Abstract
Objectives. We describe the impact of the Step On It! intervention to link taxi drivers, particularly South Asians, to health insurance enrollment and navigate them into care when necessary.
Methods. Step On It! was a worksite initiative held for 5 consecutive days from September 28 to October 2, 2011, at John F. Kennedy International Airport in New York City. Data collected included sociodemographics, employment, health care access and use, height, weight, blood pressure, and random plasma glucose. Participants were given their results, counseled by a medical professional, and invited to participate in free workshops provided by partner organizations.
Results. Of the 466 drivers participated, 52% were uninsured, and 49% did not have a primary care provider. Of 384 drivers who had blood pressure, glucose, or both measured, 242 (63%) required urgent or regular follow-up. Of the 77 (32%) requiring urgent follow-up, 50 (65%) sought medical care at least once, of whom 13 (26%) received a new diagnosis. Of the 165 (68%) requiring regular follow-up, 68 (41%) sought medical care at least once, of whom 5 (7%) received a new diagnosis.
Conclusions. This study provides encouraging results about the potential impact of an easy-to-deliver, easily scalable workplace intervention with a large, vulnerable population.
New York City alone has more than 50 000 yellow taxi drivers and a similar number of livery drivers.1 A large majority, 94%, are immigrants, mainly originating from India, Bangladesh, Pakistan, Haiti, and West African countries.1 Taxi drivers are often at greater risk for cardiovascular disease (CVD) and associated risk factors than the general population.2,3 Studies looking exclusively at taxi drivers have found a correlation between the occupation and myocardial infarctions, multivessel disease, obesity, insulin resistance, high blood pressure, high triglycerides, and high low-density lipoproteins.3 By nature of their occupation, drivers have a sedentary lifestyle.4,5 Sedentariness in the general population has been linked to a higher CVD mortality rate, secondary to coronary heart disease, sudden heart failure, hypertension, and diabetes.6–11 Environmental exposures are also to blame for high CVD and lung cancer risk for taxi drivers. Exposure to particulate matter, which is often found at high levels in closed vehicles, has been linked to lower heart rate variability, a predictor of CVD, and to lung cancer.12–14
Other factors, such as high stress, poor working conditions, long hours, unstable income, unhealthy diet, significant concern about personal safety on the job, and institutional and organizational barriers further contribute to poorer health among taxi drivers.5,15–17 Several reports and studies on the working and living conditions of taxi drivers have been released in California; Chicago, Illinois; and New York City and described similar health profiles for this population.5,15,16 In New York City, drivers typically work 10- to 12-hour shifts 6 days a week.4,16,18 Studies have also shown that a major systems-level obstacle for taxi drivers is lack of adequate health care; 60% of taxi drivers were found to be uninsured in a Chicago study19 and 52% in a New York City study.20 The occupation-related barriers to care experienced by this largely immigrant community are further exacerbated by literacy and language barriers, financial pressures, family obligations, and cultural values.4,19,21 South Asian taxi drivers, the largest group of yellow taxi drivers in New York City, potentially face a double burden for CVD because of both the nature of their occupation and the increased CVD risk associated with South Asian ethnicity.22–27
Several studies have demonstrated the successful use of occupation-based interventions to effect lifestyle changes.17,28–31 A literature review of dietary promotion programs in the workplace demonstrated that, with industry cooperation and use of a social–ecological model of intervention, worksite interventions can have gradual and favorable results.17 In one social–ecological study, changes to workplace cafeteria food service in conjunction with behavioral interventions for workers resulted in a significant increase in fruit and vegetable consumption among participants.17 Support from workplace management was crucial for the success of this program.17 Although a paucity of data exist on interventions specifically for US taxi drivers, a number of European studies have had good results for exercise and diet interventions for taxi and other drivers.29–31 A British pilot study used a peer video to encourage drivers to make healthy lifestyle changes over a 1-year study period, resulting in 73% of participating drivers reporting a significant lifestyle change, with greater physical activity, positive diet changes, and more time spent on family activities.29 Another British study used a peer education model for CVD risk education. Peer “health champions” disseminated information about free screenings and medical referrals; more than 66% of those who received medical appointments at screenings subsequently attended them.30 In Sweden, a healthy eating workplace intervention conducted at rest stops resulted in improved nutritional balance in meal choices among truck drivers.31 The results of these studies suggest that the workplace can be an effective setting for taxi driver health interventions in the United States.28
The Immigrant Health and Cancer Disparities Service (IHCD) at Memorial Sloan-Kettering Cancer Center designed and implemented a taxi driver workplace health intervention, Step On It!, in 2011 at the John F. Kennedy (JFK) International Airport yellow cab holding lot in New York City. The Step On It! intervention incorporates specific components addressing drivers’ barriers to care, including
health insurance enrollment education and enrollment assistance to address lack of health insurance;
referrals to low-cost or free health clinics and hospitals to address financial barriers to obtaining health insurance;
referrals to culturally and linguistically appropriate care to address language and cultural barriers;
events held during work hours, providing a window of opportunity, and assistance with finding clinics with flexible hours, to address drivers’ long work hours; and
onsite health screening and counseling with triage to urgent or regular follow-up to address lack of knowledge related to current health status and need for care.
After drivers were assessed for health care access and utilization, medical history, and CVD risk factors; screened for hypertension and elevated random plasma glucose; and measured for body mass index (BMI), Step On It! used a health care access navigation and case management intervention to link drivers to health insurance enrollment and navigate them into care when necessary. We describe the impact of this intervention on the primary outcome of interest, drivers’ engagement in needed medical care.
METHODS
Step On It! was a health care access navigation and case management worksite initiative that offered health assessments (health history and health behaviors); screenings for blood pressure, random plasma glucose, BMI (defined as weight in kilograms divided by the square of height in meters), and oral health; health counseling on screening results; workshops on exercise, nutrition, yoga, stress reduction, and tobacco use cessation; and assistance with scheduling appointments for free cancer screenings and facilitated health insurance enrollment and navigation into culturally and linguistically appropriate care. Step On It! grew from the groundwork established by our community-based participatory research program, the South Asian Health Initiative, and its health fair model, which was developed for the South Asian community in New York City.32 It also included topics described as priorities in a recent IHCD taxi driver focus group study that we conducted: health care access, nutrition education, stress relief, and exercise promotion.4 Step On It! was held for 5 consecutive days from September 28 to October 2, 2011, at JFK International Airport in New York City. With the support and permission of the Port Authority of New York and New Jersey, IHCD conducted Step On It! in an unused parking lot adjacent to the airport’s yellow cab holding lot. Thousands of yellow cab drivers wait in the holding lot throughout any given day. Drivers spend an average of 30 minutes, but anywhere from 10 minutes to more than 2 hours, in the holding lot awaiting customers, and many go to the holding lot multiple times within a given work week. Step On It! was a unique intervention that used a window of opportunity, time spent waiting in the airport holding lot, to recruit drivers who, given their long work hours and poor health care access, might not otherwise have sought care.4
Outreach staff administered an intake questionnaire to participants to collect data on sociodemographics, employment, health care access and use, medical history, tobacco use, and physical activity.33 Height (using a measuring tape affixed to a fence), weight (using a 7009 Lithium Electronic Scale; Taylor USA, Las Cruces, NM), blood pressure (using a 9002 E-Sphyg 2 Digital LCD desk unit sphygmomanometer), and random plasma glucose (using a OneTouch Ultra Glucometer) were measured. Each participant was given his or her results and counseled by a medical professional on making healthy lifestyle changes; this process took approximately 10 to 20 minutes, depending on the individual’s medical history and screening results. After receiving health counseling, the taxi drivers were invited to participate in free workshops provided by our partner organizations on the topics described earlier.
The Step On It! health care access navigation and case management system included health insurance providers at the event and provided health insurance education and enrollment assistance. Because of our multiday presence at the airport, we were able to review the insurance enrollment process with the drivers 1 day and then complete the enrollment process when the driver returned with his or her documents on a subsequent day. Step On It! staff met with drivers and reviewed reasons for not seeking care and barriers to obtaining care and then assisted them in finding clinics that were well matched to their needs, including clinics with weekend and evening office hours. Referral information was provided, and appointments were made on the spot. We were able to follow up with drivers at the airport over the course of the initiative to reinforce lifestyle change recommendations and repeat screenings as needed. After the Step On It! initiative, case management staff called patients for follow-up according to a structured protocol. Drivers who did not participate in any of the available health screenings were still provided with insurance education and enrollment assistance and referrals to low-cost or free health clinics and hospitals and were free to participate in the workshops provided by our partner organizations.
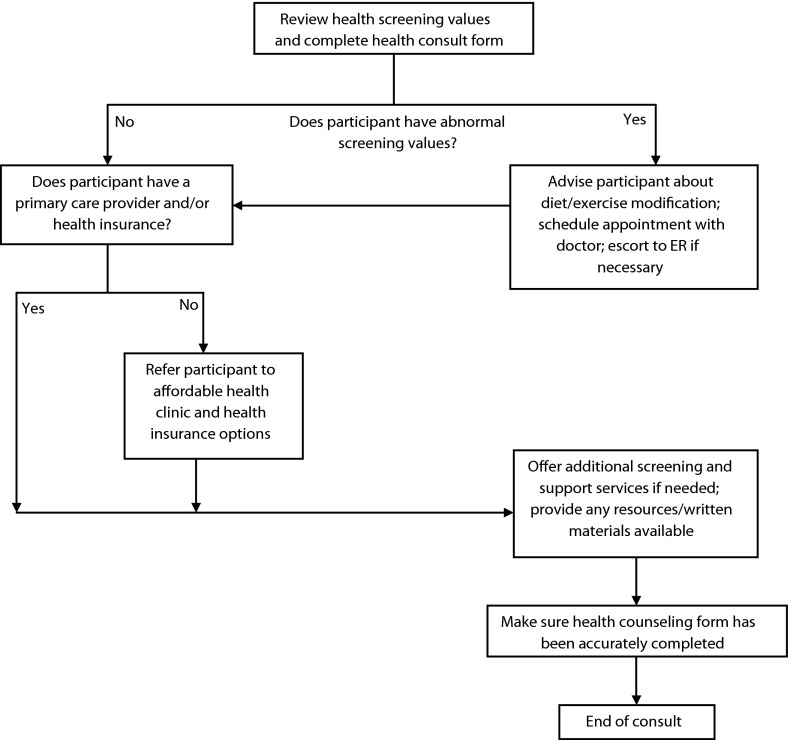
During Step On It!, if a participant had a blood pressure value higher than 180 millimeters of mercury systolic or 110 millimeters of mercury diastolic or a random plasma glucose value higher than 300 milligrams per deciliter, that participant was advised to go to a local emergency room immediately and was assigned to urgent follow-up. If any participant had a blood pressure reading between 150 and 180 millimeters of mercury systolic or between 95 and 110 millimeters of mercury diastolic or a random plasma glucose value of 150 to 200 milligrams per deciliter with no previous diagnosis of diabetes or of 200 to 300 milligrams per deciliter with a previous diagnosis of diabetes, that participant was advised to see a primary care provider (PCP) within 2 weeks. Participants without a PCP were referred to low-cost or free health clinics and hospitals. Participants in this category were also assigned to urgent follow-up. Participants who had blood pressure and random blood glucose values below the preceding ranges but still above normal values (normal blood pressure < 120/80 mmHg34; normal random glucose < 200 mg/dL35) were advised to follow up with a PCP within 3 months and were assigned to regular follow-up. Any participant who needed assistance with enrolling in insurance, finding a PCP, or scheduling an appointment or with any of the other available services (colonoscopy screening, etc.) was also assigned to regular follow-up. If a participant had normal-range values for blood pressure and random glucose, had a PCP, had health insurance, and did not want additional assistance, no follow-up was planned (Figure 1).
FIGURE 1—
Decision tree for health counseling: Step On It!, New York City, late September–early October 2011.
Note. ER = emergency room.
After the JFK event, drivers were contacted by telephone by IHCD staff to follow up on the outcome of the recommendations and the assistance with insurance enrollment and PCP appointments provided at Step On It! IHCD staff attempted to contact drivers assigned to urgent follow-up within 24 hours of the health screening; drivers assigned to regular follow-up were contacted within a month. Several additional phone calls were made to drivers by staff over the 6 months after the health screening to encourage them to enroll in insurance plans when eligible, to assist with referrals and appointment-making, and to encourage them to attend recommended and scheduled medical appointments. Referrals and appointments were made at affordable and convenient hospitals and clinics. Participants were called from at least 6 times to as many as 20 times over a period of 6 months, depending on the seriousness of their cases, number of unsuccessful attempts, and level of responsiveness. For participants not reached, a minimum of 6 attempts were made, and voice messages were left when possible (study staff had obtained participants’ permission to leave messages), all at various times (including after office hours) on both weekdays and weekends, before discontinuation of follow-up. Drivers were reminded of appointments 1 to 2 days in advance and were contacted after scheduled appointments to ascertain their attendance, document any new diagnoses or new medications prescribed, and assess self-reported adherence to prescribed medications.
We described participating drivers’ insurance status and whether they had a PCP, their health histories, and results of the health assessment. Percentages of participants who followed up with a provider were summarized. We compared pre- and postintervention percentages of participants who had diagnoses of hypertension and diabetes, who had insurance, and who had recently visited a PCP. We also compared percentages of participants who sought medical care by demographic, health care access, and health history variables. We performed comparisons between percentages using the Fisher exact test because exact tests are generally more robust against sparse cell counts in contingency tables.
RESULTS
We approached approximately 200 drivers a day, 1000 in total, for participation. Of these, 466 participated in the 5-day Step On It! event. The majority of participating taxi drivers at the onset of Step On It! were uninsured (55%), and 49% did not have a PCP. We measured blood pressure for 368 drivers and blood glucose levels for 329. BMI was calculated for 332 drivers. Fewer than half of drivers (48%) had blood pressure values less than 140/90 millimeters of mercury, only 23% had a BMI less than 25, and 9% had abnormal random glucose values (≥ 200 mg/dL). Twenty-eight percent reported having a history of hypertension, among whom 64% reported taking blood pressure medication. Fourteen percent of taxi drivers had been previously diagnosed with diabetes, 77% of whom reported taking diabetes medication. Of the respondents, 28% reported they had a previous history of cholesterol problems, 52% of whom reported taking cholesterol medication.
The Step On It! follow-up program aimed to link drivers without insurance or a PCP and those with abnormal screening results with culturally and linguistically appropriate primary care services. Of the 384 drivers who had blood pressure or glucose measured, 63% (n = 242) required either urgent or regular follow-up.
Urgent Follow-Up
Of the 384 drivers who required follow-up, 77 (32%) required urgent follow-up. Of these, 16 (21%) were unable to be reached after the event. Fifty (65%) sought medical care at least once, visiting a PCP (96%), a specialist (2%), or the emergency department (2%). An additional 7 (9%) did not seek care by the end of the follow-up period but still had plans to do so in the near future, and 4 (5%) refused to seek any medical care. Of those who sought care, 13 (26%) had a new diagnosis after their medical visit. Ten were diagnosed with hypertension (20%), and 3 with diabetes (6%); 1 had a second diagnosis of hyperlipidemia. All newly diagnosed drivers reported adhering to prescribed medication. Of those participants with a previously diagnosed condition, 6 (17%) reported being prescribed a higher medication dosage after the medical visit (Figure 2).
FIGURE 2—
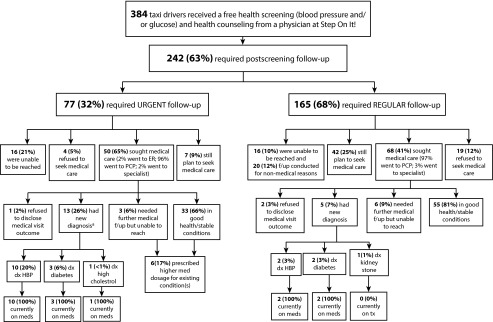
Outcomes flowchart for taxi drivers who participated in Step On It!: New York City, late September–early October 2011.
Note. dx = diagnosed; ER = emergency room; f/up = follow-up; HBP = high blood pressure; PCP = primary care provider; tx = treatment.
aTotal diagnoses are greater than the number of participants because some participants had more than 1 diagnosis.
Regular Follow-Up
Of the 282 drivers who required follow-up, 165 (68%) participants required regular follow-up. We were unable to reach 16 (10%), and an additional 20 (12%) had follow-up for nonmedical reasons (e.g., insurance or social service referrals). Sixty-eight (41%) sought medical care at least once, visiting a PCP (97%) or a specialist (3%). An additional 42 (25%) planned to seek care in the near future, and 19 (12%) refused to seek any medical care. Of those who sought care, 5 (7%) had a new diagnosis after their medical visit. Two were diagnosed with hypertension (3%), 2 with diabetes (3%), and 1 with kidney stones. All participants newly diagnosed with hypertension or diabetes reported adhering to prescribed medication. Of 38 participants who were initially screened eligible for insurance, provided with application referrals during the event, and then successfully contacted for follow-up, 12 (32%) reported filing an application for health insurance (Figure 2).
Drivers who initially reported having a PCP or recently visiting a PCP were more likely to seek medical care during the 6-month follow-up period (odds ratio [OR] = 3.52; 95% confidence interval [CI] = 1.96, 6.42; OR = 3.45; 95% CI = 1.86, 6.49, respectively). Participants with existing health insurance coverage were more likely to seek medical care (OR = 2.29; 95% CI = 1.25, 4.22), as were those with a prior diagnosis of diabetes (OR = 3.22; 95% CI = 1.41, 7.92; Table 1).
TABLE 1—
Medical Follow-Up Among Step On It! Participants (n = 242): New York City, Late September–Early October 2011
| Variables | No.a | Medical Follow-Up Status, Sought Care,b No. (%) | OR (95% CI) | Pc |
| Age, y | ||||
| ≤ 40 | 51 | 20 (17) | 0.51 (0.26, 0.98) | . . . |
| > 40 | 143 | 80 (56) | 1.00 (Ref) | |
| Residing in the United States, y | ||||
| ≤ 15 | 76 | 29 (38) | 0.50 (0.29, 0.89) | . . . |
| > 15 | 147 | 81 (55) | 1.00 (Ref) | |
| Driving taxi in the United States, y | ||||
| ≤ 15 | 146 | 65 (45) | 0.61 (0.35, 1.06) | . . . |
| > 15 | 81 | 46 (57) | 1.00 (Ref) | |
| Marital status | ||||
| Married or partnered | 172 | 85 (49) | 0.98 (0.53, 1.80) | . . . |
| Single, widowed, or divorced | 54 | 27 (50) | 1.00 (Ref) | |
| Education level | ||||
| ≤ high school graduate | 101 | 53 (52) | 1.25 (0.74, 2.12) | . . . |
| ≥ some college | 126 | 59 (47) | 1.00 (Ref) | |
| Monthly income, $ | ||||
| < 1355 | 69 | 38 (55) | 1.29 (0.71, 2.34) | . . . |
| ≥ 1355 | 119 | 58 (49) | 1.00 (Ref) | |
| English proficiency | ||||
| Very well | 102 | 44 (43) | 0.64 (0.38, 1.08) | . . . |
| Limited | 127 | 69 (54) | 1.00 (Ref) | |
| PCP status | ||||
| Has a PCP | 107 | 70 (65) | 3.52 (1.96, 6.42) | < .001 |
| Does not have a PCP | 112 | 39 (35) | 1.00 (Ref) | |
| Last PCP visit | ||||
| ≤ 6 mo | 91 | 61 (67) | 3.45 (1.86, 6.49) | < .001 |
| > 6 mo | 113 | 43 (38) | 1.00 (Ref) | |
| Insurance status | ||||
| Has insurance | 89 | 54 (61) | 2.29 (1.25, 4.22) | .005 |
| Does not have insurance | 112 | 45 (40) | 1.00 (Ref) | |
| Preintervention hypertension | ||||
| Has a prior diagnosis | 74 | 44 (59) | 1.65 (0.88, 3.10) | . . . |
| No prior diagnosis | 119 | 56 (47) | 1.00 (Ref) | |
| Preintervention diabetes | ||||
| Has a prior diagnosis | 38 | 28 (74) | 3.22 (1.41, 7.92) | .004 |
| No prior diagnosis | 166 | 77 (46) | 1.00 (Ref) | |
| Preintervention hyperlipidemia | ||||
| Has a prior diagnosis | 61 | 41 (67) | 2.37 (1.25, 4.51) | .008 |
| No prior diagnosis | 123 | 57 (46) | 1.00 (Ref) | |
Note. CI = confidence interval; OR = odds ratio; PCP = primary care provider.
All Ns are based on available cases.
Data reported are over all available data.
P values of the odds ratios were calculated using the Fisher exact test and only reported if the confidence intervals excluded the equal odds of 1.
DISCUSSION
Drivers face tremendous barriers to optimal health because of long work hours, a sedentary lifestyle, stress, and lack of adequate health care access. The taxi driver lifestyle contributes to increased risk of CVD and other comorbidities, including hypertension and diabetes, which often go unaddressed.9 The CVD risk factor assessment conducted in Step On It! corroborated this.20 This study provides encouraging results about the potential impact of an easy-to-deliver, easily scalable workplace intervention to address CVD risk in a large, vulnerable population. Step On It! provided linkages between drivers with CVD risk factors and affordable health care. Within a 6-month period, project staff reached close to 80% of drivers with a documented need for follow-up. Among the drivers reached for follow-up, those who needed urgent follow-up were more likely to seek care than those assigned to regular follow-up (65% vs 41%).
Increasing access to primary care services improves health status, particularly in minority populations living in poverty,36,37 and use of such services helps prevent illness and death.38,39 Individuals with a usual source of care—a provider from whom or facility at which they regularly receive care—experience reduced health disparities and improved health outcomes.36 Those with a usual PCP, as defined by the Medical Expenditure Panel Survey, receive a higher quality of care than those without a PCP.40,41 Of people in the United States, 86% had a usual source of ongoing care in 2009, and 76% had a usual PCP.42,43 Healthy People 2020 aims for a 10% increase in both numbers.44,45 Among New York City taxi drivers, only 45% have health insurance, and 49% do not have a usual PCP.20 Adults with health insurance and access to health care are more likely to receive preventive care and less likely to experience disparities in care.42,46,47 Lack of health insurance among taxi drivers is a significant systems-level barrier.19,20 The status of New York City drivers as independent contractors has been an obstacle to gaining health insurance.1 The advent of the Patient Protection and Affordable Care Act provides a unique opportunity to improve coordinated, integrated health care for taxi drivers.48,49 However, their Affordable Care Act uptake has been low, paralleling their low uptake of primary care (F. Gany et al., unpublished data, 2014). Ensuring uptake of health care in the taxi driver population requires a tailored approach. Lessons from men’s health initiatives, such as the Men’s Health Clinic in Baltimore, Maryland, and the Denver Men’s Health Initiative in Denver, Colorado, have emphasized the importance of a community-specific approach to both initial access to and continued use of health resources.49,50 Language, cultural, and workplace barriers faced by drivers make this essential. More than half of the taxi drivers in Step On It! reported limited English proficiency.20
This study has limitations. The sample of drivers was biased. Those who attended the event may have been more vulnerable and thus sought the assistance the event provided. Moreover, staff were unable to reach all participants in need of follow-up, which may have affected the outcomes. Drivers who were able to be reached may have had more time or resources and therefore also have been more likely to succeed at making and attending medical appointments. Those who were more likely to stay in touch with study staff may have been the ones who were more likely to follow up with care. The study was not long enough to ascertain whether the improved health access, and drivers’ attention to their health and reported adherence to prescribed medications, were sustained or whether they extinguished with the conclusion of the follow-up program. We also relied on drivers’ self-report; we did not have access to their medical charts. Despite this, the fact that all newly diagnosed drivers reported adherence to prescribed medications suggests that these types of interventions may be particularly useful for new, previously unidentified problems. Future studies should further explore the long-term impact of tailored interventions and use medical records to document outcomes. Moreover, this was not a controlled study; hence, our results are preliminary but nonetheless promising.
Addressing barriers to health care on a policy and institutional level, while simultaneously addressing community needs with direct interventions and services, is crucial for a more integrated, multilevel approach to mitigating CVD risk in this underserved occupational group. Our work implementing Step On It! and its follow-up program demonstrates the feasibility, acceptability, and preliminary effectiveness of deploying a workplace intervention in partnership with institutional authorities (in this case, the Port Authority of New York and New Jersey) to assess and address CVD risk and poor health care access among a vulnerable, hard-to-reach population. Long-term programs with institutional acceptance and buy-in, built on the Step On It! model, may be both an efficacious and a cost-effective way to improve CVD risk and health outcomes in the taxi driver community. IHCD is currently working to implement long-term programs at JFK International Airport as well as at other airports in New York City and across the country. Cost-effectiveness estimates will be an important component of these programs. Furthermore, future cohort studies should also be undertaken to investigate specific health outcomes, that is, the impact of workplace interventions on reducing CVD events such as myocardial infarctions and stroke.
Acknowledgments
Data analysis reported in this article was supported by the National Institute on Minority Health and Health Disparities (R24MD008058).
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Human Participant Protection
Approval was obtained from the Memorial Sloan-Kettering Cancer Center institutional review board.
References
- 1. New York City Taxi and Limousine Commission. 2014. Taxicab factbook. Available at: http://www.nyc.gov/html/tlc/downloads/pdf/2014_taxicab_fact_book.pdf. Accessed March 1, 2014.
- 2.Bigert C, Gustavsson P, Hallqvist J et al. Myocardial infarction among professional drivers. Epidemiology. 2003;14(3):333–339. [PubMed] [Google Scholar]
- 3.Kurosaka K, Daida H, Muto T, Watanabe Y, Kawai S, Yamaguchi H. Characteristics of coronary heart disease in Japanese taxi drivers as determined by coronary angiographic analyses. Ind Health. 2000;38(1):15–23. doi: 10.2486/indhealth.38.15. [DOI] [PubMed] [Google Scholar]
- 4.Gany FM, Gill PP, Ahmed A, Acharya S, Leng J. “Every disease... man can get can start in this cab”: focus groups to identify south Asian taxi drivers’ knowledge, attitudes and beliefs about cardiovascular disease and its risks. J Immigr Minor Health. 2013;15(5):986–992. doi: 10.1007/s10903-012-9682-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burgel BJ, Gillen M, White MC. Health and safety strategies of urban taxi drivers. J Urban Health. 2012;89(4):717–722. doi: 10.1007/s11524-012-9685-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 7.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnes AS. Obesity and sedentary lifestyles: risk for cardiovascular disease in women. Texas Heart Inst J. 2012;39(2):224–227. [PMC free article] [PubMed] [Google Scholar]
- 9.Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids. 2003;38(2):103–108. doi: 10.1007/s11745-003-1038-4. [DOI] [PubMed] [Google Scholar]
- 10.Beilin LJ. Lifestyle and hypertension—an overview. Clin Exp Hypertens. 1999;21(5-6):749–762. doi: 10.3109/10641969909061005. [DOI] [PubMed] [Google Scholar]
- 11.Kagan AR. Atherosclerosis and myocardial disease in relation to physical activity of occupation. Bull World Health Organ. 1976;53(5-6):615–622. [PMC free article] [PubMed] [Google Scholar]
- 12.Wu S, Deng F, Niu J, Huang Q, Liu Y, Guo X. Association of heart rate variability in taxi drivers with marked changes in particulate air pollution in Beijing in 2008. Environ Health Perspect. 2010;118(1):87–91. doi: 10.1289/ehp.0900818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jakobsson R, Gustavsson P, Lundberg I. Increased risk of lung cancer among male professional drivers in urban but not rural areas of Sweden. Occup Environ Med. 1997;54(3):189–193. doi: 10.1136/oem.54.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen J, Raaschou-Nielsen O, Olsen JH. Increased risk of lung cancer among different types of professional drivers in Denmark. Occup Environ Med. 1998;55(2):115–118. doi: 10.1136/oem.55.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blasi G, Leavitt J. Driving Poor: Taxi Drivers and the Regulation of the Taxi Industry in Los Angeles. Los Angeles, CA: UCLA Institute of Industrial Relations; 2006. [Google Scholar]
- 16.Waheed S, Romero-Alston L. UNFARE: Taxi drivers and the cost of moving the city. 2003. Available at: http://cdp.ujcprd.vshift.net/sites/default/files/Unfare.pdf. Accessed March 1, 2014.
- 17.Sorensen G, Linnan L, Hunt MK. Worksite-based research and initiatives to increase fruit and vegetable consumption. Prev Med. 2004;39(suppl 2):S94–S100. doi: 10.1016/j.ypmed.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 18. Schaller Consulting. The changing face of taxi and limousine drivers, U.S., large states and metro areas and New York City. 2004. Available at: http://www.schallerconsult.com/taxi/taxidriver.pdf. Accessed May 2, 2012.
- 19.Apantaku-Onayemi F, Baldyga W, Amuwo S et al. Driving to better health: Cancer and cardiovascular risk assessment among taxi cab operators in Chicago. J Health Care Poor Underserved. 2012;23(2):768–780. doi: 10.1353/hpu.2012.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gany F, Bari S, Gill Pet al. Step On It! Workplace cardiovascular risk assessment of New York City yellow taxi drivers J Immigr Minor Health In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gany F, Gill P, Baser R, Leng J. Supporting South Asian Taxi Drivers to Exercise through Pedometers (SSTEP) to decrease cardiovascular disease risk. J Urban Health. 2014;91(3):463–476. doi: 10.1007/s11524-013-9858-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anand SS, Yusuf S, Vuksan V et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE) Lancet. 2000;356(9226):279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 23.Cappuccio FP. Ethnicity and cardiovascular risk: variations in people of African ancestry and South Asian origin. J Hum Hypertens. 1997;11(9):571–576. doi: 10.1038/sj.jhh.1000516. [DOI] [PubMed] [Google Scholar]
- 24.Palaniappan LP, Wong EC, Shin JJ, Fortmann SP, Lauderdale DS. Asian Americans have greater prevalence of metabolic syndrome despite lower body mass index. Int J Obes (Lond) 2011;35(3):393–400. doi: 10.1038/ijo.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holland AT, Wong EC, Lauderdale DS, Palaniappan LP. Spectrum of cardiovascular diseases in Asian-American racial/ethnic subgroups. Ann Epidemiol. 2011;21(8):608–614. doi: 10.1016/j.annepidem.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Enas E, Senthilkumar A. Coronary artery disease in Asian Indians: an update and review. Internet J Cardiol. 2001;1(2) [Google Scholar]
- 27.Enas EA, Garg A, Davidson MA, Nair VM, Huet BA, Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1996;48(4):343–353. [PubMed] [Google Scholar]
- 28.Quintiliani L, Sattelmair J, Sorensen G. The workplace as a setting for interventions to improve diet and promote physical activity. 2007. Available at: http://www.who.int/dietphysicalactivity/Quintiliani-workplace-as-setting.pdf. Accessed March 1, 2014.
- 29. Walsall Council. Taxi! Available at: http://www.thensmc.com/sites/default/files/Taxi!%20FULL%20case%20study.pdf. Accessed March 1, 2014.
- 30.Marmot M, Allen J, Goldblatt P . Case Study Working With South Asian Taxi Drivers to Create Coronary Heart Disease Champions for Achieving Better Health in Sheffield (CABS) London, UK: Marmot Review; 2010. [Google Scholar]
- 31.Gill PE, Wijk K. Case study of a healthy eating intervention for Swedish lorry drivers. Health Educ Res. 2004;19(3):306–315. doi: 10.1093/her/cyg030. [DOI] [PubMed] [Google Scholar]
- 32.Gany F, Levy A, Basu P et al. Culturally tailored health camps and cardiovascular risk among South Asian immigrants. J Health Care Poor Underserved. 2012;23(2):615–625. doi: 10.1353/hpu.2012.0070. [DOI] [PubMed] [Google Scholar]
- 33.Changrani J, Gany FM, Cruz G, Kerr R, Katz R. Paan and Gutka use in the United States: a pilot study in Bangladeshi and Indian-Gujarati immigrants in New York City. J Immigr Refug Stud. 2006;4(1):99–110. doi: 10.300/J500v04n01_07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Heart Association. Understanding blood pressure readings. Available at: http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp. Accessed March 1, 2014.
- 35.American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Starfield B, Shi L. The medical home, access to care, and insurance: a review of evidence. Pediatrics. 2004;113(5 suppl):1493–1498. [PubMed] [Google Scholar]
- 37.Shi L, Macinko J, Starfield B, Wulu J, Regan J, Politzer R. The relationship between primary care, income inequality, and mortality in US states, 1980–1995. J Am Board Fam Pract. 2003;16(5):412–422. doi: 10.3122/jabfm.16.5.412. [DOI] [PubMed] [Google Scholar]
- 38.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations’ health: assessing the evidence. Health Aff (Millwood) 2005;(suppl web exclusives):W5-97–W5-107. doi: 10.1377/hlthaff.w5.97. [DOI] [PubMed] [Google Scholar]
- 40.Inkelas M, Schuster MA, Olson LM, Park CH, Halfon N. Continuity of primary care clinician in early childhood. Pediatrics. 2004;113(6 suppl):1917–1925. [PubMed] [Google Scholar]
- 41.Parchman ML, Burge SK. Continuity and quality of care in type 2 diabetes: a Residency Research Network of South Texas study. J Fam Pract. 2002;51(7):619–624. [PubMed] [Google Scholar]
- 42.US Department of Health and Human Services. National healthcare disparities report. 2013. Available at: http://www.ahrq.gov/research/findings/nhqrdr/nhdr12. Accessed March 1, 2014.
- 43.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: access to health care. Available at: http://meps.ahrq.gov/mepsweb/data_stats/MEPS_topics.jsp?topicid=1Z-1. Accessed March 1, 2014. [PubMed]
- 44. US Department of Health and Human Services. Healthy People 2020: 2020 topics & objectives: access to health services. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=1. Accessed March 1, 2014.
- 45.US Department of Health and Human Services. Healthy People 2020 framework. Available at: http://www.healthypeople.gov/2020/consortium/HP2020Framework.pdf. Accessed March 1, 2014.
- 46.Beal AC, Doty MM, Hernandez SE, Shea KK, Davis K. Closing the Divide: How Medical Homes Promote Equity in Health Care—Results From the Commonwealth Fund 2006 Health Care Quality Survey. New York, NY: Commonwealth Fund; 2007. [Google Scholar]
- 47.Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229–239. doi: 10.3122/jabfm.2011.03.100170. [DOI] [PubMed] [Google Scholar]
- 48.Ku L, Fund C. Promoting the Integration and Coordination of Safety-Net Health Care Providers Under Health Reform: Key Issues. New York, NY: Commonwealth Fund; 2011. [Google Scholar]
- 49. Patient Protection and Affordable Care Act, Pub L No. 111–148, 42 U.S.C. §§ 18001-18121 (2010)
- 50.Whitley EM, Jarrett NC, Young AM, Adeyemi SA, Perez LM. Building effective programs to improve men’s health. Am J Mens Health. 2007;1(4):294–306. doi: 10.1177/1557988307306956. [DOI] [PubMed] [Google Scholar]
- 51.Robertson S, Witty K, Zwolinsky S, Day R. Men’s health promotion interventions: what have we learned from previous programmes? Community Pract. 2013;86(11):38–41. [PubMed] [Google Scholar]