and psychological ramifications of the different phases of the Minnesota Experiment. During the R1-to-R12 period (weight maintenance), the level of dietary restraint was imposed by the experimenters and adhered to by the participants. If one considers the severity of binge eating after R12, it is highly probable that if they had not conformed to the experimental protocol they would have binged during this period. The citations in Table 1 are not exhaustive but are indicative of similarities between the Minnesota Experiment and recent information found in the literature.24–49
TABLE 1—
Observations and Measurements of Minnesota Experiment Participants During Weight Loss, Limited Rehabilitation, and Weight Regain4,12 With Citations to Similar Observations Reported in the Current Eating Disorders and Obesity Literature
| Category | Observations and Measurements |
| Observed during semistarvation phase (weeks S1-S24); period of weight loss | |
| Physiological | Increased appetite, hunger, desire for salt, edema, alopecia, vertigo, faintness on arising, momentary blackouts, craving for food, fatigue, weakness, hearing acuity, desire for hot food, unsteadiness, and sensitivity to cold.27 |
| Decreased production of sex hormones, blood pressure, blood glucose, tolerance of cold temperatures, endurance, strength, reaction time, coordination, sex drive, interest in opposite sex, pulse rate, metabolic rate, and capacity to lift. | |
| Cuts and wounds slower to heal, muscle cramps, soreness, and polyuria. | |
| Behavioral | Food and eating became dominant concern; collected cook books, etc.; possessive attitude toward food; total attention to food while eating; eats food formerly disliked24,25; initially gulped food, but at end ate very slowly25; all food consumed to last crumb; intolerant of food waste; daydream about foods25,26; created unusual food concoctions30; poor table manners24; added ingredients to thicken food24; smoked,31, 32 chewed gum to alleviate hunger; some started smoking31; and consumed large amounts of water, coffee, tea. |
| Increased moodiness,38,39 irritability,25,38,39 self-centeredness, narrowing of interests, and gastrointestinal distress24,25; complaints about lack of alertness, poor comprehension, lack of judgment, and deterioration of memory.33–36 | |
| Decreased ambition, self-discipline, self-control, social initiative,39 sociability,39 ability to concentrate,39 interest in opposite sex,39–42 sense of humor, and interest in learning. | |
| Psychological | Increased depression,39,43,44 apathy, dissatisfaction with their appearance, inability to sustain mental or physical effort,39 “nervousness” and general emotional instability, social withdrawal,39 and narrowing of interests. |
| Decreased decisiveness, ability to make personal plans,25 willingness to participate in group activities,39 and sexual desire.39,40,42 | |
| Increased MMPI scales4: hypochondriasis, depression, and hysteria at end of semistarvation (P<.01); depression increased >2 SD. | |
| Observed during limited rehabilitation phase (weeks R1-R12): period of weight maintenance) | |
| Physiological | Increased appetite, hunger; decreased strength (had not returned to control levels at R12). |
| Behavioral | Increased irritability,25,38,39 impatience, tenseness, and general unrest.43 |
| At R12 had not resumed academic studies and intellectual pursuits25 to level during autocontrol; inefficiency and poor study habits continued.25,33–36,39 | |
| Recovery from dizziness, apathy, and lethargy most rapid; tiredness,44 loss of sex drive,39–42 and weakness were slow to improve. Many were argumentative and negativistic45,46 and failed to reestablish efficient nonexperimental lab and work assignments.44,46–48 Food concoctions continued.30 | |
| Lack of strength, endurance; as weight increased regained humor, enthusiasm. Sociability progressively reappeared and irritability and nervousness decreased.39 | |
| Psychological | Psychobiological stress continued to greater or lesser degree depending on level of refeeding. For those who maintained weight there was a return to the depressed levels experienced during semistarvation (famine).44,46,49 |
| Feeling of well-being, range of interests, emotional stability, and sociability returned more rapidly than strength, endurance, normal eating habits, and sexual drive. | |
| Observed during no restrictions on eating phase (weeks R13-R58): period of complete disinhibition of dietary restraint) | |
| Physiological | Banquet with unlimited food served on last day of R12 produced LOC (binge days),14,15,24–26 GI distress.24,25 |
| Tiredness, unusual sleepiness; improvement in sex drive and spontaneous activity parallel increase in hunger, appetite. | |
| At R58 were similar to pre-experimental norm. | |
| Behavioral | 3 men restricted food intake to return to autodetermined weight levels.4,49 |
| Increased irritability38; food concoctions continued30; attempts to avoid wasting food even though supplies unlimited; and eats fast or slowly. | |
| At R20 (5 wks) 5 of 15 who reported for follow-up still binge eating. At R33 (8 wks) 4 of 14 still bingeing. | |
| Psychological | Distress associated with LOC. 3 men: distress with regaining “too much” weight. |
| Psychological stamina of the participants was unquestionably superior to that likely to be found in any random or more generally representative population sample.4 | |
Notes. GI = gastrointestinal; LOC = loss of control over eating; MMPI = Minnesota Multiphasic Personality Inventory.
IDEAL WEIGHT
The first widely available ideal height–weight tables were published by insurance companies in the 1940s based on actuarial analysis of longevity. They consisted of heights with corresponding weights for small, medium, and large frames. With the publication of these tables the idea of a healthy weight and losing weight to improve lifespan became plausible and desirable because higher premiums were charged for those who weighed more than their “ideal” weight.50
Currently, the National Institutes of Health defines a healthy weight as a BMI of 18.5 to 24.9, overweight as 25.0 to 29.9, and obesity as 30.0 or greater.51 It is recommended that a person with a BMI of 25 or greater should lose 5% to 10% of current weight, at a rate of 1 to 2 pounds per week, with a focus on balancing calories in–energy out, and following a healthy eating plan. The recommended caloric intake is 1000 to 1200 kilocalories per day for women and 1200 to 1600 kilocalories for men.52
However, for most people, ideal weight is related to societal appearance norms rather than health and longevity.53 Evidence that an ever-thinner ideal woman has evolved is found in an analysis of Playboy centerfolds that shows a decreasing trend in average BMI from approximately 19.8 in 1953 to approximately 17.9 in 2001.54
WEIGHT STIGMA
Weight stigma has 3 components: cognitive (stereotype), affective (prejudice), and behavioral (discrimination).55 Together these 3 components produce self-stigma.56,57 Weight stigma is part of the everyday experience of people with obesity.57 Link and Phelan58 designated it as structural discrimination: behavior that determines social relationships and whether a person receives recommendations of colleagues and friends.59 The frequency of experiencing weight stigma is similar to gender,60 race,60,61 and gay or lesbian stigma.61 Current health policy regarding obesity seems to have inadvertently supported all 3 aspects of weight stigma.62
Weight stigma is found at all ages63–68 and professions62 including teachers,69–71 dietitians,72,73 nurses,73,74 and physicians.73–76 Physicians who specialize in the treatment of obesity75,76 consider fat people lazy, stupid, and worthless on both implicit and explicit attitude measures.76 Because weight is considered controllable, not achieving weight-loss goals is attributed to lack of intelligence, motivation, will-power, self-discipline,74,75 and knowledge.74 People with obesity accept responsibility for their condition, attributing it to failure on their part even though they have tried multiple weight-loss remedies.74
Antifat bias of children increases with age.77 Recipients are subject to bullying, teasing, and verbal harassment.78 The problems caused by teasing and bullying related to weight stigma do not seem to be the events as such, but the frequency of the events,79 whether the person who receives it is bothered by it,80,81 and whether the person perceives herself or himself to be “too fat.”82 Of the people who perceive weight discrimination, those who are not obese are more likely to become obese and those already obese more likely to maintain obesity over a 4-year period.83
PERCEPTION THAT “I AM TOO FAT” IS A PROBLEM
Internalization of the cultural norm of thinness occurs when a person adopts the norm of extreme thinness as his or her private ideal. The BMI of men and women portrayed in commercial television is highly skewed compared with the actual weight distribution in the US population: 31% of the women on television are underweight versus 5% of the actual population, and only 3% obese, versus 25% of the actual population. Weight prejudice is reflected in these programs.84,85 Media exposure to thin-ideal images engenders a significant increase in body dissatisfaction compared with controls that did not view such images.86 A 5-year prospective study shows that those who read magazines that present articles and advertisements about dieting and weight loss put higher importance on weight,87 and engaged in a greater number of eating disorder–related weight control measures than their peers who do not.88 Older children and adolescents may be especially vulnerable because they look to the media, including advertisements, for information to shape their own identity.89
People of all ages and BMI levels perceive they are “too fat.”90–94 Being “too fat” has been expressed as early as age 5 to 6 years.90 Kurth and Ellert91 measured 11- to 17-year-olds regarding physical well-being, emotional (psychological) well-being, feelings of self-worth, well-being in the family, well-being in relation to friends or same-age peers, and well-being in the school domain. For every parameter measured, the behavior of those who perceived themselves to be “far too fat” was the same no matter what was their objective BMI classification. All those who self-perceived they were “just the right weight” also had the same behavior regardless of their BMI.
Of the 11- to 14-year-olds studied by Viner et al.,92 2% of the girls defined by BMI as underweight considered themselves “too heavy” but 5% were currently dieting and 10% had previously dieted. Thirteen percent of those who were normal weight and 36% of those who were overweight perceived themselves to be “too fat” and the percentage currently dieting or who had ever dieted was about double these percentages. For the obese girls, 63% considered themselves to be “too fat,” 81% were currently dieting, and 77% had previously dieted. For boys, lower misperceptions of being “too heavy” were recorded but the proportional increase in percentage of those who were currently trying to lose weight or had ever dieted was similar.92 People with BMIs of 35 to 39.9 divided themselves 50–50 between those who perceived that they were overweight and those who considered themselves obese. Those who considered themselves overweight reported fewer objective binge-eating episodes (eating an objectively large amount of food accompanied by loss of control) and less distress about eating compared with those who considered themselves obese.95
Dieting leads to long-term weight gain. Longitudinal observational studies or prospective cohort studies that last 4 to 5 years96–102 or more97,103–110 in preadolescent girls96,97 and boys,97 in girls and boys at puberty,97,98 in adolescent to early adult girls99–101,103–105 and boys,101,103,105 in women,106–109 and men102,107–110 (including 2 studies of male and female twins105,107), show that those who are dieting at the beginning of the study end up weighing more than their nondieting counterparts, even though they are not overweight at the beginning of the study.103,110,111 Two longitudinal studies112–114 show no relationship between dieting and an increase in BMI. These studies included yearly measurements of height and weight coupled with yearly administration of diet and weight-control questions.112,113 They also show selective loss to follow-up of individuals with a higher BMI.112,114 Studies of Olympic wrestlers show weight gain over time compared with nonathletes110 or athletes who have less severe cycling,110,115 but a study of collegiate athletes did not show this pattern.116
WEIGHT MAINTENANCE VERSUS SUPPRESSION
Maintaining a lower weight is considered a virtue in the obesity literature (weight maintenance) but the eating disorder literature considers it problematic (weight suppression). “Successful weight loss,” defined by the National Weight Control Registry as losing at least 10% of initial body weight and maintaining that weight loss for at least 1 year,117 is used to evaluate most weight-loss studies. However, a review of weight-loss studies that lasted 2.5 years or more shows that the ineffectiveness of dieting is frequently underestimated because of 4 methodological problems: very low follow-up with inadequate reporting of the characteristics of those who continued versus those who dropped out, not asking about additional dieting that might have occurred after the diet that was being studied, self-reported weight, and confounding the effect of dieting with that of increased physical activity. They concluded that each of these factors biases studies toward showing successful weight-loss maintenance.118
The effect of these factors can be seen in the Minnesota Experiment4 and other reports.49,117 For the Minnesota Experiment, only 21 of the original 32 men reported for follow-up at week R58. Of these, 12 (57%) had gained more than 10 pounds (R58 weight minus maximum autocontrol weight), 4 (19%) had gained between 5 and 10 pounds, 2 (10%) were within 5 pounds (gain or loss), and 3 (14%) were known to have actively dieted after their poststarvation weight increased to levels they considered unacceptable. Two men who had previously reported considerable weight gain did not show up for this evaluation.4(p1140)
Look AHEAD (Action for Health in Diabetes) was a multicenter randomized controlled trial designed to assess the efficacy of weight loss for adults with diabetes. It compared an intensive lifestyle intervention (ILI) with diabetes support and education. The goal was to lose 10% or more of initial weight during the first 6 months eventually stabilizing at a mean weight loss of 7% or more. The ILI groups initially met frequently, used portion control, and was encouraged to use meal or snack replacement products. If the participant lost 5% or less body weight at 6 months, pharmacotherapy was encouraged.119
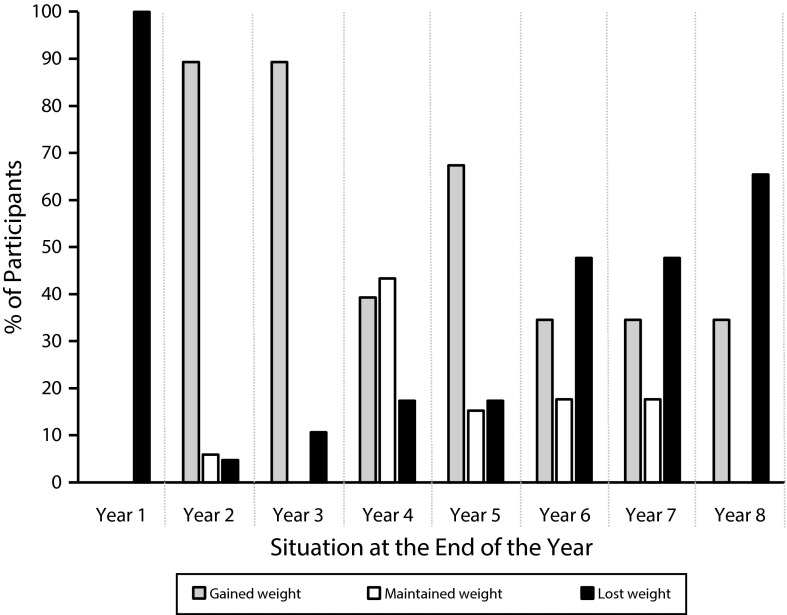
At the end of the eighth year the participants were grouped according to their year-1 weight loss (≥ 10%, 5%–9.9%, 0%–4.9% of initial weight) and then subgrouped by each category on the basis of those who in year 8 had lost 10% or more, 5% to 9.9%, 0% to 4.9%, or gained weight. Figure 1 shows that all groups lost weight during the first year. In the subsequent 2 years, 89% were in groups that gained weight. In year 4, a measurement year, 43% were in groups that maintained weight but in all other years less than 20% were in groups maintaining weight. By year 8 all groups were either gaining or losing weight.120
FIGURE 1—
Year-by-year changes in percentage of intensive lifestyle intervention participants in groups that were gaining weight, maintaining weight, or losing weight during 8 years of the Look AHEAD study.
Note. AHEAD = Action for Health in Diabetes. Calculated from grouped data included in Figures 4a to 4c of Look AHEAD Research Group.120
At year 4, the ILI group had, on average, improved weight, fitness, and cardiovascular indicators compared with the diabetes support and education group.121 At year 10, the ILI group, on average, showed improved weight loss and waist circumference, with inconsistent improvement in glycerated hemoglobin between year 6 and 10. However, no differences were found between ILI and diabetes support and education groups in terms of cardiovascular disease morbidity or mortality.122
Qualitative studies indicate that successful weight-loss maintainers constantly think about maintenance,123,124 use clothing fit as feedback,123–126 weigh themselves frequently123,125,126 (some several times a day),125,126 and keep track of their actions through journaling or worksheets.124–126 When challenges or setbacks occur they immediately institute changes to reduce their weight.125,126 But many get bored with monitoring, or decide that it is no longer worth paying constant attention to what they are eating.123,125 In one study, partners, family, and friends were reported as being saboteurs of maintenance efforts.124 In contrast, lifelong weight maintainers take a relaxed attitude toward food, do not weigh themselves frequently, nor do they stress about a few pounds.126
This analysis indicates that “successful weight loss” usually refers to weight cycling rather than lifelong maintenance. Both the National Weight Control Registry117 and the qualitative studies of weight maintainers123–126 show that people who attempt to maintain weight use activities associated with eating disorders: frequent weighing,127 continuous monitoring of weight and appearance,128 and high levels of physical activity.129 Ironically, weight loss or maintenance efforts did not produce the health benefits that the obesity literature anticipated.122
EARLY-ONSET OBESITY
Retrospective studies of the age of onset of bingeing and dieting show 2 groups: one that dieted before bingeing (D1) and another that binged before dieting (B1)28,130–140 with the B1 sequence always starting at a younger age. In studies that reported the age at which the person recalls becoming overweight, the D1 sequence is diet, binge, overweight,130–133 which is the sequence alluded to in the previous sections of this article. However, the B1 sequence is binge, overweight, diet130–133 except for young men (average age: 18.0 ±10.5 years), who dieted frequently and show a sequence of overweight, binge, diet.133 This different perception is probably attributable to their adolescent growth spurt.141 Spurrell et al.130 found that 90% of their B1 and 59% of D1 began bingeing before their 20th birthday. Women with early onset obesity (aged < 18 years) have a greater lifetime maximum weight, more dieting attempts, greater weight loss on a single diet, and increased binge eating.142
The cited studies did not differentiate between bingeing with loss of control and overeating. Loss of control over eating is a physiological response to a previous lack of food4(p846–849) but not necessarily dieting as such.143 It can result in the development of partial- or full-syndrome BED.144 Overeating is a precursor to rapid growth that occurs in childhood145 or at puberty.141 It also may occur at any age as a response to nonverbalized emotions.146–148 A person that has a sense of control over eating may eat a lot (overeating) but does not show typical eating-disorder symptoms.149 Loss of control over eating can occur with lower or higher body dissatisfaction. However, the higher the body dissatisfaction the more severe the eating-disorder symptoms.149 Children who binge with loss of control have significantly greater weight concerns,150 disordered eating attitudes,145 eating in the absence of hunger,145 and depressive and anxiety symptoms145,150,151 as well as greater use of other maladaptive strategies151 compared with overeaters.
To better understand the factors that underlie early onset obesity, I will first discuss the nature and timing of the adolescent growth spurt and the physiological changes that take place in both sexes during puberty. I then discuss how concern about obesity affects the feeding practices and interrelationships between child and parent from infancy to adolescence. This is followed by the effect of childhood trauma on the development of obesity.
Normal Growth and Development
Body mass index is currently used to indicate relative adiposity in people. However, people come in all sizes and shapes. Some are naturally more rounded, others more angular. Some have small, light bones; others have large, dense bones. Some have long trunks and short legs; others have long legs and short trunks. Those with large, dense bones; long trunks; and short legs automatically have a higher BMI than those with small, light bones; long legs; and short trunks even though they do not have higher fat mass.
The BMI cut-offs for underweight, normal weight, overweight, and obesity for children are based on cross-sectional analysis of children from birth to 20 years.152 However, longitudinally, weight increase precedes height increase.153 The age at which peak weight or height velocity occurs, the amplitude of that velocity, and the duration of the growth spurt all vary in distinct ways among individuals.154,155 Because of this, Tanner, a renowned authority on human growth,156 concluded that there can be no satisfactory weight for height standards between the ages of 7 to 18 years (girls)154 or 9 to 20 years (boys).154,155
Every organ, muscular, and skeletal dimension of the body takes part in the adolescent growth spurt. Early in the process the growth of the heart, stomach, and other visceral organs speeds up.157 In both boys and girls, the head, hands, and feet reach their adult status first. Leg length reaches peak growth velocity before trunk length. The body broadens later: hips in girls, shoulders in boys.155
During adolescence a person gains about 50% of his or her adult body weight.158 From infancy to about age 5 to 7 years, BMI decreases after which it begins to increase. This increase has been designated “adiposity rebound.”159 An earlier adiposity rebound is accompanied by being taller in childhood, having earlier pubertal development, and greater growth increase during puberty.155
Fat mass and BMI correlate well,160 but BMI is a weight-to-height ratio (kg/m2), not a measurement of body composition. Fat-free mass increases steadily in childhood and at the beginning of adiposity rebound increases more rapidly than fat mass, which does not increase appreciably until about 2 years later.161 Childhood overweight has been consistently associated with larger long-bone cross-sections in both sexes.162 In girls, nearly one third of total skeletal mineral is accumulated in the 3- to 4-year period immediately after puberty onset.158 Both boys and girls who enter puberty early have the same average adult height as those who enter later,163,164 and their comparative increased fat-free mass and bone density continues as adults.162 Thus, they naturally have higher BMIs as adults compared with their later-maturing companions. As there is an increase in fat-free mass and bone density as well as fat mass during adiposity rebound, a more appropriate designation would be preparation for pubertal growth rather than a critical period in childhood for the development of obesity.159
In adolescence, both boys and girls worry about looks, popularity, and relationships with the opposite sex.165 In girls, the worry about looks concentrates on thinness and weight165 whereas boys want to be more muscular.166 The normal physical development of girls includes increased size of visceral and sexual organs in the lower part of the trunk, increased hip breadth, and increased fat as a natural part of the process of becoming a woman. These changes are at odds with the very thin ideal for women promoted by US norms.9,10 Limiting food intake because of body image concerns, increasing exercise to burn up energy, and seriously wanting to lose weight all increase substantially in girls between 6 and 24 months postmenarche.167 The increased muscularity desired by boys is not compatible with a situation in which their strength has not caught up to their height and they are effectively managing an adult-size body with child-strength and child-size muscles.155
Parental Concerns
Parents are concerned about their children eating the right amount of food and the right kind of food. If they perceive that a child is overweight or “eats too much” the response is to restrict intake of the total amount of food or of foods high in fat and sugar.168 If the child is perceived to be underweight or not eating enough of the “right foods” the response is to pressure the child to eat more total food or more vegetables or other healthy foods.169 Restricting food leads to an increased desire to eat the restricted foods,168 and pressuring a child to eat leads to increased negative comments about the food and less desire to eat it,169,170 which sometimes lasts a lifetime.170
High concern about a child’s overweight or the possible development of overweight in the future is associated with increased weight between ages 3 and 5 years.171 Parents of children studied between birth and 5 years of age reported that 34% of the children experienced the emergence of overeating, 18% hid favorite foods, 9.7% seemed shy or inhibited when eating with parents compared with eating alone, and 9.7% ate so much that they became sick or vomited.172 Longitudinally, restriction at age 5 years predicts whether a girl eats although not hungry at age 7 years173 and 9 years174 as well as an increase in eating in the absence of hunger during these 4 years.174 A review of the literature confirmed the association between restricting foods and later increased BMI or food intake.175 These studies indicate that mothers who worry about their own weight and eating have higher concerns about daughters’ weight, higher levels of restricting daughters’ intake, and encourage daughters more frequently to lose weight.176,177 Fathers are involved but no longitudinal studies were found.
A mother’s concern that a child might become overweight seems to be dependent on trunk and leg fat related to total fat,178 eating more sweets and other palatable foods,178 eating rapidly,179 and eating more than presumed to be normal.145 Although most studies of children depend on parent observations, there is little concordance between a 6-year-old girl180 or 6- to 12-year-old child181 and his or her parent’s answers regarding the child’s food-related behavior. This discrepancy in parent–child observations could be critical in terms of future excessive weight gain. Shomaker et al.145 documented a group of children who were classified by their mothers as eating excessively but who actually were overweight with a lower fat mass than the other groups in the study (high BMI, not high fat). This indicates that, for the child, the increase in intake is best characterized as a response to the physiological need for enough food for his or her body. Because the mother sees it as overeating, this could lead to attempts to restrict intake with concomitant increased hiding or eating food when mother is not around.145,172
Childhood Trauma
Longitudinal studies show that childhood trauma (emotional neglect,182 physical neglect,183,184 physical abuse,182,183 sexual abuse,184,185 and lack of parental support182,186) result in increased BMI in adulthood. Child emotional neglect and abuse are common187 but difficult to define and measure.188 Estimates for child sexual abuse range from less than 3%182,183 to 30% in girls and 15% in boys.189 Noll et al.,185 using cross-sequential technique, found no differences between sexually abused girls and a comparison group in terms of the percentage who are obese at ages 6 to 14 years (P = .52), nor at 15 to 19 years (P = .09). However, at age 20 to 27 years, more than 40% of the sexually abused girls were obese compared with 30% of the comparison group (P < .009). A study of adults who reported childhood physical or sexual abuse found increased odds ratio (≥ 3) for recurrent fluctuations in weight, strict dieting, obesity, any eating disorder, and self-induced vomiting compared with those who had not been abused.184 Although childhood trauma occurs more frequently than we would like to admit, the incidence of child maltreatment reported in 2012, 2004, and 1999 indicates that the per capita rate has decreased.190 Thus, these factors cannot be cited as causing an increase in the prevalence of obesity.
Alexithymia, Interoceptive Awareness
Restriction of foods or physical or psychological abuse can begin at an age in which a child has little or no capacity to identify and verbalize emotions (alexithymia). Experiences of overeating to quell inexpressible emotions or hiding restricted food may result in lack of ability to distinguish hunger and satiety signals (interoceptive awareness). Several studies have cited these and related concepts as problems that lead to the development of bulimia nervosa and BED.146–148,191–193 Alexithymia may be more important in the development of obesity in men than in women.192
AN INTEGRATED THEORY OF DIETING, EATING DISORDERS, AND OBESITY
A good theory can be tested, receives empirical support, has predictive power, is internally consistent, and is as simple as possible to explain known facts.194 The basic components necessary for an integrated theory of eating disorders and obesity include sociological or psychological parameters that lead to the perception that “I am too fat” is a problem, limitation of food intake (dietary restraint) to correct that problem, hunger (from eating less food), the physiological reaction to hunger and limited food intake (disinhibition), and the psychopathology caused by lack of food (Table 1).
The transdiagnostic theory for eating disorders uses a core cycle in which overvaluation of eating, shape, and weight produces strict dieting, which in turn produces binge eating. This then loops back to renew the strict dieting. Alternative pathways show binge eating may be in balance with compensatory vomiting and laxative misuse (bulimia nervosa [BN]), whereas for anorexia nervosa (AN) the binge–compensatory cycle may be present but the behavior is basically diverted to a “starvation syndrome.”195(p521)
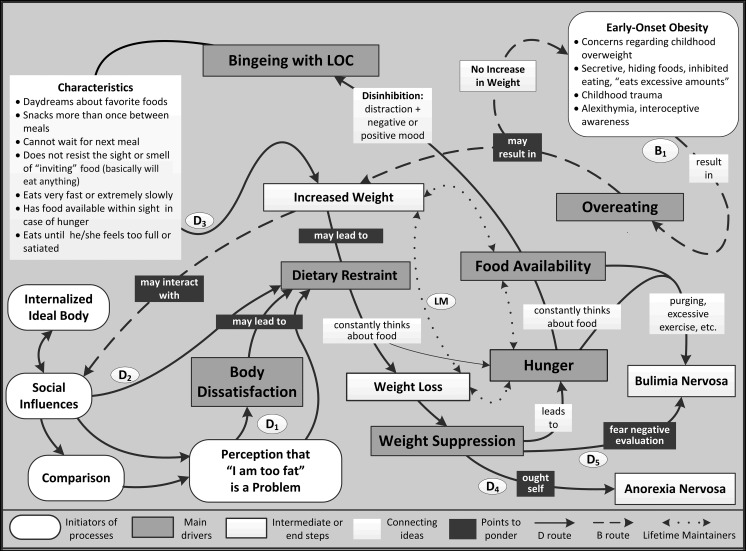
Figure 2 is a concept map of the integrated eating disorders–obesity theory, which amplifies and updates the transdiagnostic theory core cycle195 to align it with recent literature. The gray background represents the pervasive weight stigma that underlies obesity and eating disorders. The dieting routes to eating disorders and obesity (D1–5) begin in the lower left-hand corner based on the tripartite influence model.166,196-199 Social influences (media, peer influences, parental–family concerns) and comparison (judging one’s self-worth by comparison with media stereotypes, and to actual people in the immediate social environment of the individual)196,198 lead to the “perception that ‘I am too fat’ is a problem.” This phrase incorporates 3 concepts: perception of fatness, I am fat, and this is a problem I have to solve. If fatness is considered a problem, it leads to dietary restraint (“dieting” [D1]).82,91,92 High internalization of the thin ideal occurs equally frequently in high and low BMI females even though the person is not aware of it.200 Thus, comments within the immediate peer group201,202 augmented by schoolwide norms200,202 can result in girls with low to average BMI becoming increasingly concerned about weight and shape without expressing overt body dissatisfaction200 (D2).
FIGURE 2—
Integrated eating disorder–obesity theory.
Note. LM = lifetime maintainer; LOC = loss of control over eating. The gray background indicates the weight stigma that permeate any consideration of obesity. The D routes (solid-line arrows) begin in the lower left hand corner with “social influences,” etc. Starting with dietary restraint they begin a cycle that goes to weight suppression. From weight suppression they can follow a cycle that ends up with weight gain, or go to anorexia nervosa or bulimia nervosa. The B route (dashed-line arrows) begins in the upper right-hand corner and ends with “Social Influences.” It can also loop back on itself with no increase in weight. The life time maintainer route (dotted-line arrows) begins with hunger and food availability and can cycle in either direction.
Effective dietary restraint leads to weight loss. The period of weight loss is characterized by lower levels of disinhibition, practically no objective binge eating episodes, decreased depression, lack of subjective feelings of hunger, increased body satisfaction, and increased self-esteem.203 Lack of hunger results from a neurologic response to lack of food.204 The feelings of well-being and reduction of depression stem from feeling control over their weight.205
Once a lower weight is realized the person is then confronted with long-term weight suppression.120,123–126 Although negative affect is clearly seen after a famine (Table 1) this reality has been ignored in the obesity literature. The eating-disorder literature frequently assumes that it is psychological in origin.194,206,207 Body dissatisfaction is induced by peer pressure but is not accompanied by negative affect.208 Therefore the “negative affect” cited in the eating-disorder literature has to have its origins in attempting to maintain lower weight. This may explain why those who have lost weight report that friends and family act as saboteurs of their efforts to maintain the lower weight.124
Weight suppression has 3 potential outcomes: binge eating and weight regain, AN, or BN. Bingeing with loss of control is the most common and can range from levels that are indiscernible (<150 calories/d) to daily large binges.14–18 The variability of response in the Minnesota Experiment indicates that the reaction of a specific individual is probably genetic.209
Contrary to reports in the eating-disorder literature that binge eating is produced by negative affect,207 in the Minnesota Experiment, it began after a banquet.4(p843) Ecological momentary assessment studies show that binges occur most frequently when a person has moderate hunger,210,211 is alone,211 and distracted212 or in a negative211,213 or positive211 mood. Thus, the path from weight suppression to bingeing with loss of control includes hunger, constantly thinking about food, food availability, and disinhibition: distraction plus negative or positive mood. The connecting idea characteristics summarizes important aspects of bingeing with loss of control and indicates that under these conditions people will eat anything, not just highly desirable foods.4(p6),23–25 This process leads to increased weight (D3). If this is accepted, the route stops. If it is not acceptable, dieting eventually occurs again.214(p113),215 Repeated cycling through this route can lead to significant weight gain.96–110,215
It is generally thought that AN and BN (D4, D5) occur only in normal weight or very thin individuals. However the antecedents may be overweight216 or actual obesity.216,217 Dieting behavior of future AN is characterized by reduction in portion sizes, fixed meal times, and stereotyped food choices, which produce a slow, unrelenting weight loss.218 In BN, the concept of the thin ideal self is very strong and includes need for approval,219 as well as fear of negative evaluation.219,220 Future BN starts out with weight control behaviors that the obesity literature designates as unhealthy (fasted, ate little food, use of a food substitute, skipped meals) or extreme (taking diet pills, laxatives, diuretics, or vomiting).216 The weight loss results are generally poor, which leads to more restrictive diets, binge eating, and large fluctuations in weight.218 People with AN eat very slowly whereas those with BN eat rapidly. Training AN to eat progressively more rapidly, after they have agreed to gain at least 5 pounds,204,221 and BN, who have been assured that they will not gain weight, to eat less rapidly204 leads to normalization of their eating behavior and complete remission of their eating disorder and psychiatric symptoms.204,221
In Figure 2, the B1 route of early onset obesity begins in the upper right-hand corner and is shown by dashed-line arrows. Its antecedents are the indicated social factors rather than lack of food. The overeating that occurs usually includes sweets, snacks, and high-fat foods because they are readily available to a child in the community and are frequently restricted at home. If overeating is accepted, the child may become plump, but his or her body will balance the excessive calories with times in which less food is eaten. The result may be a slightly overweight person, but high levels of obesity will seldom occur. If an issue is made of the “excessive” intake and the limited plumpness that develops is considered worrisome by health professionals or concerned parents and caregivers, then these social influences may well initiate dieting in the child. This means they then follow the D3–5 routes to increased weight, AN, or BN.
The experience of lifetime maintainers126 is shown with dotted-line arrows in the middle of Figure 2. Flexible hunger and satiety determine the amounts eaten214 and physiological processes balance it out over time.5,6 At what level of lack of food, dietary restraint, and weight suppression the autonomic lifetime maintainers route turns into the perception of loss of control is unknown.
CURRENT THEORETICAL DEVELOPMENTS IN EATING DISORDERS
The terms “dietary restraint” and “disinhibition” originated with studies of dieting: the person inhibits caloric intake (dietary restraint), which is then disinhibited in response to food being available. The Restraint Scale was the first questionnaire available for measuring eating behavior in eating disorders. It was severely criticized because it measured concern for dieting and weight fluctuations rather than dietary restraint.222 The Three Factor Eating Questionnaire (TFEQ)223 and the Dutch Eating Behavior Questionnaire (DEBQ)224 were developed to correct these problems. The TFEQ purports to measure 3 physiologically sound constructs: dietary restraint, disinhibition, and hunger.223 The DEBQ purports to measure restrained eating, but the concept of disinhibition was substituted with emotional eating (eating in response to negative affect) and external eating (eating in response to food-related stimuli regardless of the internal state of hunger).224
When the transdiagnostic theory was developed,195 Fairburn and Harrison showed awareness of the close similarity between AN and postfamine psychology and behavior.39 However, the Fairburn et al. transdiagnostic theory did not indicate that other eating disorders might show less extreme aspects of this postfamine psychopathology.195
Stice et al. subtyped women with BN225 and BED226 based on measurements of dietary restraint, depression, and self-esteem. Two groups were formed: dietary (D) and dietary negative affect (DNeg). A prospective study of this dual pathway model indicated that body dissatisfaction predicted both dieting (P < .001) and negative affect (P < .01), but, although dieting predicted bulimic symptoms (P < .001), it did not predict negative affect (P < .1).227 This directly contradicts the findings of the Minnesota Experiment, which showed that mean depression scores increased to pathological levels at the end of the semistarvation period and then returned to normal in parallel with improvement in caloric intake.4(p868) In the original study with BN, although no significant difference was found between the subtypes with the TFEQ hunger scale, a significant difference was found on the BED component of the Axis I diagnostic scale (P < .01).225 In the BED study the TFEQ hunger scale shows a significant difference between BEDs (D < DNeg; P < .001).226 This suggests that if the subtyping had been based on the TFEQ hunger scale, the studies might have shown that dieting produced negative affect.
The lack of understanding of the primacy of limitation of food on subsequent psychopathology4,12 and the development of the emotional and external eating scales of the DEBQ224 opened the possibility to interpret binge eating (disinhibition) as a response to negative moods and the availability of desirable food228 rather than a response to whatever appears to be edible.24–26 A 2007 review defined disinhibition as measured by the TFEQ as “a tendency towards over-eating and eating opportunistically in an obesigenic environment.”228(p409) The review was “not concerned with the inhibition of Restraint but with the durable trait of Disinhibition” (disposition for opportunistic eating).228(p410) It concludes that “trait disinhibition” is associated with obesity and mediating variables that constribute to poorer health as well as increased severity of eating disorders.228(p409)
IMPLICATIONS FOR PUBLIC HEALTH
United States food guides based on vitamin and mineral needs have been issued periodically since 1943. The 1980 Dietary Guidelines included weight control for the first time.229 Since then the insistence on weight management to control and prevent obesity has become stronger230–232 and has increasingly been aimed at younger age groups.233 In the 2005 and 2010 Dietary Guidelines, weight control was no longer a separate goal but permeated the entire document with the exception of the section on micronutrients of concern. This increased emphasis is concomitant with a greater percentage of the population dieting234–236 and greater prevalence of obesity in the ensuing years.1 As people who are overweight or obese diet more frequently92,108 this produces a more rapid increase in weight for those at the higher end of the BMI curve.103,108
Thus, the insistence of the medical community and the dietary guidelines on weight loss, compounded by the commercial diet and weight-loss industry that makes more than $60 billion per year,237 result in dieting as a major factor producing the obesity epidemic.
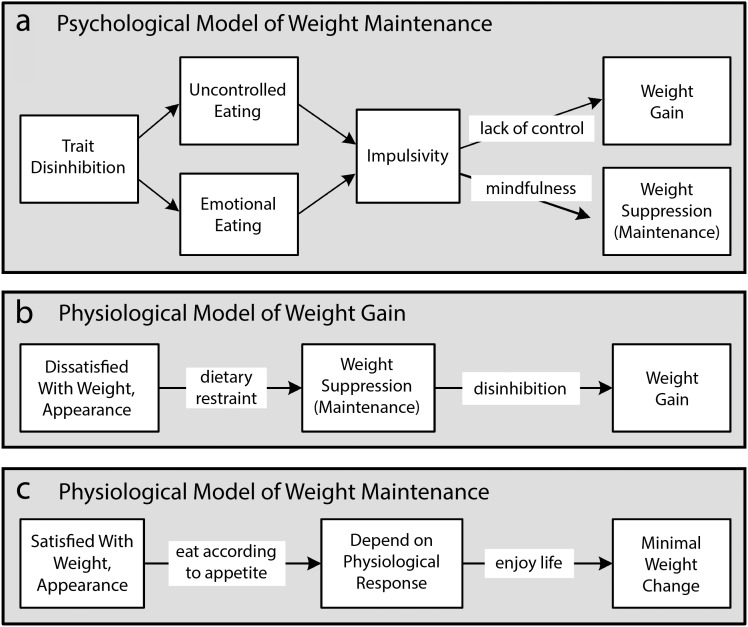
A good theory is as simple as possible to explain the known facts.194 Figure 3 contrasts a recent psychological explanation of weight control with autonomous physiological weight control. A 2011 article used the TFEQ-21 in which the 3 components refer to cognitive restraint, uncontrolled eating, and emotional eating to assess the relationships between “trait disinhibition,”228 impulsivity, mindfulness, and adverse psychological symptoms that are caused by weight suppression. Figure 3a diagrams their conclusions: “trait disinhibition” has 2 components: uncontrolled eating and emotional eating. Impulsivity, another concept that the psychological literature substitutes for disinhibition is positioned as a mediator for weight gain for both components. Since they found that mindfulness is negatively correlated to impulsivity, they conclude that it could be used to counteract the lack of control that leads to weight gain.238 However, the problem after dieting is loss of control as the result of physiological mechanisms that over several months propel the body to restore lost weight,5,6 not lack of control. Since mindful eating emphasizes controlling eating,239 it could be helpful in dealing with alexithymia or lack of interoceptive awareness, but will have minimal long-term effect on loss-of-control eating.
FIGURE 3—
Comparison of (a) a psychological explanation of weight gain and maintenance with (b) the physiological impetus to weight gain after weight loss and (c) the simplicity of weight maintenance when physiological mechanisms control weight.
Note. The grey background shows the weight stigma that permeates all considerations of obesity and eating disorders.
Figure 3b gives a succinct summary of the D1–3 routes of Figure 2. Dietary restraint is used to produce a lower weight. Disinhibition (loss-of-control eating) reflects the breakdown of that restraint and causes long-term weight gain. This diagram reinforces the conclusion of the review that disinhibition produces weight gain228 but attributes it to its correct source: physiological processes.
Figure 3c is a succinct statement of how lifetime maintainers126 keep their weight within plus or minus 5 pounds.108 Health at Every Size,240 Eating Competency,240–245 the Trust Model,246 and Intuitive Eating246 all reflect this diagram. A recent review shows that most programs based on these principles are successful in terms of weight maintenance and physiological measurements presumably related to future health problems.247 However, many of these programs do not acknowledge that eating for emotional reasons is part of life: all over the world people eat to celebrate weddings, holidays, and other special occasions, as well as offer food to console a person in difficulty. Physiological processes are perfectly capable of accommodating this variability of intake.5,6,126
Acknowledgments
This publication was made possible by a grant from the National Heart, Lung, and Blood Institute (1R01HL091826-01).
I would like to thank the additional multiple principal investigators of the National Institutes of Health proposal—Luisa Seijo-Maldonado, MSW, Robinson Rodríguez-Pérez, PhD, and Gladys Malavé-Martínez, MS—for their years of collaboration and support. In addition I would like to thank the interdisciplinary group of professors who worked with us: Dolores Miranda-Gierbolini, PhD, Karen Soto, PhD, Gloria Fidalgo, PhD, RD, Sara Benítez, MA, and Raúl Macchiavelli, PhD. Their support, doubts, comments, and questions were indispensable in developing this article. I would also like to give special thanks to Nancy M. Buss whose editorial insight was invaluable and to the anonymous peer reviewers whose comments and constructive criticism gave greater focus to this final version of the article.
Note. The article’s contents are solely the responsibility of the author and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Human Participant Protection
Institutional review board approval was not necessary for this article deals with the development of theory based on the discussion of the investigators. The study, Community Based Participatory Research to Improve Health in Children, fomented the faculty, student, and community conversations that resulted in this article. It was approved by the committee to protect humans in research studies of the University of Puerto Rico, Mayagüez Campus.
References
- 1.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available at: http://www.cdc.gov/nchs/nhanes.htm. Accessed September 29, 2014.
- 2.Flegal KM. Commentary: the epidemic of obesity—what’s in a name? Int J Epidemiol. 2006;35(1):72–74. doi: 10.1093/ije/dyi260. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. Int J Obes Relat Metab Disord. 2000;24(7):807–818. doi: 10.1038/sj.ijo.0801232. [DOI] [PubMed] [Google Scholar]
- 4.Keys A, Brožek J, Henschel A, Mickelsen O, Taylor HL. The Biology of Human Starvation. I and II. Minneapolis, MN: University of Minnesota Press; 1950. [Google Scholar]
- 5.Speakman JR, Levitsky DA, Allison DB et al. Set point, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis Model Mech. 2011;4(6):733–745. doi: 10.1242/dmm.008698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ochner CN, Barrios DM, Lee CD, Pi-Sunyer FX. Biological mechanisms that promote weight regain following weight loss in obese humans. Physiol Behav. 2013;120:106–113. doi: 10.1016/j.physbeh.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polivy J, Herman CP. Dieting and bingeing: a causal analysis. Am Psychol. 1985;40(2):193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- 8.Mayer J. Overweight: Causes, Cost, and Control. Englewood Cliffs, NJ: Prentice-Hall Inc; 1968. [Google Scholar]
- 9.Huenemann RL, Shapiro LR, Hampton MC, Mitchell BW. A longitudinal study of gross body composition and body conformation and their association with food and activity in a teen-age population. Views of teen-age subjects on body conformation, food and activity. Am J Clin Nutr. 1966;18(5):325–338. doi: 10.1093/ajcn/18.5.325. [DOI] [PubMed] [Google Scholar]
- 10.Garner DM, Garfinkel PE, Schwartz D, Thompson M. Cultural expectations of thinness in women. Psychol Rep. 1980;47(2):483–491. doi: 10.2466/pr0.1980.47.2.483. [DOI] [PubMed] [Google Scholar]
- 11.Rodin J, Silberstein L, Striegel-Moore R. Women and weight: a normative discontent. Nebr Symp Motiv. 1984;32:267–307. [PubMed] [Google Scholar]
- 12.Franklin JC, Schiele BC, Brozek J, Keys A. Observations on human behavior in experimental semi-starvation and rehabilitation. J Clin Psychol. 1948;4(1):28–45. doi: 10.1002/1097-4679(194801)4:1<28::aid-jclp2270040103>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 13.Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 14.Wolfe BE, Baker CW, Smith AT, Kelly-Weeder S. Validity and utility of the current definition of binge eating. Int J Eat Disord. 2009;42(8):674–686. doi: 10.1002/eat.20728. [DOI] [PubMed] [Google Scholar]
- 15.Latner JD, Clyne C. The diagnostic validity of the criteria for binge eating disorder. Int J Eat Disord. 2008;41(1):1–14. doi: 10.1002/eat.20465. [DOI] [PubMed] [Google Scholar]
- 16.Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG. The validity and clinical utility of binge eating disorder. Int J Eat Disord. 2009;42(8):687–705. doi: 10.1002/eat.20719. [DOI] [PubMed] [Google Scholar]
- 17.Wilson GT, Sysko R. Frequency of binge eating episodes in bulimia nervosa and binge eating disorder: diagnostic considerations. Int J Eat Disord. 2009;42(7) doi: 10.1002/eat.20726. 7:603–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Hoeken D, Veling W, Sinke S, Mitchell JE, Hoek HW. The validity and utility of subtyping bulimia nervosa. Int J Eat Disord. 2009;42(7):595–602. doi: 10.1002/eat.20724. [DOI] [PubMed] [Google Scholar]
- 19.National Task Force on the Prevention and Treatment of Obesity. Dieting and the development of eating disorders in overweight and obese adults. Arch Intern Med. 2000;160(17):2581–2589. doi: 10.1001/archinte.160.17.2581. [DOI] [PubMed] [Google Scholar]
- 20.Lowe MR, Thomas JG, Safer DL, Butryn ML. The relationship of weight suppression and dietary restraint to binge eating in bulimia nervosa. Int J Eat Disord. 2007;40(7):640–644. doi: 10.1002/eat.20405. [DOI] [PubMed] [Google Scholar]
- 21.Butryn ML, Juarascio A, Lowe MR. The relation of weight suppression and BMI to bulimic symptoms. Int J Eat Disord. 2011;44(7):612–617. doi: 10.1002/eat.20881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herzog DB, Thomas JG, Kass AE, Eddy KT, Franko DL, Lowe MR. Weight suppression predicts weight gain over 5 years in bulimia nervosa. Psychiatry Res. 2010;177(3):330–334. doi: 10.1016/j.psychres.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keel PK, Heatherton TF. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. J Abnorm Psychol. 2010;119(2):268–275. doi: 10.1037/a0019190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hagan MM, Whitworth RH, Moss DE. Semistarvation-associated eating behaviors among college binge eaters: a preliminary description and assessment scale. Behav Med. 1999;25(3):125–133. doi: 10.1080/08964289909596742. [DOI] [PubMed] [Google Scholar]
- 25.Hagan MM, Shuman ES, Oswald KD et al. Incidence of chaotic eating behaviors in binge-eating disorder: contributing factors. Behav Med. 2002;28(3):99–105. doi: 10.1080/08964280209596048. [DOI] [PubMed] [Google Scholar]
- 26.Sibilia L. The cognition of hunger and eating behaviours. Psychol Topics. 2010;19(2):341–354. [Google Scholar]
- 27.Cerrato M, Carrera O, Vazquez R, Echevarría E, Gutierrez E. Heat makes a difference in activity-based anorexia: a translational approach to treatment development in anorexia nervosa. Int J Eat Disord. 2012;45(1):26–35. doi: 10.1002/eat.20884. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer RL, Yanovski S, Wadden T et al. Binge eating disorder: its further validation in a multisite study. Int J Eat Disord. 1993;13(2):137–153. [PubMed] [Google Scholar]
- 29.Castellini G, Lelli L, Lo Sauro C et al. Anorectic and bulimic patients suffer from relevant sexual dysfunctions. J Sex Med. 2012;9(10):2590–2599. doi: 10.1111/j.1743-6109.2012.02888.x. [DOI] [PubMed] [Google Scholar]
- 30.Boggiano MM, Turan B, Maldonado CR, Oswald KD, Shuman ES. Secretive food concocting in binge eating: test of a famine hypothesis. Int J Eat Disord. 2013;46(3):212–225. doi: 10.1002/eat.22077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tomeo CA, Field AE, Berkey CS, Colditz GA, Frazier AL. Weight concerns, weight control behaviors, and smoking initiation. Pediatrics. 1999;104(4 pt 1):918–924. doi: 10.1542/peds.104.4.918. [DOI] [PubMed] [Google Scholar]
- 32.Kendzor DE, Adams CE, Stewart DW, Baillie LE, Copeland AL. Cigarette smoking is associated with body shape concerns and bulimia symptoms among young adult females. Eat Behav. 2009;10(1):56–58. doi: 10.1016/j.eatbeh.2008.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Green MW, Rogers PJ, Elliman NA, Gatenby SJ. Impairment of cognitive performance associated with dieting and high levels of dietary restraint. Physiol Behav. 1994;55(3):447–452. doi: 10.1016/0031-9384(94)90099-x. [DOI] [PubMed] [Google Scholar]
- 34.Billingsley-Marshall RL, Basso MR, Lund BC et al. Executive function in eating disorders: the role of state anxiety. Int J Eat Disord. 2013;46(4):316–321. doi: 10.1002/eat.22086. [DOI] [PubMed] [Google Scholar]
- 35.Kemps E, Tiggemann M, Marshall K. Relationship between dieting to lose weight and the functioning of the central executive. Appetite. 2005;45(3):287–294. doi: 10.1016/j.appet.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 36.D’Anci KE, Watts KL, Kanarek RB, Taylor HA. Low-carbohydrate weight-loss diets. Effects on cognition and mood. Appetite. 2009;52(1):96–103. doi: 10.1016/j.appet.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 37.Hatch A, Madden S, Kohn MR et al. In first presentation adolescent anorexia nervosa, do cognitive markers of underweight status change with weight gain following a refeeding intervention? Int J Eat Disord. 2010;43(4):295–306. doi: 10.1002/eat.20695. [DOI] [PubMed] [Google Scholar]
- 38.Arias Horcajadas F, Sánchez Romero S, Gorgojo Martínez JJ, Almodóvar Ruiz F, Fernández Rojo S, Llorente Martin F. Clinical differences between morbid obese patients with and without binge eating. Actas Esp Psiquiatr. 2006;34(6):362–370. [PubMed] [Google Scholar]
- 39.Fairburn CG, Harrison PJ. Eating disorders. Lancet. 2003;361(9355):407–416. doi: 10.1016/S0140-6736(03)12378-1. [DOI] [PubMed] [Google Scholar]
- 40.Rieger E, Wilfley DE, Stein RI, Marino V, Crow SJ. A comparison of quality of life in obese individuals with and without binge eating disorder. Int J Eat Disord. 2005;37(3):234–240. doi: 10.1002/eat.20101. [DOI] [PubMed] [Google Scholar]
- 41.Pinheiro AP, Raney TJ, Thornton LM et al. Sexual functioning in women with eating disorders. Int J Eat Disord. 2010;43(2):123–129. doi: 10.1002/eat.20671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rodríguez S, Mata JL, Lameiras M, Fernández MC, Vila J. Dyscontrol evoked by erotic and food images in women with bulimia nervosa. Eur Eat Disord Rev. 2007;15(3):231–239. doi: 10.1002/erv.724. [DOI] [PubMed] [Google Scholar]
- 43.Goossens L, Braet C, Van Vlierberghe L, Mels S. Loss of control over eating in overweight youngsters: the role of anxiety, depression and emotional eating. Eur Eat Disord Rev. 2009;17(1):68–78. doi: 10.1002/erv.892. [DOI] [PubMed] [Google Scholar]
- 44.Striegel RH, Bedrosian R, Wang C, Schwartz S. Why men should be included in research on binge eating: results from a comparison of psychosocial impairment in men and women. Int J Eat Disord. 2012;45(2):233–240. doi: 10.1002/eat.20962. [DOI] [PubMed] [Google Scholar]
- 45.Whisman MA, Dementyeva A, Baucom DH, Bulik CM. Marital functioning and binge eating disorder in married women. Int J Eat Disord. 2012;45(3):385–389. doi: 10.1002/eat.20935. [DOI] [PubMed] [Google Scholar]
- 46.Brownstone LM, Bardone-Cone AM, Fitzsimmons-Craft EE et al. Subjective and objective binge eating in relation to eating disorder symptomatology, negative affect, and personality dimensions. Int J Eat Disord. 2013;46(1):66–76. doi: 10.1002/eat.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Striegel RH, Bedrosian R, Wang C. Comparing work productivity in obesity and binge eating. Int J Eat Disord. 2012;45(8):995–998. doi: 10.1002/eat.22069. [DOI] [PubMed] [Google Scholar]
- 48.Allison KC, Grilo CM, Masheb RM, Stunkard AJ. Binge eating disorder and night eating syndrome: a comparative study of disordered eating. J Consult Clin Psychol. 2005;73(6):1107–1115. doi: 10.1037/0022-006X.73.6.1107. [DOI] [PubMed] [Google Scholar]
- 49.Phelan S, Hill JO, Lang W, Dibello JR, Wing RR. Recovery from relapse among successful weight maintainers. Am J Clin Nutr. 2003;78(6):1079–1084. doi: 10.1093/ajcn/78.6.1079. [DOI] [PubMed] [Google Scholar]
- 50.Czerniawski AM. From average to ideal. The evolution of the height and weight table in the United States, 1836–1943. Soc Sci Hist. 2007;31(2):273–296. [Google Scholar]
- 51.National Institutes of Health. How are overweight and obesity diagnosed? Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/obe/diagnosis.html. Accessed October 3, 2014.
- 52.National Institutes of Health. How are overweight and obesity treated? Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/obe/treatment.html. Accessed October 3, 2014.
- 53.Crawford D, Campbell K. Lay definitions of ideal weight and overweight. Int J Obes Relat Metab Disord. 1999;23(7):738–745. doi: 10.1038/sj.ijo.0800922. [DOI] [PubMed] [Google Scholar]
- 54.Voracek M, Fisher ML. Shapely centrefolds? Temporal change in body measures: trend analysis. BMJ. 2002;325(7378):1447–1448. doi: 10.1136/bmj.325.7378.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ottati V, Bodenhausen GV, Newman LS. Social psychological models of mental illness stigma. In: Corrigan PW, editor. On the Stigma of Mental Illness: Practical Strategies for Research and Social Change. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- 56.Corrigan PW, Kleinlein P. The impact of mental illness stigma. In: Corrigan PW, editor. On the Stigma of Mental Illness: Practical Strategies for Research and Social Change. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- 57.Puhl RM, Moss-Racusin CA, Schwartz MB. Internalization of weight bias: implications for binge eating and emotional well-being. Obesity (Silver Spring) 2007;15(1):19–23. doi: 10.1038/oby.2007.521. [DOI] [PubMed] [Google Scholar]
- 58.Link BG, Phelan JC. On stigma and its public health implications. Paper presented at: Stigma and Global Health: Developing a Research Agenda; September 6, 2001; Bethesda, MD. Available at: http://www.stigmaconference.nih.gov/FinalLinkPaper.html. Accessed July 12, 2010.
- 59.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329(14):1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 60.Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008;23(2):347–358. doi: 10.1093/her/cym052. [DOI] [PubMed] [Google Scholar]
- 61.Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes (Lond) 2008;32(6):992–1000. doi: 10.1038/ijo.2008.22. [DOI] [PubMed] [Google Scholar]
- 62.Vartanian LR, Smyth JM. Primum non nocere: obesity stigma and public health. J Bioeth Inq. 2013;10(1):49–57. doi: 10.1007/s11673-012-9412-9. [DOI] [PubMed] [Google Scholar]
- 63.Puhl RM. Weight stigmatization toward youth: a significant problem in need of societal solutions. Child Obes. 2011;7(5):359–363. [Google Scholar]
- 64.Holub SC. Individual differences in the anti-fat attitudes of preschool children. The importance of perceived body size. Body Image. 2008;5(3):317–321. doi: 10.1016/j.bodyim.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 65.Richardson SA, Goodman N, Hastorf AH, Dornbusch SM. Cultural uniformity in reaction to physical disabilities. Am Sociol Rev. 1961;26(2):241–247. [Google Scholar]
- 66.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obes Res. 2003;11(3):452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- 67.Latner JD, Stunkard AJ, Wilson GT. Stigmatized students: age, sex, and ethnicity effects in the stigmatization of obesity. Obes Res. 2005;13(7):1226–1231. doi: 10.1038/oby.2005.145. [DOI] [PubMed] [Google Scholar]
- 68.Hebl MR, Ruggs EN, Singletary SL, Beal DJ. Perceptions of obesity across the lifespan. Obesity (Silver Spring) 2008;16(suppl 2):S46–S52. doi: 10.1038/oby.2008.458. [DOI] [PubMed] [Google Scholar]
- 69.O’Brien KS, Hunter JA, Banks M. Implicit anti-fat bias in physical educators: physical attributes, ideology and socialization. Int J Obes (Lond) 2007;31(2):308–314. doi: 10.1038/sj.ijo.0803398. [DOI] [PubMed] [Google Scholar]
- 70.Zeller MH, Reiter-Purtill J, Ramey C. Negative peer perceptions of obese children in the classroom environment. Obesity (Silver Spring) 2008;16(4):755–762. doi: 10.1038/oby.2008.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133(4):557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 72.Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment bias. J Am Diet Assoc. 2009;109(3):438–444. doi: 10.1016/j.jada.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 73.Puhl RM, Heuer CA. The stigma of obesity: a review and an update. Obesity (Silver Spring) 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 74.Malterud K, Ulriksen K. Obesity, stigma, and responsibility in health care: a synthesis of qualitative studies. Int J Qual Stud Health Well-being. 2011;6:8404. doi: 10.3402/qhw.v6i4.8404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25(10):1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 76.Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11(9):1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 77.Bissell K, Hays H. Understanding anti-fat bias in children: the role of media and appearance anxiety in third to sixth graders’ implicit and explicit attitudes towards obesity. Mass Commun Soc. 2011;14:113–140. [Google Scholar]
- 78.Lumeng JC, Forrest P, Appugliese DP, Kaciroti N, Corwyn RF, Bradley RH. Weight status as a predictor of being bullied in third through sixth grades. Pediatrics. 2010;125(6):e1301–e1307. doi: 10.1542/peds.2009-0774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Libbey HP, Story MT, Neumark-Sztainer DR, Boutelle KN. Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity (Silver Spring) 2008;16(suppl 2):S24–S29. doi: 10.1038/oby.2008.455. [DOI] [PubMed] [Google Scholar]
- 80.van den Berg P, Neumark-Sztainer D, Eisenberg ME, Haines J. Racial/ethnic differences in weight-related teasing in adolescents. Obesity (Silver Spring) 2008;16(suppl 2):S3–S10. doi: 10.1038/oby.2008.445. [DOI] [PubMed] [Google Scholar]
- 81.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.van den Berg P, Neumark-Sztainer D. Fat ’n happy 5 years later: is it bad for overweight girls to like their bodies? J Adolesc Health. 2007;41(4):415–417. doi: 10.1016/j.jadohealth.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 83.Sutin AR, Terracciano A. Perceived weight discrimination and obesity. PLoS One. 2013;8(7):e70048. doi: 10.1371/journal.pone.0070048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Greenberg BS, Eastin M, Hofschire L, Lachlan K, Brownell KD. Portrayals of overweight and obese individuals on commercial television. Am J Public Health. 2003;93(8):1342–1348. doi: 10.2105/ajph.93.8.1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fouts G, Burggraf K. Television situation comedies: female weight, male negative comments, and audience reactions. Sex Roles. 2000;42(9/10):925–932. [Google Scholar]
- 86.Groesz LM, Levine MP, Murnen SK. The effect of experimental presentation of thin media images on body satisfaction: a meta-analytic review. Int J Eat Disord. 2002;31(1):1–16. doi: 10.1002/eat.10005. [DOI] [PubMed] [Google Scholar]
- 87.Neumark-Sztainer D, Wall M, Story M, Sherwood NE. Five-year longitudinal predictive factors for disordered eating in a population-based sample of overweight adolescents: implications for prevention and treatment. Int J Eat Disord. 2009;42(7):664–672. doi: 10.1002/eat.20733. [DOI] [PubMed] [Google Scholar]
- 88.van den Berg P, Neumark-Sztainer D, Hannan PJ, Haines J. Is dieting advice from magazines helpful or harmful? Five-year associations with weight-control behaviors and psychological outcomes in adolescents. Pediatrics. 2007;119(1):e30–e37. doi: 10.1542/peds.2006-0978. [DOI] [PubMed] [Google Scholar]
- 89.Harris JL, Brownell KD, Bargh JA. The food marketing defense model: integrating psychological research to protect youth and inform public policy. Soc Issues Policy Rev. 2009;3(1):211–271. doi: 10.1111/j.1751-2409.2009.01015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tremblay L, Limbos M. Body image disturbance and psychopathology in children: research evidence and implications for prevention and treatment. Curr Psychiatry Rev. 2009;5(1):62–72. [Google Scholar]
- 91.Kurth BM, Ellert U. Perceived or true obesity: which causes more suffering in adolescents? Findings of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Dtsch Arztebl Int. 2008;105(23):406–412. doi: 10.3238/arztebl.2008.0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Viner RM, Haines MM, Taylor SJC, Head J, Booy R, Stansfeld S. Body mass, weight control behaviours, weight perceptions and emotional well being in a multiethnic sample of early adolescents. Int J Obes (Lond) 2006;30(10):1514–1521. doi: 10.1038/sj.ijo.0803352. [DOI] [PubMed] [Google Scholar]
- 93.ter Bogt TF, van Dorsselaer SA, Monshouwer K, Verdurmen JE, Engels RC, Vollebergh WA. Body mass index and body weight perception as risk factors for internalizing and externalizing problem behavior among adolescents. J Adolesc Health. 2006;39(1):27–34. doi: 10.1016/j.jadohealth.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 94.Paeratakul S, White MA, Williamson DA, Ryan DH, Bray GA. Sex, race/ethnicity, socioeconomic status, and BMI in relation to self-perception of overweight. Obes Res. 2002;10(5):345–350. doi: 10.1038/oby.2002.48. [DOI] [PubMed] [Google Scholar]
- 95.Jones M, Grilo CM, Masheb RM, White MA. Psychological and behavioral correlates of excess weight: misperception of obese status among persons with class II obesity. Int J Eat Disord. 2010;43(7):628–632. doi: 10.1002/eat.20746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shunk JA, Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. J Am Diet Assoc. 2004;104(7):1120–1126. doi: 10.1016/j.jada.2004.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tanofsky-Kraff M, Cohen ML, Yanovski SZ et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117(4):1203–1209. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Field AE, Austin SB, Taylor CB et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112(4):900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- 99.Stice E, Cameron RP, Killen JD, Hayward C, Barr Taylor C. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol. 1999;67(6):967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- 100.Stice E, Presnell K, Shaw H, Rohde P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J Consult Clin Psychol. 2005;73(2):195–202. doi: 10.1037/0022-006X.73.2.195. [DOI] [PubMed] [Google Scholar]
- 101.Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc. 2006;106(4):559–568. doi: 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 102.Coakley EH, Rimm EB, Colditz G, Kawachi I, Willett W. Predictors of weight change in men: results from the Health Professionals Follow-up Study. Int J Obes Relat Metab Disord. 1998;22(2):89–96. doi: 10.1038/sj.ijo.0800549. [DOI] [PubMed] [Google Scholar]
- 103.Cuypers K, Kvaløy K, Bratberg G, Midthjell K, Holmen J, Holmen TL. Being normal weight but feeling overweight in adolescence may affect weight development into young adulthood—an 11-year followup: the HUNT study, Norway. J Obes. 2012;2012:601872. doi: 10.1155/2012/601872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Neumark-Sztainer D, Wall M, Story M, Standish AR. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. J Adolesc Health. 2012;50(1):80–86. doi: 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pietiläinen KH, Saarni SE, Kaprio J, Rissanen A. Does dieting make you fat? A twin study. Int J Obesity (Lond) 2012;36(3):456–464. doi: 10.1038/ijo.2011.160. [DOI] [PubMed] [Google Scholar]
- 106.Savage JS, Hoffman L, Birch LL. Dieting, restraint, and disinhibition predict women’s weight change over 6 y. Am J Clin Nutr. 2009;90(1):33–40. doi: 10.3945/ajcn.2008.26558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Korkeila M, Rissanen A, Kaprio J, Sørensen TIA, Koskenvuo M. Weight-loss attempts and risk of major weight gain: a prospective study in Finnish adults. Am J Clin Nutr. 1999;70(6):965–975. doi: 10.1093/ajcn/70.6.965. [DOI] [PubMed] [Google Scholar]
- 108.Field AE, Manson JE, Taylor CB, Willett WC, Colditz GA. Association of weight change, weight control practices, and weight cycling among women in the Nurses’ Health Study II. Int J Obes Relat Metab Disord. 2004;28(9):1134–1142. doi: 10.1038/sj.ijo.0802728. [DOI] [PubMed] [Google Scholar]
- 109.Stevens VL, Jacobs EJ, Sun J et al. Weight cycling and mortality in a large prospective US study. Am J Epidemiol. 2012;175(8):785–792. doi: 10.1093/aje/kwr378. [DOI] [PubMed] [Google Scholar]
- 110.Saarni SE, Rissanen A, Sarna S, Koskenvuo M, Kaprio J. Weight cycling of athletes and subsequent weight gain in middleage. Int J Obes (Lond) 2006;30(11):1639–1644. doi: 10.1038/sj.ijo.0803325. [DOI] [PubMed] [Google Scholar]
- 111.Neumark-Sztainer D, Paxton SJ, Hannan PJ, Haines J, Story M. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J Adolesc Health. 2006;39(2):244–251. doi: 10.1016/j.jadohealth.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 112.Senf JH, Shisslak CM, Crago MA. Does dieting lead to weight gain? A four-year longitudinal study of middle school girls. Obesity (Silver Spring) 2006;14(12):2236–2241. doi: 10.1038/oby.2006.262. [DOI] [PubMed] [Google Scholar]
- 113.French SA, Jeffery RW, Murray D. Is dieting good for you?: prevalence, duration and associated weight and behaviour changes for specific weight loss strategies over four years in US adults. Int J Obes Relat Metab Disord. 1999;23(3):320–327. doi: 10.1038/sj.ijo.0800822. [DOI] [PubMed] [Google Scholar]
- 114.Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Public Health. 1999;89(5):747–751. doi: 10.2105/ajph.89.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Marquet L-A, Brown M, Tafflet M et al. No effect of weight cycling on the post-career BMI of weight class elite athletes. BMC Public Health. 2013;13(1):510. doi: 10.1186/1471-2458-13-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Nitzke SA, Voichick SJ, Olson D. Weight cycling practices and long-term health conditions in a sample of former wrestlers and other collegiate athletes. J Athl Train. 1992;27(3):257–261. [PMC free article] [PubMed] [Google Scholar]
- 117.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–341. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 118.Mann T, Tomiyama AJ, Westling E, Lew A-M, Samuels B, Chatman J. Medicare’s search for effective obesity treatments: diets are not the answer. Am Psychol. 2007;62(3):220–233. doi: 10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]
- 119.Look AHEAD Research Group. Wadden TA, West DS et al. The Look AHEAD Study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring) 2006;14(5):737–752. doi: 10.1038/oby.2006.84. [erratum in Obesity (Silver Spring). 2007;15(5):1339] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD Study. Obesity (Silver Spring) 2014;22(1):5–13. doi: 10.1002/oby.20662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Look AHEAD Research Group. Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566–1575. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Look AHEAD Research Group. Wing RR, Bolin P et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369(2):145–154. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Haeffele J, Trunnell EP, Kinney A. A grounded theory approach to the process of successful and advanced weight maintenance. Int J Health Wellness Soc. 2011;1(3):43–54. [Google Scholar]
- 124.Hindle L, Carpenter C. An exploration of the experiences and perceptions of people who have maintained weight loss. J Hum Nutr Diet. 2011;24(4):342–350. doi: 10.1111/j.1365-277X.2011.01156.x. [DOI] [PubMed] [Google Scholar]
- 125.Reyes NR, Oliver TL, Klotz AA et al. Similarities and differences between weight loss maintainers and regainers: a qualitative analysis. J Acad Nutr Diet. 2012;112(4):499–505. doi: 10.1016/j.jand.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 126.Chambers JA, Swanson V. Stories of weight management: factors associated with successful and unsuccessful weight maintenance. Br J Health Psychol. 2012;17(2):223–243. doi: 10.1111/j.2044-8287.2011.02030.x. [DOI] [PubMed] [Google Scholar]
- 127.Neumark-Sztainer D, van den Berg P, Hannan PJ, Story M. Self-weighing in adolescents: helpful or harmful? Longitudinal associations with body weight changes and disordered eating. J Adolesc Health. 2006;39(6):811–818. doi: 10.1016/j.jadohealth.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 128.Grilo CM, Reas DL, Brody ML, Burke-Martindale CH, Rothschild BS, Masheb RM. Body checking and avoidance and the core features of eating disorders among obese men and women seeking bariatric surgery. Behav Res Ther. 2005;43(5):629–637. doi: 10.1016/j.brat.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 129.Goodwin H, Haycraft E, Willis A-M, Meyer C. Compulsive exercise: the role of personality, psychological morbidity, and disordered eating. Int J Eat Disord. 2011;44(7):655–660. doi: 10.1002/eat.20902. [DOI] [PubMed] [Google Scholar]
- 130.Spurrell EB, Wilfley DE, Tanofsky MB, Brownell KD. Age of onset for binge eating: are there different pathways to binge eating? Int J Eat Disord. 1997;21(1):55–65. doi: 10.1002/(sici)1098-108x(199701)21:1<55::aid-eat7>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 131.Grilo CM, Masheb RM. Onset of dieting vs. binge eating in outpatients with binge eating disorder. Int J Obes Relat Metab Disord. 2000;24(4):404–409. doi: 10.1038/sj.ijo.0801171. [DOI] [PubMed] [Google Scholar]
- 132.Reas DL, Grilo CM. Timing and sequence of the onset of overweight, dieting, and binge eating in overweight patients with binge eating disorder. Int J Eat Disord. 2007;40(2):165–170. doi: 10.1002/eat.20353. [DOI] [PubMed] [Google Scholar]
- 133.Roehrig M, Masheb RM, White MA, Grilo CM. Dieting frequency in obese patients with binge eating disorder: behavioral and metabolic correlates. Obesity (Silver Spring) 2009;17(4):689–697. doi: 10.1038/oby.2008.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bulik CM, Sullivan PF, Carter FA, Joyce PR. Initial manifestations of disordered eating behavior: dieting versus bingeing. Int J Eat Disord. 1997;22(2):195–201. doi: 10.1002/(sici)1098-108x(199709)22:2<195::aid-eat12>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 135.Pederson Mussell M, Mitchell JE, Fenna CJ, Crosby RD, Miller JP, Hoberman HM. A comparison of onset of binge eating versus dieting in the development of bulimia nervosa. Int J Eat Disord. 1997;21(4):353–360. doi: 10.1002/(sici)1098-108x(1997)21:4<353::aid-eat8>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 136.Haiman C, Devlin MJ. Binge eating before the onset of dieting: a distinct subgroup of bulimia nervosa? Int J Eat Disord. 1999;25(2):151–157. doi: 10.1002/(sici)1098-108x(199903)25:2<151::aid-eat4>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 137.Brewerton TD, Dansky BS, Kilpatrick DG, O’Neill PM. Which comes first in the pathogenesis of bulimia nervosa: dieting or bingeing? Int J Eat Disord. 2000;28(3):259–264. doi: 10.1002/1098-108x(200011)28:3<259::aid-eat2>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 138.Binford RB, Pederson Mussell M, Peterson CB, Crow SJ, Mitchell JE. Relation of binge eating age of onset to functional aspects of binge eating in binge eating disorder. Int J Eat Disord. 2004;35(3):286–292. doi: 10.1002/eat.10272. [DOI] [PubMed] [Google Scholar]
- 139.Manwaring JL, Hilbert A, Wilfley DE et al. Risk factors and patterns of onset in binge eating disorder. Int J Eat Disord. 2006;39(2):101–107. doi: 10.1002/eat.20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Carrard I, Van der Linden M, Golay A. Comparison of obese and nonobese individuals with binge eating disorder: delicate boundary between binge eating disorder and non-purging bulimia nervosa. Eur Eat Disord Rev. 2012;20(5):350–354. doi: 10.1002/erv.2174. [DOI] [PubMed] [Google Scholar]
- 141.Shomaker LB, Tanofsky-Kraff M, Savastano DM et al. Puberty and observed energy intake: boy, can they eat! Am J Clin Nutr. 2010;92(1):123–129. doi: 10.3945/ajcn.2010.29383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.McCrone S, Dennis K, Tomoyasu N, Carroll J. A profile of early versus late onset of obesity in postmenopausal women. J Womens Health Gend Based Med. 2000;9(9):1007–1013. doi: 10.1089/15246090050200042. [DOI] [PubMed] [Google Scholar]
- 143.Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA. The perceived onset of dieting and loss of control eating behaviors in overweight children. Int J Eat Disord. 2005;38(2):112–122. doi: 10.1002/eat.20158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tanofsky-Kraff M, Shomaker LB, Olsen C et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120(1):108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shomaker LB, Tanofsky-Kraff M, Elliott C et al. Salience of loss of control for pediatric binge episodes: does size really matter? Int J Eat Disord. 2010;43(8):707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Whiteside U, Chen E, Neighbors C, Hunter D, Lo T, Larimer M. Difficulties regulating emotions: do binge eaters have fewer strategies to modulate and tolerate negative affect? Eat Behav. 2007;8(2):162–169. doi: 10.1016/j.eatbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 147.Quinton S, Wagner HL. Alexithymia, ambivalence over emotional expression, and eating attitudes. Pers Individ Dif. 2005;38:1163–1173. [Google Scholar]
- 148.Mazzeo SE, Mitchell KS, Williams LJ. Anxiety, alexithymia, and depression as mediators of the association between childhood abuse and eating disordered behavior in African American and European American women. Psychol Women Q. 2008;32:267–280. [Google Scholar]
- 149.Goldschmidt A, Wilfley DE, Eddy KT et al. Overvaluation of shape and weight among children and adolescents with loss of control eating. Behav Res Ther. 2011;49(10):682–688. doi: 10.1016/j.brat.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Goldschmidt AB, Jones M, Manwaring JL et al. The clinical significance of loss of control over eating in overweight adolescents. Int J Eat Disord. 2008;41(2):153–158. doi: 10.1002/eat.20481. [DOI] [PubMed] [Google Scholar]
- 151.Czaja J, Rief W, Hilbert A. Emotion regulation and binge eating in children. Int J Eat Disord. 2009;42(4):356–362. doi: 10.1002/eat.20630. [DOI] [PubMed] [Google Scholar]
- 152.Ogden CL, Kuczmarski RJ, Flegal KM et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 153.Tillmann V, Thalange NK, Foster PJ, Gill MS, Price DA, Clayton PE. The relationship between stature, growth, and short-term changes in height and weight in normal prepubertal children. Pediatr Res. 1998;44(6):882–886. doi: 10.1203/00006450-199812000-00010. [DOI] [PubMed] [Google Scholar]
- 154.Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51(3):170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tanner JM. Normal growth and techniques of growth assessment. Clin Endocrinol Metab. 1986;15(3):411–451. doi: 10.1016/s0300-595x(86)80005-6. [DOI] [PubMed] [Google Scholar]
- 156. Professor James Tanner. Obituary. The Telegraph. October 20, 2010. Available at: http://www.telegraph.co.uk/news/obituaries/science-obituaries/8076525/Professor-James-Tanner.html. Accessed November 5, 2014.
- 157.Tanner JM, Taylor GR. Growth. New York, NY: Time Life Books; 1969. [Google Scholar]
- 158.Rogol AD, Roemmich JN, Clark PA. Growth at puberty. J Adolesc Health. 2002;31(6, suppl):192–200. doi: 10.1016/s1054-139x(02)00485-8. [DOI] [PubMed] [Google Scholar]
- 159.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59(5):955–959. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- 160.Centers for Disease Control and Prevention. Healthy weight—it’s not a diet, it’s a lifestyle. Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Accessed August 12, 2013.
- 161.Plachta-Danielzik S, Bosy-Westphal A, Kehden B et al. Adiposity rebound is misclassified by BMI rebound. Eur J Clin Nutr. 2013;67(9):984–989. doi: 10.1038/ejcn.2013.131. [DOI] [PubMed] [Google Scholar]
- 162.Uusi-Rasi K, Laaksonen M, Mikkilä V et al. Overweight in childhood and bone density and size in adulthood. Osteoporos Int. 2012;23(4):1453–1461. doi: 10.1007/s00198-011-1737-4. [DOI] [PubMed] [Google Scholar]
- 163.He Q, Karlberg J. BMI in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001;49(2):244–251. doi: 10.1203/00006450-200102000-00019. [DOI] [PubMed] [Google Scholar]
- 164.Stovitz SD, Demerath EW, Hannan PJ, Lytle LA, Himes JH. Growing into obesity: patterns of height growth in those who become normal weight, overweight, or obese as young adults. Am J Hum Biol. 2011;23(5):635–641. doi: 10.1002/ajhb.21191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wadden TA, Brown G, Foster GD, Linowitz JR. Salience of weight-related worries in adolescent males and females. Int J Eat Disord. 1991;10(4):407–414. [Google Scholar]
- 166.Karazsia BT, Crowther JH. Sociocultural and psychological links to men’s engagement in risky body change behaviors. Sex Roles. 2010;63:747–756. [Google Scholar]
- 167.Abraham S, Boyd C, Lal M, Luscombe G, Taylor A. Time since menarche, weight gain and body image awareness among adolescent girls: onset of eating disorders? J Psychosom Obstet Gynaecol. 2009;30(2):89–94. doi: 10.1080/01674820902950553. [DOI] [PubMed] [Google Scholar]
- 168.Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69(6):1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 169.Galloway AT, Fiorito LM, Francis LA, Birch LL. “Finish your soup”: counterproductive effects of pressuring children to eat on intake and affect. Appetite. 2006;46(3):318–323. doi: 10.1016/j.appet.2006.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Batsell WR, Jr, Brown AS, Ansfield ME, Paschall GY. “You will eat all of that!”: a retrospective analysis of forced consumption episodes. Appetite. 2002;38(3):211–219. doi: 10.1006/appe.2001.0482. [DOI] [PubMed] [Google Scholar]
- 171.Burdette HL, Whitaker RC, Hall WC, Daniels SR. Maternal infant-feeding style and children’s adiposity at 5 years of age. Arch Pediatr Adolesc Med. 2006;160(5):513–520. doi: 10.1001/archpedi.160.5.513. [DOI] [PubMed] [Google Scholar]
- 172.Stice E, Agras WS, Hammer LD. Risk factors for the emergence of childhood eating disturbances: a five-year prospective study. Int J Eat Disord. 1999;25(4):375–387. doi: 10.1002/(sici)1098-108x(199905)25:4<375::aid-eat2>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 173.Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr. 2002;76(1):226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78(2):215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent–child feeding strategies and their relationships to child eating and weight status. Obes Res. 2004;12(11):1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- 176.Francis LA, Birch LL. Maternal influences on daughters’ restrained eating behavior. Health Psychol. 2005;24(6):548–554. doi: 10.1037/0278-6133.24.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style: maternal and child characteristics. Appetite. 2001;37(3):231–243. doi: 10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- 178.Keller KL, Olsen A, Kuilema L, Meyermann K, van Belle C. Predictors of parental perceptions and concerns about child weight. Appetite. 2013;62:96–102. doi: 10.1016/j.appet.2012.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Berkowitz RI, Moore RH, Faith MS, Stallings VA, Kral TVE, Stunkard AJ. Identification of an obese eating style in 4-year-old children born at high and low risk for obesity. Obesity (Silver Spring) 2010;18(3):505–512. doi: 10.1038/oby.2009.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Carper JL, Fisher JO, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35(2):121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- 181.Steinberg E, Tanofsky-Kraff M, Cohen ML et al. Comparison of the child and parent forms of the Questionnaire on Eating and Weight Patterns in the assessment of children’s eating-disordered behaviors. Int J Eat Disord. 2004;36(2):183–194. doi: 10.1002/eat.20022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121(5):e1240–e1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- 183.Shin SH, Miller DP. A longitudinal examination of childhood maltreatment and adolescent obesity: results from the National Longitudinal Study of Adolescent Health (AddHealth) Study. Child Abuse Negl. 2012;36(2):84–94. doi: 10.1016/j.chiabu.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 184.Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. Am J Psychiatry. 2002;159(3):394–400. doi: 10.1176/appi.ajp.159.3.394. [DOI] [PubMed] [Google Scholar]
- 185.Noll JG, Zeller MH, Trickett PK, Putnam FW. Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics. 2007;120(1):e61–e67. doi: 10.1542/peds.2006-3058. [DOI] [PubMed] [Google Scholar]
- 186.Lissau I, Sørensen TI. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343(8893):324–327. doi: 10.1016/s0140-6736(94)91163-0. [DOI] [PubMed] [Google Scholar]
- 187.Groleau P, Steiger H, Bruce K et al. Childhood emotional abuse and eating symptoms in bulimic disorders: an examination of possible mediating variables. Int J Eat Disord. 2012;45(3):326–332. doi: 10.1002/eat.20939. [DOI] [PubMed] [Google Scholar]
- 188.Waller G, Corstorphine E, Mountford V. The role of emotional abuse in the eating disorders: implications for treatment. Eat Disord. 2007;15(4):317–331. doi: 10.1080/10640260701454337. [DOI] [PubMed] [Google Scholar]
- 189.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 190.Centers for Disease Control and Prevention. Child maltreatment. Available at: http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment. Accessed January 13, 2015.
- 191.Zeeck A, Stelzer N, Linster HW, Joos A, Hartmann A. Emotion and eating in binge eating disorder and obesity. Eur Eat Disord Rev. 2011;19(5):426–437. doi: 10.1002/erv.1066. [DOI] [PubMed] [Google Scholar]
- 192.Larsen JK, van Strien T, Eisinga R, Engels RC. Gender differences in the association between alexithymia and emotional eating in obese individuals. J Psychosom Res. 2006;60(3):237–243. doi: 10.1016/j.jpsychores.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 193.Baldaro B, Rossi N, Caterina R, Codispoti M, Balsamo A, Trombini G. Deficit in the discrimination of nonverbal emotions in children with obesity and their mothers. Int J Obes Relat Metab Disord. 2003;27(2):191–195. doi: 10.1038/sj.ijo.802228. [DOI] [PubMed] [Google Scholar]
- 194.Cooper MJ. Cognitive theory in anorexia and bulimia nervosa: progress, development and future directions. Clin Psychol Rev. 2005;25(4):511–531. doi: 10.1016/j.cpr.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 195.Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- 196.Decaluwé V, Braet C. The cogitive behavioural model for eating disorders: a direct evaluation in children and adolescents with obesity. Eat Behav. 2005;6(3):211–220. doi: 10.1016/j.eatbeh.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 197.Myers TA, Crowther JH. Social comparison as a predictor of body dissatisfaction: a meta-analytic review. J Abnorm Psychol. 2009;118(4):683–698. doi: 10.1037/a0016763. [DOI] [PubMed] [Google Scholar]
- 198.van den Berg P, Thompson JK, Obremski-Brandon K, Coovert M. The tripartite influence model of body image and eating disturbance: a covariance structural modeling investigation testing the mediational role of appearance comparison. J Psychosom Res. 2002;53(5):1007–1020. doi: 10.1016/s0022-3999(02)00499-3. [DOI] [PubMed] [Google Scholar]
- 199.Keery H, van den Berg P, Thompson JK. An evaluation of the tripartite influence model of body dissatisfaction and eating disturbances with adolescent girls. Body Image. 2004;1(3):237–251. doi: 10.1016/j.bodyim.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 200.Graff Low K, Charanasomboon S, Brown C, Hiltunen G, Long K, Reinhalter K. Internalization of the thin ideal, weight and body image concerns. Soc Behav Pers. 2003;31(1):81–90. [Google Scholar]
- 201.Forney KJ, Holland LA, Keel PK. Influence of peer context on the relationship between body dissatisfaction and eating pathology in women and men. Int J Eat Disord. 2012;45(8):982–989. doi: 10.1002/eat.22039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Eisenberg ME, Neumark-Sztainer D, Story M, Perry C. The role of social norms and friends’ influences on unhealthy weight-control behaviors among adolescent girls. Soc Sci Med. 2005;60(6):1165–1173. doi: 10.1016/j.socscimed.2004.06.055. [DOI] [PubMed] [Google Scholar]
- 203.Wadden TA, Foster GD, Sarwer DB et al. Dieting and the development of eating disorders in obese women: results of a randomized controlled trial. Am J Clin Nutr. 2004;80(3):560–568. doi: 10.1093/ajcn/80.3.560. [DOI] [PubMed] [Google Scholar]
- 204.Zandian M, Ioakimidis I, Bergh C, Södersten P. Cause and treatment of anorexia nervosa. Physiol Behav. 2007;92(1-2):283–290. doi: 10.1016/j.physbeh.2007.05.052. [DOI] [PubMed] [Google Scholar]
- 205.Shafran R, Fairburn CG, Nelson L, Robinson PH. The interpretation of severe dietary restraint. Behav Res Ther. 2003;41(8):887–894. doi: 10.1016/s0005-7967(02)00101-8. [DOI] [PubMed] [Google Scholar]
- 206.Braet C. Psychological profile to become and stay obese. Int J Obes (Lond) 2005;29(suppl 2):S19–S23. doi: 10.1038/sj.ijo.0803100. [DOI] [PubMed] [Google Scholar]
- 207.Ansell EB, Grilo CM, White MA. Examining the interpersonal model of binge eating and loss of control over eating in women. Int J Eat Disord. 2012;45(1):43–50. doi: 10.1002/eat.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Stice E, Maxfield J, Wells T. Adverse effects of social pressure to be thin on young women: an experimental investigation of the effects of “fat talk.”. Int J Eat Disord. 2003;34(1):108–117. doi: 10.1002/eat.10171. [DOI] [PubMed] [Google Scholar]
- 209.Bouchard C, Tremblay A, Després J-P et al. Response to long-term overfeeding in identical twins. N Engl J Med. 1990;322(21):1477–1482. doi: 10.1056/NEJM199005243222101. [DOI] [PubMed] [Google Scholar]
- 210.Haedt-Matt AA, Keel PK. Hunger and binge eating: a meta-analysis of studies using ecological momentary assessment. Int J Eat Disord. 2011;44(7):573–578. doi: 10.1002/eat.20868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder?: a prospective examination of precursors and consequences. Int J Eat Disord. 2007;40(3):195–203. doi: 10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- 212.Lowe MR, Kral TVE. Stress-induced eating in restrained eaters may not be caused by stress or restraint. Appetite. 2006;46(1):16–21. doi: 10.1016/j.appet.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 213.Lindberg SM, Grabe S, Hyde JS. Gender, pubertal development, and peer sexual harassment predict objectified body consciousness in early adolescence. J Res Adolesc. 2007;17(4):723–742. [Google Scholar]
- 214.Lowe MR. The effects of dieting on eating behavior: a three-factor model. Psychol Bull. 1993;114(1):100–121. doi: 10.1037/0033-2909.114.1.100. [DOI] [PubMed] [Google Scholar]
- 215.Lappalainen R, Pulkkinen P, van Gils M, Pärkkä J, Korhonen I. Long-term self-monitoring of weight: a case study. Cogn Behav Ther. 2005;34(2):108–114. doi: 10.1080/16506070510008452. [DOI] [PubMed] [Google Scholar]
- 216.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents. Implications for preventing weight-related disorders. Arch Pediatr Adolesc Med. 2002;156(2):171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]
- 217.Sim LA, Lebow J, Billings M. Eating disorders in adolescents with a history of obesity. Pediatrics. 2013;132(4):e1026–e1030. doi: 10.1542/peds.2012-3940. [DOI] [PubMed] [Google Scholar]
- 218.van der Ster Wallin G, Norring C, Holmgren S. Selective dieting patterns among anorectics and bulimics at the onset of eating disorder. Eur Eat Disord Rev. 1994;2(4):221–232. [Google Scholar]
- 219.Harrison K. Ourselves, our bodies: thin-ideal media, self-discrepancies, and eating disorder symptomatology in adolescents. J Soc Clin Psychol. 2001;20(3):289–323. [Google Scholar]
- 220.Utschig AC, Presnell K, Madeley MC, Smits JAJ. An investigation of the relationship between fear of negative evaluation and bulimic psychopathology. Eat Behav. 2010;11(4):231–238. doi: 10.1016/j.eatbeh.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 221.Bergh C, Brodin U, Lindberg G, Södersten P. Randomized controlled trial of a treatment for anorexia and bulimia nervosa. Proc Natl Acad Sci USA. 2002;99(14):9486–9491. doi: 10.1073/pnas.142284799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Heatherton TF, Herman CP, Polivy J, King GA, McGree ST. The (mis)measurement of restraint: an analysis of conceptual and psychometric issues. J Abnorm Psychol. 1988;97(1):19–28. doi: 10.1037//0021-843x.97.1.19. [DOI] [PubMed] [Google Scholar]
- 223.Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 224.van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5(2):295–315. [Google Scholar]
- 225.Stice E, Agras WS. Subtyping bulimic women along dietary restraint and negative affect dimensions. J Consult Clin Psychol. 1999;67(4):460–469. doi: 10.1037//0022-006x.67.4.460. [DOI] [PubMed] [Google Scholar]
- 226.Stice E, Agras WS, Telch CF, Halmi KA, Mitchell JE, Wilson T. Subtyping binge eating-disordered women along dieting and negative affect dimensions. Int J Eat Disord. 2001;30(1):11–27. doi: 10.1002/eat.1050. [DOI] [PubMed] [Google Scholar]
- 227.Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. J Abnorm Psychol. 2001;110(1):124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- 228.Bryant EJ, King NA, Blundell JE. Disinhibition: its effects on appetite and weight regulation. Obes Rev. 2007;9(5):409–419. doi: 10.1111/j.1467-789X.2007.00426.x. [DOI] [PubMed] [Google Scholar]
- 229.Davis C, Saltos E. Dietary recommendations and how they have changed over time. In: Frazão E, editor. America’s Eating Habits: Changes and Consequences. Agricultural Information Bulletin AIB-750. 1999. pp. 33–50. Available at: http://www.ers.usda.gov/publications/aib-agricultural-information-bulletin/aib750.aspx. Accessed August 31, 2013. [Google Scholar]
- 230.US Department of Agriculture, Center for Nutrition Policy and Promotion. Dietary Guidelines for Americans, 1980–2000. 2000. Available at: http://www.health.gov/dietaryguidelines/1980_2000_chart.pdf. Accessed August 26, 2013. [Google Scholar]
- 231.US Department of Health and Human Services, US Department of Agriculture. Dietary Guidelines for Americans, 2005. Available at: http://www.health.gov/dietaryguidelines/dga2005/document/default.htm. Accessed August 26, 2013. [Google Scholar]
- 232.US Department of Health and Human Services, US Department of Agriculture. Dietary Guidelines for Americans, 2010. Available at: http://www.cnpp.usda.gov/dietary-guidelines-2010. Accessed January 13, 2015. [Google Scholar]
- 233.Paul IM, Bartok CJ, Downs DS, Stifter CA, Ventura AK, Birch LL. Opportunities for the primary prevention of obesity during infancy. Adv Pediatr. 2009;56(1):107–133. doi: 10.1016/j.yapd.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Serdula MK, Williamson DF, Anda RF, Levy A, Heaton A, Byers T. Weight control practices in adults: results of a multistate telephone survey. Am J Public Health. 1994;84(11):1821–1824. doi: 10.2105/ajph.84.11.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Serdula MK, Mokdad AH, Williamson DF, Galuska DA, Mendlein JM, Heath GW. Prevalence of attempting weight loss and strategies for controlling weight. JAMA. 1999;282(14):1353–1358. doi: 10.1001/jama.282.14.1353. [DOI] [PubMed] [Google Scholar]
- 236.Bish CL, Blanck HM, Serdula MK, Marcus M, Kohl HW, III, Khan LK. Diet and physical activity behaviors among Americans trying to lose weight: 2000 Behavioral Risk Factor Surveillance System. Obes Res. 2005;13(3):596–607. doi: 10.1038/oby.2005.64. [DOI] [PubMed] [Google Scholar]
- 237.Market Enterprises Inc. The U.S. Weight Loss Market: 2014 Status Report & Forecast. Available at: https://www.marketresearch.com/Marketdata-Enterprises-Inc-v416/Weight-Loss-Status-Forecast-8016030. Accessed July 7, 2014. [Google Scholar]
- 238.Lattimore P, Fisher N, Malinowski P. A cross-sectional investigation of trait disinhibition and its association with mindfulness and impulsivity. Appetite. 2011;56(2):241–248. doi: 10.1016/j.appet.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 239.Framson C, Kristal AR, Schenk J, Littman AJ, Zeliadt S, Benitez D. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009;109(8):1439–1444. doi: 10.1016/j.jada.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Bombak A. Obesity, health at every size, and public policy. Am J Public Health. 2014;104(2):e60–e67. doi: 10.2105/AJPH.2013.301486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Satter E. Eating competence: definition and evidence for the Satter Eating Competence model. J Nutr Educ Behav. 2007;39(5, suppl):S142–S153. doi: 10.1016/j.jneb.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 242.Satter E. Eating competence: nutrition education with the Satter Eating Competence Model. [GEM No. 448.] J Nutr Educ Behav. 2007;39(5, suppl):S189–S194. doi: 10.1016/j.jneb.2007.04.177. [DOI] [PubMed] [Google Scholar]
- 243.Lohse B, Satter E, Horacek T, Gebreselassie T, Oakland MJ. Measuring eating competence: psychometric properties and validity of the ecSatter Inventory. J Nutr Educ Behav. 2007;39(5, suppl):S154–S166. doi: 10.1016/j.jneb.2007.04.371. [DOI] [PubMed] [Google Scholar]
- 244.Stotts JL, Lohse B. Reliability of the ecSatter Inventory as a tool to measure eating competence. J Nutr Educ Behav. 2007;39(5, suppl):S167–S170. doi: 10.1016/j.jneb.2007.03.091. [DOI] [PubMed] [Google Scholar]
- 245.Psota TL, Lohse B, West SG. Associations between eating competence and cardiovascular disease biomarkers. J Nutr Educ Behav. 2007;39(5, suppl):S171–S178. doi: 10.1016/j.jneb.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 246.Eneli IU, Crum PA, Tylka TL. The trust model: a different feeding paradigm for managing childhood obesity. Obesity (Silver Spring) 2008;16(10):2197–2204. doi: 10.1038/oby.2008.378. [DOI] [PubMed] [Google Scholar]
- 247.Schaefer JT, Magnuson AB. Review of interventions that promote eating by internal cues. J Acad Nutr Diet. 2014;114(5):734–760. doi: 10.1016/j.jand.2013.12.024. [DOI] [PubMed] [Google Scholar]