Abstract
Background: Diabetes mellitus and depression are highly prevalent conditions throughout the world and have significant impact on health outcomes. It has been estimated that diabetes mellitus type 2 affects about 246 million people in the world; nevertheless, incidence varies among countries. There is evidence that depression is associated with a poor metabolic control in patients with type 2 diabetes mellitus that present other health problems (such as hypertension and obesity). The aim of this study protocol is to determine if obesity increases the risk for depression in patient with diabetes type 2.
Methods: The analysis will be reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).The studies suitable for inclusion will be assessed by the Newcastle-Ottawa Scale (NOS) to determine their methodological quality. To identify the studies of interest, we will search on PubMed and EBSCO databases. We will use the following keyword combinations: "Diabetes Mellitus type 2 AND obesity AND depression", "depression AND Diabetes Mellitus type 2", "Diabetes Mellitus type 2 AND body mass index cross sectional study", "depression AND obesity cross-sectional study". Causes for exclusion will be publications that studied patients diagnosed with diabetes mellitus type 1; articles that focused on the treatment and complications of diabetes mellitus type 2; publications that have studied other clinical or psychiatric conditions (for instance, seizure disorder or history of schizophrenia, bipolar disorder, psychotic symptoms or dementia).
Conclusion: The results of this study will form the basis for a better understanding of the association between obesity and depression in patients with diabetes mellitus type 2, and will allow development of prediction tools and better interventions. It is evident that several modifiable and non-modifiable risk factors play an important role in the pathogenesis of diabetes among population. Currently, evidence for the deleterious effects of diabetes mellitus type 2 are based on cross-sectional or other observational designs. Therefore, this study will have important implications for future research and public health guidance.
Keywords: Diabetes Mellitus type 2; obesity; body mass index; depression.
Background
Diabetes and depression are highly prevalent conditions throughout the world and have significant impact on health outcomes. Diabetes mellitus is a chronic-degenerative disease, characterized by high levels of blood glucose 1– 3. It has been estimated that diabetes mellitus type 2 affects about 246 million people in the world 4; nevertheless, incidence varies among countries 5, 6. The International Diabetes Federation has anticipated an increase of 366 million people by 2030, giving a total of 552 million people with diabetes type 2 in the world 6, 7.
The diabetes type 2 is a complex disease, where hereditary and metabolic factors interfere 8, 9. Literature suggests there is a correlation between type 2 diabetes and mood alterations such as depression and neuropsychiatric disorders; for instance, major depressive disorder 10, 11, schizophrenia 12, 13, mild cognitive impairment 14, 15 and suicidal behavior 16. It also has been observed that depression could cause an increase in all-cause mortality risk (approximately 70%) 17; it is also the most common mental disorder and generates a great impact on people and society in terms of suffering, disability and economic costs, a phenomenon that seems to occur in many parts of the world; in this context, it has been reported that depression affects 350 million people worldwide 18; for example, a research by Talbot et al. suggests that depression is not only a direct consequence of diabetes; depression may also be a risk factor for the onset of diabetes type 2 19. Patients with diabetes mellitus type 2, often present a careless attitude towards their disease, resulting in metabolic decompensation, with high and low glycemic levels which could trigger mood alterations 20, 21. Diabetes mellitus 2 is also associated with a higher risk of comorbid depression compared with the general population 22. It has been suggested that diabetes type 2 could be conditioned by depression, anxiety or anguish 23– 25; nevertheless, the reason for this association is not clear 26, 27. The neurobiological mechanisms that could explain the association between depression and diabetes mellitus type 2 28 could include 1) the alterations involved in the metabolism of biogenic amines (serotonin and norepinephrine), from the adrenal-pituitary-hypothalamus axis (by increasing cortisol) 28– 30; 2) trophic agents such as Brain Derived Neurotrophic Factor (BDNF) through Glycogen Synthase Kinase-3 (GSK-3) 31, 32. The GSK-3 is a serine/threonine protein kinase that mediates the addition of phosphate molecules into serine and threonine amino acid residues. It consists of two isoforms, α and β 33, 34. It is possible that an over activation of GSK-3 play an important role in the pathogenesis of the development of schizophrenia and mood disorders such as bipolar disorder and major depression in patients with diabetes mellitus type 2 35, 36. Furthermore, it has been suggested that the presence of metabolic alterations in patients with diabetes type 2 such as obesity, could increase the severity of depression 37– 40. The distinct mechanisms that link obesity to insulin resistance and diabetes mellitus type 2 are related to an increased production of adipokines and more adipose tissue as a result 41, 42; these molecules are involved in many clinical manifestations of diabetes mellitus type 2 and they are also associated with arterial hypertension and cardiovascular disease 43. First, the adipose tissue of the obese patient becomes resistant to the action of insulin due to the effect of some of these adipokines; for instance, the tumoral necrosis factor alpha (TNF-α) and interleukine-6 (IL-6) 44. Secondly, this resistance occurs in other tissues; therefore, insulin and glucose levels increase. This increase, along with high adipokines levels (that occur in diabetes mellitus type 2), lead to different adverse events, such as endothelial dysfunction 45, increase in oxidative stress 46, impairments in lipoprotein metabolism and increase in blood pressure 47. For a review see Antuna puente et al. 48. For example, a research by Svenningsson et al. suggests an association between depression and obesity in patients with diabetes mellitus type 2 in both genders; this study reported that at least one in five men and one in three women showed depression in diabetic type 2 patients with obesity 49. Recently, a report showed that there is a positive association between having a high body mass index and the risk to develop diabetes mellitus type 2 50. In general, literature shows evidence that depression is associated with metabolic disorders in patients with type 2 diabetes mellitus 27.
In this work we will focus on searching a correlation between obesity and depression in patient with diabetes type 2. The aim of this study is to determine if obesity in patients with diabetes type 2 increases the risk of depression.
PICOT QUESTION: Does obesity increase the risk of depression in Diabetes Mellitus type 2 patients?
Methods/Design
The study protocol will be conducted and reported in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 51. In accordance with the guidelines, our study protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) 52, on 08 October, 2014 (registration number CRD42014014034).
Literature search strategy
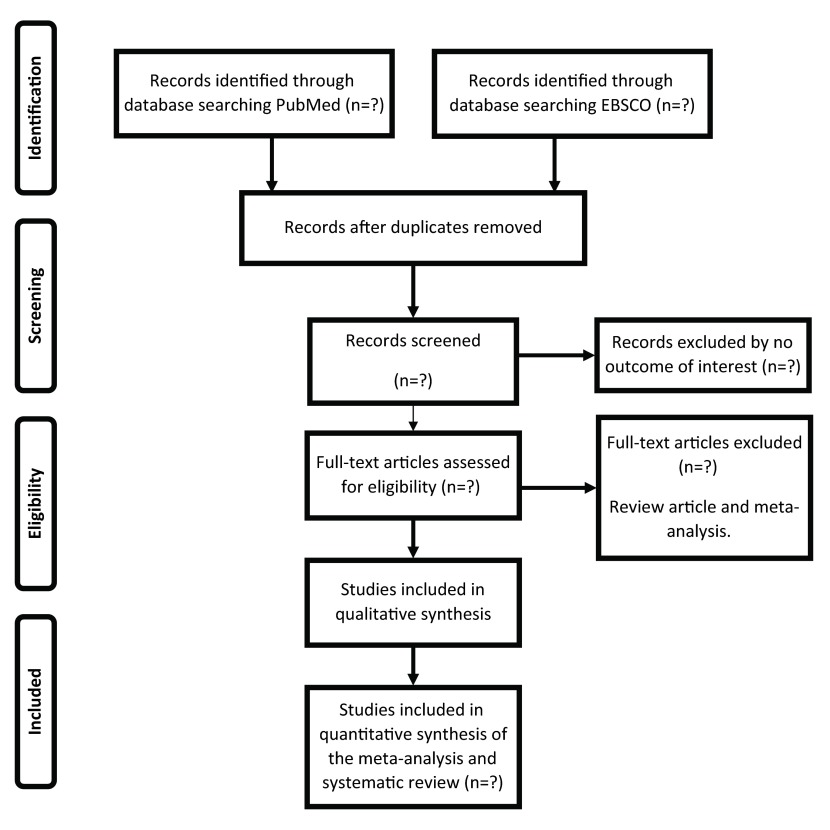
The selection of publications and the reporting of results for the study protocol will be conducted in accordance with the PRISMA guidelines 51. We will search on PubMed and EBSCO databases. We will further scan reference lists in relevant reviews and publications retrieved for the purpose of our study protocol. There will be no initial limit on the date of publication. We will use the following keyword combinations: "Diabetes Mellitus type 2 AND obesity AND depression", "depression AND Diabetes Mellitus type 2", "Diabetes Mellitus type 2 AND body mass index AND cross sectional study", "depression AND obesity AND cross-sectional study". The bibliography of the articles chosen will also be examined in order to find more articles that might not be on the electronic databases. We will only include case-control, cross-sectional and cohort studies. The planned procedure is illustrated in Figure 1.
Figure 1. Flow chart for the search strategy and the inclusion/exclusion criteria used in the meta-analysis and systematic review.
Eligibility criteria
Titles and abstracts will be screened for eligibility according to the following inclusion and exclusion criteria.
Inclusion criteria
For the purpose of this study protocol will be included publications in English language that examined the relation of body mass index (BMI > 30 kg/m 2) and severity of depression in patients with diabetes type 2.
Exclusion criteria
Causes for exclusion will be: publications that studied patients diagnosed with diabetes mellitus type 1; articles that focused on treatment and/or complications of diabetes mellitus type 2; publications or clinical trial that have focused on treatment of metabolic and psychiatric disease (for instance, mood stabilizers, neuroleptic, antidepressant, benzodiazepines, seizure disorder, history of schizophrenia, bipolar disorder, psychotic symptoms and dementia).
Type of studies
This study protocol will include case-control, cross-sectional and existing cohort studies up to date.
Type of participants
The participants will be adults (aged 18 years and over), diagnosed with diabetes mellitus type 2. For the purpose of this review, only overweight and obese type 2 diabetes mellitus patients with symptoms of depression will be included.
Screening
First, Two independent reviewers will read the titles of all the citations retrieved from the electronic database searches and removed all citations that are clearly not related to our study. Next, the abstract will be assessed to determine if the study satisfies the inclusion criteria. If from the abstract it is unclear whether the selection criteria are met or not, the full article will be scanned. Any discrepancy for inclusion will be discussed with a third or fourth author. Once the appropriate articles have been chosen for further analysis, two or three authors (independently) will be involved in the assessment of each article and data extraction. Further studies may be excluded as a result of not being relevant for our study. Further studies may be included through searching the reference lists in publications selected for the review. All the studies included will be read in detail and the relevant information extracted. The degree of agreement between the observers will be calculated by the Kappa coefficient; the studies that cause disagreement will be reviewed again, then the observers will decide the inclusion/exclusion together. The studies selected will be evaluated for quality and incorporation of gender perspective. Studies deemed for inclusion will be scored for methodological quality using the Newcastle-Ottawa Assessment Scale (NOS) 53. Results will be analyzed using a narrative synthesis. To give more support to our analysis, we will consider the GRADES scale procedures ( http://www.gradeworkinggroup.org).
Analysis of results
A descriptive synthesis of important characteristics will be undertaken independently, including, author, year study, sample characteristics, type of study design, length of follow-up (for cohort studies), exposure variable characteristics, dependent variable characteristics, method used to ascertain diabetes status and body mass index; assessment of depression, relative risk or equivalent associated with diabetes mellitus type 2 and obesity. A quantitative synthesis of effects will not be attempted because of substantial methodological heterogeneity among studies.
Whenever possible, adjusted relative risk (RR) or equivalent and associated 95% CI will be extracted directly from studies. For studies that present RR by subgroups (for example, relative risk associated with Body Mass Index, kg/m 2 ≥30) the data for each subgroup will be additionally extracted. Authors will be contacted via email for any missing relevant information. Also, data will be analyzed descriptively. The systematic review will be presented in tables comparing quality measurements and the data previously mentioned.
Discussion
The aim of this study protocol is to verify if there is a direct relation between depression and obesity in patients diagnosed with Diabetes Mellitus type 2, with the aim of improving the treatment of these patients, through an updated and quantitative estimate of the risk of depression associated with obesity. This study protocol will include a wide number of study designs; therefore, a subgroup analysis will be performed, to understand the relation between depression and obesity in patients with type 2 diabetes according to type of study. Furthermore, literature suggests that age is associated with depression, as well as other emotional alterations 54, 55; therefore, age could also influence patients with obesity to develop depression. Nevertheless; up to today, there are no-systematic reviews that search for this association. It is important to know if there is a connection between a high body mass index (BMI) and emotional alterations of diabetes mellitus type 2 patients 56, 57. Finally, depression and obesity appear to be linked with poorer behavioral management of diabetes and glycemic control; therefore, the need for comprehensive interventions worldwide that target depression in conjunction with the type 2 diabetes mellitus management. The findings from this study protocol will be widely disseminated through discussions with stake-holders, publication in a peer-reviewed journal and a conference presentation. This study protocol on diabetes and depression will bring to light knowledge gaps in the area and will offer directions for future researches.
Abbreviations
BDNF: Brain Derived Neurotrophic Factor; BMI: Body Mass Index; CRH: Corticotropin-Releasing Hormone; GSK-3: Glycogen Synthase Kinase-3; IL-6: Interleukine-6; NOS: Newcastle-Ottawa Scale; PRISMA: preferred reporting items for systematic reviews and meta-analyses; PROSPERO: Prospective Register of Systematic Reviews; RR: risk ratio; TNF-α: Tumoral Necrosis Factor alpha; T2DM: Type 2 Diabetes Mellitus.
Funding Statement
This study protocol presents independent research. The views expressed in this publication are those of the author(s); therefore this study has not received funding.
v1; ref status: indexed
References
- 1. Alharbi KK, Khan IA, Munshi A, et al. : Association of the genetic variants of insulin receptor substrate 1 (IRS-1) with type 2 diabetes mellitus in a Saudi population. Endocrine. 2014;47(2):472–477. 10.1007/s12020-014-0177-2 [DOI] [PubMed] [Google Scholar]
- 2. Ganasegeran K, Renganathan P, Manaf RA, et al. : Factors associated with anxiety and depression among type 2 diabetes outpatients in Malaysia: a descriptive cross-sectional single-centre study. BMJ Open. 2014;4(4):e004794. 10.1136/bmjopen-2014-004794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. 10.2337/dc10-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garduno-Diaz SD, Khokhar S: Prevalence, risk factors and complications associated with type 2 diabetes in migrant South Asians. Diabetes Metab Res Rev. 2012;28(1):6–24. 10.1002/dmrr.1219 [DOI] [PubMed] [Google Scholar]
- 5. Alibasic E, Ramic E, Alic A: Prevention of diabetes in family medicine. Mater Sociomed. 2013;25(2):80–82. 10.5455/msm.2013.25.80-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wild S, Roglic G, Green A, et al. : Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. 10.2337/diacare.27.5.1047 [DOI] [PubMed] [Google Scholar]
- 7. Scanlon PH, Aldington SJ, Stratton IM: Epidemiological issues in diabetic retinopathy. Middle East Afr J Ophthalmol. 2013;20(4):293–300. 10.4103/0974-9233.120007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bershtein LM, Vasil'ev DA, Poroshina TE, et al. : [Hormonal-metabolic pattern of postmenopausal females with new onset of diabetes mellitus type 2: the role of cancer and hereditary predisposition to diabetes]. Vestn Ross Akad Med Nauk. 2013; (2):29–34. [DOI] [PubMed] [Google Scholar]
- 9. Ginter E, Simko V: Type 2 diabetes mellitus, pandemic in 21st century. Adv Exp Med Biol. 2012;771:42–50. 10.1007/978-1-4614-5441-0_6 [DOI] [PubMed] [Google Scholar]
- 10. Kohler B, Kruse J: [Treatment of a patient with type-2 diabetes mellitus and a depressive disorder]. Dtsch Med Wochenschr. 2014;139(12):592–595. 10.1055/s-0033-1360101 [DOI] [PubMed] [Google Scholar]
- 11. Van der Feltz-Cornelis CM, Nuyen J, Stoop C, et al. : Effect of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2010;32(4):380–395. 10.1016/j.genhosppsych.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 12. Takayanagi Y, Cascella NG, Sawa A, et al. : Diabetes is associated with lower global cognitive function in schizophrenia. Schizophr Res. 2012;142(1–3):183–187. 10.1016/j.schres.2012.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hsu JH, Chien IC, Lin CH, et al. : Incidence of diabetes in patients with schizophrenia: a population-based study. Can J Psychiatry 2011;56(1):19–26. [DOI] [PubMed] [Google Scholar]
- 14. Lee YJ, Kang HM, Kim NK, et al. : Factors associated for mild cognitive impairment in older Korean adults with type 2 diabetes mellitus. Diabetes Metab J. 2014;38(2):150–157. 10.4093/dmj.2014.38.2.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Winkler A, Dlugaj M, Weimar C, et al. : Association of diabetes mellitus and mild cognitive impairment in middle-aged men and women. J Alzheimers Dis. 2014;42(4):1269–77. 10.3233/JAD-140696 [DOI] [PubMed] [Google Scholar]
- 16. Myers AK, Grannemann BD, Lingvay I, et al. : Brief report: depression and history of suicide attempts in adults with new-onset Type 2 Diabetes. Psychoneuroendocrinology. 2013;38(11):2810–2814. 10.1016/j.psyneuen.2013.06.013 [DOI] [PubMed] [Google Scholar]
- 17. Eaton WW, Martins SS, Nestadt G, et al. : The burden of mental disorders. Epidemiol Rev. 2008;30:1–14. 10.1093/epirev/mxn011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Marcus M, Yasamy MT, Van Ommeren M, et al. : Depression: A global public health concern. World health organization paper on depression. 2012;6–8. Reference Source [Google Scholar]
- 19. Talbot F, Nouwen A: A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care. 2000;23(10):1556–1562. 10.2337/diacare.23.10.1556 [DOI] [PubMed] [Google Scholar]
- 20. Shao W, Ahmad R, Khutoryansky N, et al. : Evidence supporting an association between hypoglycemic events and depression. Curr Med Res Opin. 2013;29(12):1609–1615. 10.1185/03007995.2013.830599 [DOI] [PubMed] [Google Scholar]
- 21. Bai F, Jiang FF, Lu JJ, et al. : The impact of hyperglycemic emergencies on the kidney and liver. J Diabetes Res. 2013;2013:967097. 10.1155/2013/967097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ell K, Katon W, Xie B, et al. : Collaborative care management of major depression among low-income, predominantly Hispanic subjects with diabetes: a randomized controlled trial. Diabetes Care. 2010;33(4):706–713. 10.2337/dc09-1711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sumlin LL, Garcia TJ, Brown SA, et al. : Depression and adherence to lifestyle changes in type 2 diabetes: a systematic review. Diabetes Educ. 2014;40(6):731–744. 10.1177/0145721714538925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zeman M, Jirak R, Zak A, et al. : [Metabolic syndrome and depression--clinical relations]. Cas Lek Cesk 2008;147(2):75–80. [PubMed] [Google Scholar]
- 25. Stankovic Z, Jasović-Gasić M, Lecić-Tosevski D: Psychological problems in patients with type 2 diabetes--clinical considerations. Vojnosanit Pregl. 2013;70(12):1138–1144. 10.2298/VSP1312138S [DOI] [PubMed] [Google Scholar]
- 26. Degmecic D, Bacun T, Kovac V, et al. : Depression, anxiety and cognitive dysfunction in patients with type 2 diabetes mellitus--a study of adult patients with type 2 diabetes mellitus in Osijek, Croatia. Coll Antropol. 2014;38(2):711–716. [PubMed] [Google Scholar]
- 27. Egede LE, Zheng D, Simpson K: Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25(3):464–470. 10.2337/diacare.25.3.464 [DOI] [PubMed] [Google Scholar]
- 28. Mello AF, Mello MF, Carpenter LL, et al. : Update on stress and depression: the role of the hypothalamic-pituitary-adrenal (HPA) axis. Rev Bras Psiquiatr. 2003;25(4):231–238. 10.1590/S1516-44462003000400010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nestler EJ, Barrot M, DiLeone RJ, et al. : Neurobiology of depression. Neuron. 2002;34(1):13–25. 10.1016/S0896-6273(02)00653-0 [DOI] [PubMed] [Google Scholar]
- 30. Belmaker RH, Agam G: Major depressive disorder. N Engl J Med. 2008;358(1):55–68. 10.1056/NEJMra073096 [DOI] [PubMed] [Google Scholar]
- 31. Groves JO: Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12(12):1079–1088. 10.1038/sj.mp.4002075 [DOI] [PubMed] [Google Scholar]
- 32. Castillo-Quan JI, Barrera-Buenfil DJ, Pérez-Osorio JM, et al. : [Depression and diabetes: from epidemiology to neurobiology]. Rev Neurol. 2010;51(6):347–359. [PubMed] [Google Scholar]
- 33. Koo J, Yue P, Gal AA, et al. : Maintaining glycogen synthase kinase-3 activity is critical for mTOR kinase inhibitors to inhibit cancer cell growth. Cancer Res. 2014;74(9):2555–2568. 10.1158/0008-5472.CAN-13-2946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Qu ZS, Li L, Sun XJ, et al. : Glycogen synthase kinase-3 regulates production of amyloid-β peptides and tau phosphorylation in diabetic rat brain. ScientificWorldJournal. 2014;2014:878123. 10.1155/2014/878123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ronai Z, Kovacs-Nagy R, Szantai E, et al. : Glycogen synthase kinase 3 beta gene structural variants as possible risk factors of bipolar depression. Am J Med Genet B Neuropsychiatr Genet. 2014;165B(3):217–222. 10.1002/ajmg.b.32223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jope RS: Glycogen synthase kinase-3 in the etiology and treatment of mood disorders. Front Mol Neurosci. 2011;4:16. 10.3389/fnmol.2011.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Blazer DG, Moody-Ayers S, Craft-Morgan J, et al. : Depression in diabetes and obesity: racial/ethnic/gender issues in older adults. J Psychosom Res. 2002;53(4):913–916. 10.1016/S0022-3999(02)00314-8 [DOI] [PubMed] [Google Scholar]
- 38. Everson SA, Maty SC, Lynch JW, et al. : Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res. 2002;53(4):891–895. 10.1016/S0022-3999(02)00303-3 [DOI] [PubMed] [Google Scholar]
- 39. Sacco WP, Wells KJ, Vaughan CA, et al. : Depression in adults with type 2 diabetes: the role of adherence, body mass index, and self-efficacy. Health Psychol. 2005;24(6):630–4. 10.1037/0278-6133.24.6.630 [DOI] [PubMed] [Google Scholar]
- 40. Labad J, Price JF, Strachan MW, et al. : Symptoms of depression but not anxiety are associated with central obesity and cardiovascular disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetologia. 2010;53(3):467–471. 10.1007/s00125-009-1628-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Julia C, Czernichow S, Charnaux N, et al. : Relationships between adipokines, biomarkers of endothelial function and inflammation and risk of type 2 diabetes. Diabetes Res Clin Pract. 2014;105(2):231–238. 10.1016/j.diabres.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 42. de Luis DA, Aller R, Izaola O, et al. : Role of insulin resistance and adipocytokines on serum alanine aminotransferase in obese patients with type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci. 2013;17(15):2059–2064. [PubMed] [Google Scholar]
- 43. Ziegler D: Type 2 diabetes as an inflammatory cardiovascular disorder. Curr Mol Med. 2005;5(3):309–322. 10.2174/1566524053766095 [DOI] [PubMed] [Google Scholar]
- 44. Pereira FO, Frode TS, Medeiros YS: Evaluation of tumour necrosis factor alpha, interleukin-2 soluble receptor, nitric oxide metabolites, and lipids as inflammatory markers in type 2 diabetes mellitus. Mediators Inflamm. 2006;2006(1):39062. 10.1155/MI/2006/39062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bachmayer C, Kemmer A, Ehrmann N, et al. : Adipokines and endothelial dysfunction in obesity WHO°III. Microvasc Res. 2013;89:129–133. 10.1016/j.mvr.2013.04.007 [DOI] [PubMed] [Google Scholar]
- 46. Crujeiras AB, Díaz-Lagares A, Carreira MC, et al. : Oxidative stress associated to dysfunctional adipose tissue: a potential link between obesity, type 2 diabetes mellitus and breast cancer. Free Radical Res. 2013;47(4):243–256. 10.3109/10715762.2013.772604 [DOI] [PubMed] [Google Scholar]
- 47. Adler AI, Stratton IM, Neil HA, et al. : Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ (Clinical research ed.). 2000;321(7258):412–419. 10.1136/bmj.321.7258.412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Antuna-Puente B, Feve B, Fellahi S, et al. : Adipokines: the missing link between insulin resistance and obesity. Diabetes Metab. 2008;34(1):2–11. 10.1016/j.diabet.2007.09.004 [DOI] [PubMed] [Google Scholar]
- 49. Svenningsson I, Björkelund C, Marklund B, et al. : Anxiety and depression in obese and normal-weight individuals with diabetes type 2: a gender perspective. Scand J Caring Sci. 2012;26(2):349–354. 10.1111/j.1471-6712.2011.00940.x [DOI] [PubMed] [Google Scholar]
- 50. Ganz ML, Wintfeld N, Li Q, et al. : The association of body mass index with the risk of type 2 diabetes: a case–control study nested in an electronic health records system in the United States. Diabetol Metab Syndr. 2014;6(1):50. 10.1186/1758-5996-6-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Moher D, Liberati A, Tetzlaff J, et al. : Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Booth A, Clarke M, Dooley G, et al. : PROSPERO at one year: an evaluation of its utility. Syst Rev. 2013;2(1):4. 10.1186/2046-4053-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Stang A: Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 54. Katon WJ, Simon G, Russo J, et al. : Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care. 2004;42(12):1222–1229. [DOI] [PubMed] [Google Scholar]
- 55. Kendrick T, Dowrick C, McBride A, et al. : Management of depression in UK general practice in relation to scores on depression severity questionnaires: analysis of medical record data. BMJ (Clinical research ed.). 2009;338:b750. 10.1136/bmj.b750 [DOI] [PubMed] [Google Scholar]
- 56. Gudelj-Radi J, Davidović D, Avramović D, et al. : [Factors mediating the depression in the adult obese outpatients]. Srp Arh Celok Lek. 2007;135(1–2):61–66. 10.2298/SARH0702061G [DOI] [PubMed] [Google Scholar]
- 57. Sacco WP, Wells KJ, Friedman A, et al. : Adherence, body mass index, and depression in adults with type 2 diabetes: the mediational role of diabetes symptoms and self-efficacy. Health Psychol. 2007;26(6):693–700. 10.1037/0278-6133.26.6.693 [DOI] [PubMed] [Google Scholar]