Abstract
Although preventing youth overweight and obesity is a public health priority, quality physical education (PE) is marginalized in practice. In May 2014, we estimated energy expenditure (EE; derived from PE frequency, duration, and intensity; mean student mass; and class size) from national recommendations and data from the 19 US states with PE duration guidelines, under 3 scenarios: potential (quality PE, defined as 50% moderate-to-vigorous physical activity [MVPA]), reality (MVPA = 35%), and classroom instruction only. Students in schools following nationally recommended PE standards from grades 1 through 10 could expend from 35 000 to 90 000 more kilocalories than students who received classroom instruction instead. PE's potential for increasing student EE will only be realized with stronger school policies and increased accountability.
The prevalence of overweight and obesity among school-aged youths in the United States remains high.1 Of particular concern is that obesity in childhood tracks into adulthood and is associated with a host of chronic morbidities.2 Although most of these diseases typically are not manifest until adulthood (e.g., stroke, cancer), the prevalence of type 2 diabetes and metabolic syndrome during childhood is increasing.3 Prevention of overweight and obesity among youths requires that energy expenditure (EE) exceed energy intake. Engaging in physical activity (PA) is a widely accepted approach to preventing and treating childhood obesity, and 2008 United States Physical Activity Guidelines, published by the US Department of Health and Human Services (USDHHS), recommends that youths engage in at least 60 minutes of mostly moderate-to-vigorous PA (MVPA) daily.2
Schools have long been identified as important venues for the provision of PA, especially during physical education (PE) classes.4,5 PE, a mandated curriculum area in 43 states for elementary grades, 41 for middle schools, and 44 for high schools,6 includes substantial amounts of PA during class time and is considered a public health resource for combating and preventing overweight and obesity.4–10 Although numerous health organizations and publications, including Healthy People 2020,11 recommend daily PE, only 19 of 50 states reported having policies identifying the frequency of delivery and specific number of minutes for PE.6 Of these states, only 5 reported having these policies at all 3 levels of primary and secondary school. A 2012 Institute of Medicine report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation, identified requiring school PE as a key strategy for obesity prevention in the United States.7 Analyses of data from the Early Childhood Longitudinal Study showed that PE reduced body mass index among first-grade girls who were overweight or at risk for overweight in kindergarten8 and reduced the probability of obesity among fifth-grade boys.9
Recently, the Institute of Medicine recommended an average daily dose of 30 minutes (elementary school) and 45 minutes (middle and high school) of activity per PE lesson that is composed of at least 50% MVPA.10 Although some PE lessons surpass the 50% MVPA criterion, researchers have demonstrated that most fall short of this mark. Fairclough and Stratton reviewed 44 studies of elementary school PE and found that children averaged 37.4% (±15.7%) of lesson time in MVPA (mean = 12.6 min MVPA/lesson; 21.0% of USDHHS total daily guidelines).12 Fairclough and Stratton also reviewed 40 studies of middle and high schools and found that students averaged 27.7% to 46.8% of PE time in MVPA, depending in part on the method of assessment.13 These authors did not report mean lesson length, but at the recommended 45 minutes per lesson at the secondary level,10 students on average could have accumulated between 12.5 and 21.1 MVPA minutes (20.8% and 35.1% of USDHHS total daily guidelines, respectively).
Although PE has many objectives (e.g., physical fitness; motor skills; cognitive, social, and emotional development), not all of which require engaging in PA during lesson time, many medical and professional communities consider sufficient MVPA to be a useful proxy for PE quality.14,15 This approach has yielded positive changes in professional development policy, as reported in the School Health Policies and Practices Study 2012.16 Between 2000 and 2012, the percentage of states that funded or provided professional development for teachers to learn methods to improve MVPA during PE increased from 28.0% to 66.7%. Despite this positive trend, only Idaho specifies the percentage of a lesson to be spent in MVPA (i.e., 33% in grades K–5; 50% in grades 6–12), and only Texas specifies required minutes of a lesson in MVPA (30 min/d for grades K–8).17 Carlson et al. noted that no policy addressed funding or enforcement; that policy was not uniform across states, within school levels, and within states across school levels; and that only Idaho specified a means for objectively evaluating whether MVPA goals were met.17
Lesson frequency and length, percentage of lesson time in MVPA, and steps per minute have all been used to define PE policy for quantity and quality. These metrics, however, do not readily reveal the potential public health impact that PE has on controlling childhood overweight and obesity.9
In public health forums, EE is frequently expressed in METs (metabolic equivalents of task) and MET hours, and in the PE context, 4.5 METs have been equated with MVPA.18 Bassett et al. computed a weighted mean EE of 1.70 MET hours gained per day for studies where PE was a mandatory policy.19 This mean value equates to a gain of 23 minutes of MVPA per day (38.3% of USDHHS guidelines) versus no PE. Although this latter metric may be more comprehensible to practitioners than a MET-based one, it still provides only derivative information about EE. We used the Bassett et al. data,19 along with the mean weights of children in elementary, middle, and high school, and calculated that children in middle school (98 kcal/day) and high school (121 kcal/day) PE could surpass the additional caloric expenditure of 64 kilocalories per day deemed necessary to reach overall youth obesity prevalence targets by 2020.20 These predicted EE estimates provide a useful starting point for discussion, but they are based on a limited number of large-scale interventions that do not reflect the potential or real impact of existing PE policy on EE.
We aimed to quantify the potential caloric impact of quality PE (i.e., at 50% MVPA) on the estimated EE of individual students and classes under conditions (frequency, duration, class size) recommended by professionals and by those states that have education policies mandating number of minutes for PE. We also compared estimated EE under these conditions to calculations derived from (1) data from studies where the intensity of PA was observed during PE lessons (i.e., the reality) and (2) estimations of student EE if they spent equivalent periods in classroom activities instead of PE.
METHODS
Our May 2014 calculation of caloric im-pact considered PE frequency and duration, PA intensity during lessons, class size, and children's body mass.
Sample
We based our EE estimates on data for elementary schools (grades 1–6), middle schools (grades 7 and 8), and high schools (grades 9 and 10), and we performed calculations for hypothetical boys and girls aged 6 to 15 years. We excluded kindergarten because few states had a PE duration policy, and we excluded grades 11 and 12 because only Illinois and New Jersey identified high school graduation requirements beyond 2.0 units of PE.6
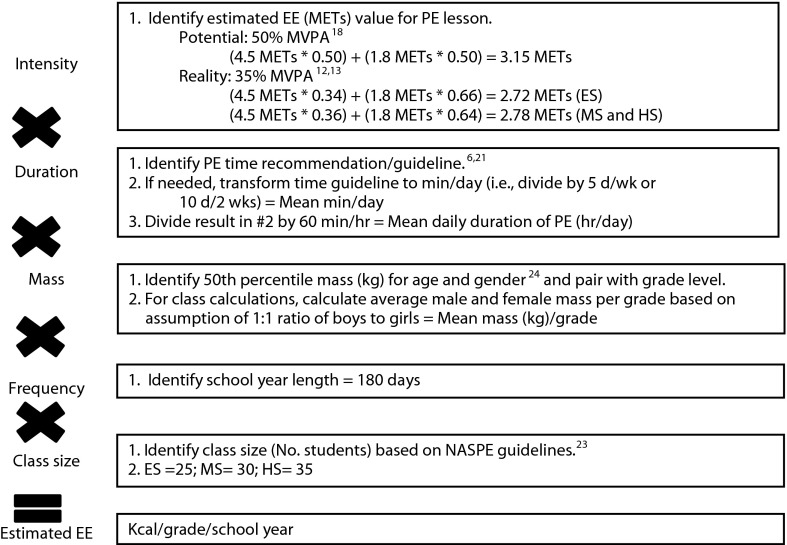
We used National Association for Sport and Physical Education (NASPE) guidelines for PE lesson time6 and review articles of MVPA levels in PE12,13 to calculate estimated EE. We also used data from the 19 states that reported specific quantitative values for policy pertaining to PE minutes in the Shape of the Nation Report (Table 1).6 We used these states to calculate an average score for the samples available at the different school levels: elementary school (16 states), middle school (14 states), and high school (9 states). (Figure 1 shows step-by-step calculation procedures.)
TABLE 1—
Estimated Yearly Energy Expenditure in Physical Education Classes by School Level: United States, May 2014
| Elementary School |
Middle School |
High School |
||||
| PE, Minutes/Day or Mean (SE) | EE, kcal/Class | PE, Minutes/Day or Mean (SE) | EE, kcal/Class | PE, Minutes/Day or Mean (SE) | EE, kcal/Class | |
| NASPE | 30.0 | 1 466 758 | 45.0 | 1 402 049 | 45.0 | 1 926 701 |
| Alabama | 30.0 | 1 466 758 | 50.0 | 1 557 883 | . . . | . . . |
| Arkansas | 12.0 | 586 703 | 12.0 | 373 880 | . . . | . . . |
| California | 20.0 | 977 839 | 40.0 | 1 246 266 | 40.0 | 1 712 624 |
| Florida | 30.0 | 1 466 758 | . . . | . . . | . . . | . . . |
| Hawaii | 6.0 | 293 352 | . . . | . . . | 40.0 | 1 712 624 |
| Iowa | . . . | . . . | . . . | . . . | 9.0 | 338 156 |
| Louisiana | 30.0a | 1 466 758 | 30.0a | 934 700 | . . . | . . . |
| Mississippi | 10.0 | 488 919 | 10.0 | 311 567 | . . . | . . . |
| Missouri | 10.0 | 488 919 | 9.0 | 280 410 | . . . | . . . |
| Montana | . . . | . . . | 45.0b | 1 402 049 | 45.0b | 1 926 701 |
| New Jersey | 30.0 | 1 466 758 | 30.0 | 934 700 | 30.0 | 1 284 468 |
| New York | 24.0 | 1 173 407 | 19.0 | 591 976 | 18.0 | 676 312 |
| North Dakota | 23.8 | 1 163 628 | 9.0 | 280 410 | . . . | . . . |
| Oklahoma | 12.0 | 586 703 | . . . | . . . | . . . | . . . |
| Rhode Island | 20.0 | 977 839 | 20.0 | 623 133 | 20.0 | 856 312 |
| South Carolina | 12.0 | 586 703 | . . . | . . . | . . . | . . . |
| Utah | . . . | . . . | 45.0b | 1 402 049 | 45.0b | 1 926 701 |
| Washington | 20.0 | 977 839 | 20.0 | 623 133 | . . . | . . . |
| West Virginia | 18.0 | 880 055 | 45.0 | 1 402 049 | 45.0b | 1 926 701 |
| State averagec | 19.2 (2.0) | 940 559 (100 454) | 27.4 (4.1) | 854 586 (126 696) | 32.4 (4.6) | 1 373 400 (203 495) |
Note. EE = energy expenditure; NASPE = National Association for Sport and Physical Education; PE = physical education. Ellipses indicate that a state policy for PE duration at that school level was not reported or did not exist and estimated EE could not be calculated.
Indicates a policy for which ≥ 150 min/wk were mandated.
Indicates a policy for which ≥ 225 min/wk were mandated.
Data from all states (n = 19) with a policy mandating or recommending specific PE minutes. Total mean and SE were calculated because data were normally distributed.
FIGURE 1—
Procedures used to calculate annual class energy expenditure (EE) in physical education lessons in 19 US states: May 2014.
Note. ES = elementary school; HS = high school; MET = metabolic equivalents task; MS = middle school; MVPA = moderate-to-vigorous physical activity; NASPE = National Association for Sport and Physical Education; PE = physical education.
Characteristics of Physical Education Classes
Duration refers to the number of minutes required for PE lessons, and frequency refers to the specific number of lessons to be offered. These numbers were variously presented, but primarily referred to requirements per day, week, or 2-week period.6 To reduce confusion among the diverse state policies for duration and frequency, we calculated a common metric across states: minutes per day. For example, in California, 400 minutes (duration) of PE were required every 10 days (frequency) at the middle and high school levels. Thus, we used 40 minutes per day to calculate EE at these 2 levels. Several states identified a minimum number of minutes; in these instances, we used the maximum numerical value identified. For example, Montana requires 225 or more minutes per week at the secondary level, so we used 225 minutes, with minutes per day equated to 45.0. For comparison, we used the NASPE frequency and duration guidelines21: 150 minutes per week (elementary school) and 225 minutes per week (middle and high school).
To derive an estimated annual dose of PE, we multiplied minutes per day by lesson frequency (length of the school year in days). We extracted the number of school days by state from the 2007 to 2008 Schools and Staffing Survey data repository.22 We used 180 days because only 4 of the 19 states listed fewer than that; for these states, we overestimated EE values by 2 (Arkansas), 3 (Louisiana), 6 (Missouri), or 5 (North Dakota) days (range = 0.1%–0.3%).
We used a value of 3.15 METs to represent the average PA intensity during PE (50% of lesson time in MVPA at 4.5 METs and 50% in sedentary-to-light activity at 1.8 METs).18 For comparison purposes, we calculated EE for an equivalent amount of time spent in classrooms (no PE) at 1.4 METs, which reflects EE associated with studying, taking notes, class discussion, and writing (i.e., all sitting activities).23 Only Arkansas and Mississippi mandated specific teacher-to-student class ratios,6 so we used NASPE class size recommendations (≤ 25 elementary, ≤ 30 middle school, and ≤ 35 high school students/class).24
We extracted nationally representative values of mean body mass of students, independent of height, from the most recent USDHHS anthropometric reference data.25 Estimated EE calculations used year-by-year 50th percentile mass values for boys and girls aged 6 years (first grade) and 15 years (10th grade).25 Class-level calculations assumed a 1-to-1 ratio of boys to girls, and we used a mean mass–by–grade level value.
Energy Expenditure Formulas and Data Calculation
We calculated the following estimated EE data: (1) kilocalories for boys and girls per grade (grades 1–10) according to both NASPE and average state policy guidelines (from the states with guidelines), (2) kilocalories per class per school level according to NASPE and average state policy guidelines, and (3) 10-year cumulative kilocalories for boys and girls across grades 1 to 10 according to NASPE and average state policy guidelines, Fairclough and Stratton estimates of MVPA in PE derived from average state mean lesson duration,12,13 and equivalent time spent in classrooms rather than in PE.
We calculated the overall caloric impact of PE during these scenarios according to the following formulas, with adjustments for mass derived from children's gender and age (Figure 1):
annual individual estimated EE (kcal/student/y) = intensity (MET) × mass (kg) × duration (lesson min/d) × frequency (days of school instruction/y)
annual class estimated EE (kcal/class/y) = intensity (MET) × mass (mean kgclass) × duration (lesson min/d) × frequency (days of school instruction/y) × class size (mean number of students/class)
We summed the products of formula 2 across grades to determine the estimated cumulative EE per class for elementary school through high school levels (Table 1).
RESULTS
Table 1 shows the cumulative estimated EE for an entire class of students at each school level according to NASPE recommendations as well as by state and the average of guidelines for the states with such guidelines. We observed large variability across the states and at the 3 school levels for both PE minutes per day and estimates of EE. For example, at the elementary school level, cumulative estimated EE for Alabama, Florida, Louisiana, and New Jersey was 1 466 758 kilocalories across grades 1 to 6, which was 5 times higher than Hawaii. At the middle school level, the range of more than 1.2 million kilocalories between Alabama (1 557 883 kcal) and Missouri and North Dakota (280 410 kcal) reflected a difference of more than 5.5 times between duration guidelines. At the high school level, the range of nearly 1.6 million kilocalories between the 3 highest states (Montana, Utah, West Virginia) and Iowa reflected a difference of 5.0 times between the PE duration guidelines. Overall, the mean state guidelines for PE minutes per day were substantially less than the NASPE recommendations for elementary (69.6%; by 10.8 min), middle (60.9%; by 17.6 min), and high (72.2%; by 12.5 min) schools (Table 1). These were reflected in the estimated EEs for the 3 levels.
Table 2 presents the estimated EE (kcal/student/y) for students during PE (grades 1–10) according to national professional recommendations (NASPE) and the average state guidelines. For both boys and girls, the annual EE increased linearly from grade 1 to 6, reflecting similar recommendations and guidelines at the elementary school level and annual increases in children's body mass. We found substantial differences in the values estimated for professional recommendations and state policies, with children in elementary schools that followed NASPE recommendations expending 1.56 times the estimated energy of those complying only with average state guidelines. In grades 2 and 3 and 5 to 7, girls expended relatively more energy than boys—a reflection of greater mass for age among girls than boys, who later catch up and then permanently exceed girls by eighth grade.
TABLE 2—
Estimated Yearly Energy Expenditure During Physical Education Classes According to National Professional Recommendations and the 19 US States With Duration Guidelines: May 2014
| Grade |
||||||||||
| 1, kcal/Student | 2, kcal/Student | 3, kcal/Student | 4, kcal/Student | 5, kcal/Student | 6, kcal/Student | 7, kcal/Student | 8, kcal/Student | 9, kcal/Student | 10, kcal/Student | |
| Boys | ||||||||||
| NASPE | 6 889 | 7 569 | 8 874 | 10 376 | 11 340 | 13 211 | 21 900 | 25 175 | 27 173 | 29 810 |
| State average | 4 418 | 4 854 | 5 690 | 6 654 | 7 272 | 8 472 | 13 314 | 15 305 | 19 592 | 21 493 |
| Girls | ||||||||||
| NASPE | 6 691 | 7 598 | 9 044 | 10 064 | 11 652 | 13 466 | 22 241 | 24 154 | 26 195 | 26 918 |
| State average | 4 290 | 4 872 | 5 799 | 6 454 | 7 472 | 8 635 | 13 521 | 14 684 | 18 887 | 19 408 |
Note. NASPE = National Association for Sport and Physical Education.
We observed a large increase over elementary levels at the onset of middle school in annual estimated EE (Table 2). Specifically, from grade 6 to 7, boys and girls increased by more than 8600 kilocalories (NASPE) and more than 4800 kilocalories (state average). This jump reflected both accelerated gains in body mass associated with pubescence and PE policy changes that increased PE time in middle schools. Children in middle school PE programs that followed NASPE recommendations expended 1.56 times the estimated energy of those following only the average state guidelines.
We did not observe a jump in annual estimated EE between grades 8 and 9 (i.e., the transition between middle school and high school), reflecting the proportional gains in mass between these grades as well as no substantial change in PE policy between the 2 school levels (Table 2). Children in high school PE programs that followed NASPE recommendations expended 1.39 times (proportionally the lowest of the 3 school levels) the energy of average state guidelines. This decreased difference suggested that average state guidelines at the high school level were more closely aligned with NASPE recommendations than those at the middle and elementary school levels.
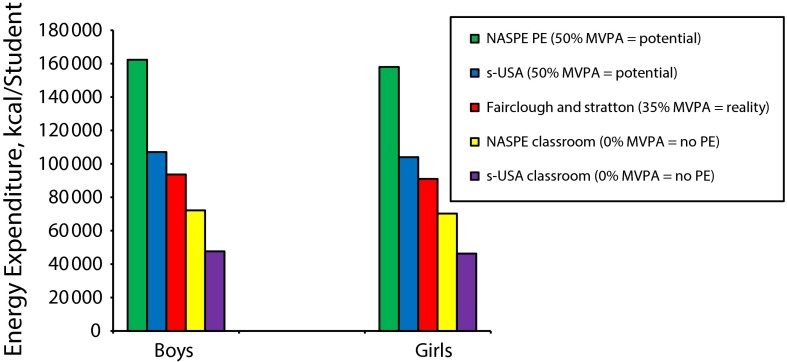
Figure 2 illustrates the cumulative estimated EE over 10 years for boys and girls under 5 scenarios. The first column for each gender shows estimated EE according to NASPE professional recommendations for PE duration and intensity (50% MVPA). The second column shows estimated EE derived from the average recommended duration of PE at 50% MVPA for the 19 states that had PE length standards. The third column shows estimated EE for PE in these 19 states at 35% MVPA, the typical intensity level found in PE studies,12,13 and under the recommended 50% MVPA level. Because students expend energy at school when they are not in PE, columns 4 and 5 show the estimated EE for equivalent amount of time spent in classroom activities according to NASPE and average state recommendations, respectively.
FIGURE 2—
Cumulative (grades 1–10) estimated EE during PE lessons and equivalent classroom time according to NASPE recommendations and average state guidelines: United States, May 2014.
Note. EE = energy expenditure; MVPA = moderate-to-vigorous physical activity; NASPE = National Association for Sport and Physical Education; PE = physical education; s-USA = state policy guidelines.
The cumulative difference between a student in a school that followed NASPE recommendations and one in a school that adhered to the average state guidelines was 55 256 kilocalories for boys and 54 001 kilocalories for girls. The cumulative difference between a student in a school that followed NASPE recommendations and one attending a school with the more common reality of approximately 35% MVPA in PE12,13 was 68 660 kilocalories for boys and 67 047 kilocalories for girls.
Among students who spent an equivalent amount of time in the classroom, boys and girls in schools following NASPE recommendations would expend an additional 90 177 and 87 791 kilocalories, respectively, over students who spent a period equivalent to PE in the classroom. Finally, in our reality scenario of PE (35% MVPA), boys and girls would expend an additional 46 007 kilocalories and 44 679 kilocalories, respectively, over the same amount of time spent in a classroom.
DISCUSSION
Pate et al.26 reviewed the PE, PA, and health literature and found only limited studies that addressed either short- or long-term public health effects of PE. Following their recommendation that the health implications of PE be given high research priority, we focused specifically on EE, which has implications for child overweight and obesity. We estimated student EE (adjusting for mean body mass by children's age and gender) during PE under 2 policy conditions: (1) national professional recommendations and (2) the recommendations of the 19 states that had policies for schools to provide a specific duration for PE. In both instances we assumed that students engaged in MVPA for 50% of lesson time, the proportion recommended by both professional organizations and health entities, and we assigned a value of 3.15 METs to represent the average PA intensity during lessons (based on 4.5 METs for MVPA and 1.8 METS for sedentary-to-light activity). In our calculations, we also considered the amount of energy that students would likely expend if they spent an equivalent amount of time in classrooms (i.e., at 1.4 METs) instead of in PE.
The Potential
Under both NASPE and average state policy conditions the average child would expend substantial amounts of energy during PE annually, as well as over a 10-year period. Because of gains in children's body mass and changes in PE policies as children move into secondary schools, estimated EE increased over time, but not linearly. Only 19 states had policies for the number of PE minutes that students should receive, and their 10-year estimated EE averaged only 66% of the NASPE recommendations. Had students not participated in PE, but spent an equivalent amount of school time in the classroom, their EE for that time would be approximately 44% of that likely accrued during PE lessons.
Although the static model of energy balance is imperfect and controversial,27,28 the frequently used formula of 3500 kilocalories equaling 1 pound of body fat can usefully illustrate the potential impact of PE on body weight. For example, EE differences between engaging in classroom activities and engaging in PE at the NASPE- and average state-recommended levels roughly equated to 2.7 and 1.7 pounds per year, respectively, for boys and 2.5 and 1.8 pounds per year, respectively, for girls.
The Reality
PE is the “pill not taken,”15 and its actual implementation in schools—frequency, duration, scope, PA intensity levels—falls far short of both the NASPE recommendations and state policies for PE.6,12,13,16,26,29–32 Three large studies—1 at each school level—specifically demonstrate the EE ramifications of inadequate provision of PE. We analyzed data on PA level during PE for 814 third-grade students in 9 states33 and calculated annual EE values of 6010 kilocalories per boy, 5640 kilocalories per girl, and 133 725 kilocalories per class. From observed PA levels during PE of 1720 middle school students in Southern California,34 we calculated annual EE ranges of 20 911 to 26 285 kilocalories for boys, 21 454 to 24 288 kilocalories for girls, and 811 746 to 882 502 kilocalories for classes. We also analyzed data on observed PA levels among 656 ninth- and 10th-grade Pennsylvania students during single-gender and coeducational PE lessons35 and calculated annual EE values of 21 341 kilocalories per boy and 15 340 kilocalories per girl in single-gender classes and 519 701 kilocalories per coeducational class. Collectively, these estimates fall far short of the EE potential of PE derived from national recommendations, state policies, or both.
Across the country, PE varies widely in frequency, duration, goals, curriculum, credentials for teachers, and facilities. This lack of standardization starts with the absence of any federal law that requires PE and diverse state requirements for minutes of PE that range from none at all in 31 states and the District of Columbia to 50 minutes per day in Alabama. All states have some established guidelines for PE (including identifying courses and activities that may be used as a waiver or substitute for PE), but it is the responsibility of school districts to implement them. This responsibility is passed on to individual schools, and with current emphasis on site-based management, district and school policies for PE do not always align.36
Even when states have specific guidelines for PE duration and frequency, often they are not followed.30,32,37 For example, of 91 236 fifth graders followed in California, the vast majority (82%) attended schools in districts that failed to provide the mandated minimum level of PE.30 Of the nearly 1000 schools nationwide that reported in the 2006 School Health Policies and Programs Study, approximately 69% of elementary schools, 84% of middle schools, and 95% of high schools required at least some PE; however, only 3.8% of elementary schools, 7.9% of middle schools, and 2.1% of high schools reported that their students had PE daily or an equivalent number of minutes per week.29
Most of these data were derived from reports by state, district, and school officials who likely were not involved in the actual conduct of lessons, and a closer look at actual student PA engagement during lessons is warranted. PA during lesson time has been measured with heart rate monitors, pedometers, accelerometers, and direct observation. Reviews of studies indicate that students rarely meet the recommended 50% MVPA level during lessons.12,13,26 Teachers determine how PE content is delivered in different contexts, and MVPA percentage is greater in classes that involve fitness and playing games than in management and knowledge contexts. MVPA percentage is generally higher at the secondary than the elementary level, because relatively more time is spent on physical fitness and games and less on management, knowledge, and motor skill development. Classes held outdoors usually provide more PA than those conducted indoors, and boys are typically more active than girls, especially during secondary school lessons.
Direct observations by trained assessors in schools indicate that many scheduled lessons are cancelled. For example, T. M. evaluated PE in nearly 80 schools in 1 large geographic area over 13 years and found that although each school had a PE teacher and a gymnasium, an average of 19% of scheduled lessons did not take place. Primary reasons for failure to provide PE in a sample of 225 cancelled lessons were unavailability of the regular PE teacher (24%), special school events (20%), academic priorities (20%), and holiday celebrations (19%). These cancelled lessons were in addition to those that did not take place because of school closures for events such as teacher development workshops and inclement weather.
Not only are lessons frequently cancelled, but observations show that actual PE lesson length (i.e., the amount of time that students spend in the instructional station) is substantially less than scheduled length, especially in secondary schools, where actual length has been found to be only 65% to 78% of scheduled length.35,38 Class size is also important, because large classes increase management time and reduce student PA engagement. No definitive national data on PE class sizes are available, but it is fair to assume that the values presented in our study reflect underestimates of true PE class sizes,39 which compromise PE quality.34,40
In addition to promoting PA, physical skills, and fitness, PE traditionally has had many other objectives (e.g., cognitive, social, and emotional development),21 not all of which are related to either PA or health outcomes. No individual state provides or recommends a single, specific PE curriculum; thus, teachers have wide leeway in what and how to teach. The result is tremendous variability in the amount of student PA, and this is related to numerous factors such as lesson goals, content, and placement within an instructional unit; class size and gender composition; grade level; individual differences among students; lesson location; available equipment and facilities (e.g., size of instructional space); and teacher preparation, skills, and behavior.15,26,41
Recently, health-optimizing PE, which prioritizes student PA during lessons, has been promoted as a vehicle for actualizing PE’s potential to improve public health.42 The provision of MVPA during lesson time has also been promoted as a major defining factor in the quality of PE.15,42 The Institute of Medicine recently reported that enhanced PE—lessons delivered by well-trained specialists with instructional practices that provide substantial MVPA—has been shown to increase PA during school hours among youths.10 Evidence-based PE programs that incorporate health-optimizing PE principles have been shown to increase MVPA in lessons by up to 18%, but they face barriers to adoption, including lack of interest by school administrators and the costs of staff development.43
Limitations
In the absence of solid data, we made assumptions that limit the accuracy and generalizability of our analyses. For example, no national surveillance study of PE has directly observed the conduct of PE, and it is well known that the implementation of state PE guidelines is less than perfect. Our state sample comprised only the 19 states that specified PE duration in their guidelines, and only 1 state specified an intensity level for PA during PE (Idaho: 33% MVPA for grades 1–5 and 50% MVPA for grades 6–12).
The association between EE and body weight is complex and definitely not linear,27,28 precluding precise predictions of body weight changes as the result of PE. Also, we did not consider any potential ancillary health benefits resulting from PE, such as increased physical fitness and accrual of knowledge and behavioral strategies designed to increase student PA outside of lesson time and into adulthood.
Conclusions
One benefit of PA during PE is that it requires student EE, and this in turn helps to control overweight and obesity. We examined the potential and reality of the immediate effects of school PE on controlling overweight and obesity solely related to estimated PA during lesson time. We used 2 best-case scenarios, one based on the recommendations of professional organizations and health proponents8,20 and the other on the policies of the 19 US states that have guidelines for PE duration.
It is clear, even from conservative EE estimates, that PE has great potential for helping to control child and adolescent overweight, especially when conducted at a dosage recommended by either national (i.e., NASPE) standards or the 19 states that specify PE time requirements. Many barriers interfere with the realization of this potential, however; the most prominent is the lack of strong PE policies at state and district levels and the lack of accountability imposed on schools. The extent of these barriers, however, is not well known, and very few PE programs are subjected to an annual review.43
Substantial time and resources are spent on PE, and yet not enough is known about how it is being implemented at the micro level across the country. In addition to the need for a national study, it is important that states and districts implement ongoing surveillance systems to ensure that PE is being conducted as recommended. Such strategies could help ensure that children receive sufficient amounts of both PE and PA, which will improve their health, including helping to control overweight and obesity.
Human Participant Protection
The study was exempted by the San Diego State University institutional review board.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of child and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Dept of Health and Human Services. 2008 Physical activity guidelines for Americans. 2008. Available at: http://www.health.gov/PAGuidelines/pdf/paguide.pdf. Accessed May 15, 2014.
- 3.De Ferranti SD, Osganian SK. Epidemiology of paediatric metabolic syndrome and type 2 diabetes mellitus. Diab Vasc Dis Res. 2007;4(4):285–296. doi: 10.3132/dvdr.2007.055. [DOI] [PubMed] [Google Scholar]
- 4.Sallis JF, McKenzie TL. Physical education’s role in public health. Res Q Exerc Sport. 1991;62(2):124–137. doi: 10.1080/02701367.1991.10608701. [DOI] [PubMed] [Google Scholar]
- 5.Pate RR, Leavy Small M, Ross JG et al. School physical education. J Sch Health. 1995;65(8):312–318. doi: 10.1111/j.1746-1561.1995.tb03380.x. [DOI] [PubMed] [Google Scholar]
- 6.National Association for Sport and Physical Education, American Heart Association. 2012 Shape of the Nation Report: Status of Physical Education in the USA. Reston, VA: American Alliance for Health, Physical Education, Recreation and Dance; 2012. [Google Scholar]
- 7.Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: National Academies Press; 2012. [Google Scholar]
- 8.Datar A, Sturm R. Physical education in elementary school and body mass index: evidence from the Early Childhood Longitudinal Survey. Am J Public Health. 2004;94(9):1501–1506. doi: 10.2105/ajph.94.9.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cawley J, Frisvold D, Meyerhoefer C. The impact of physical education on obesity among elementary school children. J Health Econ. 2013;32(4):743–755. doi: 10.1016/j.jhealeco.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine. Educating the student body: taking physical activity and physical education to school. 2013. Available at: http://www.iom.edu/Reports/2013/Educating-the-Student-Body-Taking-Physical-Activity-and-Physical-Education-to-School.aspx. Accessed May 16, 2014. [PubMed]
- 11.US Dept of Health and Human Services. Healthy people 2020. 2010. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf. Accessed July 29, 2014.
- 12.Fairclough SJ, Stratton G. A review of physical activity levels during elementary school physical education. J Teach Phys Educ. 2006;25(2):239–257. [Google Scholar]
- 13.Fairclough S, Stratton G. Physical activity levels in middle and high school physical education: a review. Pediatr Exerc Sci. 2005;17(3):217–236. [Google Scholar]
- 14.American Heart Association. Learning for life: physical education in public schools. 2011. Available at: https://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_428448.pdf. Accessed May 16, 2014.
- 15.McKenzie TL, Lounsbery MA. Physical education teacher effectiveness in a public health context. Res Q Exerc Sport. 2013;84(4):419–430. doi: 10.1080/02701367.2013.844025. [DOI] [PubMed] [Google Scholar]
- 16.Lee SM, Nihiser AJ, Fulton JE, Borgogna B, Zavacky F. National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Adolescent and School Health. Results From the School Health Policies and Practices Study 2012. Atlanta, GA: Centers for Disease Control and Prevention; 2013. Physical education and physical activity: results from the School Health Policies and Practices Study 2012; pp. 33–48. Available at: http://www.cdc.gov/healthyyouth/shpps/2012/pdf/shpps-results_2012.pdf. Accessed May 16, 2014. [Google Scholar]
- 17.Carlson JA, Sallis JF, Chriqui JF, Schneider L, McDermid LC, Agron P. State policies about physical activity minutes in physical education or during school. J Sch Health. 2013;83(3):150–156. doi: 10.1111/josh.12010. [DOI] [PubMed] [Google Scholar]
- 18.Wang YC, Hsiao A, Orleans CT, Gortmaker SL. The caloric calculator: average caloric impact of childhood obesity interventions. Am J Prev Med. 2013;45(2):e3–e13. doi: 10.1016/j.amepre.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 19.Bassett DR, Fitzhugh EC, Heath GW et al. Estimated energy expenditures for school-based policies and active living. Am J Prev Med. 2013;44(2):108–113. doi: 10.1016/j.amepre.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 20.Wang YC, Orleans CT, Gortmaker SL. Reaching the healthy people goals for reducing childhood obesity: closing the energy gap. Am J Prev Med. 2012;42(5):437–444. doi: 10.1016/j.amepre.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 21.National Association for Sport and Physical Education. Physical Education Is Critical to Educating the Whole Child. Reston, VA: American Alliance for Health, Physical Education, Recreation and Dance; 2011. [Google Scholar]
- 22.National Center for Education Statistics. Schools and staffing survey 2007–2008. Available at: http://nces.ed.gov/surveys/sass/question0708.asp. Accessed November 13, 2014.
- 23.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. Int J Behav Nutr Phys Act. 2008;5:45. doi: 10.1186/1479-5868-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Association for Sport and Physical Education. Teaching Large Class Sizes in Physical Education. Guidelines and Strategies. Reston, VA: American Alliance for Health, Physical Education, Recreation and Dance; 2006. [Google Scholar]
- 25.Fryar CD, Gu Q, Ogden CL. Anthropometric reference data for children and adults: United States, 2007–2010. 2012. Available at: http://www.cdc.gov/nchs/data/series/sr_11/sr11_252.pdf. Accessed May 16, 2014. [PubMed]
- 26.Pate RR, O’Neill JR, McIver KL. Physical activity and health: does physical education matter? Quest. 2011;63(1):19–35. [Google Scholar]
- 27.Shook RP, Hand GA, Blair SN. Top 10 research questions related to energy balance. Res Q Exerc Sport. 2014;85(1):49–58. doi: 10.1080/02701367.2013.872017. [DOI] [PubMed] [Google Scholar]
- 28.Hall KD, Heymsfield SB, Kemnitz JW, Klein S, Schoeller DA, Speakman JR. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012;95(4):989–994. doi: 10.3945/ajcn.112.036350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee SM, Burgeson CR, Fulton JE, Spain CG. Physical education and physical activity: results from the School Health Policies and Programs Study 2006. J Sch Health. 2007;77(8):435–463. doi: 10.1111/j.1746-1561.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- 30.Sanchez-Vaznaugh EV, O’Sullivan M, Egerter S. When school districts fail to comply with state physical education laws, the fitness of California’s children lags. A policy brief. 2013. Available at: http://activelivingresearch.org/sites/default/files/PolicyBrief_PEPolicyCali.pdf. Accessed May 15, 2014.
- 31.San Diego State University. Physical education matters. A policy brief from the California Endowment. 2008. Available at: http://www.calendow.org/uploadedfiles/publications/by_topic/disparities/obesity_and_diabetes/pe%20matters%20long%20versionfinal.pdf. Accessed May 15, 2014.
- 32.Thompson HR, Linchey J, Madsen KA. Are physical education policies working? A snapshot from San Francisco, 2011. Prev Chronic Dis. 2013;10:E142. doi: 10.5888/pcd10.130108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The National Institute of Child Health and Human Development Study of Early Child Care and Youth Development Network. Frequency and intensity of activity of third-grade children in physical education. Arch Pediatr Adolesc Med. 2003;157(2):185–190. doi: 10.1001/archpedi.157.2.185. [DOI] [PubMed] [Google Scholar]
- 34.McKenzie TL, Marshall SJ, Sallis JF, Conway TL. Student activity levels, lesson context, and teacher behavior during middle school physical education. Res Q Exerc Sport. 2000;71(3):249–259. doi: 10.1080/02701367.2000.10608905. [DOI] [PubMed] [Google Scholar]
- 35.Smith NJ, Lounsbery MA, McKenzie TL. Physical activity in high school physical education: impact of lesson context and class gender composition. J Phys Act Health. 2014;11(1):127–135. doi: 10.1123/jpah.2011-0334. [DOI] [PubMed] [Google Scholar]
- 36.Lounsbery MAF, McKenzie TL, Morrow JR, Monnat SM, Holt KA. District and school physical education policies: implications for physical education and recess time. Ann Behav Med. 2013;45(1, suppl):131–141. doi: 10.1007/s12160-012-9427-9. [DOI] [PubMed] [Google Scholar]
- 37.Diamant AL, Babey SH, Wolstein J. Adolescent Physical Education and Physical Activity in California. Los Angeles, CA: UCLA Center for Health Policy Research; 2011. [PubMed] [Google Scholar]
- 38.McKenzie TL, Catellier DJ, Conway T et al. Girls’ activity levels and lesson contexts in middle school PE: TAAG baseline. Med Sci Sports Exerc. 2006;38(7):1229–1235. doi: 10.1249/01.mss.0000227307.34149.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lafleur M, Strongin S, Cole BL et al. Physical education and student activity: evaluating implementation of a new policy in Los Angeles public schools. Ann Behav Med. 2013;45(1, suppl):122–130. doi: 10.1007/s12160-012-9431-0. [DOI] [PubMed] [Google Scholar]
- 40.UCLA Center to Eliminate Health Disparities, Samuels and Associates. Failing fitness: physical activity and physical education in schools. 2007. Available at: http://www.calendow.org/uploadedFiles/failing_fitness.pdf. Accessed July 25, 2014.
- 41.Levin S, McKenzie TL, Hussey JR, Kelder SH, Lytle LA. Variability of physical activity during physical education lessons across elementary school grades. Meas Phys Educ Exerc Sci. 2001;5(4):207–218. [Google Scholar]
- 42.Sallis JF, McKenzie TL, Beets MW, Beighle A, Erwin H, Lee S. Physical education’s role in public health: steps forward and backward over 20 years and HOPE for the future. Res Q Exerc Sport. 2012;83(2):125–135. doi: 10.1080/02701367.2012.10599842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lounsbery MAF, McKenzie TL, Trost S, Smith NJ. Facilitators and barriers to adopting evidence-based physical education in elementary schools. J Phys Act Health. 2011;8(1, suppl):S17–S25. doi: 10.1123/jpah.8.s1.s17. [DOI] [PubMed] [Google Scholar]