Abstract
Objectives. We developed and evaluated a novel National Institutes of Health–sponsored Research and Mentorship Program for African American and Hispanic medical students embedded within the international, multisite HIV Vaccine Trials Network, and explored its impact on scientific knowledge, acquired skills, and future career plans.
Methods. Scholars conducted social, behavioral, clinical, or laboratory-based research projects with HIV Vaccine Trials Network investigators over 8 to 16 weeks (track 1) or 9 to 12 months (track 2). We conducted an in-depth, mixed-methods evaluation of the first 2 cohorts (2011–2013) to identify program strengths, areas for improvement, and influence on professional development.
Results. A pre–post program assessment demonstrated increases in self-reported knowledge, professional skills, and interest in future HIV vaccine research. During in-depth interviews, scholars reported that a supportive, centrally administered program; available funding; and highly involved mentors and staff were keys to the program’s early success.
Conclusions. A multicomponent, mentored research experience that engages medical students from underrepresented communities and is organized within a clinical trials network may expand the pool of diverse public health scientists. Efforts to sustain scholar interest over time and track career trajectories are warranted.
African Americans and Hispanics are underrepresented in the research workforce, but these groups are disproportionately affected by a number of conditions and diseases, in particular the HIV/AIDS epidemic in the United States.1 African Americans account for approximately 13% of the US population2 and 44% of new HIV infections3 but only represent 7% of newly enrolled US medical students4 and 1% of US medical school full professors.5 Likewise, Hispanics represent 16% of the US population6 and 21% of new HIV infections,3 but only 9% of newly enrolled medical students,4 and 3% of medical school full professors.5 In addition, the low success rate for many minority subpopulations in securing research funding is thought to be associated with inadequate mentoring as determined by sophisticated methods of statistical concept mapping.7 A key goal of the pilot program described herein is to develop mentoring strategies to enhance HIV science and career development of medical students early in their training.
Despite high HIV/AIDS rates among African Americans and Hispanics, these groups are underrepresented in clinical trials of HIV prevention and treatment strategies.8–10 Including African Americans and Hispanics in clinical trials is important because it is possible that immune responses to an HIV vaccine may vary according to race and ethnicity and underrepresentation may limit the generalizability of trial results in these populations.11–14 In addition, increased participation may ultimately translate to greater acceptability and uptake of newly available products for the prevention and treatment of HIV/AIDS.
One way to address the lack of African American and Hispanic participation in clinical trials is to increase representation of physician scientists from these communities. In one survey, 51% of African American and 57% of Hispanic physicians considered their race/ethnicity an important factor in helping patients overcome their reluctance to participate in clinical trials, compared with only 9% of Whites and 21% of Asians.15 Underrepresented minority researchers are in a unique position to help address health disparities, enhance results dissemination strategies, and strengthen the public health impact of HIV/AIDS research. They may also have a better understanding of the participation barriers specific to underserved communities and may be more likely than their White counterparts to focus on issues that have disproportionate impacts on minority populations. In addition, these researchers are more likely to serve underrepresented minority populations in their careers15 and are important role models for future minority physicians and scientists. Minority researchers are often able to identify pertinent research topics and unique interventions for their communities of origin16 and can bring diverse perspectives, experiences, and values to research. There is evidence suggesting that diverse groups comprising members with varying perspectives outperform those that have members with more similar backgrounds and perspectives.17 Capitalizing on the advantages that a diverse group of scientists can provide is particularly important in a field like HIV vaccine research because of its various challenges and complexities.
Because racial and ethnic minorities are underrepresented in medical schools, health professions,18 and in research careers,19 scientists, educators, and policymakers have addressed potential barriers and possible solutions to overcome them to build the pipeline toward career development.20 Despite recent improvements, research indicates that underrepresented minority students are still lost at every key transition point along the academic pipeline.21 A recent study of medical students found that those from racial and ethnic minority backgrounds perceived having greater difficulty succeeding in academia, and desired more coordinated exposure to academic career paths and research training as well as enhanced infrastructure to support diversity and mentoring.22 Although strong mentorship is critical to the success of trainees in academic settings,23 formal mentoring programs for medical students are limited.24 To the best of our knowledge there are only a few published reports describing mentoring programs for minorities in HIV science: an Internet-based program on NeuroAIDS translational research for pre- and postdoctoral fellows,25 a research education training program on behavioral prevention targeting early career faculty,16,26 and a training program for early career minority scientists in HIV prevention research.27 This represents the first report of a mentoring program in HIV science for medical students from underrepresented diverse racial and ethnic groups.
The HIV Vaccine Trials Network (HVTN), a National Institutes of Health (NIH)–sponsored clinical trials network dedicated to the search for a safe and effective HIV vaccine since 1999, focused on medical students for its first diversity pipeline initiative—a group at an important formative stage of training that may benefit the most from high-quality mentored research experiences as a way to spark interest in future research careers.22 It is important for the HVTN to invest in the career development pipeline of future African American and Hispanic physician scientists with the goal of attracting them to careers in HIV vaccine research so they can inform the search for a safe and effective vaccine. We hypothesize that by leveraging existing HVTN resources and engaging with medical students early in their training and career development, we will be better able to attract and retain them into the HIV vaccine research field. In light of the fact that pressing biomedical challenges are increasingly being addressed by large, multidisciplinary scientific consortia, clinical trial networks are poised to offer student scholars a wide range of research projects under the guidance of their collaborating investigators. Network-based mentored research programs also promise research placements in diverse geographic settings, access to several ongoing research protocols and available data for analysis, basic science– as well as social and behavioral science–focused projects, and sufficient network administrative infrastructure and coordination to orient the students to HIV research and support them throughout their experiences.
We describe the NIH-supported Research and Mentorship Program (RAMP) for African American and Hispanic medical students and present evaluation data to inform future program development.
In 2005, the HVTN formed the Legacy Project with the goal of identifying and addressing barriers to increased participation of African American and Hispanics in HIV vaccine clinical trials. A Legacy Project external advisory committee postulated that a more representative scientific workforce could be beneficial, and recommended that the HVTN develop a program to attract a more diverse pool of researchers into the field at an early stage in their career development.
The aim of RAMP is to attract African American and Hispanic medical students to the field of HIV vaccine research through a multicomponent strategy (Figure 1). The development of RAMP was guided by formative in-depth interviews with 7 HIV/AIDS prevention researchers of color (Neva Pemberton et al., unpublished data presented at RAMP Advisory Board Meeting, November 3, 2010). This exploratory study identified factors that facilitated their career choices, emphasizing the need for strong mentorship and acknowledging the importance of building mentee self-efficacy, setting clear goals, and defining outcome expectations—central tenets of social cognitive career theory.28 From its inception, RAMP has aimed to integrate the scholars into the academic and social systems of the HVTN and affiliated trial sites as a way to strengthen their commitment to future HIV research careers. The program actively encourages mentors to give mentees opportunities to build skills and achieve “early wins,” to clarify expectations, and to revisit goal setting by completing an individual development plan.
FIGURE 1—
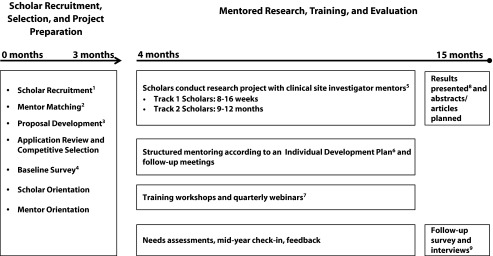
Program schema of the HIV Vaccine Trials Network (HVTN) Research and Mentorship Program (RAMP) for African American and Hispanic medical students.
Note. (1) RAMP for African American and Hispanic medical students was advertised through all accredited US medical schools. (2) Mentor matching was based on scientific field of interest, geography, and other factors (e.g., personal attributes, academic performance). (3) Mentors and applicants developed a feasible research project aligned with the HVTN research agenda and wrote proposal with budget. (4) Scholars completed a baseline survey before beginning work or participating in training activities. (5) Projects were conducted at an HVTN domestic or international research site and were laboratory, social, or behaviorally based. (6) A signed individual development plan by scholars and mentors defined mentoring expectations and meeting frequency. (7) Scholars participated in several centrally organized trainings throughout RAMP on topics such as HIV vaccine science, cultural responsiveness, biostatistics, and article writing. (8) Scholars gave oral and poster presentations at HVTN conferences. (9) Follow-up surveys and interviews were conducted shortly after final presentations.
Medical students in the United States receive support from RAMP to conduct research projects under the mentorship of HVTN-affiliated investigators on a variety of topics aligned with the HVTN’s scientific agenda. All RAMP scholars conduct their projects at a domestic or international HVTN research site and are encouraged to participate in site research activities, meetings, and trainings. Most students conduct projects in the summer between their first and second year of medical school or as a research elective during their fourth year (track 1) or as a dedicated research year either as a standalone research experience or as a component of a master’s or doctoral program (track 2). Scholars are awarded up to $20 000 for 8- to 16-week projects and up to $60 000 for 9- to 12-month projects. Funding supports research project costs, living stipend, travel, and conference attendance. Scholars also participate in several in-person workshops and webinars organized by the HVTN’s training program. Topics include cultural responsiveness in academic settings, professional development (e.g., manuscript writing, effective oral presentations), and scientific areas relevant to HIV vaccine research. All scholars are expected to present their research at an HVTN semiannual conference and are highly encouraged to submit abstracts and prepare manuscripts for submission to peer-reviewed journals.
African American and Hispanic medical students who are US citizens or permanent residents and have matriculated at an accredited US medical school are eligible to apply for RAMP. A dedicated project manager who is extensively networked with HVTN-affiliated research mentors advertises the program, fields student inquiries, and works with applicants to identify the type of research they are interested in pursuing, discuss project ideas, and match them with mentors. Applications are reviewed and selected by a 13-member review board comprising program staff, HVTN investigators, research site coordinators, NIH project officers, and RAMP alumni. Reviews are based on several criteria including the merit of their research proposal originated jointly with their network-affiliated mentors, academic standing, and motivations to pursue a future career in HIV research.
The HVTN Core Operations Center in Seattle, Washington, administers RAMP. A program leadership team with research, training, and mentoring expertise meets regularly to guide the implementation of RAMP. The RAMP project manager provides scholars and mentors information, guidance, and project support throughout the program. An HVTN evaluation project manager oversees evaluation activities.
The HVTN investigator mentors are responsible for working with student applicants to define a project and write a research proposal application. Mentors receive training in best mentoring practices such as structuring mentor encounters and reviewing individual development plans. Mentors are also responsible for overseeing all aspects of the scholars’ research projects. Although the primary focus of the mentoring is research and training, most mentors also offer career advice, and discuss with mentees work–life balance and the value of professional networking. Primary mentors receive stipends of $1500 for 8- to 16-week projects and $10 000 for 9- to 12-month projects. Mentors represent several academic disciplines including social and behavioral science, laboratory science, clinical research, and clinical practice.
Through RAMP, scholars are provided with an experience that mirrors that of applying for and conducting NIH-sponsored research (proposal development, competitive review, institutional review board submission, research implementation, etc.). Skills developed through this process will benefit scholars should they apply for NIH or other sponsor funding in the future. In addition, some projects involve the secondary analysis of data obtained through HVTN-conducted studies, providing scholars the opportunity to navigate the review and approval of research concepts by HVTN committees. Because HIV vaccine research requires multidisciplinary approaches, scholars have a variety of project options including social, behavioral, clinical, and laboratory-based projects. To date, scholars have conducted projects in basic science research (n = 3); HIV vaccine trial recruitment, participation, and retention (n = 6); and behavioral or psychosocial research (n = 4). It is notable that the majority of scholar projects focused on social and behavioral research questions. Scholar project selection may underscore the value of social and behavioral science for minority medical students interested in working in HIV/AIDS research, and the need to engage more investigators with social and behavioral science expertise as RAMP mentors.
METHODS
We conducted an evaluation of the first 2 RAMP cohorts (2011–2013) to explore the program’s impact on scholars’ knowledge, acquired skills, and future career plans and to identify program strengths and areas for improvement. We collected data by using mixed methods through surveys and interviews with scholars and mentors.
All scholars (n = 13) completed surveys at baseline and at the end of their projects when they presented their research results. Baseline surveys included 17 five-point Likert scale questions and 2 open-ended questions. Topics included self-reported knowledge, skills, and future career plans. The follow-up survey repeated all baseline survey questions and included 39 additional Likert scale questions and 14 additional questions exploring project experience, mentoring, training, and program satisfaction. We also conducted postprogram surveys of the mentors (n = 16) to assess their satisfaction with RAMP and willingness to remain in contact with the scholar to offer additional support, if needed. We performed the Wilcoxon signed-rank test by using RStudio version 0.97.551 (RStudio, Boston, MA) to evaluate changes in scholar self-reported knowledge, skills, and career plans.
All scholars from the first 2 cohorts (n = 13) as well as a majority of mentors from the first cohort (n = 9) participated in one-on-one interviews. Two authors (C. S. and R. C.) conducted all interviews, each lasting 30 to 60 minutes. Audio-recorded interviews were transcribed verbatim, and uploaded into a qualitative data analysis software tool, ATLAS.ti version 6.2.28 (ATLAS.ti GmbH, Berlin, Germany), for coding. The interviewers and 1 additional coder independently did the coding. We reviewed the first 3 interviews to establish a preliminary list of codes. During this initial review process, codes fell into 4 major categories: program strengths, factors that facilitated scholar success, program challenges, and suggested program improvements. We used these categories to develop a codebook, which we used to code all subsequent interviews. The 2 coders met to review codes and compare for consistency. They discussed any discrepancies until consensus was reached.
RESULTS
During recruitment of the first 2 RAMP cohorts, a total of 103 eligible African American and Hispanic medical students contacted the RAMP project manager expressing interest in the program. Thirty-seven applications were submitted, 14 medical students were selected as scholars, and 13 of them have completed the program. Of the 13 medical students from both cohorts who have completed RAMP, more than half (62%) were male; 7 (54%) identified as African American and 6 (46%) as Hispanic. Seven (54%) of the scholars were in their first (n = 6) or second (n = 1) year of medical school and 6 (46%) were in their third (n = 3) or fourth (n = 3) year. Ten of the 13 (77%) projects were short-term, ranging from 8 to 16 weeks (track 1), and 3 (23%) were year-long projects (track 2). A majority (77%) of the projects focused on social and behavioral research questions and 3 (23%) were laboratory focused. Nine (69%) of the projects were conducted at a domestic site and 4 (31%) at an international site.
All 13 scholars who have completed RAMP (100%) participated in baseline and follow-up surveys. The pre–post program assessment demonstrated significant increases in all self-reported knowledge domains and several of the professional skill–related questions including qualitative research, human participants, and scientific writing (Figures 2 and 3). Scholars’ self-reported knowledge about HIV vaccine career opportunities did increase significantly (P = .001) as did their belief that those career opportunities were available to them (P = .01; data not shown). Among scholars completing the program, we observed a trend toward greater intention to pursue a career in HIV vaccine research (25% “agree” or “strongly agree” at baseline vs 62% at follow-up; P = .095). Interviews and open-ended survey questions provided additional support that RAMP has influenced career plans. For example, one scholar wrote
[RAMP] revealed many more paths within the area of HIV prevention research than I could have ever uncovered on my own. I am sure that my eventual destination in HIV research will have originated with an opportunity I learned about through RAMP.
FIGURE 2—
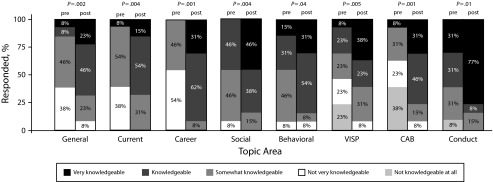
Scholar’s (n = 13) self-reported knowledge assessed pre- and postprogram from cohorts 1 and 2: HIV Vaccine Trials Network (HVTN) Research and Mentorship Program for African American and Hispanic medical students, United States, 2011–2013.
Note. CAB = community advisory board; VISP = vaccine-induced seropositivity. General indicates general knowledge about vaccines; Current indicates current status of HIV vaccine research; Career indicates career opportunities in HIV vaccine research. Social indicates the role of social science within a vaccine trials network; Behavioral indicates the rationale for collecting behavioral risk data within an HIV vaccine clinical trial. CAB indicates the role of CABs within the HVTN. Conduct indicates the responsible conduct of clinical research. P values were calculated with the Wilcoxon signed-rank test.
FIGURE 3—
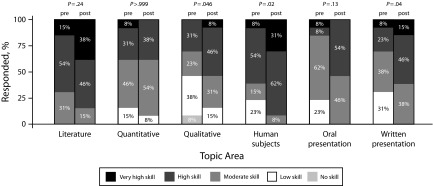
Scholar’s (n = 13) self-reported skills assessed pre- and postprogram from cohorts 1 and 2: HIV Vaccine Trials Network Research and Mentorship Program for African American and Hispanic medical students, United States, 2011–2013.
Note. Literature indicates conducting a literature search. Quantitative indicates collecting and analyzing quantitative data. Qualitative indicates collecting and analyzing qualitative data. Human Subjects indicates understanding when a research project should be submitted for human participant review. Oral presentation indicates presenting research findings orally. Written presentation indicates presenting research findings in writing. P values were calculated with the Wilcoxon signed-rank test.
Another scholar wrote, “The mentorship I have received has been outstanding and has changed my career path completely.”
At the end of the program, all 13 scholars (100%) were “satisfied” (n = 1) or “very satisfied” (n = 12) with RAMP overall. We collected postprogram surveys from 16 mentors over the 2 cohorts (9 of 11 [82%] from cohort 1, and 7 of 12 [58%] from cohort 2). All 16 mentors (100%) “agreed” (n = 2) or “strongly agreed” (n = 14) that they enjoyed their experience as a RAMP mentor and “agreed” (n = 5) or “strongly agreed” (n = 11) that they expect to maintain a relationship with their scholar in the future.
We conducted one-on-one interviews with all 13 scholars (100%) who completed RAMP from 2 cohorts after they had finished their final project presentation and with 9 out of 11 (82%) participating mentors from cohort 1. Qualitative data revealed 4 program themes that emphasized facilitators and strengths and 4 that reflected challenges and suggestions for improvement. Factors identified as program strengths that facilitated success include excellent research site capacity, access to appropriate funding to support the scholar and research costs, highly involved mentors and administrative staff, and substantial learning and networking opportunities (Table 1). Challenges and suggestions for improvement fell into the following 4 thematic areas: logistical issues, mentor accessibility, a need for more explicit communication with both mentors and scholars about expectations during the program’s outset, and a desire to increase opportunities for scholars to interact with each other during RAMP and in the future (Table 1).
TABLE 1—
Sample Quotes From Interviews With the Scholars and Mentors Demonstrating the Identified Program Facilitators, Strengths, Challenges, and Suggestions for Improvement: HIV Vaccine Trials Network Research and Mentorship Program for African American and Hispanic Medical Students, Cohorts 1 and 2; United States; 2011–2013
| Interview Themes | Definition | Scholar or Mentor Comments |
| Program facilitators and strengths | ||
| Site capacity | Site capacity includes having staff, expertise, and other resources available at the site to provide assistance and additional mentoring to the scholar. | “I definitely could not have done the project if I hadn't had buy-in at the sites and had that kind of effort done by all of the staff, not just my mentors, but everyone that worked there. . . .”–Scholar |
| “[T]he site I was in had all the infrastructure in place to really hit the ground running, which was really necessary for the short, summer projects.”–Scholar | ||
| Access to funding | The level of funding available to the scholars attracted them to the program initially, and helped them complete their projects. | “All of my legitimate financial needs for the project were met with RAMP . . . that removed a lot of needless stress, when you don't have to worry about, ‘Well, we can't do that part of the project because there just aren't funds to do that.’”–Scholar |
| “Most budgets for medical students were like $5000 and you really can't do much with that, and you certainly can't go to scientific meetings and do research with that, so I thought the budget was like a wonderful way to learn. It just allows you to do so much more with research and with coming up with a project that's big. . . .”–Scholar | ||
| Highly involved mentors and program administration | An engaged and available mentor was commonly identified by scholars and mentors as a facilitator during application, project, and mentoring activities. Comprehensive and hands-on program administration was also identified as a strength. | “Well I think the strengths are . . . the mentoring aspect, at least in my experience, wasn’t an afterthought. It was a really deliberate effort on the part of my mentor to be a good mentor.”–Scholar |
| “[The RAMP Project Manager] was incredibly helpful in every aspect, in terms of getting the application together, then after that working with the budget. . . . I think that was really great. All those details were able to be centralized and she was the point person.”–Scholar | ||
| Learning and networking opportunities | Learning and networking opportunities including trainings, workshops, conference attendance, and the ability to present their project results were seen as key strengths by both scholars and mentors. | “So, I think that from my perspective [the project] went really well because I learned a lot of new methods of doing research.”–Scholar |
| “I think it’s, again, a great opportunity to meet people from all over the world who are engaged in really important work.”–Scholar | ||
| “And now I have an even bigger professional network, and that is something that will definitely benefit me in the future.”–Scholar | ||
| Challenges and suggestions | ||
| Project logistics | Project logistics were identified by both mentors and scholars as a common challenge. Examples include the institutional review board process, time constraints, scheduling conflicts, funding allocation issues, international coordination, and project management. | “[W]hen you're going to an international site . . . there was a lot of nonacademic logistical things that kind of make your experience less efficient.”–Scholar |
| “I only had 1 month to do my project, so I had to have everything organized and ready to go by the time I got there and that was a really hard thing to get done. . . .” –Scholar | ||
| “One of the things that is just a great limiting step for [Research and Mentorship Program] scholars, or anybody who has a limited amount of time to collect data, is [institutional review board] approval.”–Scholar | ||
| Mentor accessibility | The accessibility of mentors was identified by the scholars as a challenge. | “I think logistics of accessibility was difficult sometimes. Just because [the mentors’] availability obviously fluctuated and sometimes when they were available, they weren’t both available at the same time.”–Scholar |
| “[The mentors] are both really, really busy, so it would have been good to have had to have been assigned someone earlier that was more hands-on than them.” –Scholar | ||
| More explicit communication | Scholars and mentors suggested more explicit communication and clarification of expectations from the outset of the program. | “[It would be helpful to] have sort of a road map for what needs to be done now, having that available for mentors in the [United States] . . . so that they can go through the steps that are necessary to get this accomplished.” –Mentor |
| “Maybe like 1 or 2 points of preference would be a little more advance notice on the fact that we were going to be asked to create a poster.”—Scholar | ||
| Opportunities for scholar interaction during and after the Research and Mentorship Program | Scholars and mentors suggested increasing opportunities for scholars to interact with one another during the program and finding ways to maintain contact with them after the program. | “I do wish that I had gotten to meet the other scholars earlier, or maybe more often because we only actually met, say like twice really.” –Scholar |
| “One good thing would be to make sure that . . . we hold, like, regular maybe conference calls as the program keeps going. . . . To link the current fellows with past fellows and kind of keep that community alive, and make sure that those who have finished the program are sort of kept abreast of what is happening in the field, and have an opportunity to kind of link back to [HIV Vaccine Trials Network] and the work that we do.”–Mentor |
Note. RAMP = Research and Mentorship Program.
DISCUSSION
The search for a safe and effective HIV vaccine continues to be one of the most pressing biomedical research challenges of our time. A more diverse HIV research workforce could contribute substantially to this important effort. However, if advantages of a diverse HIV vaccine research workforce are to be had, concerted efforts are needed to engage the next generation of clinical investigators of color. We developed, implemented, and evaluated a mentored research program for African American and Hispanic medical students embedded within an HIV clinical trials network. An evaluation of the first 2 RAMP cohorts demonstrated an increase in scholars’ self-reported knowledge about HIV research concepts and key professional skills that will serve them well should they wish to pursue a career in HIV research, or in academic careers more generally. Although measures to assess intention to pursue a career in HIV research did not increase significantly from baseline, qualitative data suggest that RAMP may be influential in this regard. Interviews with both scholars and mentors also revealed several factors that were key to the program’s success: highly engaged mentors; a comprehensive, network-administered program; and adequate funding levels to support the scholars’ time at their mentors’ clinical site and research-related costs. In addition, the resources and opportunities accessible through the HVTN infrastructure were seen as critical elements of the program’s success. The HVTN offered ample learning and networking opportunities, interactions with established mentors, access to a broad range of expertise and research staff at the clinical trial sites, and the opportunity to present and publish research results.
Because this is one of the first programs of its kind, we were committed to iterative evaluation and incorporated changes to RAMP in response to suggestions from scholars and mentors. For example, because many of the primary mentors are senior investigators with significant time commitments, some scholars perceived that they had limited accessibility to them. With our most current round of scholars, we advocated co-mentoring teams that actively involved junior as well as senior investigators at the site. A team mentoring approach is used commonly in academic settings29 and is thought to be an important model for developing academic medicine faculty.30 This model also expands the potential pool of mentors for future cohorts of scholars as junior investigators become more seasoned mentors. In addition, we found that once scholars completed the program, they all desired ongoing contact with RAMP. Future program development includes plans to foster peer mentorship and connection to HVTN activities. As the goals of RAMP are to both attract and retain physician scientists of color, additional efforts are needed to engage promising scholars continuously through residency and fellowship training, effectively competing with attractive options outside academia and HIV research.31–33
Limitations
Our evaluation had several limitations. First, because of the small sample size of the 2 RAMP scholar cohorts studied, only large differences between baseline and follow-up survey measures of future intent to pursue HIV research could be detected. As the majority of the scholars who participated in RAMP did so early in their medical school training, changes in intent to pursue a career in HIV vaccine research were likely small as they had not completed clinical rotations, and would not be in a position to begin a career in research for at least 5 years. However, as we did see a positive trend toward pursuing a career in the field, capturing motivations for initial RAMP participation and subsequent interest in HIV research might help us understand why this occurred given that solving the HIV problem may not be as attractive a career choice as it once was.
Second, as is typical of pipeline programs that support future workforce development, the evaluation outcomes measured are proximal to the true desired outcomes that include future publications, grants obtained, and research faculty appointments. We intend to monitor these milestones annually for all scholars completing RAMP. Lastly, although we observed improvement in RAMP scholars’ knowledge and skills, we do not know whether these can be attributed to the program beyond that experienced by a comparable group of medical school students who did not participate in RAMP. However, the highly specialized nature of the information covered (e.g., HIV vaccine–induced seropositivity) that is infrequently covered in medical school curricula make non–program-related improvements in these knowledge domains less likely. Nonetheless, based on the early successes with RAMP, a robust evaluation process that includes a comparison with a control group could help us more thoroughly explore the association of our mentored research program with the short- and long-term outcomes of interest. After demonstrating that the program itself is causally responsible for the observed changes, it would be useful to develop programs that target retention in view of repeated findings by many that, as minority scientists climb the academic or research ladder from one career stage to the next, there is increased attrition in diversity.34
Conclusions
In summary, our experience indicates that a multicomponent, mentored research experience that engages medical students from underrepresented communities and is organized within an established clinical trials network may help expand the pool of diverse physician scientists. Evaluation results from the first 2 RAMP cohorts are promising but indicate that efforts to track scholars’ progress and expand the program to sustain scholar and mentor interest over time will be vitally important for ongoing success. Given the long-term, national commitment to HIV vaccine research,35 the HVTN is well positioned to foster ongoing relationships with alumni scholars, follow the career trajectories of scholars over time, nurture longitudinal mentoring relationships, and encourage junior investigators to serve as future RAMP mentors. The HVTN can also consider opportunities for RAMP alumni to pursue vaccine research during residency and fellowship training as well as invest in mentor development and explore funding options to support ongoing commitment from RAMP mentors. Ultimately, we hope to cement long-lasting relationships with RAMP scholars that address their unique mentoring needs, strengthen their connection to HIV research, and increase the likelihood that they will go on to pursue a career in the field. We believe that others who are seeking to increase representation of minority scientists in public health research fields should consider programs that focus on early intervention, offer adequate resources, and make deliberate efforts to sustain interest over time.
Acknowledgments
The Research and Mentorship Program is supported by the HIV Vaccine Trials Network through its cooperative agreement with the National Institute of Allergy and Infectious Diseases (UM1 AI068614) and through an administrative supplement from the National Institutes of Mental Health linked to this grant.
The authors would like to acknowledge the dedicated group of Research and Mentorship Program scholars and mentors who have participated in the program. They would also like to thank Phillip Renzullo, PhD, for his commitment to supporting this early stage investigator program; Neva Pemberton, PhD, for her formative research work; Marissa McGregor for her assistance coding interviews; Lisa Donohue for her contributions to the data figures; and Alex Berger and Danielle Harden for their programmatic support.
Human Participant Protection
This project was conducted under a 45 CFR 46.101(b) exemption determination made by the Institutional Review Office of the Fred Hutchinson Cancer Research Center, approval date July 9, 2013.
References
- 1.National Academy of Sciences. Expanding Underrepresented Minority Participation: America’s Science and Technology Talent at the Crossroads. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Rastogi S, Johnson TD, Hoeffel EM, Drewery MP., Jr . Washington, DC: US Census Bureau; 2011. 2010 census brief C2010BR-06: the Black population: 2010. [Google Scholar]
- 3. Centers for Disease Control and Prevention. HIV in the United States: at a Glance. Available at: http://www.cdc.gov/hiv/statistics/basics/ataglance.html. Accessed December 17, 2013.
- 4. Association of American Medical Colleges. First-time enrollees to US medical schools, 2005–2012. Available at: https://www.aamc.org/download/310122/data/2012applicantandenrollmentdatacharts.pdf. Accessed December 17, 2013.
- 5. Association of American Medical Colleges. US Medical School Faculty, 2012. Available at: https://www.aamc.org/data/facultyroster/reports/325958/usmsf12.html. Accessed August 7, 2014.
- 6.Ennis SR, Rios-Vargas M, Albert NG. Washington, DC: US Census Bureau; 2011. 2010 census brief C2010BR-04: the Hispanic population: 2010. [Google Scholar]
- 7.Shavers VL, Fagan P, Lawrence D et al. Barriers to racial/ethnic minority application and competition for NIH research funding. J Natl Med Assoc. 2005;97(8):1063–1077. [PMC free article] [PubMed] [Google Scholar]
- 8.Moutsiakis DL, Chin PN. Why Blacks do not take part in HIV vaccine trials. J Natl Med Assoc. 2007;99(3):254–257. [PMC free article] [PubMed] [Google Scholar]
- 9.Sengupta S, Strauss RP, DeVellis R, Quinn SC, DeVellis B, Ware WB. Factors affecting African-American participation in AIDS research. J Acquir Immune Defic Syndr. 2000;24(3):275–284. doi: 10.1097/00126334-200007010-00014. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan PS, McNaghten AD, Begley E, Hutchinson A, Cargill VA. Enrollment of racial/ethnic minorities and women with HIV in clinical research studies of HIV medicines. J Natl Med Assoc. 2007;99(3):242–250. [PMC free article] [PubMed] [Google Scholar]
- 11.Sobieszczyk ME, Xu G, Goodman K, Lucy D, Koblin BA. Engaging members of African American and Latino communities in preventive HIV vaccine trials. J Acquir Immune Defic Syndr. 2009;51(2):194–201. doi: 10.1097/qai.0b013e3181990605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Djomand G, Katzman J, di Tommaso D et al. Enrollment of racial/ethnic minorities in NIAID-funded networks of HIV vaccine trials in the United States, 1988 to 2002. Public Health Rep. 2005;120(5):543–548. doi: 10.1177/003335490512000509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montefiori DC, Metch B, McElrath MJ et al. Demographic factors that influence the neutralizing antibody response in recipients of recombinant HIV-1 gp120 vaccines. J Infect Dis. 2004;190(11):1962–1969. doi: 10.1086/425518. [DOI] [PubMed] [Google Scholar]
- 14.Cocklin SL, Schmitz JE. The role of Fc receptors in HIV infection and vaccine efficacy. Curr Opin HIV AIDS. 2014;9(3):257–262. doi: 10.1097/COH.0000000000000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Getz K, Faden L. Racial disparities among clinical research investigators. Am J Ther. 2008;15(1):3–11. doi: 10.1097/MJT.0b013e31815fa75a. [DOI] [PubMed] [Google Scholar]
- 16.Marín BV, Diaz RM. Collaborative HIV Prevention Research in Minority Communities Program: a model for developing investigators of color. Public Health Rep. 2002;117(3):218–230. doi: 10.1093/phr/117.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page SE. The Difference: How the Power of Diversity Creates Better Groups, Firms, Schools and Societies. Princeton, NJ: Princeton University Press; 2007. [Google Scholar]
- 18.Smith SG, Nsiah-Kumi PA, Jones PR, Pamies RJ. Pipeline programs in the health professions, part 1: preserving diversity and reducing health disparities. J Natl Med Assoc. 2009;101(9):836–840. doi: 10.1016/s0027-9684(15)31030-0. 845–851. [DOI] [PubMed] [Google Scholar]
- 19.Reynolds CF, III, Pilkonis PA, Kupfer DJ, Dunn L, Pincus HA. Training future generations of mental health researchers: devising strategies for tough times. Acad Psychiatry. 2007;31(2):152–159. doi: 10.1176/appi.ap.31.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stoff DM, Forsyth A, Marquez ED, McClure S. Introduction: the case for diversity in research on mental health and HIV/AIDS. Am J Public Health. 2009;99(suppl 1):S8–S15. doi: 10.2105/AJPH.2008.153536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim YM. Washington, DC: The American Council on Education; 2011. Minorities in higher education: twenty-fourth status report: 2011 supplement. [Google Scholar]
- 22.Sánchez JP, Peters L, Lee-Ray E et al. Racial and ethnic minority medical students’ perceptions of and interest in careers in academic medicine. Acad Med. 2013;88(9):1299–1307. doi: 10.1097/ACM.0b013e31829f87a7. [DOI] [PubMed] [Google Scholar]
- 23.Stamm M, Buddeberg-Fischer B. The impact of mentoring during postgraduate training on doctors’ career success. Med Educ. 2011;45(5):488–496. doi: 10.1111/j.1365-2923.2010.03857.x. [DOI] [PubMed] [Google Scholar]
- 24.Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students—a review of the PubMed literature 2000–2008. BMC Med Educ. 2010;10:32. doi: 10.1186/1472-6920-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown A, Shiramizu B, Nath A, Wojna V. Translational research in NeuroAIDS: a neuroimmune pharmacology-related course. J Neuroimmune Pharmacol. 2011;6(1):80–88. doi: 10.1007/s11481-010-9222-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dolcini MM, Grinstead Reznick OA, Marin BV. Investments in the future of behavioral science: the University of California, San Francisco, Visiting Professors Program. Am J Public Health. 2009;99(suppl 1):S43–S47. doi: 10.2105/AJPH.2007.121301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sutton MY, Lanier YA, Willis LA et al. Strengthening the network of mentored, underrepresented minority scientists and leaders to reduce HIV-related disparities. Am J Public Health. 2013;103(12):2207–2214. doi: 10.2105/AJPH.2013.301345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lent RW, Brown SD, Hackett G. Toward a unifying social cognitive theory of career and academic interest, choice and performance. J Vocat Behav. 1994;45:79–122. [Google Scholar]
- 29.Luckhaupt SE, Chin MH, Mangione CM et al. Mentorship in academic general internal medicine. Results of a survey of mentors. J Gen Intern Med. 2005;20(11):1014–1018. doi: 10.1111/j.1525-1497.2005.215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeCastro R, Sambuco D, Ubel PA, Stewart A, Jagsi R. Mentor networks in academic medicine: moving beyond a dyadic conception of mentoring for junior faculty researchers. Acad Med. 2013;88(4):488–496. doi: 10.1097/ACM.0b013e318285d302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wyatt GE, Williams JK, Henderson T, Sumner L. On the outside looking in: promoting HIV/AIDS research initiated by African American investigators. Am J Public Health. 2009;99(suppl 1):S48–S53. doi: 10.2105/AJPH.2007.131094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forsyth AD, Stoff DM. Key issues in mentoring in HIV prevention and mental health for new investigators from underrepresented racial/ethnic groups. Am J Public Health. 2009;99(suppl 1):S87–S91. doi: 10.2105/AJPH.2008.155085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kahn JS, Greenblatt RM. Mentoring early-career scientists for HIV research careers. Am J Public Health. 2009;99(suppl 1):S37–S42. doi: 10.2105/AJPH.2008.135830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chubin DE. The Big Picture: Contexts for URM Training. Presented orally at: Modeling Scientific Workforce Diversity, National Institute of General Medical Sciences; October 3, 2007; Bethesda, MD.
- 35.White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States. Washington, DC: White House Office of National AIDS Policy; 2010. Available at: http://www.aids.gov/federal-resources/policies/national-hiv-aids-strategy/nhas.pdf. Accessed April 28, 2014. [Google Scholar]


