Abstract
Hennepin Health provides integrated medical and social services to low-income Medicaid patients in a large county located in Minneapolis, Minnesota. Data sharing is critical to program operations along with care coordination provided by community health workers. Early evidence indicates fewer emergency department visits and increased use of outpatient primary care. By focusing on prevention, coordination, and team-based care, the county hopes to improve individuals’ quality of life while reducing costs through better care management and reductions in emergency department use.
Hennepin Health represents a new model of integrated care targeted to low-income individuals with complex health and social needs—needs very similar to the Affordable Care Act Medicaid expansion population. The program is supported by enhanced data integration to better coordinate medical care with other needed social services in a capitated Accountable Care Organization (ACO) framework. The positive outcomes achieved and the ability to reinvest in the model have helped to garner political support and have motivated providers and care teams who see the opportunities to make a difference in the lives of a largely disenfranchised patient population. Hennepin Health provides an integrated care management model that other care plans can use to improve care and lower costs for the Medicaid expansion population under the Affordable Care Act.
INNOVATIVE COORDINATED CARE MODEL
Hennepin Health is an ACO made up of 4 county-affiliated organizations that jointly contract with the Minnesota Department of Human Services to provide Medicaid and social services to a population of 8700 members with incomes below 133% of the federal poverty level. Medicaid pays the ACO on a per-member, per-month basis, and partners share in all gains and losses associated with the program. The 4 organizations provide a range of health, mental health, social services, and claims processing services:
Hennepin County Human Services and Public Health Department, the county’s social services agency, public health department, and home to several clinical providers including health care for the homeless and the county’s mental health center,
Hennepin County Medical Center, an urban safety net health system, including a hospital, primary care, and specialty clinics,1
Metropolitan Health Plan, a county-operated not-for-profit health maintenance organization,2
NorthPoint Health & Wellness Center, a county-operated Federally Qualified Health Center.3
Hennepin County residents, when applying for Medicaid, select among participating health plans including Hennepin Health. Enrollees are autoassigned if no selection is made, and Hennepin Health is the default assignment for Hennepin County enrollees aged 21 to 64 years with incomes below 133% of the federal poverty level who do not have disability status. After enrollment, each new member is linked to a designated clinic that serves as the hub of their care coordination. The clinic is identified through an algorithm that uses claims data that identify the clinic where the member has received the most primary care. Alternatively, the member’s zip code is used to link to a clinic closest to where the enrollee lives. NorthPoint Health and Wellness Center (the Federally Qualified Health Center) represents 1 clinic site; Hennepin County Medical Center has 7 participating clinics.
Role of Community Health Workers
Community health workers located in participating clinics often serve as the primary point of contact for members and coordinate needed health and social services. The care coordination team (generally starting with the community health worker) contacts the member, conducts the first patient visit and the initial care need assessment, and develops a coordinated care plan when appropriate. Hennepin Health coordinates with local service providers and is able to address many of the nonmedical determinants of health, including
Housing and social service navigation: Social work staff from the county are available to coordinate social services and supportive housing options.
Job placement supports: A local community organization provides career counseling and job placement services.
Emergency department triage: Contracted staff from a community organization engage frequent emergency department users and connect them to community and clinic resources.
Intensive case management team: County staff provide additional case management for members with complex behavioral health needs.
Promise of Technology and Data Sharing
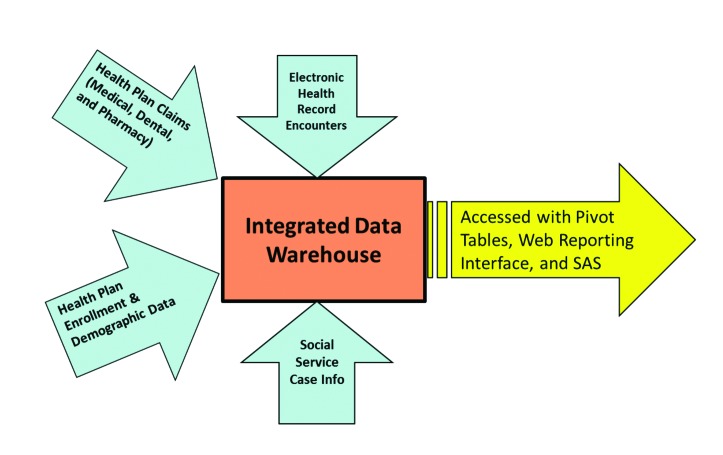
To better coordinate care, Hennepin Health uses an integrated Electronic Medicare Record and data warehouse that combines the Electronic Medicare Record with enrollment information, provider claims, and social service case data (Figure 1).4 The system produces a patient-level daily computer-accessible dashboard reflecting service use at the clinic level. Hennepin Health monitors cost, service use, patient satisfaction, and health outcomes with a monthly quality scorecard.
FIGURE 1—
Hennepin Health data warehouse model: Minneapolis, MN.
The data warehouse contains the data used to link members to clinics and to develop member risk tier profiles. Information from the initial patient assessment is entered into an electronic health record, and assignment to a risk tier is completed. Risk tier assignment is primarily based on past medical care, substance abuse, and mental health service use and ranges from low to high care coordination needs. Members with the highest care coordination needs have had 3 or more annual inpatient admissions in a year. (Hennepin Health is moving to a 4-tier system based on cutpoints in patients’ prospective hierarchical condition category risk score. (For a more detailed description of the utilization-based tiers, see http://www.innovations.ahrq.gov/content.aspx?id=3835&tab=1.)
Each of the 8 participating clinics is accountable for all of its Hennepin Health members whether the member is engaged in care management or used services. The initial patient assessment data including tier assignment allows care coordination teams to focus on the highest-risk patients, but accountability for health is monitored across all enrollees.
PRELIMINARY RESULTS AND PERFORMANCE OUTCOMES
Hennepin Health started in January 2012 and by June 2014 had enrolled approximately 8700 and by December 2014 had enrolled close to 10 000 members. Enrollees are likely to be non-White middle-aged men with significant mental health and substance abuse needs and unstable housing.
Early results are promising. As shown in Table 1, comparing the program’s first year of operation (2012) with its second year (2013), the rate of outpatient visits increased by 3.3%, whereas the rate of emergency department and inpatient admissions decreased by 9.1% and 3.0%, respectively. These desirable utilization changes were accompanied by increasing rates of quality for patients with diabetes, asthma, and vascular conditions, and 87% of enrollees indicated satisfaction with their care experience. (Quality scores are defined by and reported to Minnesota Community Measurement: http://www.mncm.org.)
TABLE 1—
Hennepin Health Utilization Outcomes Based on Patient Claims: Minneapolis, MN
| 2012 | 2013 | % Change | |
| Outpatient clinic visits per 1000 member months | 299 | 309 | +3.3 |
| Emergency department visits per 1000 member months | 120 | 109 | −9.1 |
| Inpatient admissions per 1000 member months | 16.4 | 15.9 | −3.0 |
SUMMARY
The goal of Hennepin Health is to treat each person holistically through the coordination of medical and social services to improve health outcomes and reduce costs.5 In the first 2 years of operation, Hennepin Health made significant reinvestments with savings achieved through efficient and targeted service delivery. New projects under way to further improve care include an increasing walk-in appointment capacity in an expanded coordinated care center, additional dental and primary care capacity at North Point Community Clinic, and expanded vocational support services. A new “sobering center” is also planned to assist with the care of patients undergoing detoxification presenting at the emergency department. New efforts are being made to provide for better documentation of socioeconomic indicators to measure and monitor persistent health disparities.6
This new model of care is not without its challenges. Program staff report difficulties in enrolling and retaining eligible patients because of systemic problems with Medicaid renewals, working with the state policymakers to better facilitate data sharing, and continued pressures to find stable funding for the range of services needed to serve a vulnerable patient population. Another concern is the ability to bring the Hennepin Health model to scale without a state or national ACO strategy for low-income populations.
Early results show promise of integrated medical and social service care for a historically underserved population similar to the Medicaid expansion population under the Affordable Care Act.7 In adopting an ACO model that focuses on prevention, coordination, and team-based care, the county hopes to improve individuals’ quality of life while reducing costs through reductions in emergency department use. Key to this work is care coordination, which is proactive in linking patients to primary care providers and to needed social services with a holistic focus on the unique needs of each patient.
Acknowledgments
L. A. Blewett’s contribution was funded by a grant from the Robert Wood Johnson Foundation to the State Health Access Data Assistance Center, University of Minnesota School of Public Health.
Human Participant Protection
No institutional review board approval was required because no human subjects were involved.
References
- 1.Hennepin County Medical Center. About Hennepin County Medical Center. Available at: http://www.hcmc.org/about/index.htm. Accessed July 23, 2104.
- 2.Minnesota Department of Health. Health Maintenance Organizations - Health Plan Information. HMO Profile—Metropolitan Health Plan (MHP) Available at: http://www.health.state.mn.us/hmo/mhp.htm. Accessed February 17, 2014.
- 3.NorthPoint Health and Wellness Center. About NorthPoint. Available at: http://northpointhealth.org/AboutNorthPoint/tabid/72/Default.aspx. Accessed February 17, 2014.
- 4.Kocot SL, Dang-Vu C, White R, McClellan M. Early experiences with accountable care in Medicaid: special challenges, big opportunities. Popul Health Manag. 2013;16(suppl 1):S4–S11. doi: 10.1089/pop.2013.0058. [DOI] [PubMed] [Google Scholar]
- 5. DeCubellis J. Hennepin Health. People. Care. Respect. Presentation at: 8th Annual National Policy Conference of the National Committee on Quality Assurance (NCQA): Forging Ahead on Health Reform; November 8, 2013; Washington, DC.
- 6.Sandberg SF, Erikson C, Owen R et al. Hennepin Health: a safety-net accountable care organization for the expanded Medicaid population. Health Aff (Millwood). 2014;33(11):1975–1984. doi: 10.1377/hlthaff.2014.0648. [DOI] [PubMed] [Google Scholar]
- 7.Lowen T. On the path to ACOs. Minn Med. 2012;95(11):20–25. [PubMed] [Google Scholar]